Abstract
Background
The non-pharmaceutical interventions (NPIs) implemented to curb the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) early in the coronavirus disease 2019 (COVID-19) pandemic, substantially disrupted the activity of other respiratory viruses. However, there is limited data from low-and-middle income countries (LMICs) to determine whether these NPIs also impacted the transmission of common enteric viruses. Here, we investigated the changes in the positivity rate of five enteric viruses among hospitalised children who presented with diarrhoea to a referral hospital in coastal Kenya, during COVID-19 pandemic period.
Methods
A total of 870 stool samples from children under 13 years of age admitted to Kilifi County Hospital between January 2019, and December 2022 were screened for rotavirus group A (RVA), norovirus genogroup II (GII), astrovirus, sapovirus, and adenovirus type F40/41 using real-time reverse-transcription polymerase chain reaction. The proportions positive across the four years were compared using the chi-squared test statistic.
Results
One or more of the five virus targets were detected in 282 (32.4%) cases. A reduction in the positivity rate of RVA cases was observed from 2019 (12.1%, 95% confidence interval (CI) 8.7–16.2%) to 2020 (1.7%, 95% CI 0.2–6.0%; p < 0.001). However, in the 2022, RVA positivity rate rebounded to 23.5% (95% CI 18.2%–29.4%). For norovirus GII, the positivity rate fluctuated over the four years with its highest positivity rate observed in 2020 (16.2%; 95% C.I, 10.0–24.1%). No astrovirus cases were detected in 2020 and 2021, but the positivity rate in 2022 was similar to that in 2019 (3.1% (95% CI 1.5%–5.7%) vs. 3.3% (95% CI 1.4–6.5%)). A higher case fatality rate was observed in 2021 (9.0%) compared to the 2019 (3.2%), 2020 (6.8%) and 2022 (2.1%) (p < 0.001).
Conclusion
Our study finds that in 2020 the transmission of common enteric viruses, especially RVA and astrovirus, in Kilifi Kenya may have been disrupted due to the COVID-19 NPIs. After 2020, local enteric virus transmission patterns appeared to return to pre-pandemic levels coinciding with the removal of most of the government COVID-19 NPIs.
Similar content being viewed by others
Introduction
Although water sanitation and hygiene (WASH) programmes and new vaccine introductions have resulted in significant reductions of paediatric diarrhoea morbidity and mortality globally, virus-associated diarrhoea is still a major cause of hospital admissions in several low and middle-income settings [1]. In 2019, approximately 300,000 deaths were recorded globally in children below 14 years of age due to rotavirus group A (RVA), norovirus GI and GII, and adenovirus F40/41 infections [2].
Following the emergence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the aetiological agent of coronavirus disease 2019 (COVID-19), several reports have indicated perturbations in the epidemiology of common enteric viruses associated with diarrhoeal disease. For instance, in France [3], Poland [4], China [5, 6] and USA [7], the prevalence of RVA during the year 2020 was lower compared to 2018 and 2019. However, in 2021 there was a surge of RVA cases in these countries. Like RVA, a decrease in cases of norovirus GII, sapovirus, adenovirus F40/41 and astrovirus was reported in 2020 in Spain [8] and Korea [9] compared to previous years. However, this decrease in virus detection has been followed by remarkable outbreaks in 2021 [5, 10]. Sporadic outbreaks of norovirus have also been reported in China in September 2020 and in the USA, where a total of 992 norovirus outbreaks were reported between August 2021 and July 2022 [5, 11, 12].
The decline of the detection rates of some of the enteric viruses in the early COVID-19 pandemic phase has been postulated to be a result of the stringent non-pharmaceutical interventions (NPIs) that were implemented to abrogate the pandemic [13]. Some of the measures included those that may impact enteric pathogen transmission such as frequent hand washing, increased hygiene, social distancing, closure of restaurants and restricted movement either locally or internationally [13].
In coastal Kenya, the prevalence of enteric viruses over the past decade has been closely monitored through a hospital-based surveillance [14]. No significant change in the prevalence has been detected for all enteric viruses except sapovirus (7.6% vs. 4.0%, p value < 0.05) pre-post rotavirus vaccine introduction in July 2014 [14]. RVA positivity in hospital admissions decreased significantly only among ELISA detected cases but not RT-PCR detected cases [15]. Continuous monitoring of these enteric viruses is key in providing insights on their epidemiology for disease management and informing public health policy. In this study, we aimed to describe the epidemiological patterns of 5 common enteric viruses associated with diarrhoea during the period spanning the COVID-19 pandemic.
Methods
Study site and population
This study was undertaken as part of our routine surveillance of RVA infections in Kilifi County Hospital (KCH), Kenya [14, 16, 17]. To be recruited, a participant had to satisfy the following criteria: (a) admitted with diarrhoea (passing of ≥ three loose stools within the last 24 h) as one of their illness symptom(s) [18], (b) aged < 13-year-old, (c) consent given from a parent or guardian to be in the study [14, 16, 17]. The surveillance started in 2009 and has continued to date (2023). In this analysis we focused on participants recruited between 1st January 2019 and 31st December 2022.
Laboratory methods
Molecular testing for common enteric viruses
Total nucleic acid (TNA) extraction
TNA was extracted from 0.2 g of stool (or 200ul if liquid) using the QIAamp Fast DNA Stool Mini kit (Qiagen, Manchester, UK) and eluted in 200ul of elution buffer as previously described [14, 16].
Virus (RT)-PCR screening
The extracted TNA was combined with the TaqMan Fast Virus 1-step master mix and virus specific primers (Additional file 1: Table S1) for each of the five viruses [16, 19] and processed on a real-time Quantistudio 5-flex instrument. The reaction mix comprised 2.5 µl of the TaqMan master mix, 1.2 µl of the primer-probe mix, 3.8 µl of nuclease free water and 5 µl of TNA. The thermocycling conditions were as follows; 95 °C for 20 s and 35 cycles of 94 °C for 15 s and 60 °C for 30 s. A cycle threshold cut-off of < 35.0 was applied to define virus positive samples for all targets screened.
RVA genotyping
TNA from RVA positives were amplified using VP4 and VP7 segment specific primers, sequenced on the Illumina Miseq platform as previously described [20]. VP4 and VP7 segments were assembled from the short read data using a de novo assembly approach as previously described [20]. RVA genotypes were assigned using either BLAST or an online RVA genotyping tool [21]. The accession numbers for the RVA genotype data are MZ096489 to MZ096854.
Statistical analysis
All statistical analysis was undertaken using R version 4.1.1 (2021-08-10). The level of government intervention was summarised using the Oxford Stringency index (SI), a composite measure based on nine response indicators including school closures, workplace closures, and travel bans, rescaled to a value from 0 to 100 (100 = strictest) [22]. Local stringency measures have been highlighted elsewhere [23] and summarized in Additional file 1: Table S2.
The virus positivity rate during each year was calculated as the proportion of samples that tested positive for the given virus given the total number of samples tested in the defined year. The data from 2019 has been previously reported elsewhere and formed a reference base of the situation before COVID-19 [16]. Comparisons across different years and groups were done using the chi-squared test statistic. Kruskal Wallis and Wilcoxon rank-sum tests were used to compare the distribution of continuous variables. Disease severity was estimated using the Vesikari Clinical Severity Scoring System Manual as previously described [16, 24].
Results
Basic demographic characteristics
Between January 2019 and December 2022, 1,613 patients aged under 13 years presented with diarrhoea as one of their illness symptoms at KCH. Of these, 870 (54.0%) consented enrolment into the study, gave a stool sample, and were included in this analysis. The reasons for missed sample collection in the study were: consent refusal (n = 344), other (n = 133), death (n = 68), discharged before sample collection(n = 35) and transferred before sample collection (n = 3).
All the 870 stool samples were screened for the five common enteric viruses. The majority of the recruited patients were in their first year of life (n = 371, 42.6%) and all suffered moderate-to-severe diarrhoeal disease (Table 1). The characteristics of the observed cases across the four years in terms of gender and age were similar (p value > 0.05). However, fatal outcome appeared more likely to occur in 2021 (9.0%) compared to 2019 (3.2%), 2020 (6.8%) and 2022 (2.1%) (p value < 0.001, Table 1). Less severe disease was also reported in 2020 compared to the other three years, Table 1.
Trends in diarrhoeal cases in the context of the COVID-19 pandemic
After the initial detection of the first COVID-19 case in Kenya on 12th March 2020 [25], the government implemented a range of NPIs to curb the pandemic (summarised in Fig. 1a using the Oxford Stringency index and local restrictions listed in supplementary Table 2). The trend of monthly recorded diarrhoea cases recruited into our surveillance between January 2019 and December 2022 is shown in Fig. 1b. The highest monthly peak in cases was recorded in 2019 before the COVID-19 pandemic. The lowest number of diarrhoea cases was in the 2020, but a gradual rebound was observed in 2021 and 2022.
(A) COVID-19 stringency index quantifying the government NPI measures aimed to curb the spread of SARS-CoV-2. (Sourcehttps://ourworldindata.org/covid-stringency-index). (B) Temporal trends of monthly diarrhoea and virus cases between January 2019 and December 2022. The blue and red line graphs show the total eligible and recruited diarrhoea cases respectively, while the bar graphs show the total virus positive cases per month
Single virus Infections and coinfections
At least one of the five virus targets were detected in 282 (32.4%) cases. The proportion of samples positive for the five viruses we tested in the stool samples for the different years is summarised in Table 1. The positivity rate of RVA deeped in 2020, at 1.7% (95% C.I, 0.2–6.0%) compared to 2019 (12.1% (95% C.I, 8.7–14.9%) and gradually rose in 2021 (16.9% (95% C.I, 12.0 − 22.8%)) and 2022 (23.5% (95% C.I, 18.2 − 29.4%)) and the differences were statistically significant (p value < 0.001) (Table 2).
The norovirus GII positivity rate fluctuated over the four years and the difference was statistically significant (p = 0.04) (Table 2). The highest positivity rate for norovirus GII was 16.2% (95% C.I, 10.0–24.1%) in 2020 and lowest at 6.4% (95% C.I, 3.4–10.8%) in 2021 (Table 2). No astrovirus cases were detected in the 2020 and 2021, but the cases in 2022 (3.3%) with a similar positivity rate to what was reported in 2019 (3.1%, Table 2). The positivity rates for sapovirus and adenovirus type F40/41 did not change across the three phases (p value > 0.05, χ2).
Between 2019 and 2022, 13 samples had a coinfection of two or more viruses of the screened viruses. The most common coinfections were RVA and norovirus GII (n = 4), adenovirus 40/41 and astrovirus (n = 3), and adenovirus 40/41 and sapovirus (n = 3) (Additional file 1: Table S3).
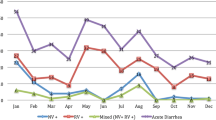
Monthly virus trends
In all the years, peak RVA cases were observed in the month of August, except in 2020 where only two RVA cases were detected, Fig. 2. The peak months for norovirus GII varied across the different years. Less than five cases were reported over the four years for adenovirus F40/41, sapovirus and astrovirus in each month. In 2020 and 2021, no astrovirus cases were detected but it re-emerged in 2022 (Fig. 2).
Monthly temporal distribution of common enteric virus cases in children under 13 years admitted to KCH with diarrhoea between January 2019 and December 2022. The black trendline shows the monthly diarrhoeal cases over time and the vertical dotted line represents when the first COVID-19 case was detected in Kenya
RVA genotypes and vaccination status of positive cases
Of the 130 RVA positive detected during the study, 87 (66.9%) and 70 (53.8%) successively sequenced in the VP7 and VP4 segment, respectively. The years 2019, 2020 and 2021 were predominated by the G3P[8] genotype (n = 48, 80.0%). In 2022, we observed replacement of the G3P[8] genotype with multiple genotypes: G2P[4] (n = 2), G9P[8] (n = 10), and G9P[4] (n = 4). To note, in the 2022 there was some incomplete genotyping due to failed sequencing in the VP4 and VP7 segments G2P[x] (n = 5) and GxP[8] (n = 8).
In 2019, 2020, 2021 and 2022, 73.8%, 67.5%, 65.1% and 66.8% of the participants had received at least one dose of the Rotarix® vaccine. Among the 130 RVA positive cases, 88 (67.7%) had received at least one dose of the Rotarix® vaccine two doses, 18 (12.9%) had not received a vaccine and 24 (16.9%) had no vaccination records. One participant was RVA positive five days after receiving a Rotarix dose and their sample genotyped as G3P[8].
Disease outcome
In the study, a total of 41 (4.7%) cases succumbed among the 870 that we analysed. Only nine of these cases were positive for at least of the viruses we tested i.e., norovirus GII (n = 4), adenovirus type F40/41 (n = 2), RVA (n = 1), sapovirus (n = 1) and a coinfection (RVA & sapovirus, n = 1) (Additional file 1: Table S3). The other 32 cases had none of the five viruses detected.
Discussion
Our study observed a decrease in paediatric diarrhoea admissions to a coastal Kenya county referral hospital in the first year of the COVID-19 pandemic (2020) compared to the pre-pandemic year (2019). This may have occurred due to the government NPIs such as (a) restriction of people movement limiting healthcare usage, (b) increased hygiene practices that may have limited transmission of the enteric pathogens [8] among other reasons. Further there was a health worker strike in December 2020.
Previous data shows that in this region, diarrhoea cases usually peak in June–July of every year [16]. Both in the years 2020 and 2021, the months of June and July coincided with high stringency measures in the country [23]. Importantly, after March 2021, targeted COVID-19 vaccination campaigns started replacing NPIs and by August 2021, the government had dropped most of the NPI measures such as closure of schools, curfews, lockdowns and restriction of public gatherings and restrictions in public transport.
While effective rotavirus vaccines are available, RVA remains the number one cause of paediatric diarrhoea admissions in many LMICs [26]. Notably, our study report a significant decrease in RVA positivity rate in 2020 compared to 2019 followed by a rebound in 2021 and 2022, a finding consistent with other studies elsewhere [4, 6,7,8]. Notably, the positivity rate of RVA in 2022 was higher compared to all the previous years. Such a resurgence of RVA activity was also been observed elsewhere e.g., in Hong Kong after the first year of the pandemic [5].
The return and apparent increase of RVA activity in the 2021 and 2022 can be attributed in a number of factors e.g., the gradual relaxation of the COVID-19 NPIs, the reduction of RVA population immunity during the first year of the pandemic due to the limited circulation of the virus, circulation of RVA strains heterologous to the Rotarix® vaccine in 2021 and 2022 (e.g. G9P[8], G9P[4] and G2P[4]). Some of these strains have been noted to have limited cross-reactivity with the Rotarix G1P[8] strain [27]. Further, vaccination delays and Rotarix® vaccine stockouts that occurred in between June 2022 and January 2023 when a vaccine switch to Rotavac® was made in Kenya [28]. The introduction of G9 genotypes in Malaysia was associated with an increase RVA prevalence [29] similar to what we observed in coastal Kenya 2022 whereby the G3P[8] was replaced by the G9P[8], G9P[4] and G2P[4] genotypes.
Our previous analysis indicated that in Kilifi, the prevalence of norovirus GII increased post-rotavirus vaccine introduction [14, 16]. Strikingly, the positivity rate of norovirus GII was highest in 2020 phase compared to other years. It appeared that norovirus activity was unimpacted by the NPI measures. Norovirus is known to be highly contagious infectious agent that requires an exceptionally small number of viral particles to transmit to susceptible individuals [30]. We hypothesize that the persistent norovirus GII activity even in the face of the pandemic NPIs may is indicative local transmission of a new strain that that the population was less immune to and reflected the resistance of norovirus inactivation to common disinfecting agents such as hypochlorite and 70% ethanol that were commonly used during the pandemic [31]. An increase in norovirus activity and multiple sporadic outbreaks have reported in the USA, China and South Africa during the COVID-19 period [5, 11, 12, 32].
While astrovirus, sapovirus, and adenovirus F40/41 are among the most common causes of diarrhoea, their prevalence is much lower than that of RVA and norovirus [14, 16]. Astrovirus was not detected in the 2020 and 2021 but re-emerged in the 2022 with a positivity rate similar to what was observed in 2019. Astrovirus and sapovirus detection on the Kenyan coast has been always characterised by very low prevalence (< 5%) [14, 16]. The non-detection of astrovirus in 2020 and 2021 does not necessarily imply it was out of circulation but if its transmission decreased, it will have required a larger sample size that that utilised in this study to detect it. This we cannot confirm that the virus was completely out of circulation during 2020 and 2021 [14, 16].
In China, enteric virus coinfections especially with RVA and norovirus was associated with severe diarrhoeal disease [33]. Similarly in coastal Kenya, a coinfection of RVA and norovirus GII coincided with severe disease. However, its key to note that 72% of the participants in the study presented with severe diarrhoeal disease. In 2020, there was a significant difference in mortality rate (9.0%) compared to the 2019 (3.2%), 2021 (6.8%) and 2022 (2.1). We hypothesize that the high mortality rate in the 2020 and partly 2021 may have been driven by the challenges with timely access to the hospitals and health care services during the pandemic, background circulation and potential infection with SARS-CoV-2 of for some of the patients seeking care for diarrhoeal disease [34].
This study had several limitations. We did not analyse healthy controls from the same population to adjust the aetiological fraction for asymptomatic carriage in the population. With the small number of detections for some of the virus targets, it hard to confidently infer seasonality without a larger study. There was substantial data missingness e.g., on deaths and almost half of the eligible participants refused consent to be in the study. For a conclusive inference of changes of the incidence of these viruses before during and after the pandemic, a population-based study with a clear population-based denominator is necessary.
In conclusion, our study observed a decrease in total diarrhoea admissions and enteric virus activity during in 2020 and 2021. However, in 2022 an increase in RVA and astrovirus activity is restored to pre-pandemic positivity rate or even higher. Our continuous enteric virus surveillance contributes understanding to the temporal changes in positivity rate of these viruses following the COVID-19 pandemic and provides important data to inform future public health policy.
Data availability
The datasets used and/or analyzed during the current study are available from the KWTRP Research repository via https://doi.org/10.7910/DVN/EG6MEH.
References
Reiner RC, Wiens KE, Deshpande A, Baumann MM, Lindstedt PA, Blacker BF et al. Mapping geographical inequalities in childhood diarrhoeal morbidity and mortality in low-income and middle-income countries, 2000–17: analysis for the Global Burden of Disease Study 2017. Lancet [Internet]. 2020;395(10239):1779–801. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0140673620301148.
Institute for Health Metrics and Evaluation I. Default results are global all-cause deaths and DALYs for 2019 with trends since 1990 [Internet]. 2022 [cited 2022 Sep 27]. Available from: https://vizhub.healthdata.org/gbd-results/.
Cohen PR, Rybak A, Werner A, Béchet S, Desandes R, Hassid F, et al. Trends in pediatric ambulatory community acquired Infections before and during COVID-19 pandemic: a prospective multicentric surveillance study in France. Lancet Reg Heal - Eur. 2022;22:1–10.
Toczylowski K, Jackowska K, Lewandowski D, Kurylonek S, Waszkiewicz-Stojda M, Sulik A. Rotavirus gastroenteritis in children hospitalized in northeastern Poland in 2006–2020: Severity, seasonal trends, and impact of immunization. Int J Infect Dis [Internet]. 2021;108:550–6. https://doi.org/10.1016/j.ijid.2021.05.070.
Chan MCW. Return of Norovirus and Rotavirus Activity in Winter 2020–21 in City with Strict COVID-19 Control Strategy, China. Emerg Infect Dis [Internet]. 2022;28(3):713–6. Available from: https://wwwnc.cdc.gov/eid/article/28/3/21-2117_article.htm.
Fang C, Zhou Z, Li J, Zhou M. Incident changes of rotavirus enteritis among children during the coronavirus disease-2019 pandemic in Hangzhou, China. J Infect [Internet]. 2022;84(1):e9–10. https://doi.org/10.1016/j.jinf.2021.09.007.
Burnett E, Parashar UD, Winn A, Tate JE. Trends in Rotavirus Laboratory Detections and Internet Search Volume Before and After Rotavirus Vaccine Introduction and in the Context of the Coronavirus Disease 2019 Pandemic-United States, 2000–2021. J Infect Dis [Internet]. 2022;226(6):967–74. Available from: http://www.ncbi.nlm.nih.gov/pubmed/35184198.
Maldonado-Barrueco A, García-Rodríguez J, Yániz-Ramirez J, Serrano-Vaquero I, Parra-Alonso JC, Vega-Nieto C et al. Impact of the SARS-CoV-2 pandemic on the prevalence and incidence of gastrointestinal viruses in children up to five Years Old: a Retrospective Cohort Study. Microbiol Spectr. 2022;10(3).
Ahn SY, Park JY, Lim IS, Chae SA, Yun SW, Lee NM, et al. Changes in the occurrence of gastrointestinal Infections after COVID-19 in Korea. J Korean Med Sci. 2021;36(24):1–9.
Douglas A, Sandmann FG, Allen DJ, Celma CC, Beard S, Larkin L. Impact of COVID-19 on national surveillance of norovirus in England and potential risk of increased Disease activity in 2021. J Hosp Infect. 2021;112:124–6.
Kambhampati AK, Wikswo ME, Barclay L, Vinjé J, Mirza SA. Norovirus outbreaks reported through NoroSTAT — 12 States, August 2012–July 2022. MMWR Recomm Reports. 2022;71(38):1222–4.
Lu Y, Zhang Z, Xie H, Su W, Wang H, Wang D, et al. The rise in Norovirus-related Acute Gastroenteritis during the fight against the COVID-19 pandemic in Southern China. Front Public Heal. 2022;9(January):1–7.
Zhang W, Wu Y, Wen B, Zhang Y, Wang Y, Yin W et al. Non-pharmaceutical interventions for COVID-19 reduced the incidence of infectious diseases: a controlled interrupted time-series study. Infect Dis Poverty [Internet]. 2023;12(1):15. https://doi.org/10.1186/s40249-023-01066-3.
Agoti CN, Curran MD, Murunga N, Ngari M, Muthumbi E, Lambisia AW et al. Differences in epidemiology of enteropathogens in children pre- and post-rotavirus vaccine introduction in Kilifi, coastal Kenya. Gut Pathog [Internet]. 2022;14(1):32. Available from: https://gutpathogens.biomedcentral.com/articles/https://doi.org/10.1186/s13099-022-00506-z.
Lambisia AW. Comparison of the Diagnostic Performance of TaqMan Array Cards, Enzyme Immunoassay, Real-Time PCR and Next Generation Sequencing in Investigation of Five Common Diarrhoea-Associated Enteric Viruses in Kilifi, Kenya [Internet]. JKUAT-COHES; 2021. Available from: http://ir.jkuat.ac.ke/handle/123456789/5621.
Lambisia AW, Onchaga S, Murunga N, Lewa CS, Nyanjom SG, Agoti CN. Epidemiological Trends of Five Common Diarrhea-Associated Enteric Viruses Pre- and Post-Rotavirus Vaccine Introduction in Coastal Kenya. Pathogens [Internet]. 2020;9(8):660. Available from: https://www.mdpi.com/2076-0817/9/8/660.
Nokes DJ, Abwao J, Pamba A, Peenze I, Dewar J, Maghenda JK et al. Incidence and Clinical Characteristics of Group A Rotavirus Infections among Children Admitted to Hospital in Kilifi, Kenya. PLOS Med [Internet]. 2008;5(7):e153. https://doi.org/10.1371/journal.pmed.0050153.
World Health organization - WHO. The Treatment of diarrhoea: a manual for physicians and other senior health workers. -- 4th rev [Internet]. Vol. 17. 2005 [cited 2023 Oct 2]. p. 562–3. Available from: https://www.who.int/publications/i/item/9241593180.
Lambisia AW, Makori TO, Mutunga M, Cheruiyot R, Murunga N, Quick J, et al. Genomic epidemiology of human adenovirus F40 and F41 in coastal Kenya: a retrospective hospital-based surveillance study (2013–2022). Virus Evol. 2023;9(1):vead023.
Makori TO, Bargul JL, Lambisia AW, Mwanga MJ, Murunga N, de Laurent ZR et al. Genomic epidemiology of the rotavirus G2P[4] strains in coastal Kenya pre- and post-rotavirus vaccine introduction, 2012–8. Virus Evol [Internet]. 2023;9(1):vead025. https://doi.org/10.1093/ve/vead025.
Vennema H, Kroneman A, Rotavirus. A Genotyping Tool [Internet]. [cited 2022 Apr 15]. Available from: https://www.rivm.nl/mpf/typingtool/rotavirusa/.
Mathieu E, Ritchie H, Rodés-Guirao L, Appel C, Giattino C, Hasell J et al. Coronavirus Pandemic (COVID-19). Our World Data. 2020.
Brand SPC, Ojal J, Aziza R, Were V, Okiro EA, Kombe IK et al. COVID-19 transmission dynamics underlying epidemic waves in Kenya. Science (80-) [Internet]. 2021;374(6570):989–94. Available from: https://www.science.org/doi/https://doi.org/10.1126/science.abk0414.
Lewis K. Vesikari Clinical Severity Scoring System Manual. Path [Internet]. 2011;(May):1–50. Available from: https://www.path.org/publications/files/VAD_vesikari_scoring_manual.pdf.
Health M. of. First case of coronavirus disease confirmed in Kenya. Press Release. 2020;1–3.
Lee B. Update on rotavirus vaccine underperformance in low- to middle-income countries and next-generation vaccines. Hum Vaccin Immunother [Internet]. 2021;17(6):1787–802. Available from: https://www.tandfonline.com/doi/full/https://doi.org/10.1080/21645515.2020.1844525.
Steele AD, Neuzil KM, Cunliffe NA, Madhi SA, Bos P, Ngwira B et al. Human rotavirus vaccine Rotarix™ provides protection against diverse circulating rotavirus strains in African infants: a randomized controlled trial. BMC Infect Dis [Internet]. 2012;12(1):213. Available from: https://bmcinfectdis.biomedcentral.com/articles/https://doi.org/10.1186/1471-2334-12-213.
Standard. Newborns at risk as shortage of the rotavirus vaccine is felt in various clinics [Internet]. [cited 2023 Jun 2]. Available from: https://www.standardmedia.co.ke/health/health-science/article/2001448711/newborns-at-risk-as-shortage-of-the-rotavirus-vaccine-is-felt-in-various-clinics.
Amit LN, John JL, Mori D, Chin AZ, Mosiun AK, Ahmed K. Increase in rotavirus prevalence with the emergence of genotype G9P[8] in replacement of genotype G12P[6] in Sabah, Malaysia. Arch Virol [Internet]. 2023;168(6):173. https://doi.org/10.1007/s00705-023-05803-9.
Teunis PFM, Moe CL, Liu P, Miller E, Lindesmith S, Baric L et al. RS,. Norwalk virus: How infectious is it? J Med Virol [Internet]. 2008;80(8):1468–76. Available from: https://onlinelibrary.wiley.com/doi/https://doi.org/10.1002/jmv.21237.
Duizer E, Bijkerk P, Rockx B, de Groot A, Twisk F, Koopmans M. Inactivation of Caliciviruses. Appl Environ Microbiol [Internet]. 2004;70(8):4538–43. Available from: https://journals.asm.org/doi/https://doi.org/10.1128/AEM.70.8.4538-4543.2004.
Khumela R, Kabue JP, de Moraes MTB, Traore AN, Potgieter N. Prevalence of Human Norovirus GII.4 Sydney 2012 [P31] between 2019 and 2021 among Young Children from Rural Communities in South Africa. Viruses [Internet]. 2023;15(8):1682. Available from: https://www.mdpi.com/1999-4915/15/8/1682.
Zhang SX, Zhou YM, Xu W, Tian LG, Chen JX, Chen SH et al. Impact of co-infections with enteric pathogens on children suffering from acute diarrhea in southwest China. Infect Dis Poverty [Internet]. 2016;5(1):64. Available from: http://idpjournal.biomedcentral.com/articles/https://doi.org/10.1186/s40249-016-0157-2.
Filip R, Gheorghita Puscaselu R, Anchidin-Norocel L, Dimian M, Savage WK. Global Challenges to Public Health Care Systems during the COVID-19 Pandemic: A Review of Pandemic Measures and Problems. J Pers Med [Internet]. 2022;12(8):1295. Available from: https://www.mdpi.com/2075-4426/12/8/1295.
Acknowledgements
We are grateful to the study participants who provided samples and members of the pathogen epidemiology and omics group at KEMRI-Wellcome Trust Programme who did sample collection and laboratory processing. This manuscript was written with the permission of Director KEMRI CGMRC.
Funding
This study was funded by the Wellcome Trust (102975, 220985 and 226002/Z/22/Z). Dr Charles Agoti was supported by the Initiative to Develop African Research Leaders (IDeAL) through the DELTAS Africa Initiative [DEL-15-003]. The DELTAS Africa Initiative is an independent funding scheme of the African Academy of Sciences (AAS)’s Alliance for Accelerating Excellence in Science in Africa (AESA) and supported by the New Partnership for Africa’s Development Planning and Coordinating Agency (NEPAD Agency). The views expressed in this report are those of the authors and not necessarily those of AAS, NEPAD Agency and The Wellcome. This research was funded in whole or in part by the Wellcome Trust [102975, 220985 and 226002/Z/22/Z], For the purpose of Open Access, the author has applied a CC-BY public copyright license to any author accepted manuscript version arising from this submission.
Author information
Authors and Affiliations
Contributions
CAN and DJN sourced the study funding. CNA, DJN and AWL designed the study laboratory assay. AWL, MM, TOM, CR, and GM did the laboratory experiments. NM and AWL managed the study data and did the data analysis. AWL did data visualization. AWL and CAN wrote the first manuscript draft. All authors read, revised, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research protocol for the study was approved at Kenya Medical Research Institute (KEMRI), by the Scientific and Ethics Review Unit (SSC#2861) in Nairobi, Kenya.
Consent for publication
All authors provide consent for publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1:
Primer and probe sequences used in the detection of five common enteric viruses
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lambisia, A.W., Murunga, N., Mutunga, M. et al. Temporal changes in the positivity rate of common enteric viruses among paediatric admissions in coastal Kenya, during the COVID-19 pandemic, 2019–2022. Gut Pathog 16, 2 (2024). https://doi.org/10.1186/s13099-023-00595-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13099-023-00595-4