Abstract
Background
Burnout is characterized by physical and emotional exhaustion from long-term exposure to emotionally demanding work. Burnout affects interpersonal skills, job performance, career satisfaction, and psychological health. However, little is known about the burden of burnout among healthcare providers in sub-Saharan Africa.
Methods
Relevant articles were identified through a systematic review of PubMed, Web of Science (Thomson Reuters), and PsycINFO (EBSCO). Studies were selected for inclusion if they examined a quantitative measure of burnout among healthcare providers in sub-Saharan Africa.
Results
A total of 65 articles met our inclusion criteria for this systematic review. Previous studies have examined burnout in sub-Saharan Africa among physicians (N = 12 articles), nurses (N = 26), combined populations of healthcare providers (N = 18), midwives (N = 2), and medical or nursing students (N = 7). The majority of studies assessed burnout using the Maslach Burnout Inventory. The highest levels of burnout were reported among nurses, although all healthcare providers showed high burnout. Burnout among healthcare providers is associated with their work environments, interpersonal and professional conflicts, emotional distress, and low social support.
Conclusions
Available studies on this topic are limited by several methodological challenges. More rigorously designed epidemiologic studies of burnout among healthcare providers are warranted. Health infrastructure improvements will eventually be essential, though difficult to achieve, in under-resourced settings. Programs aimed at raising awareness and coping with burnout symptoms through stress management and resilience enhancement trainings are also needed.
Similar content being viewed by others
Introduction
Burnout is a psychological syndrome involving emotional exhaustion, feelings of helplessness, depersonalization, negative attitudes towards work and life, and reduced personal accomplishment [1]. The prevalence of burnout in high-income countries among the general working population has been reported to range between 13 and 27% [2, 3]. However, healthcare providers have been described as a high-risk population for experiencing burnout [4,5,6], and the prevalence of burnout among healthcare providers has been increasing in recent years [7]. The prevalence among physicians is reported to be as high as 70% [8] and nearly 50% among nurses [6, 9, 10]. Studies conducted in the United States show 54% of physicians [7], 35% of hospital nurses [11], and 35.2% of medical students reported burnout [12]. Similar rates of burnout among healthcare providers have been reported in other high-income countries [13,14,15].
Burnout is of great public health concern due to its physical health consequences including aches, digestive upset, and poor quality of life [12, 16,17,18]. Furthermore, burnout is highly comorbid with a myriad of psychiatric disorders including depression [19, 20], anxiety [21], substance abuse [19, 22], and suicidality [12, 23] among healthcare providers. In addition to self-reported health outcomes, burnout is associated with hypothalamus-pituitary-adrenal axis dysregulation [24,25,26], inflammatory responses [27, 28], and increased allostatic load [29, 30]. It has been reported that individuals with occupational burnout exhibit changes in the brain, such as reduction in gray matter volume of the anterior cingulate, caudate and putamen [31]. In addition, occupational burnout has also been associated with a reduced ability to downregulate emotional stressors, altered functioning of the limbic networks [32], and changes in subcortical volume [33]. Studies have shown that physicians with burnout are more likely to report career dissatisfaction and intention to leave the medical profession [34]. Lastly, burnout among healthcare providers has been associated with increased self-reported errors, reduction in time devoted to providing clinical care, and higher mortality rates [35, 36]. In summary, burnout among healthcare providers has profound personal and professional consequences, impacting the quality of patient care and functionality of healthcare systems [37].
Furthermore, appallingly little is known about the collective burden of burnout and its effects on healthcare providers in low- and middle-income countries [38]. Few studies in low- and middle- income countries have reported burnout among healthcare providers including in China [39, 40], Brazil [41], and Egypt [42, 43]. Additionally, there has been an exodus of physicians from sub-Saharan Africa due to the global labor market [44, 45]. In 2015, about 6% of all international medical graduates in the US workforce were from sub-Saharan Africa [46]. Moreover, in half of the countries in sub-Saharan Africa, more than 30% of physicians trained locally have migrated to high-income countries [47]. This has resulted in shortages of healthcare providers in sub-Saharan Africa, and a higher risk of burnout among those who remain to care for a disproportionally greater number of acutely ill patients [47]. Similar migrations from other low- and middle-income countries [48, 49] and from rural areas of high-income countries [50], have led to a scarcity of healthcare providers to care for patients. The remaining healthcare providers have increased responsibility to care for patients and a high risk of burnout. In view of these circumstances, we conducted a systematic literature review to examine the burden of burnout among healthcare providers in sub-Saharan Africa. We were specifically interested in how the construct of burnout was assessed, which healthcare sectors were included, and any interventions that were evaluated. This review is also intended to set the stage for subsequent contributions aimed at reducing the burden of burnout among healthcare providers in sub-Saharan Africa. Effective interventions will need to identify and address individual and structural barriers contributing to burnout among healthcare providers.
Methods
This systematic review was conducted according to Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines [51] (Additional file 1: Table S1).
Study selection and criteria for inclusion
In PubMed, Web of Science (Thomson Reuters), and PsycINFO (EBSCO), we identified studies using search terms for burnout and sub-Saharan African countries (Additional file 1: Table S2). Search terms included all sub-Saharan African countries. All articles published prior to February 14, 2019 were eligible for inclusion. We only included articles available in English. Based on the title and abstract review of all articles, we rejected any articles that were not relevant or did not meet the study criteria. Studies were selected for inclusion if (1) they examined a quantitative measure of burnout, (2) the study population was healthcare providers, and (3) the study was conducted in a sub-Saharan African country. Healthcare providers included physicians, nurses, medical or nursing students, midwives, and other hospital workers. Studies were excluded for (1) not including a quantitative measure of burnout, (2) not measured in healthcare providers, or (3) not conducted in sub-Saharan Africa.
Full texts of articles examining populations of healthcare providers were reviewed. Reference sections of included articles were also reviewed for additional relevant studies. A companion article examines burnout among healthcare providers in the Middle East and Northern Africa (Chemali et al, under review).
Data extraction and quality assessment
The following data were extracted independently for each included article: first author, publication year, study population, burnout assessment, reported burnout, and main findings. P-values, confidence intervals, and odds ratios were extracted when available. Methodological quality of studies was assessed using the Newcastle-Ottawa Scale for cross-sectional studies [52], the Newcastle-Ottawa Scale for cohort studies [53], and the Cochrane Risk of Bias Tool for randomized controlled trials [54]. Study quality assessment is presented in Additional file 1: Tables S3, S4, S5, and S6.
Findings
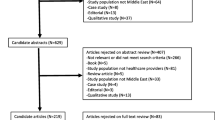
The initial literature search identified a total of 233 unique articles in PubMed, 384 articles in PsycINFO, and 322 articles in the Web of Science database (Fig. 1). Duplicate articles were removed, and 740 unique articles remained for title review. Articles were rejected on title review if they were not relevant or did not meet search criteria. After reviewing article titles, 363 articles remained for abstract review. Candidate abstracts of the remaining studies were rejected for not being relevant or not meeting the search criteria. Studies in populations of healthcare providers (N = 144) were selected for full-text review. In the full-text review, articles were rejected if they were qualitative studies, not available in English, did not include healthcare providers, or were not relevant to the search criteria.
A total of 65 articles met our inclusion criteria for this systematic review. Included articles examined burnout in sub-Saharan Africa among physicians (N = 12 articles), nurses (N = 26), combined populations of healthcare workers (N = 18), midwives (N = 2), and medical or nursing students (N = 7). Twenty-seven studies examined burnout among healthcare providers in South Africa, 13 studies in Nigeria, 4 studies in Ethiopia, and 4 studies in Ghana. Three studies each examined burnout among healthcare providers in Cameroon and Malawi. Two studies each examined burnout among healthcare providers in Kenya and Zambia. One study each examined burnout in Zimbabwe, Botswana, Mozambique, Uganda, Namibia, and Senegal. Additionally, one study examined burnout in Kenya, Tanzania, and Uganda. Of the 65 eligible articles for inclusion, 45 used versions of the Maslach Burnout Inventory (MBI) to measure burnout. An additional 5 studies used the burnout subscale of the Professional Quality of Life Scale (ProQOL), 4 studies used the Oldenburg Burnout Inventory, 3 studies used the Copenhagen Burnout Inventory, 1 study used the Executive Burnout Scale, and 1 study used the Compassion Fatigue Self Test.
Burnout among physicians
Twelve articles examined burnout among physicians in sub-Saharan Africa, comprising a total of 2031 participants across Ethiopia, Nigeria, Ghana, and South Africa (Table 1). In nine of the studies, burnout was assessed using the Maslach Burnout Inventory-Human Services Survey (MBI-HSS) [56, 57, 61, 66], MBI [55, 58, 60, 64], or an abbreviated MBI [59]. One study assessed burnout using the Copenhagen Burnout Inventory [63]. In South Africa, Schweitzer used one question (‘Do you ever feel so emotionally exhausted that you feel negative about yourself and about your job and lose the feeling of concern for your patients?’) to assess burnout based on the definition in Pine and Maslach [67]. Lastly in Nigeria, two questions were used to examine emotional exhaustion (‘I feel burned out from my work’) and depersonalization (‘I have become more callous toward people since I took this job’) [65].
Physicians reported high levels of burnout. For example, among physicians at rural district hospitals in South Africa (N = 36), 81% of participants reported burnout, with 31% reporting high burnout on all three of the MBI-HSS subscales [56]. On the MBI-HSS subscales, 65.2% of physicians in southern Ethiopia (N = 491) reported high emotional exhaustion, 91% low personal accomplishment, and 85.1% high depersonalization [57]. Physicians undergoing residency training at a hospital in Nigeria (N = 204) reported a high prevalence of burnout according to the MBI, in which 45.6% of residents reporting burnout on emotional exhaustion, 57.8% depersonalization, and 61.8% reduced personal accomplishment [58]. Among physicians who participated in the web-based survey in Ghana (N = 200), burnout measures were high on the emotional exhaustion (mean ± standard deviation (SD): 9.1 ± 2.6), personal accomplishment (5.8 ± 1.6), and depersonalization (5.2 ± 2.1) subscales of the abbreviated MBI [59]. South African physicians in public sector emergency centers (N = 93) had high burnout scores on all subscales of the MBI-HSS [61]. Among physician anesthetists at a university hospital in South Africa, 45.2% reported high emotional exhaustion, 50% reported high depersonalization, and 46% reported low personal accomplishment on the MBI-HSS [66]. Among South African anesthetists in private practice, 20.9% reported high emotional exhaustion, 26.7% reported high depersonalization, and 37.2% reported low personal accomplishment on the MBI-HSS [66]. In a population of junior physicians in South Africa (N = 126), 77.8% had experienced burnout, with 52.4% experiencing burnout at their current job. Among these doctors, scores on the Physician Stress Inventory were significantly higher among those with burnout (p < 0.001) [62]. Lastly, in a small mixed-methods study of junior physicians at a children’s hospital in South Africa (N = 22), all participants experienced high levels of burnout on at least 1 MBI subscale, and mean scores on the emotional exhaustion and depersonalization subscales were significantly higher than those in a normative comparison group (p < 0.001) [64].
Burnout among nurses
A total of 26 articles examined burnout among nurses in Ghana, South Africa, Nigeria, Kenya, Tanzania, Uganda, Cameroon, Namibia, and Zimbabwe (Table 2). The majority of studies were conducted in South African (N = 13) or Nigerian (N = 8) nursing populations. Of the 26 articles, a total of 20 studies used the Maslach Burnout Inventory-General Survey (MBI-GS), MBI-HSS, MBI, or the MBI emotional exhaustion subscale to measure burnout. Two studies used the Oldenburg Burnout Inventory [74, 85], one study used the burnout subscale of the ProQOL [83], and one study used first-hand coding by an observer according to the Exhaustion-Disengagement Model [84], which uses job demand and resources to identify exhaustion and disengagement. One study used the Executive Burnout Scale, which was developed in Nigeria as a culturally-sensitive tool to measure burnout [68, 95]. One study did not specify the burnout measure used [73]. A total of 5 studies did not report measured burnout levels in the study population [79, 84, 86, 89, 94].
High levels of reported burnout were found in nursing populations (Table 2). For example, in a large study of nurses at national referral hospitals in South Africa (N = 1187), 45.8% participants reported high levels of burnout on the emotional exhaustion subscale of the MBI [71]. Among hospital nurses in Nigeria (N = 270), 39.1% had burnout on the emotional exhaustion subscale of the MBI, 29.2% on the depersonalization subscale, and 40.0% on the reduced personal accomplishment subscale [81]. In a population of nurses at private and public hospitals in Kenya, Tanzania, and Uganda, (N = 309), 32.1% reported burnout on the MBI [91]. Among nursing populations in South Africa, burnout was associated with high workloads [73, 76, 82, 89] and lack of support [79, 80, 91, 92].
Burnout among combined populations of healthcare workers
A total of 18 articles examined burnout among combined populations of healthcare workers (Table 3). Three studies each were conducted in Ethiopia and Malawi. Two studies each were conducted in Nigeria, Ghana, Zambia, South Africa, and Kenya. One study each was conducted in Botswana and Mozambique. A total of 12 studies used the MBI, MBI-GS, or MBI-HSS to assess burnout [96, 99,100,101, 104,105,106, 108,109,110,111,112]. For example, in a small sample of healthcare workers in a trauma unit in South Africa (N = 38), 61% had high emotional exhaustion, 50% high depersonalization, and 50% reduced personal accomplishment on MBI subscales [99]. Among healthcare workers providing clinical care for HIV-positive patients in Malawi (N = 520), 62% met the MBI criteria for burnout [101]. Additionally, one study used the Compassion Fatigue Self Test [102] and one used the Copenhagen Burnout Inventory [97]. Two studies measured burnout as a sub-domain of motivation [98, 113]. One study measured burnout using a five item scale of occupational burnout [103]. Mutale and colleagues used two questions to measure burnout (“I feel emotionally drained at the end of the day” and “Sometimes when I get up in the morning, I dread having to face another day at work”) [107]. In combined populations of healthcare workers, nurses often had the highest level of reported burnout [97, 111].
Burnout among midwives
Two studies examined burnout among midwives in Uganda [114] and Senegal [115] (Table 4). Among midwives in two rural districts in Uganda (N = 224), burnout was measured using the burnout subscale of the Professional Quality of Life Scale [114]. Burnout and secondary traumatic stress were associated with level of education (p < 0.01), marital status (p < 0.01), involvement in non-midwifery health care activities (p < 0.01), and physical well-being (p < 0.01) [114]. Among midwives from 22 hospitals in Senegal (N = 226), 55% reported burnout on the MBI, with 80% reporting burnout on emotional exhaustion, 57.8% on depersonalization, and 12.4% on diminished personal accomplishment subscales. Furthermore, emotional exhaustion was inversely associated with remuneration (p = 0.02) and task satisfaction (p = 0.03). Active job searching was associated with being dissatisfied with job security (p < 0.01), and voluntary quitting was associated with dissatisfaction with continuing education (p < 0.01) [115].
Burnout among health professional students
Lastly, 7 articles examined burnout among medical and nursing students in South Africa or Cameroon (Table 4). Among medical students in South Africa (N = 91), 46.1% reported high, 33.8% moderate, and 20% low burnout on the MBI-HSS burnout scale [116]. Colby and co-authors also found significant associations between scores on the World Health Organization Quality of Life Assessment and the MBI subscales (p < 0.01) [116]. Among oral hygiene students in South Africa, there were significant differences in burnout levels on the MBI subscales between 1st, 2nd, and 3rd year students (p = 0.039) [117]. Among nursing students in South Africa (N = 80), 63.8% had a moderate to high risk of burnout [118]. In a population of undergraduate nursing students in South Africa (N = 67), Mathias and coauthors found on the burnout subscale of the Professional Quality of Life Scale (ProQOL) that 6% of participants had low levels of burnout, 94% had moderate, and none reported high levels of burnout [119]. Among nursing students (N = 447) and medical students (N = 413) in Cameroon, burnout was examined using the Oldenburg Burnout Inventory [120, 121]. Lastly, in a population of paramedic students in South Africa (N = 93), 31% of participants reported high levels of burnout on the Copenhagen Burnout Inventory [122].
Risk and protective factors associated with burnout among healthcare providers
Overall, burnout was associated with measures of the work environment, including heavy workload, inadequate personnel, difficult work conditions, and low career satisfaction. For example, nurses in South Africa with more favorable work environments were less likely to report high levels of burnout (OR = 0.55; 95% CI: 0.41–0.75) [71]. Heavy workloads were also significantly associated with high levels of reported burnout in populations of nurses [76, 82, 89, 91, 123] and other healthcare workers [108, 109]. Among nurses in South Africa, workload was a significant predictor of emotional exhaustion as measured by the MBI (β = 0.547,p = < 0.001) [76]. Among hospital workers in Nigeria, inadequate number of nursing personnel (OR = 2.6, 95% CI: 1.5–5.1), and frequent night duties (OR = 3.1, 95% CI: 1.7–5.6) were predictors of burnout on the emotional exhaustion subscale of the MBI. Frequent night duties (OR = 2.4, 95% CI: 1.5–4.8) were predictors of burnout on the depersonalization subscale. High nursing hierarchy (OR = 2.7, 95% CI: 1.5–4.8), poor wages (OR = 2.9, 95% CI: 1.6–5.6), and frequent night duties (OR = 2.3, 95% CI: 2.3–4.5) were predictors of burnout on the reduced personal accomplishment subscale of the MBI [81].
Patient care was also affected by high rates of burnout among healthcare providers [79, 80, 101]. For example, among healthcare providers in Malawi, burnout was associated with self-reported suboptimal patient care (OR = 3.22, 95% CI: 2.11–4.90; p < 0.0001). Additional factors in the work environment associated with burnout include nursing hierarchy and poor wages [81], staffing issues [79], difficulty communicating with patients [62], organizational complaints [89], job insecurity [97], and intention to quit [88].
Among healthcare providers, burnout is also associated with interpersonal and professional conflicts. Burnout is associated with high level of doctor/doctor conflict [58], doctor/nurse conflict [81], work/family conflict [69], and interpersonal conflict in general [89]. Among doctors in Nigeria (N = 204), those who did not report doctor/doctor conflict were less likely to have burnout on the depersonalization subscale of the MBI (OR = 0.36; 95% CI = 0.17–0.76) [58]. Among nurses in Nigeria (N = 270), doctor/nurse conflict was a predictor of burnout on the MBI emotional exhaustion subscale (OR = 3.1, 95% CI: 1.9–6.3) and on the depersonalization subscale (OR = 3.4, 95% CI: 2.2–7.6) [81]. Among nurses from public hospitals in Ghana (N = 134), work-to-family and family-to-work conflict accounted for 20% of the variance in burnout [69].
Experiences of stress and emotional distress were associated with increased odds of burnout. Among junior physicians in South Africa (N = 126), the Physician Stress Inventory (PSI) score was significantly higher among participants with burnout (p < 0.001) [62]. Physicians undergoing residency training in Nigeria who reported emotional distress were more likely to report burnout (p < 0.001) [58]. In a population of nurses in South Africa (N = 122), emotional management and emotional control, as measured by the Swinburne University Emotional Intelligence test, were associated with self-reported stress and burnout subscales (p < 0.01). Emotional intelligence was a moderator of the relationship between stress and burnout, explaining 59.5% of the variance in the emotional exhaustion and 23.9% of the variance in the depersonalization subscale of burnout [76]. Among nurses at a hospital in Nigeria, use of emotion-focused coping strategies was positively associated with the MBI burnout subscales of emotional exhaustion (β = 0.32, p = 0.01) and depersonalization (β = 0.18, p = 0.01) [86].
Lastly, social support was found to be protective against burnout among healthcare providers [58, 79, 80, 91, 97]. Specifically, among physicians in Nigeria, adequate support from management (OR = 0.45; 95% CI:0.22–0.90) were protective from burnout on the MBI subscale of reduced personal accomplishment [59]. Among nurses in Kenya, Tanzania, and Uganda (N = 309), lower social support from colleagues was associated with increased burnout on the MBI subscale of higher emotional exhaustion (β = − 0.15, p < 0.05) [91].
Burnout intervention programs
Programs aimed at coping with burnout are sparse. Only two studies, in combined populations of healthcare workers, examined burnout-related interventions [104, 105]. The Support, Train and Empower Managers (STEM) study was designed to implement a support intervention and measure the impact on healthcare workers in Mozambique [105]. At baseline, 67.1% of healthcare workers reported low, 15.9% moderate, and 17.1% high burnout on the MBI. After the intervention, 71.1% reported low, 17.8% moderate, and 11.1% high burnout. However, the authors found no statistically significant differences in emotional exhaustion from baseline to post-intervention for any intervention groups. Job satisfaction, emotional exhaustion and work engagement also showed no significant differences between baseline and post-intervention [105]. Ledikwe and colleagues examined healthcare workers at a public health facility in Botswana (N = 1348) after participation in Botswana’s Workplace Wellness Program (WWP) [104]. Job satisfaction, assessed by the Job In General Scale, was significantly higher for healthcare workers who participated in 7 or more activities in the WWP compared to those who did not participate in any activities (p = 0.004). Healthcare workers who participated in seven or more WWP activities had significantly higher scores on the Job Descriptive Index subscales related to satisfaction with work, supervision, promotion opportunities and pay, with the highest levels found among those participating in seven or more WWP activities (p < 0.05). Additionally, stress levels (p = 0.006), measured on the Stress in General scale, and exhaustion (p < 0.001), measured on the MBI, were significantly lower among those with high participation in WWP activities [104].
Discussion
Burnout is common among physicians, nurses, and other healthcare providers in sub-Saharan Africa with prevalence estimates ranging from 40 to 80%. Our findings can be compared to other systematic reviews of burnout among healthcare providers. Among physicians in China (N = 9302 participants from 11 studies), burnout prevalence ranged from 66.5–87.8% [39]. Among healthcare providers in Arab countries (N = 4108 from 19 studies), high burnout prevalence was estimated in the MBI subscales of emotional exhaustion (20.0–81.0%), depersonalization (9.2–80.0%), and personal accomplishment (13.3–85.8%) [43]. In a recent review (N = 109,628 from 182 studies), 67% of physicians reported burnout [124]. Finally, high prevalence of burnout has been reported among emergency room (26%) [125] and pediatric nurses (21–39%) [126].
In sub-Saharan Africa, the highest levels of burnout were recorded among nurses, although all healthcare providers reported high levels of burnout. High levels of burnout were associated with unfavorable work conditions, high job demands, and low job satisfaction. Studies in sub-Saharan Africa support other studies among healthcare providers that have shown burnout is more common among women [43, 127, 128], those of younger age [129], and those with less support or resources to manage workloads [39, 82, 130,131,132].
Limitations of current studies
The majority of studies assessed burnout using the MBI. Among those that used the MBI, burnout scores were variously reported as (1) percentage of participants with high burnout on each subscale [58, 72, 81, 87, 99, 106, 116], (2) percentage of participants with high burnout on each subscale and total score [55, 66, 101] (3) percentage of participants with high total burnout [91, 105], (4) percentage of participants with high burnout on emotional exhaustion subscale only [71], (5) total and individual burnout as a continuous scores [59], (6) total burnout as continuous score [69, 78, 110], (7) individual burnout as continuous score [60, 64, 70, 73, 75, 76, 82, 88, 90, 104, 108, 109, 112, 115, 117], or (8) both individual burnout as continuous sores and percentages of participants with high burnout [56, 57, 61, 77, 96]. Furthermore, included studies used four different versions of the MBI to assess burnout including the MBI, MBI-HSS, Abbreviated MBI, and MBI-GS. This introduced difficulty in directly comparing burnout rates between different populations of healthcare providers. Concerns have been raised about how the MBI operationalizes burnout [133]. Despite evidence documenting increasing burnout in sub-Saharan Africa, none of the studies reviewed discuss the conceptual definitions of burnout from a theoretical perspective. Most used the MBI and adopted the three domains of burnout from the MBI scale. Additionally, prior studies have not validated the MBI in healthcare workers in sub-Saharan Africa, and there may be different cultural interpretations of questions related to the construct of burnout. Although it’s difficult to quantitatively compare across populations due to variation in how burnout was defined, burnout prevalence reported using MBI subscales ranged from 12.5–65.2% on emotional exhaustion, 5–57.8% on depersonalization, and 25–85.1% on reduced personal accomplishment. On other instruments, burnout prevalence was 52.4% using one question (‘Do you ever feel so emotionally exhausted that you feel negative about yourself and about your job and lose the feeling of concern for your patients’) [62], 95.4% on the Compassion Fatigue Self-Test [102], 51% using an occupational burnout scale [103], and 63.75% using the ProQOL burnout subscale [118]. Given the variability that exists in assessing burnout in different contexts and with different instruments, there is a need to design studies aimed at evaluating the reliability of various burnout screening instruments cross-culturally.
There are additional limitations to the current studies. A total of 18 studies examined burnout among combined populations of healthcare workers in sub-Saharan Africa (Table 3). These populations include all workers in a clinic or hospital setting, who may have highly variable job responsibilities and workload. In addition, the majority of studies were cross-sectional. Only two studies examined burnout-related interventions in sub-Saharan African populations. Additionally, among the included studies, sample sizes were relatively small and study quality varied widely (Additional file 1: Table S3-S6).
Future studies need to address the drivers of burnout among healthcare providers in sub-Saharan Africa. Although burnout among healthcare providers has been associated with violence against healthcare providers [134, 135]; few studies have examined violence [99] and secondary traumatic stress [114] in sub-Saharan Africa. Performing longitudinal assessments of burnout along with measurements of mood, substance use, suicidality, cognition, performance and quality of life will add to our understanding of the burnout syndrome and its consequences. Efforts should also include utilizing consistent measures of burnout with an instrument validated in specific geographical and cultural contexts.
Conclusions
Burnout has received a great deal of attention in high-income countries with awareness and intervention programs designed to cope with burnout symptoms. In the United States, a recent report recommends addressing physician burnout by improving physician access to mental health services, improving the usability of electronic medical records, and appointing wellness officials to assess and improve burnout interventions at their institutions [136]. However, burnout among healthcare providers is not only a crisis in high-income countries [124]. It is a significant problem in low and middle income countries as well. Programs aimed at raising awareness, promoting well-being and prevention, and improving coping with burnout symptoms through evidence-based stress management and resilience training in sub-Saharan Africa are needed. Given the ever-increasing burden of major public health threats of communicable and non-communicable diseases in sub-Saharan Africa amidst a dearth of resources and lack of support, along with the adverse health effects of this burden for patients and providers alike, more attention needs to be paid to healthcare provider burnout in low-income settings in Africa and around the world. Additional studies need to address both personal and organizational barriers that increase the risk of burnout among healthcare providers [137]. Individual and structural interventions will need to be combined to effectively reduce burnout among healthcare providers [138]. These interventions should include advocacy for better resource provisions and support for healthcare providers so that healthcare infrastructure and patient care can be improved.
Availability of data and materials
Not applicable
Abbreviations
- CBI:
-
Copenhagen Burnout Inventory
- MBI:
-
Maslach Burnout Inventory
- MBI-GS:
-
Maslach Burnout Inventory - General Survey
- MBI-HSS:
-
Maslach Burnout Inventory - Human Services Survey
- PRISMA:
-
Preferred Reporting Items for Systematic Review and Meta-Analyses
- ProQOL:
-
Professional Quality of Life Scale
- STEM:
-
Support, Train and Empower Managers
- WWP:
-
Workplace Wellness Program
References
Maslach C, Jackson SE. The measurement of experienced burnout. J Occup Behav. 1981;2:99–113.
Lindblom K, Linton S, Fedeli C, Bryngelsson I. Burnout in the working population: relations to psychosocial work factors. Int J Behav Med. 2006;13(1):51–9.
Norlund S, Reuterwall C, Hoog J, Lindahl B, Janlert U, Birgander LS. Burnout, working conditions and gender--results from the northern Sweden MONICA study. BMC Public Health. 2010;10:326.
Bender A, Farvolden P. Depression and the workplace: a progress report. Curr Psychiatry Rep. 2008;10(1):73–9.
Morse G, Salyers MP, Rollins AL, Monroe-DeVita M, Pfahler C. Burnout in mental health services: a review of the problem and its remediation. Admin Pol Ment Health. 2012;39(5):341–52.
Gelsema T, Doef M, Maes S, Janssen M, Akerboom S, Verhoeven C. A longitudinal study of job stress in the nursing profession: causes and consequences. J Nurs Manag. 2006;14(4):289–99.
Shanafelt TD, Hasan O, Dyrbye LN, Sinsky C, Satele D, Sloan J, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–13.
Lamothe M, Boujut E, Zenasni F, Sultan S. To be or not to be empathic: the combined role of empathic concern and perspective taking in understanding burnout in general practice. BMC Fam Pract. 2014;15:15.
Aiken L, Clarke S, Sloane D, Sochalski J, Silber J. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–93.
Poncet MC, Toullic P, Papazian L, Kentish-Barnes N, Timsit JF, Pochard F, et al. Burnout syndrome in critical care nursing staff. Am J Respir Crit Care Med. 2007;175(7):698–704.
McHugh MD, Kutney-Lee A, Cimiotti JP, Sloane DM, Aiken LH. Nurses’ widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Aff (Millwood). 2011;30(2):202–10.
Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89(3):443–51.
Soler JK, Yaman H, Esteva M, Dobbs F, Asenova RS, Katic M, et al. Burnout in European family doctors: the EGPRN study. Fam Pract. 2008;25(4):245–65.
Wu S, Singh-Carlson S, Odell A, Reynolds G, Su Y. Compassion fatigue, burnout, and compassion satisfaction among oncology nurses in the United States and Canada. Oncol Nurs Forum. 2016;43(4):E161–9.
Sharma A, Sharp DM, Walker LG, Monson JR. Stress and burnout in colorectal and vascular surgical consultants working in the UK National Health Service. Psychooncology. 2008;17(6):570–6.
Landrigan CP, Fahrenkopf AM, Lewin D, Sharek PJ, Barger LK, Eisner M, et al. Effects of the accreditation council for graduate medical education duty hour limits on sleep, work hours, and safety. Pediatrics. 2008;122(2):250–8.
Maslach C, Leiter MP. Early predictors of job burnout and engagement. J Appl Psychol. 2008;93(3):498–512.
Eckleberry-Hunt J, Lick D, Boura J, Hunt R, Balasubramaniam M, Mulhem E, et al. An exploratory study of resident burnout and wellness. Acad Med. 2009;84(2):269–77.
Rath KS, Huffman LB, Phillips GS, Carpenter KM, Fowler JM. Burnout and associated factors among members of the Society of Gynecologic Oncology. Am J Obstet Gynecol. 2015;213(6):824 e1–9.
de Oliveira GS Jr, Chang R, Fitzgerald PC, Almeida MD, Castro-Alves LS, Ahmad S, et al. The prevalence of burnout and depression and their association with adherence to safety and practice standards: a survey of United States anesthesiology trainees. Anesth Analg. 2013;117(1):182–93.
Papathanasiou IV, Tsaras K, Kleisiaris CF, Fradelos EC, Tsaloglidou A, Damigos D. Anxiety and depression in staff of mental units: the role of burnout. Adv Exp Med Biol. 2017;987:185–97.
Jackson ER, Shanafelt TD, Hasan O, Satele DV, Dyrbye LN. Burnout and alcohol abuse/dependence among U.S. medical students. Acad Med. 2016;91(9):1251–6.
van der Heijden F, Dillingh G, Bakker A, Prins J. Suicidal thoughts among medical residents with burnout. Arch Suicide Res. 2008;12(4):344–6.
Penz M, Stalder T, Miller R, Ludwig VM, Kanthak MK, Kirschbaum C. Hair cortisol as a biological marker for burnout symptomatology. Psychoneuroendocrinology. 2018;87:218–21.
Oosterholt BG, Maes JH, Van der Linden D, Verbraak MJ, Kompier MA. Burnout and cortisol: evidence for a lower cortisol awakening response in both clinical and non-clinical burnout. J Psychosom Res. 2015;78(5):445–51.
Fernandez-Sanchez JC, Perez-Marmol JM, Blasquez A, Santos-Ruiz AM, Peralta-Ramirez MI. Association between burnout and cortisol secretion, perceived stress, and psychopathology in palliative care unit health professionals. Palliat Support Care. 2018;16(3):286–97.
Grossi G, Perski A, Evengård B, Blomkvist V, Orth-Gomér K. Physiological correlates of burnout among women. J Psychosom Res. 2003;55(4):309–16.
Toker S, Shirom A, Shapira I, Berliner S, Melamed S. The association between burnout, depression, anxiety, and inflammation biomarkers: C-reactive protein and fibrinogen in men and women. J Occup Health Psychol. 2005;10(4):344–62.
Juster RP, Sindi S, Marin MF, Perna A, Hashemi A, Pruessner JC, et al. A clinical allostatic load index is associated with burnout symptoms and hypocortisolemic profiles in healthy workers. Psychoneuroendocrinology. 2011;36(6):797–805.
Hintsa T, Elovainio M, Jokela M, Ahola K, Virtanen M, Pirkola S. Is there an independent association between burnout and increased allostatic load? Testing the contribution of psychological distress and depression. J Health Psychol. 2016;21(8):1576–86.
Blix E, Perski A, Berglund H, Savic I. Long-term occupational stress is associated with regional reductions in brain tissue volumes. PLoS One. 2013;8(6):e64065.
Golkar A, Johansson E, Kasahara M, Osika W, Perski A, Savic I. The influence of work-related chronic stress on the regulation of emotion and on functional connectivity in the brain. PLoS One. 2014;9(9):e104550.
Savic I. Structural changes of the brain in relation to occupational stress. Cereb Cortex. 2015;25(6):1554–64.
Williams ES, Konrad TR, Scheckler WE, Pathman DE, Linzer M, McMurray JE, et al. Understanding Physicians’ intentions to withdraw from practice: the role of job satisfaction, job stress, mental and physical health. Health Care Manag Rev. 2001;26(1):7–19.
Wallace J, Lemaire J, Ghali W. Physician wellness: a missing quality indicator. Lancet. 2009;374(9702):1714–21.
Shanafelt TD, Mungo M, Schmitgen J, Storz KA, Reeves D, Hayes SN, et al. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc. 2016;91(4):422–31.
Salyers MP, Bonfils KA, Luther L, Firmin RL, White DA, Adams EL, et al. The relationship between professional burnout and quality and safety in healthcare: a meta-analysis. J Gen Intern Med. 2017;32(4):475–82.
Dugani S, Afari H, Hirschhorn LR, Ratcliffe H, Veillard J, Martin G, et al. Prevalence and factors associated with burnout among frontline primary health care providers in low- and middle-income countries: a systematic review. Gates Open Res. 2018;2:4.
Lo D, Wu F, Chan M, Chu R, Li D. A systematic review of burnout among doctors in China: a cultural perspective. Asia Pac Fam Med. 2018;17:3.
Li H, Cheng B, Zhu X. Quantification of burnout in emergency nurses: a systematic review and meta-analysis. Int Emerg Nurs. 2018;39:46–54.
Cubero DI, Fumis RR, de Sa TH, Dettino A, Costa FO, Van Eyll BM, et al. Burnout in medical oncology fellows: a prospective multicenter cohort study in Brazilian institutions. J Cancer Educ. 2016;31(3):582–7.
Abdo SA, El-Sallamy RM, El-Sherbiny AA, Kabbash IA. Burnout among physicians and nursing staff working in the emergency hospital of Tanta University, Egypt. East Mediterr Health J. 2016;21(12):906–15.
Elbarazi I, Loney T, Yousef S, Elias A. Prevalence of and factors associated with burnout among health care professionals in Arab countries: a systematic review. BMC Health Serv Res. 2017;17(1):491.
Stilwell B, Diallo K, Zurn P, Vujicic M, Adams O, Poz MD. Migration of health-care workers from developing countries: strategic approaches to its management. Bull World Health Organ. 2004;2004(82):8.
Naicker S, Plange-Rhule J, Tutt R, Eastwood J. Shortage of healthcare workers in developing countries--Africa. Ethn Dis. 2009;19(1 Supp 1):S1–60–4.
Duvivier RJ, Burch VC, Boulet JR. A comparison of physician emigration from Africa to the United States of America between 2005 and 2015. Hum Resour Health. 2017;15(1):41.
Kasper J, Bajunirwe F. Brain drain in sub-Saharan Africa: contributing factors, potential remedies and the role of academic medical centres. Arch Dis Child. 2012;97(11):973–9.
Castro-Palaganas E, Spitzer DL, Kabamalan MM, Sanchez MC, Caricativo R, Runnels V, et al. An examination of the causes, consequences, and policy responses to the migration of highly trained health personnel from the Philippines: the high cost of living/leaving-a mixed method study. Hum Resour Health. 2017;15(1):25.
Walton-Roberts M, Runnels V, Rajan SI, Sood A, Nair S, Thomas P, et al. Causes, consequences, and policy responses to the migration of health workers: key findings from India. Hum Resour Health. 2017;15(1):28.
Rice K, Webster F. Care interrupted: poverty, in-migration, and primary care in rural resource towns. Soc Sci Med. 2017;191:77–83.
Moher D, Liberati A, Tetzlaff J, Altman D, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41.
Herzog R, Alvarez-Pasquin M, Diaz C, Barrio JD, Estrada J, Gil A. Are healthcare workers’ intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health. 2013;13:154.
Wells G, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality if nonrandomised studies in meta-analyses. Ottawa: Ottawa Health Research Institute; 1999. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. cited 2015 Acessed 12 Nov 2015
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Coker AO, Omoluabi PF. Burnout and stress reaction among psychiatrist working in Lagos, Nigeria. IFE PsychologIA. 2010;18(1):1–7.
Liebenberg A, Coetzee J, Conradie H, Coetzee J. Burnout among rural hospital doctors in the Western cape: comparison with previous south African studies. Afr J Prim Health Care Fam Med. 2018;10(1):e1–7.
Lrago T, Asefa F, Yitbarek K. Physicians’ burnout and factors in southern Ethiopia affecting it. Ethiop J Health Sci. 2018;28(5):589–98.
Ogundipe OA, Olagunju AT, Lasebikan VO, Coker AO. Burnout among doctors in residency training in a tertiary hospital. Asian J Psychiatr. 2014;10:27–32.
Opoku ST, Apenteng BA. Career satisfaction and burnout among Ghanaian physicians. Int Health. 2014;6(1):54–61.
Peltzer K, Mashego TA, Mabeba M. Occupational stress and burnout among south African medical practitioners. Stress Health. 2003;19(5):275–80.
Rajan S, Engelbrecht A. A cross-sectional survey of burnout amongst doctors in a cohort of public sector emergency centres in Gauteng, South Africa. Afr J Emerg Med. 2018;8(3):95–9.
Schweitzer B. Stress and burnout in junior doctors. S Afr Med J. 1994;84(6):352–4.
Stassen W, Van Nugteren B, Stein C. Burnout among advanced life support paramedics in Johannesburg, South Africa. Emerg Med J. 2013;30(4):331–4.
Stodel J, Stewart-Smith A. The influence of burnout on skills retention of junior doctors at red cross war memorial Children’s hospital: a case study. S Afr Med J. 2011;101(2):115–8.
Ugwu FO, Ugwu C, Njemanze VC, Nwosu I. Family cohesion and family size moderating burnout and recovery connection. Occup Med (Lond). 2019;69(1):28–34.
van der Walt N, Scribante J, Perrie H. Burnout among anaesthetists in South Africa. S Afr J Anaesth Analg. 2015;21(6):169–72.
Pines A, Maslach C. Characteristics of staff burnout in mental health settings. Hosp Community Psychiatry. 1978;29(4):233–7.
Amoo G, Fatoye FO. Burnout in South-Western Nigeria: a preliminary report among nurses and teachers. IFE PsychologIA. 2008;16(2):178–87.
Asiedu EEA, Annor F, Amponsah-Tawiah K, Dartey-Baah K. Juggling family and professional caring: role demands, work-family conflict and burnout among registered nurses in Ghana. Nurs Open. 2018;5(4):611–20.
Buitendach JH, Moola MA. Coping, occupational wellbeing and job satisfaction of nurses. J Psychol Afr. 2011;21(1):43–52.
Coetzee SK, Klopper HC, Ellis SM, Aiken LH. A tale of two systems--nurses practice environment, well being, perceived quality of care and patient safety in private and public hospitals in South Africa: a questionnaire survey. Int J Nurs Stud. 2013;50(2):162–73.
Davhana-Maselesele M, Igumbor J. The impact of caring for persons living with HIV and AIDS on the mental health of nurses in the Limpopo Province. Curationis. 2008;31(2):67–73.
Engelbrecht MC, Bester CL, van den Berg H, van Rensburg HCJ. A study of predictors and levels of burnout: the case of professional nurses in primary health care facilities in the free state. S Afr J Econ. 2008;76:S15–27.
Ezenwaji IO, Eseadi C, Okide CC, Nwosu NC, Ugwoke SC, Ololo KO, et al. Work-related stress, burnout, and related sociodemographic factors among nurses: implications for administrators, research, and policy. Medicine (Baltimore). 2019;98(3):e13889.
Gandi JC, Beben WW, Gyarazama Y. Nurse’s roles and the mediating effects of stress on job performance in low and developing economies. Psychology. 2011;2(4):323–30.
Gorgens-Ekermans G, Brand T. Emotional intelligence as a moderator in the stress-burnout relationship: a questionnaire study on nurses. J Clin Nurs. 2012;21(15–16):2275–85.
Heyns PM, Venter JH, Esterhuyse KG, Bam RH, Odendaal DC. Nurses caring for patients with Alzheimer’s disease: their strengths and risk of burnout. S Afr J Psychol. 2003;33(2):80–5.
Ifeagwazi CM. The influence of marital status on self-report of symptoms of psychological burnout among nurses. Omega J Death Dying. 2005;52(4):359–73.
Khamisa N, Oldenburg B, Peltzer K, Ilic D. Work related stress, burnout, job satisfaction and general health of nurses. Int J Environ Res Public Health. 2015;12(1):652–66.
Khamisa N, Peltzer K, Ilic D, Oldenburg B. Work related stress, burnout, job satisfaction and general health of nurses: a follow-up study. Int J Nurs Pract. 2016;22(6):538–45.
Lasebikan VO, Oyetunde MO. Burnout among nurses in a Nigerian general hospital: prevalence and associated factors. ISRN Nurs. 2012;2012:402157.
Levert T, Lucas M, Ortlepp K. Burnout in psychiatric nurses: contributions of the work environment and a sense of coherence. S Afr J Psychol. 2000;30(2):36–43.
Mashego TAB, Nesengani DS, Ntuli T, Wyatt G. Burnout, compassion fatigue and compassion satisfaction among nurses in the context of maternal and perinatal deaths. J Psychol Afr. 2016;26(5):469–72.
Mbambo S, Uys L, Groenewald B. A job analysis of selected health workers in a district health system in KwaZulu-Natal. Part two: job analysis of nurses in primary health care settings. Curationis. 2003;26(3):42–52.
Mbanga C, Makebe H, Tim D, Fonkou S, Toukam L, Njim T. Determinants of burnout syndrome among nurses in Cameroon. BMC Res Notes. 2018;11(1):893.
Mefoh PC, Ude EN, Chukwuorji JC. Age and burnout syndrome in nursing professionals: moderating role of emotion-focused coping. Psychol Health Med. 2019;24(1):101–7.
Okwaraji FE, Aguwa EN. Burnout and psychological distress among nurses in a Nigerian tertiary health institution. Afr Health Sci. 2014;14(1):237–45.
Pienaar JW, Bester CL. The impact of burnout on the intention to quit among professional nurses in the Free State region—a national crisis? S Afr J Psychol. 2011;41(1):113–22.
Roomaney R, Steenkamp J, Kagee A. Predictors of burnout among HIV nurses in the Western cape. Curationis. 2017;40(1):e1–9.
van der Colff JJ, Rothmann S. Burnout of registered nurses in South Africa. J Nurs Manag. 2014;22(5):630–42.
van der Doef M, Mbazzi FB, Verhoeven C. Job conditions, job satisfaction, somatic complaints and burnout among east African nurses. J Clin Nurs. 2012;21(11–12):1763–75.
van Doorn Y, van Ruysseveldt J, van Dam K, Mistiaen W, Nikolova I. Understanding well-being and learning of Nigerian nurses: a job demand control support model approach. J Nurs Manag. 2016;24(7):915–22.
van Wijk C. Factors influencing burnout and job stress among military nurses. Mil Med. 1997;162(10):707–10.
Wilson D, Chiwakata L. Locus of control and burnout among nurses in Zimbabwe. Psychol Rep. 1989;65(2):426.
Olley B. The executive burnout scale: construction and validation. Niger J Clin Couns Psychol. 1998;4:149–58.
Bhagavathula AS, Abegaz TM, Belachew SA, Gebreyohannes EA, Gebresillassie BM, Chattu VK. Prevalence of burnout syndrome among health-care professionals working at Gondar University Hospital, Ethiopia. J Educ Health Promot. 2018;7:145.
Biksegn A, Kenfe T, Matiwos S, Eshetu G. Burnout status at work among health care professionals in a tertiary hospital. Ethiop J Health Sci. 2016;26(2):101–8.
Bonenberger M, Aikins M, Akweongo P, Wyss K. The effects of health worker motivation and job satisfaction on turnover intention in Ghana: a cross-sectional study. Hum Resour Health. 2014;12(43):1–12.
Crabbe JM, Bowley DM, Boffard KD, Alexander DA, Klein S. Are health professionals getting caught in the crossfire? The personal implications of caring for trauma victims. Emerg Med J. 2004;21(5):568–72.
Fiadzo E, Golembiewski R, Luo H, Bradbury M, Rivera T. Burnout in Ghanaian hospitals: phase model findings in sub-Saharan Africa. J Health Hum Serv Adm. 1997;19(4):442–66.
Kim MH, Mazenga AC, Simon K, Yu X, Ahmed S, Nyasulu P, et al. Burnout and self-reported suboptimal patient care amongst health care workers providing HIV care in Malawi. PLoS One. 2018;13(2):e0192983.
Kokonya DA, Mburu JM, Kathuku DM, Ndetei DM. Burnout syndrome among medical workers at Kenyatta National Hospital (KNH), Nairobi, Kenya. Afr J Psychiatry. 2014;17(6):1–7.
Kruse GR, Chapula BT, Ikeda S, Nkhoma M, Quiterio N, Pankratz D, et al. Burnout and use of HIV services among health care workers in Lusaka District, Zambia: a cross-sectional study. Hum Resour Health. 2009;7:55.
Ledikwe JH, Kleinman NJ, Mpho M, Mothibedi H, Mawandia S, Semo BW, et al. Associations between healthcare worker participation in workplace wellness activities and job satisfaction, occupational stress and burnout: a cross-sectional study in Botswana. BMJ Open. 2018;8(3):e018492.
Madede T, Sidat M, McAuliffe E, Patricio SR, Uduma O, Galligan M, et al. The impact of a supportive supervision intervention on health workers in Niassa, Mozambique: a cluster-controlled trial. Hum Resour Health. 2017;15(1):58.
McAuliffe E, Bowie C, Manafa O, Maseko F, MacLachlan M, Hevey D, et al. Measuring and managing the work environment of the mid-level provider - the neglected human resource. Hum Resour Health. 2009;7:9.
Mutale W, Ayles H, Bond V, Mwanamwenge M, Balabanova D. Measuring health workers’ motivation in rural health facilities: baseline results from three study districts in Zambia. Hum Resour Health. 2013;11(8):1–8.
Ndetei D, Pizzo M, Maru H, Ongecha F, Khasakhala L, Mutiso V, et al. Burnout in staff working at the Mathari psychiatric hospital. Afr J Psychiatry (Johannesbg). 2008;11(3):199–203.
Nel JA, Jonker CS, Rabie T. Emotional intelligence and wellness among employees working in the nursing environment. J Psychol Afr. 2013;23(2):195–204.
Ojedokun O, Idemudia ES, Kute VO. Burnout and fear of contagion as factors in aggressive tendency of health-care workers treating people with Aids. Soc Behav Pers. 2013;41(10):1625–34.
Olley B. A comparative study of burnout syndrome among health professionals in a Nigerian teaching hospital. Afr J Med Med Sci. 2003;32(3):297–302.
Thorsen VC, Tharp AL, Meguid T. High rates of burnout among maternal health staff at a referral hospital in Malawi: a cross-sectional study. BMC Nurs. 2011;10:9.
Weldegebriel Z, Ejigu Y, Weldegebreal F, Woldie M. Motivation of health workers and associated factors in public hospitals of West Amhara, Northwest Ethiopia. Patient Prefer Adherence. 2016;10:159–69.
Muliira RS, Ssendikadiwa VB. Professional quality of life and associated factors among Ugandan midwives working in Mubende and Mityana rural districts. Matern Child Health J. 2016;20(3):567–76.
Rouleau D, Fournier P, Philibert A, Mbengue B, Dumont A. The effects of midwives’ job satisfaction on burnout, intention to quit and turnover: a longitudinal study in Senegal. Hum Resour Health. 2012;10(9):1–14.
Colby L, Mareka M, Pillay S, Sallie F, Staden C, Plessis E, et al. The association between the levels of burnout and quality of life among fourth-year medical students at the University of the Free State. S Afr J Psychiatry. 2018;24:1–6.
Gordon NA, Rayner CA, Wilson VJ, Crombie K, Shaikh AB, Yasin-Harnekar S. Perceived stressors of oral hygiene students in the dental environment. Afr J Health Prof Educ. 2016;8(1):20–4.
Mason HD, Nel JA. Compassion fatigue, burnout and compassion satisfaction: prevalence among nursing students. J Psychol Afr. 2012;22(3):451–6.
Mathias C, Wentzel D. Descriptive study of burnout, compassion fatigue and compassion satisfaction in undergraduate nursing students at a tertiary education institution in KwaZulu-Natal. Curationis. 2017;40(1):e1–6.
Njim T, Mbanga C, Mouemba D, Makebe H, Toukam L, Kika B, et al. Determinants of burnout syndrome among nursing students in Cameroon: cross-sectional study. BMC Res Notes. 2018;11(1):450.
Njim T, Makebe H, Toukam L, Kika B, Fonkou S, Fondungallah J, et al. Burnout syndrome amongst medical students in Cameroon: a cross-sectional analysis of the determinants in preclinical and clinical students. Psychiatry J. 2019;2019:4157574.
Stein C, Sibanda T. Burnout among paramedic students at a university in Johannesburg, South Africa. Afr J Health Prof Educ. 2016;8(2):193–5.
Engelbrecht M, van den Berg H, Bester C. Burnout and compassion fatigue: the case of professional nurses in primary health care facilities in the Free State Province, South Africa. In: Psychology of Burnout: Predictors and Coping Mechanisms: Psychology Research Progress. Hauppage: Nova Science Publishers; 2009. p. 1–38.
Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, et al. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320(11):1131–50.
Adriaenssens J, Gucht VD, Maes S. Determinants and prevalence of burnout in emergency nurses: a systematic review of 25 years of research. Int J Nurs Stud. 2015;52(2):649–61.
Pradas-Hernandez L, Ariza T, Gomez-Urquiza JL, Albendin-Garcia L, De la Fuente EI, Canadas-De la Fuente GA, et al. PLoS One. 2018;13(4):e0195039.
Rabatin J, Williams E, Baier Manwell L, Schwartz MD, Brown RL, Linzer M. Predictors and outcomes of burnout in primary care physicians. J Prim Care Community Health. 2016;7(1):41–3.
Shenoi AN, Kalyanaraman M, Pillai A, Raghava PS, Day S. Burnout and psychological distress among pediatric critical care physicians in the United States. Crit Care Med. 2018;46(1):116–22.
Levin K, Shanafelt T, Keran C, Busis N, Foster L, Molano J, et al. Burnout, career satisfaction, and well-being among US neurology residents and fellows in 2016. Neurology. 2017;89(5):492–501.
Busis N, Shanafelt T, Keran C, Levin K, Schwarz H, Molano J, et al. Burnout, career satisfaction, and well-being among US neurologists in 2016. Neurology. 2017;88(8):797–808.
Popa-Velea O, Diaconescu L, Mihailescu A, Jidveian Popescu M, Macarie G. Burnout and its relationships with alexithymia, stress, and social support among romanian medical students: a cross-sectional study. Int J Environ Res Public Health. 2017;14(6):1–10.
Woodhead EL, Northrop L, Edelstein B. Stress, social support, and burnout among long-term care nursing staff. J Appl Gerontol. 2016;35(1):84–105.
Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen burnout inventory: a new tool for the assessment of burnout. Work Stress. 2005;19(3):192–207.
Erdur B, Ergin A, Yuksel A, Turkcuer I, Ayrik C, Boz B. Assessment of the relation of violence and burnout among physicians working in the emergency departments in Turkey. Ulus Travma Acil Cerrahi Derg. 2015;21(3):175–81.
Yoon H, Sok S. Experiences of violence, burnout and job satisfaction in Korean nurses in the emergency medical Centre setting. Int J Nurs Pract. 2016;22(6):596–604.
Jha AK, Iliff AR, Chaoui AA, Defossez S, Bombaugh MC, MIller YR. A crisis in healthcare: a call to action on physician burnout. Boston: Massachuetts Medical Society; 2019.
Dyrbye LN, Shanafelt TD, Sinsky CA, Cipriano PF, Bhatt J, Ommaya A, West CP, Meyers D. Burnout among health care professionals: A call to explore and address this underrecognized threat to safe, high-quality care. NAM Perspect. 2017:1–11.
West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272–81.
Acknowledgments
Not applicable.
Funding
MLD was supported by K23AT009218 from the National Center for Complementary and Integrative Health at the National Institutes of Health (NIH). The NIH had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
BWD, ZC, GLF, and BG conceived and designed the review. LF and BG performed the literature search. BWD, LEF, ZC, JWD, DHM, AA, GLF, MLD, BG contributed to the writing and editing of the manuscript. BWD, LEF, ZC, JWD, DHM, AA, GLF, MLD, BG have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable
Competing interests
JWD has received research support for investigator-initiated studies from Onyx/Amgen and Basis/Intel. All other authors declare that they have no competing interests. MLD has received remuneration from Harvard Health Publishing.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Table S1. Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines. Table S2. Database terms of search. Table S3. Quality assessment of studies on burnout among physicians in sub-Saharan Africa (N = 12). Table S4. Quality assessment of studies on burnout among nurses in sub-Saharan Africa (N = 26). Table S5. Quality assessment on burnout among healthcare workers in sub-Saharan Africa (N = 18). Table S6. Quality assessment on burnout among midwives and health professional students in sub-Saharan Africa (N = 9). (DOCX 34 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Dubale, B.W., Friedman, L.E., Chemali, Z. et al. Systematic review of burnout among healthcare providers in sub-Saharan Africa. BMC Public Health 19, 1247 (2019). https://doi.org/10.1186/s12889-019-7566-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-019-7566-7