Abstract
Background
Maintaining a motivated health workforce is critical to health system effectiveness and quality of care. Scant evidence exists on whether interventions aimed to strengthen health infrastructure in low-resource settings affect health workers. This study evaluated the impact of an intervention providing solar light and electricity to rural maternity facilities in Uganda on health workers’ job satisfaction.
Methods
We used a mixed-methods design embedded in a cluster randomized trial to evaluate whether and how the We Care Solar Suitcase intervention, a solar electric system providing lighting and power, affected health workers in rural Ugandan maternity facilities with unreliable light. Facilities were randomly assigned to receive the intervention or not without blinding in a cluster-randomized controlled trial. Outcomes were assessed through two rounds of surveys with health workers. We used regression analyses to examine the intervention’s impact on job satisfaction. We used an inductive approach to analyze qualitative data to understand the study context and interpret quantitative findings.
Results
We interviewed 85 health workers across 30 facilities, the majority of whom were midwives or nurses. Qualitative reports indicated that unreliable light made it difficult to provide care, worsened facility conditions, and harmed health workers and patients. Before the intervention, only 4% of health workers were satisfied with their access to light and electricity. After the installation, satisfaction with light increased by 76 percentage points [95% confidence interval (CI): 61–92 percentage points], although satisfaction with electricity did not change. Experience of negative impacts of lack of overhead light also significantly decreased and the intervention modestly increased job satisfaction. Qualitative evidence illustrated how the intervention may have strengthened health workers’ sense of job security and confidence in providing high-quality care while pointing towards implementation challenges and other barriers health workers faced.
Conclusions
Reliable access to light and electricity directly affects health workers’ ability to provide maternal and neonatal care and modestly improves job satisfaction. Policy makers should invest in health infrastructure as part of multifaceted policy strategies to strengthen human resources for health and to improve maternal and newborn health services.
Trial registration socialscienceregistry.org: AEARCTR-0003078. Registered June 12, 2018, https://www.socialscienceregistry.org/trials/3078
Additionally registered on: ClinicalTrials.gov: NCT03589625, Registered July 18, 2018, https://clinicaltrials.gov/ct2/show/NCT03589625)
Similar content being viewed by others
Background
Improving maternal and newborn care quality is critical for reaching the Sustainable Development Goals and achieving universal health coverage. Sub-Saharan Africa (SSA) has the highest burden of maternal and perinatal mortality, accounting for 66% of maternal deaths and 42% of neonatal deaths globally [1, 2]. Most of these adverse outcomes can be prevented with high quality care [1], but many health facilities in SSA fall short of care that is “safe, effective, timely, efficient, equitable, and people-centered” as recommended by the World Health Organization [3, 4].
The health care workforce is the most important resource for health systems to provide high quality care and a critical building block to meet countries’ health goals [5, 6]. SSA has only 12.8 skilled health workers per 10,000 population, compared to the global average of 52.8 [7]. For health systems to tackle the health workforce shortage and to provide high quality of care, it is a priority to maintain a motivated health care workforce [8, 9]. This is of particular importance for maternity care workers in SSA, who provide essential services around the clock and often in remote rural areas with inadequate health infrastructure. However, levels of job satisfaction and morale are generally low as less than half of midwives and others who provided maternity care reported being satisfied with their current job in previous studies in SSA [10,11,12].
Health infrastructure, including access to electricity and light in health facilities, is critical to maternal health care delivery. According to a study across eight countries in SSA, 28% of health facilities are not connected to the power grid and 34% of hospitals suffer from frequent power outages [13]. Existing evidence suggests that lack of reliable light affects health workers’ job performance, job satisfaction, morale, and retention [14,15,16,17,18,19,20]. Some health workers in Kenya, Nigeria, and Tanzania identified inadequate access to electivity as a critical factor affecting their motivation and retention [14, 17, 20]. Maternity health workers in Burkina Faso and Tanzania prefer to serve in urban over rural areas partially due to availability of electricity [18]. Recent systematic reviews have associated poor physical work conditions with high levels of health worker burnout [21, 22]. A study in Uganda found that poor infrastructure at maternity facilities frustrated health workers and made them feel they could not offer quality care to patients [23]. In Tanzania, facility infrastructure and supportive interpersonal relationships were highly correlated with providers’ job satisfaction [24]. Electricity and light are particularly important to health workers in rural areas, where power grid access is limited and health workers typically use accommodations provided by health facilities [19, 20, 23]. However, there is little empirical evidence as to whether interventions aimed to strengthen health infrastructure can improve health workers’ job satisfaction.
We conducted a cluster-randomized controlled trial to evaluate the impact of the “We Care Solar Suitcase,” a solar electric system that provides medical lighting and electricity, on health workers’ job satisfaction in maternity facilities in rural Uganda. Using a mixed-methods approach, this study examines whether and how access to light and electricity affects health workers’ outcomes.
Methods
Study setting
The study was conducted in maternity facilities in Central, Eastern, and Western regions of Uganda [25]. Uganda has a population of 44.3 million in 2019, with a total fertility rate of 4.8 live births per woman [26]. In 2016, about 74.2% of deliveries were assisted by a skilled birth attendant and 73.4% of deliveries occurred in a health facility [27]. Uganda’s health system is divided into public and private sectors. The public sector consists of national and regional hospitals and a tiered district health system composed of health centers at four levels. Most lower-level health centers are not connected to the central electricity grid and power shortages are frequent [28, 29]. A 2015 survey suggested that kerosene lamps supplied 42% of lighting needs in Health Center IIs [29]. In our study, 40% of health facilities did not have electricity or relied on lanterns as the primary source of light at the time of the baseline survey [30].
Intervention
The intervention, a “Solar Suitcase” manufactured by the non-government organization We Care Solar, is a complete solar electric system that contains high efficiency movable LED lights for medical use, rechargeable headlamps, USB ports for charging cell phones and small medical devices, and a portable fetal heart rate Doppler [30]. One Solar Suitcase was installed in each facility, with 2–4 overhead LED lights for each delivery room, depending on its size. A full description of the Solar Suitcase and its implementation, including training of health workers, maintenance, and costs have been previously published [25, 30].
Study design
We used an embedded mixed-methods design to evaluate whether and how the intervention affected health workers’ job satisfaction and their experiences of working at night [31, 32]. Specifically, we embedded qualitative data collection within an experimental design before and after the intervention implementation to understand the study context and interpret quantitative results.
The experimental study was a stepped-wedge cluster-randomized controlled trial. The trial was conducted between June 2018 and April 2019. Level II, III, and IV health centers that lacked access to a reliable, bright light source in the maternity ward were eligible for inclusion in the study. Facilities were randomized into one of two groups of 15 facilities to either receive the intervention in the first or second sequence. The focus of this analysis used data collected from the baseline (when no facility received the intervention) and the first follow up survey (6 weeks after the first 15 facilities had received the intervention) (Fig. 1). Within facilities, we interviewed all consenting health workers who were involved in labor and delivery. The interview consisted of both quantitative survey questions and qualitative open-ended questions. The purpose of the open-ended questions was to elicit narratives of the study context and intervention impact to facilitate interpretation of quantitative findings. Enumerators followed an interview guide to ask these open-ended questions and recorded health workers’ responses as field notes. Details of the trial design, including sampling methods, randomization, and sample size, have been previously published [25, 30].
A total of 15 female and 5 male enumerators conducted the health worker surveys. These enumerators had at least a certificate in Comprehensive Nursing or Midwifery and completed a 2-week training on research protocol, data collection methods, and human subjects research. With permission from the district and facility leaders, enumerators interviewed health workers at a private space using a questionnaire with both closed and open-ended questions. The research team comprised two researchers with PhDs in health policy and mixed-methods training (SR and WC), a researcher with a PhD in economics (JC), a researcher with a PhD in medicine (PW), and a researcher with a post-graduate diploma in monitoring and evaluation (BM). Three team members were female (JC, SR, and WC) and two were male (BM & PW).
Sample size
Before the trial began, we calculated the minimum detectable effect size for health workers’ satisfaction with light and electricity to be 0.62, assuming a total of 3 health workers per facility across 30 facilities, a mean health worker satisfaction score of 2 (out of a 1–5 range), and an intra-cluster correlation (ICC) of 0.3. In practice, our observed sample size was about 2 health workers per facility, the baseline satisfaction score was 3.1, and the ICC was 0.2. Using these parameters, our ex post minimum detectable effect size for health worker satisfaction was 0.36.
Measures
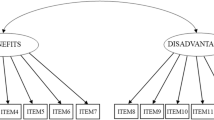
The pre-registered primary outcomes included health workers’ overall job satisfaction as well as their satisfaction with light and electricity. Job satisfaction was measured via an index and calculated as the mean of health workers’ responses to four statements about their motivation to work, how satisfied they are with their job, the morale level at their department, and their plans to stay at the same job, with higher scores indicating greater job satisfaction. Satisfaction with light and electricity is a binary variable equal to one if a health worker “agreed” or “strongly agreed” to both statements: “I am satisfied with the availability and brightness of light in this facility” and “I am satisfied with the availability of electricity in this facility.” Detailed definitions of quantitative outcomes are provided in Appendix Table 4.
For pre-registered secondary outcomes, we constructed an index to measure health worker’s experiences of the impact of lack of overhead light during nighttime deliveries in the past month. The index was calculated as the mean of 14 items that measured how often health workers conducted deliveries at night without overhead light; had to hold a torch (i.e., flashlight) in hand to see a patient; experienced lack of light that affected normal care provided; delayed care; feared to move around the facility; and were affected in ability to suture, find/use equipment, conduct examinations of the mother, provide emergency care, provide newborn care, monitor fetal heartrate, administer medication, clean up after delivery, and manage infection control. Responses were scored on a 1–5 Likert scale from “Never” to “Every nighttime delivery”, so that higher scores on the index indicated more frequent occurrence of negative impacts of lack of overhead light.
In addition to the pre-registered outcomes, we examined each of the indicators that constituted the 4-item job satisfaction index individually. We further examined outcomes that measured concepts closely related to health workers’ job satisfaction, such as job security, self-confidence, adequate support in terms of supplies and equipment, and workload. Responses to these measures were assessed on a 1–5 Likert scale to indicate levels of agreement, with higher scores indicating greater satisfaction.
As part of the open-ended questions, health workers were asked to comment on the impacts of lack of overhead light on their job, difficulties with using kerosene lanterns or candles, memorable situations where lack of lighting affected patient care, comparison between lack of lighting and other challenges at facilities, and their feelings about working without reliable light. After receiving the intervention, health workers were asked to comment on whether the intervention helped them to care for patients and what kind of challenges they encountered in using the intervention.
Data analyses
First, we evaluated the effects of the intervention on health worker outcomes by analyzing quantitative data collected from health worker surveys. To supplement the quantitative findings, we analyzed qualitative data collected from the open-ended questions.
Quantitative analysis We used linear probability models that included facility fixed effects to estimate the impact of the intervention on primary and secondary outcomes at the level of health workers. Standard errors in all models were clustered at the facility level.
To assess the robustness of the models, we used alternative model specifications including non-linear models (logistic for binary outcomes and Poisson for count outcomes), facility random effects, inclusion of health worker control variables in regression models, and adjustment of standard errors using the wild cluster bootstrap method given the small number of facilities [33]. In addition, we assessed whether the results were driven by compositional changes in health workers after installation of the intervention by examining heath worker retention rates as a robustness check. Data were analyzed with Stata version 15.1 [34].
Qualitative analyses We used an inductive analytical approach to analyze the qualitative data [32]. One member of the research team began the qualitative analysis by reading the field notes in full until reaching a high level of familiarity with the content of the text. She organized enumerators’ field notes based on the open-ended questions, created initial codes by open coding the field notes, and coded the text to generate themes. A second member of the research team read the coded text and provided feedback. The two research team members iteratively analyzed the codes, coded the field notes, and finalized categories and themes. Throughout the process, we considered how our training, identity, and world view influenced our interpretation of the qualitative findings and consulted other research team members to draw on interdisciplinary insights. We did not present the qualitative results to health worker participants for comments, but we shared the findings with our in-country team who agreed that the findings reflected the reality in the clinical setting. Qualitative data were analyzed with Taguette version 0.10.1, a web-based text management and analysis software [35].
Results
Baseline characteristics and context
All eligible health workers agreed to participate in the health worker surveys (Fig. 1). At the baseline survey, 85 health workers participated in the health worker interview. At the follow-up survey, 54 health workers were interviewed. Common reasons for loss-to-follow-up included being transferred to another facility, having left the job, or being on maternity leave. The intervention assignment had no effect on health worker retention (Table 5).
Table 1 shows the baseline characteristics of health workers and facilities and tests for balance in these characteristics across facilities randomized to the intervention or control group. Characteristics of health workers retained vs. not retained in the follow-up survey are presented in Appendix Table 6. The majority of health workers were enrolled midwives or nurses (68%), followed by clinical or nursing officers (16%) and assistants or traditional birth attendants (15%). Almost all of them had post-secondary education (98%) with an average of 7.9 years of experience since obtaining their certificates. These health workers reported conducting an average of 17 deliveries in the past month. At the facility level, most of the 30 facilities were Level III Health Centers (73%) with an average patient volume of 33.6 per month. The intervention and control groups did not differ in health worker or facility characteristics. Health workers’ assessment of light and electricity and their job satisfaction levels were also similar at baseline.
Qualitative data provided contextual information regarding what it was like to work in a maternity ward at night without sufficient light or electricity (Fig. 2 and Panel A of Table 7). Lack of light made it more difficult to provide care, affecting clinical procedures such as suturing, inserting IV lines, and monitoring blood loss. Sometimes these procedures were delayed until the morning or skipped altogether. Sometimes health workers referred out primigravida women by default because of the concern that they may not see clearly enough to suture potential tears appropriately. Lack of light or electricity also harmed health workers directly, as many felt anxious, fearful, or stressed to work at night without sufficient light and a few reported needlestick injuries. Health workers were also less motivated and felt a loss of dignity when they could not provide good care to patients. Most health workers used kerosene lamps at night, which stained the walls and ceilings, created a fire hazard, irritated the respiratory system, and only provided dim light that led to eyestrain. Other health workers reported needing to hold a torch or their own cell phone in the mouth, which made procedures harder to perform and led to damages when the phone was dropped by accident. Patients or their companions were asked to provide light or hold the torch during procedures, which eroded patient privacy and reduced community respect for health workers. Health workers also attributed a few cases of maternal and perinatal deaths to lack of light and electricity.
Intervention effects on health worker’s satisfaction with light and electricity
Table 2 shows the main results from the regression analyses. The intervention did not have a significant effect on health worker’s satisfaction with light and electricity together. However, looking at light and electricity separately, the intervention increased health workers’ satisfaction with light by 76 percentage points [95% confidence interval (CI): 61–92 percentage points], an almost 20-fold increase from the control mean of 4%. In comparison, the intervention had no effect on health workers’ satisfaction with electricity. Restricting the sample to health workers present at both surveys (Panel B of Table 2) or analyzing the outcomes as continuous instead of binary (Table 8) did not change the results.
Similarly, the intervention significantly reduced health worker’s experience of negative impacts of lack of overhead light, lowering the index score by 1.96 points (95% CI: − 2.63 to − 1.29) from a control mean of 3.28 points. This can be interpreted as a change from lack of overhead light affecting workers during some nighttime deliveries before the intervention to almost never affecting workers during nighttime deliveries after the intervention.
Qualitative data supplemented these results by showing how the intervention made many clinical and administrative procedures easier to perform, such as conducting episiotomy, suturing tears, and removing the placenta (Table 3). In their response to the open-ended questions, health workers also provided many examples of how the headlamp, overhead light, and fetal Doppler from the intervention reduced unnecessary referrals and delays in care, enhanced health workers’ personal security, and created a better work environment overall.
Intervention effects on job satisfaction
The intervention significantly increased health workers’ job satisfaction by 0.30 points (95% CI: 0.08–0.51), an increase of about 10% from the control mean (Table 2). Restricting the sample to health workers present at both surveys did not change the results (Panel B of Table 2). Regarding the individual items included in the job satisfaction index, the intervention increased health workers’ reported motivation to work hard by 0.6 points (95% CI: 0.02–1.17) from a control mean of 3.18, but had almost no effect on health workers’ job satisfaction when assessed as a single question, nor on their morale or intention to stay (Table 8).
The qualitative data provided insights that may explain the lack of stronger intervention effects on health workers’ job satisfaction (Panel B of Table 6). First, health workers mentioned a few problems related to using the Solar Suitcase effectively, such as the short battery span of the overhead light, no refill of ultrasound gel for the Doppler, and lack of training on how to use the Solar Suitcase for new staff who joined after the original installation. Based on the quantitative data, 24% of health workers recruited in the follow-up survey were not fully trained on how to use the Solar Suitcase. Second, health workers faced many other challenges at the facility in addition to insufficient light, such as lack of supplies, space, clean water, security, and accommodation. Moreover, poor community relationships and understaffing may have lowered the feeling of fulfillment health workers could derive from their job despite better infrastructure.
In addition to the primary outcome on job satisfaction, the intervention had significant positive effects on health workers’ sense of job security, confidence in their capacity to take care of patients, and capability to do their job (Fig. 3). Based on the qualitative data (Table 3), midwives worried about losing their job because they could not do it well without adequate light, which may explain the effect on job security. Health workers reported that the fetal Doppler that came with the intervention made detecting the fetal heart rate much faster and easier than a fetoscope, which improved the timeliness of care and increased patient satisfaction. Health workers also reported that the intervention provided lighting necessary to monitor patients and detect complications, which reduced delay in diagnosis and treatment. These qualitative examples illustrated how the intervention may have strengthened health workers’ confidence in providing good patient care.
Impact of intervention on individual items related to job satisfaction. Linear regression results show point estimates and 95% confidence interval. Standard errors are clustered at facility level. Sample consists of all health workers present at the baseline survey. Health workers rated to what extent they agreed with each statement on a 1–5 scale, with 1 being “strongly disagree” and 5 “strongly agree”.
In our robustness checks, we found that using alternative model specifications produced generally similar results (Table 9). The exceptions were for satisfaction with light and electricity and the job satisfaction index in non-linear models. In the logistic model, the odds of being satisfied with light and electricity was significantly higher for the intervention group. In the Poisson model, the intervention had a positive but not significant effect on the incidence rate ratio for the job satisfaction index. Including facility random effects or adjusting standard errors using the wild bootstrap method did not change the results presented in Table 2. Adding health worker controls to the regression models did not change the results (Table 10).
Discussion
Using a mixed-methods approach, this study examined whether and how an infrastructure-improvement intervention affected the job satisfaction of health workers who provided maternal and newborn care in rural Uganda. The results show that the Solar Suitcase installed in maternity facilities improved health workers’ satisfaction with light but not with electricity, reduced health worker’s experiences of negative impacts of lack of overhead light during night-time deliveries, and had a modest effect on health workers’ job satisfaction. The intervention addressed most problems posed by insufficient light in maternity facilities and strengthened health workers’ sense of job security and confidence in providing high-quality care. However, a range of challenges may have prevented the Solar Suitcase from having a larger impact on the job satisfaction of health workers who often faced many prominent barriers in a resource-constrained setting.
The installation of the Solar Suitcase increased the proportion of health workers who were satisfied with light from 4% to more than 80%. The intervention also reduced how often lack of overhead light negatively affected health workers’ ability to provide maternity and newborn care, essentially reducing the impacts from affecting some nighttime deliveries to nearly never affecting deliveries. These large impacts on subjective measures of light and electricity echo our findings previously that the Solar Suitcase was well-adopted and increased the brightness and adequacy of lighting measured by enumerators and light sensors [36]. Given these large effects, future research could explore the Solar Suitcase’s application in other clinical domains. However, the intervention did not significantly increase health worker’s satisfaction with electricity, probably because electric power derived from the Suitcase was limited to charging mobile phones and small medical devices, as opposed to, for example, powering a refrigerator to store blood products or powering the whole facility. It is also possible health workers interpreted “electricity” to mean availability of the electric grid, which the Suitcase did not affect.
Results from the study also illustrated how improvement in health infrastructure could enhance health workers’ job satisfaction, as suggested by previous research in LMIC [24, 37, 38]. The intervention increased health workers’ score on the job satisfaction index by about ten percent. Qualitative evidence suggested that better lighting and electricity improved work environment, living conditions, and personal security, which are especially important to female health workers in rural areas [39]. In addition, sufficient light may also have signaled higher quality of care to the community, earned more respect for health workers, and made their work more rewarding, which all contribute to greater job satisfaction [15, 39]. Given the importance of health workers’ motivation to successful guideline implementation in obstetric care in LMICs and the limited existing research on effective approaches to motivate health workers [9, 40], our study contributes to the literature by generating rigorous and contextual evidence for cross-sectional investment in health infrastructure as a policy option for human resources for health. [7]
However, the intervention’s impact on job satisfaction was only modest and not always significant in our sensitivity analyses. One explanation could be that while the intervention provides bright and reliable light, it is limited in that it is only installed within the maternity ward, leaving other facility areas unlit, and may not meet all of a facility’s energy needs. In addition, factors other than light or electricity, such as financial incentives, career development, or management issues [37], also play a significant role in health workers’ job satisfaction in our study setting. Qualitative data also underlined other facility challenges important to health workers, such as lack of medical supplies, equipment, space, security, and training, which are common challenges for health workers in resource-constrained settings [9, 38, 41]. Consistent with previous evidence [9, 40, 42, 43], our findings highlight the necessity of reliable light for health facilities to improve quality of maternal and newborn care while pointing toward the importance of comprehensive interventions tailored to address multiple barriers in a health system.
This study has several limitations. First, we were unable to identify or use a validated scale to measure job satisfaction of health workers that provide maternal and neonatal care in our study setting. However, we drew from existing measurement developed in similar settings, covered key aspects that determine job satisfaction for health workers in general, and supplemented quantitative surveys with qualitative data [44,45,46]. Second, there is a possibility of interviewer bias as health workers might have felt compelled to report higher job satisfaction after receiving the Solar Suitcase. However, the main items included in the job satisfaction index were not directly related to light or electricity. In addition, qualitative data provided ample examples of specific patient cases where the Solar Suitcase was critical to maternity care. Third, we were not able to conduct a thorough qualitative investigation that analyzed fully-transcribed in-depth interviews with health workers. Future research could conduct a stand-alone qualitative inquiry for a deeper understanding of the intervention’s impact on health workers. Fourth, the study had a small sample size and due to high turnover, we were only able to re-interview 64% of health workers in the follow-up survey, which might explain the lack of effects on individual job satisfaction outcomes. However, our power analysis showed that the study was sufficiently powered on the main job satisfaction index and health workers lost at the follow-up survey were not different from the remaining ones based on observed characteristics. Finally, our study assessed the effects of the intervention within a relatively short time period. A longer follow-up survey could reveal whether and how a one-time investment on health infrastructure could have sustained impact on health workers and maternity care.
Conclusions
Maintaining a motivated health workforce is essential to quality of maternal and neonatal care, but evidence on effective strategies to improve health workers’ job satisfaction in resource-constrained settings is limited. We find that installation of a solar electric system addresses the challenges posed by insufficient light in maternity facilities, enhances health workers’ ability to provide maternal and neonatal care, and may be an important determinant of health workers’ job satisfaction. Policy makers should consider greater investment in health infrastructure to strengthen human resources for health and to improve maternal and newborn care, as part of multifaceted, systemic policy changes for health system strengthening.
Availability of data and materials
The data sets during and/or analyzed during the current study available from the corresponding author on reasonable request.
References
WHO, UNICEF, UNFPA, Group WB, Division the UNP. Trends in maternal mortality: 2000 to 2017. Geneva, Switzerland, 2019.
UN Inter-Agency Group for Child Mortality Estimation. Levels and trends in child mortality: Report 2020. New York, 2020.
Bailey PE, Andualem W, Brun M, et al. Institutional maternal and perinatal deaths: a review of 40 low and middle income countries. BMC Pregnancy Childbirth. 2017;17:295.
World Health Organization. Standards for improving quality of maternal and newborn care in health facilities. 2016.
de Savigny D, Adam T. Systems thinking for health systems strengthening. Geneva: Alliance for Health Policy and Systems Research, WHO; 2009.
World Health Organization. Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. Geneva: World Health Organization, 2010 https://apps.who.int/iris/handle/10665/258734 (accessed Feb 8, 2022).
World Health Organization. Global strategy on human resources for health: Workforce 2030. Geneva, Switzerland: World Health Organization, 2016.
Global Health Workforce Alliance and World Health Organization. A universal truth: No health without a workforce. 2013.
Stokes T, Shaw EJ, Camosso-Stefinovic J, Imamura M, Kanguru L, Hussein J. Barriers and enablers to guideline implementation strategies to improve obstetric care practice in low- and middle-income countries: a systematic review of qualitative evidence. Implement Sci. 2016;11:144.
Naburi H, Mujinja P, Kilewo C, et al. Job satisfaction and turnover intentions among health care staff providing services for prevention of mother-to-child transmission of HIV in Dar es Salaam, Tanzania. Human Resour Health. 2017;15:61.
Bekru ET, Cherie A, Anjulo AA. Job satisfaction and determinant factors among midwives working at health facilities in Addis Ababa city, Ethiopia. PLoS ONE. 2017;12:e0172397.
Muluneh MD, Moges G, Abebe S, Hailu Y, Makonnen M, Stulz V. Midwives’ job satisfaction and intention to leave their current position in developing regions of Ethiopia. Women Birth. 2021; S1871–5192(21)00029-9.
Adair-Rohani H, Zukor K, Bonjour S, et al. Limited electricity access in health facilities of sub-Saharan Africa: a systematic review of data on electricity access, sources, and reliability. Global Health Sci Pract. 2013;1:249.
Adegoke AA, Atiyaye FB, Abubakar AS, Auta A, Aboda A. Job satisfaction and retention of midwives in rural Nigeria. Midwifery. 2015;31:946–56.
Essendi H, Johnson FA, Madise N, et al. Infrastructural challenges to better health in maternity facilities in rural Kenya: community and healthworker perceptions. Reprod Health. 2015;12:103.
Knight HE, Self A, Kennedy SH. Why are women dying when they reach hospital on time? A systematic review of the ‘Third Delay.’ PLoS ONE. 2013;8:e63846.
Ojakaa D, Olango S, Jarvis J. Factors affecting motivation and retention of primary health care workers in three disparate regions in Kenya. Human Resour Health. 2014. https://doi.org/10.1186/1478-4491-12-33.
Prytherch H, Kagoné M, Aninanya GA, et al. Motivation and incentives of rural maternal and neonatal health care providers: a comparison of qualitative findings from Burkina Faso, Ghana and Tanzania. BMC Health Serv Res. 2013;13:149.
Sabitova A, Sajun SZ, Nicholson S, Mosler F, Priebe S. Job morale of physicians in low-income and middle-income countries: a systematic literature review of qualitative studies. BMJ Open. 2019;9:e028657.
Shemdoe A, Mbaruku G, Dillip A, et al. Explaining retention of healthcare workers in Tanzania: moving on, coming to ‘look, see and go’, or stay? Human Resour Health. 2016. https://doi.org/10.1186/s12960-016-0098-7.
Dubale BW, Friedman LE, Chemali Z, et al. Systematic review of burnout among healthcare providers in sub-Saharan Africa. BMC Public Health. 2019;19:1247.
Dugani S, Afari H, Hirschhorn LR, et al. Prevalence and factors associated with burnout among frontline primary health care providers in low- and middle-income countries: a systematic review. Gates Open Res. 2018;2:4.
Munabi-Babigumira S, Glenton C, Willcox M, Nabudere H. Ugandan health workers’ and mothers’ views and experiences of the quality of maternity care and the use of informal solutions: a qualitative study. PLoS ONE. 2019;14:e0213511.
Mbaruku GM, Larson E, Kimweri A, Kruk ME. What elements of the work environment are most responsible for health worker dissatisfaction in rural primary care clinics in Tanzania? Hum Resour Health. 2014;12:38.
Rokicki S, Mwesigwa B, Schmucker L, Cohen JL. Shedding light on quality of care: a study protocol for a randomized trial evaluating the impact of the Solar Suitcase in rural health facilities on maternal and newborn care quality in Uganda. BMC Pregnancy Childbirth. 2019;19:306.
United Nations Department of Economic and Social Affairs Population Division. World Population Prospects 2019: Volume II: Demographic Profiles. 2019.
Uganda Bureau of Statistics—UBOS, ICF. Uganda Demographic and Health Survey 2016. 2018.
Institute for Health Metrics and Evaluation. Health service provision in Uganda: Assessing facility capacity, costs of care, and patient perspective. Seattle, WA, 2014.
United Nations Foundastion, ASD, United Nations Foundation, ASD. Health facility energy needs assessment: Uganda country summary report. 2015.
Rokicki S, Mwesigwa B, Waiswa P, Cohen J. Impact of solar light and electricity on the quality and timeliness of maternity care: a stepped-wedge cluster-randomized trial in Uganda. Global Health Sci Pract. 2021;9:777–92.
Creswell JW, Clark VLP. Choosing a mixed methods design. In: Designing and Conducting Mixed Methods Research. Thousand Oaks: SAGE Publications, 2007: 58–89.
Ulin PR, Robinson ET, Tolley EE. Qualitative methods in public health: a field guide for applied research. San Francisco: Jossey-Bass; 2005.
Rokicki S, Cohen J, Fink G, Salomon JA, Landrum MB. Inference with difference-in-differences with a small number of groups. Med Care. 2018;56:97–105.
StataCorp. Stata Statistical Software: Release 15. 2017.
Rampin, R. & Rampin, V. Taguette: open-source qualitative data analysis, https://doi.org/10.21105/joss.03522 (2021).
Rokicki S, Mwesigwa B, Waiswa P, Cohen J. The importance of light in safe childbirth: Evidence from a stepped wedge cluster randomized trial with maternity facilities in Uganda. Global Health: Science and Practice 2021; Forthcomin.
Willis-Shattuck M, Bidwell P, Thomas S, Wyness L, Blaauw D, Ditlopo P. Motivation and retention of health workers in developing countries: a systematic review. BMC Health Serv Res. 2008;8:247.
Muthuri R, Senkubuge F, Hongoro C. Determinants of motivation among healthcare workers in the East African community between 2009–2019: a systematic review. Healthcare. 2020;8:164.
Belaid L, Dagenais C, Moha M, Ridde V. Understanding the factors affecting the attraction and retention of health professionals in rural and remote areas: a mixed-method study in Niger. Hum Resour Health. 2017;15:60.
Gupta J, Patwa MC, Khuu A, Creanga AA. Approaches to motivate physicians and nurses in low- and middle-income countries: a systematic literature review. Hum Resour Health. 2021;19:4.
Girma B, Nigussie J, Molla A, Mareg M. Health professional’s job satisfaction and its determinants in Ethiopia: a systematic review and meta-analysis. Arch Public Health. 2021;79:141.
Rowe AK, Rowe SY, Peters DH, Holloway KA, Chalker J, Ross-Degnan D. Effectiveness of strategies to improve health-care provider practices in low-income and middle-income countries: a systematic review. Lancet Glob Health. 2018;6:e1163–75.
Das JK, Kumar R, Salam RA, Lassi ZS, Bhutta ZA. Evidence from facility level inputs to improve quality of care for maternal and newborn health: interventions and findings. Reprod Health. 2014;11:S4.
Alpern R, Canavan ME, Thompson JT, et al. Development of a brief instrument for assessing healthcare employee satisfaction in a low-income setting. PLoS ONE. 2013. https://doi.org/10.1371/journal.pone.0079053.
Mbindyo PM, Blaauw D, Gilson L, English M. Developing a tool to measure health worker motivation in district hospitals in Kenya. Hum Resour Health. 2009;7:40.
Faye A, Fournier P, Diop I, Philibert A, Morestin F, Dumont A. Developing a tool to measure satisfaction among health professionals in sub-Saharan Africa. Hum Resour Health. 2013;11:30.
Acknowledgements
We are grateful to the study participants and our Uganda Ministry of Health partners who devoted their time to this study. From We Care Solar, we thank Laura Stachel and Christina Briegleb for extremely valuable input on the study.
Funding
This trial was funded by a grant from the UBS Optimus Foundation to the NGO We Care Solar (WCS), with a contract to conduct an independent evaluation to Innovations for Poverty Action, the Harvard School of Public Health, and University College Dublin.
Author information
Authors and Affiliations
Contributions
WC, JC, BM, PW, and SR designed the study. SR, BM, and JC developed the protocol and managed implementation and data collection. WC, JC, and SR conducted data analysis and wrote the manuscript. WC, SR, BM, PW, and JC provided substantial comments to the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by Institutional Review Boards at the Harvard T.H. Chan School of Public Health, the Midmay Uganda Research Ethics Committee, and the Uganda National Council for Science and Technology. Written informed consent was obtained from the facility in-charge or head, all maternal care providers, and all women older than 16 years of age that presented for normal deliveries at facilities.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
See Tables 4, 5, 6, 7, 8, 9, 10.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chang, W., Cohen, J., Mwesigwa, B. et al. Impact of reliable light and electricity on job satisfaction among maternity health workers in Uganda: A cluster randomized trial. Hum Resour Health 20, 30 (2022). https://doi.org/10.1186/s12960-022-00722-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12960-022-00722-3