Abstract
Background
Understanding of malaria ecology is a prerequisite for designing locally adapted control strategies in resource-limited settings. The aim of this study was to utilize the spatial heterogeneity in malaria transmission for the designing of adaptive interventions.
Methods
Field collections of clinical malaria incidence, asymptomatic Plasmodium infection, and malaria vector data were conducted from 108 randomly selected clusters which covered different landscape settings including irrigated farming, seasonal flooding area, lowland dryland farming, and highlands in western Kenya. Spatial heterogeneity of malaria was analyzed and classified into different eco-epidemiological zones.
Results
There was strong heterogeneity and detected hot/cold spots in clinical malaria incidence, Plasmodium prevalence, and vector abundance. The study area was classified into four zones based on clinical malaria incidence, parasite prevalence, vector density, and altitude. The two irrigated zones have either the highest malaria incidence, parasite prevalence, or the highest malaria vector density; the highlands have the lowest vector density and parasite prevalence; and the dryland and flooding area have the average clinical malaria incidence, parasite prevalence and vector density. Different zones have different vector species, species compositions and predominant species. Both indoor and outdoor transmission may have contributed to the malaria transmission in the area. Anopheles gambiae sensu stricto (s.s.), Anopheles arabiensis, Anopheles funestus s.s., and Anopheles leesoni had similar human blood index and malaria parasite sporozoite rate.
Conclusion
The multi-transmission-indicator-based eco-epidemiological zone classifications will be helpful for making decisions on locally adapted malaria interventions.
Similar content being viewed by others
Background
Although it is preventable and treatable, malaria continues to be one of the greatest global public health threats, despite considerable progress made through intensive interventions in the past two decades [1]. According to the World Health Organization (WHO), in 2021 there were an estimated 247 million malaria cases in 84 malaria-endemic countries, with an estimated 619,000 deaths. About 95% of cases occurred in Africa [1]. In 2015, the WHO set the target of reducing global malaria incidence and mortality by at least 90% by 2030 [2], and many endemic African countries have set their milestones with the aim of eliminating malaria by 2030 [3,4,5,6]. However, controlling malaria requires effective strategies, and to achieve optimal cost-effectiveness the strategies must adapt to local eco-epidemiological settings [7, 8]. A better understanding of malaria biology/ecology is key to designing such intervention strategies [7,8,9].
Malaria is a mosquito-borne infectious tropical disease transmitted by bites from infected female Anopheles mosquitoes. Transmission spatial heterogeneity is one of the key epidemiological characteristics of vector-borne infectious diseases, including malaria, due to the heterogeneity of environments supporting vector development and reproduction and disease pathogen transmission [10,11,12,13]. In malaria studies, researchers have found that temperature/precipitation patterns, land use land cover, elevation, and landscape features such as valley shape, rivers, and slopes all affect the transmission and distribution of malaria vectors and Plasmodium parasite infections [14,15,16,17,18]. Many studies found that Plasmodium infections (both symptomatic and asymptomatic) showed aggregated patterns in certain areas (i.e., hotspots) and in many cases at the household or village level [11,12,13, 19, 20], suggesting the potential for focused interventions [10, 21,22,23]. However, targeted interventions produced mixed results [10, 21, 23]. The failure of hotspot-targeted interventions to accelerate malaria elimination is likely due to confounding factors and to the incomplete understanding of spatial transmission dynamics [20, 22, 24]. Geographical micro-variations in malaria transmission may be a universal feature [22, 25, 26]. Fine-scale, i.e., household- or village-level, risk factor analysis is useful for informing household-based intervention strategies, but it may not be suitable for regional- or national-level intervention planning and implementation [21, 22, 25, 27]. It is important to optimally utilize the spatial information collected to prioritize locally adapted interventions in resource-limited settings. The question is how to make use of household/village-level information for regional malaria control planning.
Malaria risk can be measured using several indicators, including asymptomatic Plasmodium infection prevalence, clinical malaria incidence, and vector density [21, 24, 28,29,30]. These indicators are also used for spatial heterogeneity and household/village-level risk assessments [11,12,13, 19, 31]. In addition to cluster/village-level heterogeneity analyses, a recent study shows that through in-depth analyses the same information can also potentially be used for regional intervention planning [32]. The selection of interventions is based on epidemiological status, but it should be adapted to the local ecological conditions that support the development and survival of malaria vectors. Previous study used Plasmodium infection prevalence, Anopheles adult density, and clinical malaria incidence from different seasons to classify study areas into different eco-epidemiological zones [32], which can potentially be used for intervention planning. However, previous study did not analyse the potential spatial heterogeneity of malaria transmission, and the study area was relatively small. An expanded study area including more diverse eco-epidemiological areas would enable researchers to draw generalized conclusions.
In this study, the study area was expanded to include areas with more diverse eco-epidemiological conditions. The spatial heterogeneity of transmission was examined based on epidemiological and entomological observations and conducted classification analyses to determine the eco-epidemiological zones. The eco-epidemiological zone classifications will be helpful for making decisions on locally adapted malaria interventions.
Methods
Study area
The study was conducted in 108 clusters in Muhoroni (top), Nyando (middle) and Nyakach (bottom) sub-counties of Kisumu County, western Kenya (Fig. 1). The study areas cover an area of about 1,440 km2 and a population of about 466,000. The climatic/environmental conditions and the definition of a cluster have been described in previous studies [32, 33]. The north end of the Muhoroni study area is a large sugarcane plantation, and the central western area borders rice paddies (Fig. 1). In the south, about half of the Nyakach study area is on the Lake Victoria shore plain with swamps (elevation 1,140–1,200 m), with a sloped transition area leading to a highland plateau (elevation 1,550–1,650 m) at the southern border of the study area (Fig. 1). Nyando lays in the centre of the Kano plain along the Lake Victoria shoreline. Nyando presents a contrast in agricultural practices between its western and eastern halves, with rice fields dominating the western side and dryland maize cultivation in the flooded (during the long-rainy season) plains of the eastern region (Fig. 1). Malaria transmission in the study area is perennial with an annual peak from May to July during the long rainy season [32, 33]. Malaria vectors are Anopheles funestus sensu lato (s.l.) and Anopheles arabiensis in the Muhoroni area and An. funestus, An. arabiensis and Anopheles gambiae sensu stricto (s.s.) in the Nyakach area [32,33,34]. Malaria vector species in Nyando area is not clear. Also present are Anopheles coustani, a potential malaria vector in Kenya, and Anopheles pharoensis [32,33,34,35].
Entomological survey
Cross-sectional indoor and outdoor mosquito surveys were conducted at all 108 clusters. Indoor-resting mosquitoes were collected using the pyrethrum spraying collection (PSC) method. Both indoor and outdoor host-seeking mosquitoes were collected using CDC light traps. In each cluster for each sampling method, 20–25 houses were randomly selected, and samplings were conducted monthly from May to September 2021. Location and altitude of sampling houses were determined using a handheld GPS. Mosquito species were identified morphologically, and female anopheline mosquitoes were classed as unfed, blood fed, half-gravid, and gravid. Specimens of An. gambiae s.l. and An. funestus s.l. were further analysed by rDNA-PCR for species identification. Mosquito density was calculated as the number of Anopheles females per house per night.
Asymptomatic parasite infection prevalence
Cross-sectional Plasmodium parasite infection surveys were conducted from May to September 2021. The details of the sample collections have been described in previous study [32]. Briefly, about 100–120 participants were randomly selected at each cluster. On signing of the informed consent/assent (for minors younger than 18 years) forms, blood samples were collected using the standard finger-prick method. Thin and thick blood smears were prepared for laboratory microscopy examination, and filter paper blood dots were prepared for PCR detection of parasite infection status and species. Parasite prevalence was calculated as the proportion of positive samples over total samples tested based on the PCR test results.
Active malaria case detection
Clinical malaria incidence was determined through active case detection (ACD) conducted at all clusters from April to September 2021. The details of ACD have been described in previous studies [30, 32]. Briefly, a cohort of 100–150 households, comprising about 500 residents, was selected randomly from each cluster, and all residents in the selected households were invited to participate in the study based on the inclusion and exclusion criteria. Written informed consent/assent (for minors younger than 18 years) for study participation was obtained from all consenting heads of households and from each individual who was willing to participate in the study. Participants were visited bi-weekly by a team of government trained and certified local Community Health Volunteers (CHVs) and screened for clinical malaria. Body temperature and symptoms and signs of illness were recorded on a case report form (CRF). For anybody who had malaria-like symptoms, a rapid diagnosis test (RDT) was administered on-spot. Clinical cases were referred to the nearest government-run hospital or health centre for free treatment. A clinical malaria case is defined as an individual with fever (axillary temperature of 37.5 °C or higher) and other related symptoms such as chills, severe malaise, headache, or vomiting at the time of examination or 1–2 days before the examination, together with a Plasmodium-positive RDT. The incidence rate was calculated as the number of cases per 1,000 people per year based on the RDT test results.
Data statistical analyses
Spatial heterogeneity of mosquito density, parasite prevalence and clinical malaria incidence was examined using the Getis-Ord Gi* statistic of the ArcGIS Hot Spot Analysis tool (ArcGIS Pro 3.0, ESRI Inc., Redlands, CA, USA) [36]. Trend surfaces of malaria incidence, parasite prevalence and malaria vector density were produced using the completely regularized spline smoothing method of radial basis kernel function of ArcGIS. The study clusters were then classified into different zones, using hierarchical clustering method, based on the combination of all risk factors measured, including mosquito density, parasite prevalence, clinical malaria incidence, and elevation. Analysis of variance (ANOVA) was used to assess differences in parasite prevalence (with arcsine transformation), clinical malaria incidence (with logarithmic transformation), and malaria vector density among different zones. The post hoc Tukey HSD test was used for pairwise tests. The χ2 test was used to test the differences in Anopheles mosquito species composition among different zones, and differences in sporozoite rate and bloodmeal sources between indoors and outdoors and between different vector species.
Results
Descriptive statistics
For the ACD surveillance, 10–12 rounds of home visits were carried out, 364,176 person-visits were conducted, and 1,862 RDT-positive malaria cases were detected, with an overall annual incidence rate of 122.7 cases/1,000 people (95% CI 121.6–123.8) (Table 1).
For the Plasmodium prevalence surveys, a total of 11,554 blood samples were collected and PCR was done on 9,184 samples (Table 1). PCR detected 2,686 infected samples, a prevalence of 29.2% (95% CI 28.3–30.1). Among the PCR-positive samples, 2,541 (94.6%) were Plasmodium falciparum, 26 (1.0%), Plasmodium malariae, 34 (1.3%), Plasmodium ovale, 15 (0.6%) mixed P. falciparum and P. ovale, and 60 (2.2%) mixed P. falciparum and P. malariae.
For the vector surveillance, a total of 5,173 trap-nights were sampled, and 12,600 Anopheles mosquitoes were captured (Table 1). Among the mosquitoes captured, 9,020 (72.6%) were morphologically identified as An. gambiae s.l., 2,218 (17.6%) An. funestus s.l., 825 (6.5%) An. coustani, 425 (3.4%) An. pharoensis, and 112 (0.9%) unidentified species. PCR analyses found that among An. gambiae s.l., 89.5% (759/848) were An. arabiensis and the rest were An. gambiae s.s.; among An. funestus s.l., 86.3% (761/882) were An. funestus s.s. and the rest were An. leesoni. A total of 46,050 Culex and 54 Aedes were collected.
Although there were significant time-lagged correlations between Anopheles densities and parasite prevalence and clinical malaria incidence (Additional file 1: Table S1), the overall pairwise correlations between the four malaria transmission indicators, parasite prevalence, clinical malaria incidence, vector density and elevation, were not very high, with the highest correlation of 0.41 between parasite prevalence and clinical malaria incidence (Additional file 1: Table S2).
Trend surface and hot spot analyses
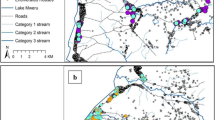
Trend surface analysis illustrated strong spatial heterogenous distribution of clinical malaria incidence (Fig. 2A), asymptomatic parasite prevalence (Fig. 2B), and malaria vector density (Fig. 2C). Clinical incidence was very high in the northwestern section of the study area, parasite prevalence was high across the northern part plus a few sparse clusters across the study area, while vector density was high across the northwestern part of the study area (Fig. 2A–C).
Both hot and cold spots were detected in the study areas (Fig. 2D–F). A small hotspot of clinical incidence was detected in the northwestern area (Fig. 2D). For parasite prevalence, a large hotspot was detected in the north and a large cold spot in the south (Fig. 2E). For vector density, cold spots were detected in the south similar to that of prevalence, while the locations of the hot spots were different from both clinical incidence and parasite prevalence (Fig. 2F). In general, at the top of the highland plateau there was low parasite prevalence, low malaria incidence and low vector density, while the northern area surrounded by the sugarcane plantation and rice fields had high parasite prevalence, high malaria incidence and high vector density (Fig. 2).
Malaria risk classification and characterization
The study areas could be classified into four zones based on parasite prevalence, clinical malaria incidence, malaria vector density, and elevation (Fig. 3). Parasite prevalence was significantly higher in the north (42.3 ± 2.0%) (Figs. 3, 4 Zone 4) compared to the other zones (11.8–17.5%) (Tukey HSD test, P < 0.05, Figs. 3, 4). The northern zone (Zone 4 on Fig. 3) had significantly higher clinical malaria incidence (290.3 ± 27.5 cases/1,000 people/year) and Zone 2 had significantly lower clinical malaria incidence (96.5 ± 7.2 cases/1,000 people/year) (Tukey HSD test, P < 0.05, Figs. 3, 4). Zone 1 had the highest malaria vector density (3.8 ± 0.9 females/house/night) and the highland (Zone 3) had the lowest vector density (0.4 ± 0.1 females/house/night) (Tukey HSD test, P < 0.05, Figs. 3, 4). Clearly, the highland zone had the highest elevation (1514 ± 22 m above sea level) compared to the other zones (1128–1193 m a.s.l.) (Tukey HSD test, P < 0.05, Figs. 3, 4).
From a malaria transmission and vector control point of view, malaria vector species composition is also an important parameter. An. gambiae s.l. was dominant in all lowland zones while An. funestus was dominant in the highlands (χ2 = 838.09, d.f. = 9, P < 0.0001, Fig. 5A). Female density varied significantly among zones for all species (ANOVA, P < 0.05 for all). Anopheles gambiae and An. funestus had significantly higher densities in Zone 1, and the density of An. funestus was also high in Zone 4 (highland), while An. coustani had the highest density in Zone 1 (Fig. 5B). Density of An. pharoensis was low in all zones (Fig. 5B).
For An. gambiae and An. funestus complexes, 3,291 females were randomly selected for PCR species identifications. A total of 2,660 females have been identified to species with 1,708 (64.2%) An. arabiensis, 116 (4.4%) An. gambiae s.s., 736 (27.7) An. funestus s.s., and 100 (3.8%) An. leesoni. The species compositions were significantly different between indoor and outdoor catches (χ2 = 14.75, d.f. = 4, P = 0.0052, Figs. 5C, D), as well as among different zones for indoor catches (χ2 = 120.60, d.f. = 12, P < 0.0001, Fig. 5C) and for outdoor catches (χ2 = 45.73, d.f. = 12, P < 0.0001, Fig. 5D).
Bloodmeal source and sporozoite infections
A total of 1,730 female mosquitoes were examined for bloodmeal source and sporozoite infections, of them 65 (3.8%) had sporozoite infections, 117 (6.8%) had bovine bloodmeals, 66 (3.8%) had human blood meals, and human bloodmeal index (HBI) was 0.36 (Table 2). Interestingly, sporozoite rate was significantly higher in mosquitoes collected outdoors (5.0%) compared to indoors (2.9%) (χ2 = 4.91, d.f. = 1, P = 0.0265, Table 2). Proportions of female mosquitoes having bovine bloodmeals was also significantly higher in mosquitoes collected outdoors (8.4%) compared to indoors (5.7%) (χ2 = 4.84, d.f. = 1, P = 0.0278, Table 2). Proportions of female mosquitoes having human bloodmeals was similar between mosquitoes collected outdoors (3.7%) and indoors (3.9%) (χ2 = 0.04, d.f. = 1, P = 0.8314, Table 2). Sporozoite infections have been detected from all four species of An. gambiae and An. funestus complexes, but sporozoite rates varied among species and between indoor and outdoor collected females, with the highest sporozoite rate of 9.1% for indoor collected An. leesoni and 0% for outdoor collected An. gambiae s.s. (χ2 = 3.48, d.f. = 1, P = 0.0622, Table 2). Due to the small number of sporozoite infected females, bloodmeal source and sporozoite infection were not analysed by zones. Bloodmeals and sporozoite infections in An. coustani and An. pharoensis were not examined.
Discussion
Malaria transmission heterogeneity is universal due to the nature of environmental heterogeneity. For maximum effectiveness, malaria interventions should be adapted to local eco-epidemiological conditions [7, 8, 37]. The question is how to best utilize the data on transmission heterogeneity to form the optimal strategy for malaria intervention planning. Many studies have analysed malaria transmission heterogeneity, especially micro-geographical transmission hotspots. Interventions targeting high-transmission areas have yielded mixed effectiveness [21, 23, 38]. Bousema et al. conducted interventions in hotspots and found that the impact on parasite prevalence of interventions targeting malaria vectors and human infections was modest, transient, and restricted to the targeted hotspot areas, suggesting that a community-wide approach may be more beneficial [21]. In an earlier study by Zhou et al. conducted in the highlands of western Kenya at a time when vector resistance to insecticides was low, they found that indoor residual spraying in the high-transmission area (i.e., area-wide targeted intervention) significantly reduced vector density and new Plasmodium infections in school-aged children across the community [23]. In the study by Zhou et al., the targeted area was not a simple small hotspot but an area where most breeding habitats and Plasmodium infections were located [29, 39, 40]; i.e., the selection of intervention strategy was based on the eco-epidemiological settings of the area [7, 8]. For malaria control decision makers, the important question is how to determine the different eco-epidemiological settings so that different adaptive intervention strategies can be formed. In this study, based on multiple malaria risk parameters, the study areas were classified into four eco-epidemiological conditions. Since the four zones have distinct malaria transmission characteristics, the four areas may need different intervention strategies. It should be noted that in most previous studies, detection of transmission hotspots was based on a single risk indicator, in many cases using one-time-point surveillance data [21, 24, 27,28,29]. This study used Plasmodium infection prevalence (all-age inclusive), clinical malaria incidence (six months/12 rounds of active case surveillance) and malaria vector density (six-month samplings). This comprehensive surveillance data may strengthen the reliability of the classification results.
Household- and village-level heterogeneity and risk analysis is important for informing household malaria prevention strategies. However, decision-makers need regional-level eco-epidemiological analysis to form the basis for malaria control planning. For example, in the highlands, malaria vector habitats and Plasmodium infections are usually concentrated in the valleys [29, 31, 39, 40]. At the top of the highland plateau, habitats are usually man-made water ponds and sparsely distributed [32]; in these areas, habitat management may be an effective strategy for malaria control [23, 41, 42]. On the other hand, in the rice-growing area, although larviciding has proven to be an effective vector control strategy [43], large-scale larviciding in rice fields can be costly in terms of larvicide usage and implementation costs if larvicides are applied in multiple rounds during the rice-growing season [44], making it a less cost-effective strategy. From this point of view, this study provides useful information for vector control planning; i.e., the four zones may need different vector and malaria management strategies. For example, in the high-prevalence and high-incidence zones, an effective strategy might be enhancing diagnosis and clinical treatment to reduce the parasite reservoir, supplemented by indoor spraying with the new formulation of insecticides such as pirimiphos-methyl Actellic® 300CS [35, 45, 46]. Cost-effectiveness should be considered when selecting any intervention strategy.
Malaria risk changes over time, and both malaria risk and intervention strategies may need to be reevaluated over time to adapt to the changed epidemiology [20, 22, 24]. For example, in western Kenya, supplementing LLINs with Actellic® IRS has significantly reduced the malaria burden in both Migori and Homa Bay counties [35, 45, 46]. However, malaria vector density is still high in Homa Bay irrigation sites [35], and thus malaria transmission potential is still high in the area. Vector mosquito species in Homa Bay have shifted from An. gambiae s.s., An. funestus and An. arabiensis to An. arabiensis alone after several years of the enhanced Actellic® IRS intervention [35, 45]. Since An. arabiensis is a predominantly zoophilic and exophilic species [47, 48] and IRS and LLINs work mainly indoors (although they may reduce overall mosquito density), different vector intervention strategies may be required to eliminate malaria transmission potential. Similarly, in the lake shore lowland and highland plateau parts of the study area, Actellic® IRS and piperonyl butoxide LLINs (PBO-LLINs) were implemented in the study clusters in 2020 [49]. Compared with the 2019 data from the previous study [32], malaria burden and transmission have significantly reduced, indicating the effectiveness of both PBO-LLIN and LLIN + IRS interventions. Cost-effectiveness should be analysed to determine the optimal interventions.
The higher proportion of bovine (compared to human) bloodmeals and higher sporozoite infection rate from outdoor (compared to indoor) collected female mosquitoes highlighted the importance of outdoor residual transmission of malaria in western Kenya. An. arabiensis is an opportunistic blood sucker and rests both indoors and outdoors [50]. Studies conducted in the same area in the 1990s found that both An. gambiae s.s. and An. funestus generally fed indoors on humans preferably and rests indoors [50,51,52,53]. However, after the universal coverage of LLINs started since mid-2000s, there are amounting reports on outdoor host seeking and resting of An. gambiae s.s. and An. funestus from various places including western Kenya [33, 34, 54, 55]. In this study, about 40% bovine bloods were detected from indoor-collected An. funestus and higher sporozoite rate in outdoor-collected An. funestus, similar HBI and sporozoite rate for indoor and outdoor collected An. gambiae s.s., indicating the behavioural changes in both vector species in the study area, which concurs with other studies [56,57,58]. Outdoor transmission may have contributed a great proportion to maintaining the high parasite prevalence detected in the study areas, cost-effective control measures need to be developed and implemented to reduce the outdoor residual malaria transmission.
The major missing part of this study is seasonal surveys. Malaria transmission in the study area peaks during the long rainy season, usually from April to June. The low season is from December to February, which is usually hot and dry [32]. A cluster-randomized adaptive intervention has been implemented and is ongoing in the study area [49], which prevents us from conducting low-season surveillance. Nonetheless, both rice and sugarcane need water (irrigation) during the usually dry, hot low-transmission season, which may affect malaria transmission in the northern part of the study area. During the dry season, farms usually irrigate sugarcane and rice fields with flood irrigation utilizing the natural river water flow, which creates huge areas of An. arabiensis and An. funestus larval breeding habitats, supporting very high malaria vector density both indoors and outdoors [33,34,35, 50, 53]. However, irrigation agriculture is nearly null in the southern and central eastern part of the study area, so adding dry-season surveys may not change the four-zone clustering results.
Conclusion
In conclusion, regional heterogeneity of malaria burden and transmission is universal. Examining these heterogeneities is not only important for understanding the current malaria epidemiology but also provides useful information for planning vector control strategies. Implementing interventions adapted to regional eco-epidemiological conditions may yield the robust cost-effectiveness that is especially important in resource-deficient malaria-endemic African countries.
Data availability
Aggregated data at cluster level is available to public and can be obtained from the correspondence author.
References
WHO. World Malaria Report 2021. Geneva: World Health Organization; 2021.
WHO. Global technical strategy for malaria 2016–2030, 2021 update. Geneva: World Health Organization; 2021.
Ethiopia Ministry of Health. National Malaria Elimination Strategic Plan: 2021–2025: Towards a Malaria Free Ethiopia. Addis Ababa, Ethiopia, 2020. https://e-library.moh.gov.et/library/wp-content/uploads/2021/06/Ethiopia-Malaria-Elimination-Strategic-Plan-2021-2025-Agust-31.pdf. Accessed 5 Sept 2022.
Awine T, Malm K, Bart-Plange C, Silal SP. Towards malaria control and elimination in Ghana: challenges and decision making tools to guide planning. Glob Health Action. 2017;10:1381471.
Kenya National Malaria Control Programme. Kenya Malaria Strategy 2019–2023: Towards a Malaria Free Kenya. Ministry of Health, Nairobi, Kenya, 2019.
SADC Elimination 8. SADC Elimination 8 Strategic Plan: 2021–2025. SADC Elimination 8, Windhoek, Namibia, 2021. https://malariaelimination8.org/sites/default/files/publications/e8_-_strategic_plan_2021_0.pdf. Accessed 5 Sept 2022.
Killeen GF. Characterizing, controlling and eliminating residual malaria transmission. Malar J. 2014;13:330.
Benelli G, Beier JC. Current vector control challenges in the fight against malaria. Acta Trop. 2017;174:91–6.
Ferguson HM, Dornhaus A, Beeche A, Borgemeister C, Gottlieb M, Mulla MS, et al. Ecology: a prerequisite for malaria elimination and eradication. PLoS Med. 2010;7:e1000303.
Debebe Y, Hill SR, Tekie H, Dugassa S, Hopkins RJ, Ignell R. Malaria hotspots explained from the perspective of ecological theory underlying insect foraging. Sci Rep. 2020;10:21449.
Kabaghe AN, Chipeta MG, Gowelo S, Mburu M, Truwah Z, McCann RS, et al. Fine-scale spatial and temporal variation of clinical malaria incidence and associated factors in children in rural Malawi: a longitudinal study. Parasit Vectors. 2018;11:129.
Kamau A, Mtanje G, Mataza C, Bejon P, Snow RW. Spatial-temporal clustering of malaria using routinely collected health facility data on the Kenyan Coast. Malar J. 2021;20:227.
Kigozi SP, Kigozi RN, Sebuguzi CM, Cano J, Rutazaana D, Opigo J, et al. Spatial-temporal patterns of malaria incidence in Uganda using HMIS data from 2015 to 2019. BMC Public Health. 2020;20:1913.
Atieli HE, Zhou G, Lee MC, Kweka EJ, Afrane Y, Mwanzo I, et al. Topography as a modifier of breeding habitats and concurrent vulnerability to malaria risk in the western Kenya highlands. Parasit Vectors. 2011;4:241.
Baidjoe AY, Stevenson J, Knight P, Stone W, Stresman G, Osoti V, et al. Factors associated with high heterogeneity of malaria at fine spatial scale in the Western Kenyan highlands. Malar J. 2016;15:307.
Eba K, Habtewold T, Yewhalaw D, Christophides GK, Duchateau L. Anopheles arabiensis hotspots along intermittent rivers drive malaria dynamics in semi-arid areas of Central Ethiopia. Malar J. 2021;20:154.
Gul D, Rodríguez-Rodríguez D, Nate E, Auwan A, Salib M, Lorry L, et al. Investigating differences in village-level heterogeneity of malaria infection and household risk factors in Papua New Guinea. Sci Rep. 2021;11:16540.
Wanjala CL, Waitumbi J, Zhou G, Githeko AK. Identification of malaria transmission and epidemic hotspots in the western Kenya highlands: its application to malaria epidemic prediction. Parasit Vectors. 2011;4:81.
Kessler A, Shylla B, Singh US, Lyngdoh R, Mawkhlieng B, van Eijk AM, et al. Spatial and temporal village-level prevalence of Plasmodium infection and associated risk factors in two districts of Meghalaya. India Malar J. 2021;20:70.
Mwakalinga VM, Sartorius BK, Mlacha YP, Msellemu DF, Limwagu AJ, Mageni ZD, et al. Spatially aggregated clusters and scattered smaller loci of elevated malaria vector density and human infection prevalence in urban Dar es Salaam. Tanzania Malar J. 2016;15:135.
Bousema T, Stresman G, Baidjoe AY, Bradley J, Knight P, Stone W, et al. The impact of hotspot-targeted interventions on malaria transmission in Rachuonyo South district in the Western Kenyan Highlands: a cluster-randomized controlled trial. PLoS Med. 2016;13:e1001993.
Stresman G, Bousema T, Cook J. Malaria hotspots: is there epidemiological evidence for fine-scale spatial targeting of interventions? Trends Parasitol. 2019;35:822–34.
Zhou G, Githeko AK, Minakawa N, Yan G. Community-wide benefits of targeted indoor residual spray for malaria control in the western Kenya highland. Malar J. 2010;9:67.
Tewara MA, Mbah-Fongkimeh PN, Dayimu A, Kang F, Xue F. Small-area spatial statistical analysis of malaria clusters and hotspots in Cameroon; 2000–2015. BMC Infect Dis. 2018;18:636.
Stresman G, Whittaker C, Slater HC, Bousema T, Cook J. Quantifying Plasmodium falciparum infections clustering within households to inform household-based intervention strategies for malaria control programs: an observational study and meta-analysis from 41 malaria-endemic countries. PLoS Med. 2020;17:e1003370.
Mogeni P, Omedo I, Nyundo C, Kamau A, Noor A, Bejon P, Hotspot Group Authors. Effect of transmission intensity on hotspots and micro-epidemiology of malaria in sub-Saharan Africa. BMC Med. 2017;15:121.
Okebe J, Dabira E, Jaiteh F, Mohammed N, Bradley J, Drammeh NF, et al. Reactive, self-administered malaria treatment against asymptomatic malaria infection: results of a cluster randomized controlled trial in The Gambia. Malar J. 2021;20:253.
Howes RE, Mioramalala SA, Ramiranirina B, Franchard T, Rakotorahalahy AJ, Bisanzio D, et al. Contemporary epidemiological overview of malaria in Madagascar: operational utility of reported routine case data for malaria control planning. Malar J. 2016;15:502.
Zhou G, Munga S, Minakawa N, Githeko AK, Yan G. Spatial relationship between adult malaria vector abundance and environmental factors in western Kenya highlands. Am J Trop Med Hyg. 2007;77:29–35.
Zhou G, Afrane YA, Malla S, Githeko AK, Yan G. Active case surveillance, passive case surveillance and asymptomatic malaria parasite screening illustrate different age distribution, spatial clustering and seasonality in western Kenya. Malar J. 2015;14:41.
Minakawa N, Omukunda E, Zhou G, Githeko A, Yan G. Malaria vector productivity in relation to the highland environment in Kenya. Am J Trop Med Hyg. 2006;75:448–53.
Zhou G, Zhong D, Lee MC, Wang X, Atieli HE, Githure JI, et al. Multi-indicator and multistep assessment of malaria transmission risks in Western Kenya. Am J Trop Med Hyg. 2021;104:1359–70.
Ototo EN, Mbugi JP, Wanjala CL, Zhou G, Githeko AK, Yan G. Surveillance of malaria vector population density and biting behaviour in western Kenya. Malar J. 2015;14:244.
Degefa T, Yewhalaw D, Zhou G, Lee MC, Atieli H, Githeko AK, et al. Indoor and outdoor malaria vector surveillance in western Kenya: implications for better understanding of residual transmission. Malar J. 2017;16:443.
Zhou G, Hemming-Schroeder E, Jeang B, Wang X, Zhong D, Lee MC, et al. Irrigation-induced environmental changes sustain malaria transmission and compromise intervention effectiveness. J Infect Dis. 2022;226:1657–66.
Getis A, Ord JK. The analysis of spatial association by use of distance statistic. Geogr Analysis. 1992;24:189–206.
Kweka EJ, Zhou G, Munga S, Lee MC, Atieli HE, Nyindo M, et al. Anopheline larval habitats seasonality and species distribution: a prerequisite for effective targeted larval habitats control programmes. PLoS ONE. 2012;7:e52084.
Hast MA, Stevenson JC, Muleba M, Chaponda M, Kabuya JB, Mulenga M, et al. The impact of three years of targeted indoor residual spraying with pirimiphos-methyl on household vector abundance in a high malaria transmission area of Northern Zambia. Am J Trop Med Hyg. 2020;104:683–94.
Ernst KC, Adoka SO, Kowuor DO, Wilson ML, John CC. Malaria hotspot areas in a highland Kenya site are consistent in epidemic and non-epidemic years and are associated with ecological factors. Malar J. 2006;5:78.
Munyekenye OG, Githeko AK, Zhou G, Mushinzimana E, Minakawa N, Yan G. Plasmodium falciparum spatial analysis, western Kenya highlands. Emerg Infect Dis. 2005;11:1571–7.
Fillinger U, Ndenga B, Githeko A, Lindsay SW. Integrated malaria vector control with microbial larvicides and insecticide-treated nets in western Kenya: a controlled trial. Bull World Health Organ. 2009;87:655–65.
Afrane YA, Mweresa NG, Wanjala CL, Gilbreath TM, Zhou G, Lee MC, et al. Evaluation of long-lasting microbial larvicide for malaria vector control in Kenya. Malar J. 2016;15:577.
Mazigo HD, Massawe IS, Rumisha SF, Kweka EJ, Mboera LEG. Rice farmers’ perceptions and acceptability in the use of a combination of biolarvicide (Bacillus thuringiensis var. israeliensis) and fertilizers application for malaria control and increase rice productivity in a rural district of central Tanzania. Malar J. 2019;18:71.
Rahman R, Lesser A, Mboera L, Kramer R. Cost of microbial larviciding for malaria control in rural Tanzania. Trop Med Int Health. 2016;21:1468–75.
Abong’o B, Gimnig JE, Torr SJ, Longman B, Omoke D, Muchoki M, et al. Impact of indoor residual spraying with pirimiphos-methyl (Actellic 300CS) on entomological indicators of transmission and malaria case burden in Migori County, Western Kenya. Sci Rep. 2020;10:4518.
Dulacha D, Were V, Oyugi E, Kiptui R, Owiny M, Boru W, et al. Reduction in malaria burden following the introduction of indoor residual spraying in areas protected by long-lasting insecticidal nets in Western Kenya, 2016–2018. PLoS ONE. 2022;17:e0266736.
Mahande A, Mosha F, Mahande J, Kweka E. Feeding and resting behaviour of malaria vector, Anopheles arabiensis with reference to zooprophylaxis. Malar J. 2007;6:100.
Zembere K, Chirombo J, Nasoni P, McDermott DP, Tchongwe-Divala L, Hawkes FM, et al. The human-baited host decoy trap (HDT) is an efficient sampling device for exophagic Anopheles arabiensis within irrigated lands in southern Malawi. Sci Rep. 2022;12:3428.
Zhou G, Lee MC, Atieli HE, Githure JI, Githeko AK, Kazura JW, et al. Adaptive interventions for optimizing malaria control: an implementation study protocol for a block-cluster randomized, sequential multiple assignment trial. Trials. 2020;21:665.
Githeko AK, Adungo NI, Karanja DM, Hawley WA, Vulule JM, Seroney IK, et al. Some observations on the biting behavior of Anopheles gambiae s.s., Anopheles arabiensis, and Anopheles funestus and their implications for malaria control. Exp Parasitol. 1996;82:306–15.
Githeko AK. The behaviour and ecology of malaria vectors and malaria transmission in Kisumu District of western Kenya. Dissertation from University of Liverpool, 1992.
Githeko AK, Service MW, Mbogo CM, Atieli FK. Resting behaviour, ecology and genetics of malaria vectors in large scale agricultural areas of Western Kenya. Parassitologia. 1996;38:481–9.
Githeko AK, Service MW, Mbogo CM, Atieli FK, Juma FO. Plasmodium falciparum sporozoite and entomological inoculation rates at the Ahero rice irrigation scheme and the Miwani sugar-belt in western Kenya. Ann Trop Med Parasitol. 1993;87:379–91.
Meyers JI, Pathikonda S, Popkin-Hall ZR, Medeiros MC, Fuseini G, Matias A, et al. Increasing outdoor host-seeking in Anopheles gambiae over 6 years of vector control on Bioko Island. Malar J. 2016;15:239.
Moiroux N, Gomez MB, Pennetier C, Elanga E, Djènontin A, Chandre F, et al. Changes in Anopheles funestus biting behavior following universal coverage of long-lasting insecticidal nets in Benin. J Infect Dis. 2012;206:1622–9.
Salomé G, Riddin M, Braack L. Species composition, seasonal abundance, and biting behavior of malaria vectors in rural Conhane Village, Southern Mozambique. Int J Environ Res Public Health. 2023;20:3597.
Nzioki I, Machani MG, Onyango SA, Kabui KK, Githeko AK, Ochomo E, et al. Current observations on shifts in malaria vector biting behavior and changing vulnerability to malaria transmission in contrasting ecosystems in Western Kenya. Res Square. 2023. https://doi.org/10.21203/rs.3.rs-2772202/v1.
Machani MG, Ochomo E, Amimo F, Mukabana WR, Githeko AK, Yan G, Afrane YA. Behavioral responses of pyrethroid resistant and susceptible Anopheles gambiae mosquitoes to insecticide treated bed net. PLoS ONE. 2022;17:e0266420.
Acknowledgements
The authors wish to thank our colleagues and field staff at the Kenya Medical Research Institute in Kisumu and Tom Mboya University College in Homa Bay who were involved in the project. We acknowledge the assistance provided by the Homa Bay and Kisumu County division office of the Ministry of Health and local healthcare facilities. We thank the local communities for their willingness to participate in the project.
Funding
This study is funded by the National Institutes of Health (R01 A1050243, D43 TW001505, and U19 AI129326). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Design of study: GY, JK, AKG and GZ; Data collection: JH, HA, GZ, DZ, MCL; Field coordination: JG and HA; Data management: MCL and GZ; Laboratory analyses: XM and DZ; Data analyses: GZ, MCL and DZ; Draft of manuscript: GZ, JG, DZ and JK.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the Ethical Review Committee of Maseno University, Kenya (MSU/DRPI/MUERC/00778/19) and the Institutional Review Board (IRB) of the University of California, Irvine, USA (HS# 2017-3512). Volunteers were enrolled from primary schools in the study sites through school administrators with the permission of the division office of the Ministry of Health. Written assent for children (< 18 years of age) was obtained by the participants and their parents or guardians. For parasitological surveillance, written consent and assent for households was obtained from the head of the household and each individual who was willing to participate in the study. Inclusion criteria included providing informed consent and having no reported chronic or acute illness except malaria. Individuals who were unwilling to participate and infants under the age of 6 months were excluded from the study. According to the standard malaria treatment guidelines of the Ministry of Health of Kenya, asymptomatic infections were not treated with antimalarials while symptomatic volunteers were referred to the local government hospital or clinic for diagnosis and treatment free of charge. For entomological surveillance, oral consent was obtained from the head of the household for each participating household. In all surveillance activities, personal identifiers were not included in the data.
Competing interests
All authors: No reported competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Time-lagged correlation between Anopheles density and parasite prevalence and clinical malaria incidence. Table S2. Pairwise correlation between mean Anopheles density, parasite prevalence, clinical malaria incidence, and elevation. Critical value of correlation at significant level of 0.05 is 0.188.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhou, G., Githure, J., Lee, MC. et al. Malaria transmission heterogeneity in different eco-epidemiological areas of western Kenya: a region-wide observational and risk classification study for adaptive intervention planning. Malar J 23, 74 (2024). https://doi.org/10.1186/s12936-024-04903-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-024-04903-4