Abstract
Background
A prospective observational cohort study of COVID-19 patients in a single Emergency Department (ED) showed that sTREM-1- and IL-6-based algorithms were highly predictive of adverse outcome (Van Singer et al. J Allergy Clin Immunol 2021). We aim to validate the performance of these algorithms at ED presentation.
Methods
This multicentric prospective observational study of PCR-confirmed COVID-19 adult patients was conducted in the ED of three Swiss hospitals. Data of the three centers were retrospectively completed and merged. We determined the predictive accuracy of the sTREM-1-based algorithm for 30-day intubation/mortality. We also determined the performance of the IL-6-based algorithm using data from one center for 30-day oxygen requirement.
Results
373 patients were included in the validation cohort, 139 (37%) in Lausanne, 93 (25%) in St.Gallen and 141 (38%) in EOC. Overall, 18% (93/373) patients died or were intubated by day 30. In Lausanne, 66% (92/139) patients required oxygen by day 30. The predictive accuracy of sTREM-1 and IL-6 were similar compared to the derivation cohort. The sTREM-1-based algorithm confirmed excellent sensitivity (90% versus 100% in the derivation cohort) and negative predictive value (94% versus 100%) for 30-day intubation/mortality. The IL-6-based algorithm performance was acceptable with a sensitivity of 85% versus 98% in the derivation cohort and a negative predictive value of 60% versus 92%.
Conclusion
The sTREM-1 algorithm demonstrated good reproducibility. A prospective randomized controlled trial, comparing outcomes with and without the algorithm, is necessary to assess its safety and impact on hospital and ICU admission rates. The IL-6 algorithm showed acceptable validity in a single center and need additional validation before widespread implementation.
Similar content being viewed by others
Background
The coronavirus disease 2019 (COVID-19) pandemic has challenged health care systems over the world since its appearance in Wuhan in December 2019 [1]. The development of prognostic tools to help clinicians recognize patients at risk of unfavorable outcome at presentation is essential to allocate medical resources to appropriate patients [2].
Many host biomarkers have been associated with COVID-19 disease severity including soluble triggering receptor expressed on myeloid cells 1 (sTREM-1) and interleukin-6 (IL-6) [3,4,5,6]. Activation of the sTREM-1 signaling pathway on monocytes/macrophages might contribute to the development of a cytokine storm in the context of COVID-19, and justify using sTREM-1 concentrations to predict hospitalization for oxygen therapy, intubation or death [5]. IL-6 is a pro-inflammatory cytokine increased in patients with severe COVID-19 disease that has been used as a prognostic marker and a therapeutic target for blockade of its signaling pathways [7].
Our team showed in a prospective observational cohort study of COVID-19 patients recruited in the Emergency Department (ED) of Lausanne University Hospital that sTREM-1- and IL-6-based algorithms were highly predictive of adverse outcome [5]. Confirmation of the algorithms predictive value is necessary before their implementation as triage tools [5].
Since post-acute sequelae of COVID-19 (PASC) are reported in ~ 10% of patients with COVID-19 infection, their early detection by initial biomarker levels would be of great additional interest [8].
In the current study, we aimed to externally validate the performance of the sTREM-1 based algorithm at ED presentation, for 30-day intubation/mortality as well as the IL-6 based algorithm for 30-day oxygen requirement. We also aimed to evaluate the predictive value of sTREM-1 and IL-6 for PASC.
Methods
Study design and participants
This multicenter prospective observational study of PCR-confirmed COVID-19 adult patients was conducted in the ED of three Swiss hospitals (Lausanne University Hospital, Kantonsspital St.Gallen, a network of four regional hospitals in Southern Switzerland part of the Ente Ospedaliero Cantonale (EOC)). Patients’ data from the three centers were retrospectively completed and merged to form a multicenter cohort used to validate the previously described algorithms, which were derived from a cohort of patients recruited in the ED of the Lausanne University Hospital during the first wave of the pandemic, between February 6 and April 3, 2020 [5].
The validation multicenter cohort was constituted of three cohorts: patients included during the second and third wave of the pandemics between August 18, 2020, and June 10, 2021 in the ED of the Lausanne University Hospital, patients included in the EDs of EOC between March 10 and April 17, 2020 (first wave) and of Kantonsspital St.Gallen between June 7 and November 11, 2020 (second wave). Inclusion methodology was identical to the one used for the derivation cohort [5].
Patients’ demographics, comorbidities, symptoms, vital signs were recorded.
Host biomarkers
Plasma samples were prospectively collected in the ED of the Lausanne University Hospital, as previously described [5], and serum samples were collected in EOC and St.Gallen hospitals EDs within 24 h after admission. All samples were stored at -80° and retrospectively analyzed head-to-head on a Luminex platform to measure IL-6 and sTREM-1 (R&D Systems, Minneapolis, MN; custom plate, 1:2 dilution). As the samples of the derivation cohort were previously analyzed on an Ella platform, a correction factor was applied on the IL-6 results of the validation cohort, as previously described [9]. In the absence of a validated correction factor between Luminex and ELLA platforms for sTREM-1, this biomarker was measured in the samples of the derivation cohort using the Luminex platform in order to limit potential measurement biases.
Post-acute sequelae of COVID-19
To assess the post-acute sequelae of COVID-19 (PASC), a comprehensive survey was developed and sent once by mail to patients that presented to the Emergency Department between June and November 2020 at St. Gallen Kantonsspital with PCR-confirmed COVID-19 and between February 2020 and February 2021 at the Lausanne University Hospital Emergency Department (N = 1598). Of those, 474 patients submitted evaluable feed-back. All patients who responded to the survey and whom data on IL-6 and sTREM-1 plasma/serum concentrations were available were included for analysis. Questions were asked 13 to 18 months after confirmed SARS-CoV-2 infection for patients from St Gallen and 12 months after infection for patients from Lausanne.
Long-term outcomes were categorized in no PASC vs. those with PASC (if any PASC category present) with the latter divided into three main domains (neurological and cardiopulmonary) to capture the prominent long-term effects of COVID-19.
To determine the frequency of neurological effects, we listed 25 symptoms and asked whether these symptoms had occurred. Each symptom had to be rated twice, at the time of the infection and at the time of the survey. To assess the cardiopulmonary status, we applied the New York Heart Association (NYHA) classification as well as the Canadian Cardiovascular Society (CCS) classification (22 items overall) to determine the presence and extent of cardiopulmonary complaints twice, within 6 months prior to infection and at the time of the survey.
Definition of PASC
In order to determine the presence of PASC we categorized the symptoms into two different phenotypes: (1) Neurological PASC defined by the presence of anosmia, dysgeusia, “pressure” or “fog” in the head, the feeling of being slowed down, concentration problems or forgetfulness, as these seven characteristics were the most frequently occurring among all patients in our cohort. And (2) Cardiopulmonary PASC defined as an increase in NYHA class and/or CCS by ≥ 1 point.
Statistical analyses
We used the same primary outcome as described in the algorithm derivation study consisting of 30-day intubation/mortality. For the Lausanne validation cohort (patients included during the second and third waves of the pandemics) only, a secondary outcome was evaluated: 30-day oxygen requirement (all patients hospitalized with oxygen requirement) [5]. This item was not available in the two other cohorts.
Patients with neurological or cardiopulmonary symptoms (see definitions above) at 12–18 months were classified as having PASC.
Differences between groups were evaluated by 1-way ANOVA, Kruskal-Wallis, or chi-square tests, as appropriate. A two-sided P value < 0.05 was considered indicative of statistical significance.
We first updated the classification and regression tree analysis (CRT) of the derivation cohort, as previously described [5], to determine the adapted cut-off for the sTREM-1 based algorithm using the measurements on the Luminex platform. The updated sTREM-1 cut-off was at 225 pg/mL (compared with 689 pg/ml when measured with the ELLA platform). The respiratory rate cut-off remained unchanged as determined by CRT analysis in the previous study [5]. The prognostic performance of the updated algorithm for 30-day intubation/mortality was similar to the previous CRT model [5].
In a second step, we assessed the diagnostic accuracy of sTREM-1 and IL-6 in the multicenter validation cohort by calculating the area under the receiver-operating characteristic curve (AUROC) for the 30-day intubation/mortality and for the PASC outcome, as previously described [5].
In a third step, we determined the predictive accuracy of the sTREM-1 based algorithm (including first respiratory rate with a cut-off point at 24/min and, second, sTREM-1 with a cut-off at 225 pg/mL), for the multicenter validation. We also determined the performance of the IL-6 based algorithm (including IL-6 with a cut-off at 15.1 pg/mL), using the Lausanne validation cohort solely, as data on oxygen requirement were unavailable in the St. Gallen and EOC cohorts.
For exploratory purposes, we performed another classification and regression tree analysis (CRT), as described [5], including all vital signs, clinical severity scores, and biomarkers, to determine if another algorithm could be determined with the data from all the centers to predict 30-day intubation/mortality.
All analyses were performed with R Core Team (2019), IBM SPSS version 26 and 29 (IBM Corporation, Armonk, NY) and Excel for Windows.
Consent for publication
All included patients signed an informed consent form.
Ethics approval
The Ethics Committees of the canton of Vaud (CER-VD 2019–02283) and of East Switzerland (BASEC 2020–03059 EKOS 20/244) gave ethical approval.
Results
Demographics, clinical characteristics and outcome comparison between cohorts
373 patients were included in the multicenter validation cohort, 139 (37%) in Lausanne, 141 (38%) in Ente Ospedaliero Cantonale (EOC) and 93 (25%) in St. Gallen. Overall, 18% (68/373) patients died or were intubated by day 30: 16% (22/139) in Lausanne, 13% (19/141) in EOC and 29% (27/93) in St. Gallen. In Lausanne, 66% (92/139) patients required oxygen by day 30.
Among included patients, long-term follow-up data for PASC were available for 72 patients in St. Gallen and 45 in Lausanne. PASC was present in 62% of patients, with neurological and cardiopulmonary predominance in 47 (76%) and 11 (18%), respectively.
Table 1 and 2 presents patients’ demographics, clinical characteristics and outcome in the derivation cohort, the validation cohort and in the different centers of the multicenter validation cohort. Patients’ characteristics differed between centers of the validation cohort regarding age and the proportion of patients with comorbidities. The proportion of patients meeting the primary outcome did not differ between the derivation and validation cohorts (p = 0.43) although there was a difference between centers (16% in Lausanne vs. 13% in EOC vs. 29% in St. Gallen; p = 0.007).
Patients with adverse outcome (30-day intubation/mortality) were older (p < 0.001), had more often cardiovascular disease (p = 0.049) and a higher respiratory rate (p < 0.001).
Il-6 and sTREM-1 predict 30-day intubation/mortality in the validation multicenter cohort
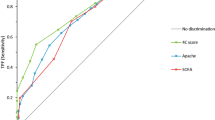
Overall, IL-6 and sTREM-1 levels were significantly higher in patients meeting the primary outcome of intubation/mortality in the multicenter validation cohort (Fig. 1). The predictive accuracy of sTREM-1 and IL-6 were similar in the multicenter validation cohort compared with the derivation cohort (Fig. 2).
Prognostic accuracy of IL-6 and sTREM-1 measured at the ED for 30-day intubation/mortality in the derivation cohort (d) and in the multicenter validation cohort (m). Nonparametric ROC curves were generated and compared between the derivation and multicenter validation cohort using the DeLong method. Area under the receiver-operating characteristic curves (AUROC) with 95% confidence intervals (CI) are presented on the right of the forest plot
Multicenter validation of sTREM-1 based algorithm
We tested the sTREM1 based algorithm in the multicenter validation cohort for prediction of 30-day intubation/mortality, after excluding 32 patients with missing respiratory rate. We obtained a sensitivity of 90%, specificity of 35%, positive likelihood ratio (PLR) of 1.37 and negative likelihood ratio (NLR) of 0.30 confirming generalizability and good performances, particularly with a high sensitivity and moderate NLR, for a safe management of COVID-19 patients. These results were similar to the derivation cohort (updated values from the original derivation study after biomarkers dosing on the Luminex platform and new classification and regression tree analysis (CRT) analysis): sensitivity: 100%, specificity: 62%, PLR: 2.66 and NLR: 0.0) demonstrating good reproducibility.
Validation of the IL-6-based algorithm to predict 30-day oxygen requirement
We tested the IL-6 based algorithm to predict 30-day oxygen requirement solely on the Lausanne validation cohort and had a sensitivity of 85%, specificity of 45%, PLR of 1.53 and NLR of 0.34. This performance was lower than in the derivation cohort (sensitivity 98%, specificity 50%, PLR 1.96 and NLR 0.04) but demonstrated acceptable reproducibility. Indeed, an 85% sensitivity in predicting low-severity events like oxygen requirement is considered acceptable.
Classification and regression tree analysis in the multicenter validation cohort
We performed a new CRT analysis in the multicenter validation cohort (Fig. 3), which resulted in a very similar visual decision-making tree compared with the one of the derivation cohort. It included first respiratory rate and then sTREM-1. Its prognostic performance was similar to the previous CRT model (sensitivity 96%, specificity 47%, PLR 1.81 and NLR 0.09). Similar to the previous decision tree (from the derivation cohort), sTREM-1 enabled the detection of patients with a lower respiratory rate (between the identified cut-off) who were at an elevated risk of intubation or mortality.
Classification and regression tree analysis (CRT) algorithm to predict 30-day intubation/mortality in patients of the multicenter validation cohort. CRT analysis including all biomarkers and vital signs identified the model including a combination of respiratory rate and sTREM-1. The cost of misclassifying a patient who was intubated or died was designated as 10 times the cost of misclassifying a patient who survived without intubation. Cut-off points selected by the CRT analysis are shown between the parent and child nodes. The outcome prediction of the model is indicated below each terminal node
Lack of PASC prediction
Neither IL-6 (area under the receiver-operating characteristic curve (AUROC) 0.562; 95%CI 0.402–0.721) nor sTREM-1 (AUROC 0.499; 95%CI 0.33–0.668) was able to accurately identify patients with PASC (evaluated 12 to 18 months after confirmed SARS-CoV-2).
Discussion
In this multicenter prospective cohort study of SARS-CoV-2 infected patients, we validated our algorithm based on the respiratory rate and sTREM-1 using newly acquired independent data to predict 30-day intubation and mortality. We also validated the IL-6 algorithm to predict 30-day oxygen requirement using single center data (Lausanne) [5]. However, neither of the tested biomarkers was predictive of development of PASC.
Triage tools to help ED clinicians identify patients at risk of adverse outcome are essential to optimize resource allocation, especially in the context of a global pandemic [10]. Increased sTREM-1 levels are associated with poor clinical outcome in patients with COVID-19, as shown in various studies and a meta-analysis. It is therefore a good candidate as triage tool [4,5,6, 11,12,13]. IL-6 plays a role in the genesis of the pro-inflammatory lung-systemic loop leading to a cytokine storm syndrome and acute respiratory distress syndrome [14]. It has been associated with adverse outcome in patients with COVID-19 and might be used to guide clinicians in the identification of patients with severe COVID-19 early in their disease course [15, 16].
Our study had several limitations. First, a different technique for the measurement of biomarkers concentrations with the derivation cohort that required a repeated sTREM-1 measurement with the Luminex platform and an updated sTREM-1-based algorithm based on a new cut-off. Second, plasma samples were used in the derivation and Lausanne validation cohorts, while serum samples were used in EOC and St. Gallen. This could have affected the results of our study. Third, recruitment processes differed between study sites. For example, in EOC and St. Gallen, only admitted patients were included, while in Lausanne, outpatients were also eligible, which could explain the differences of characteristics and main outcome frequency seen in Table 1.1. Finally, the lack of PASC prediction by biomarkers might be related to our small sample size, although a true lack of association is a possibility.
Conclusion
The respiratory rate and sTREM-1 based algorithm demonstrated good reproducibility and generalizability in our multicenter validation study. This provides additional support for its potential real-life use in the ED for early triage of COVID-19 patients and making decisions regarding hospital admission and/or the need for intensive monitoring.
The IL-6 based algorithm for 30-day oxygen requirement prediction showed acceptable local validity and needs to be validated in external centers prior to widespread implementation in the ED.
These biomarker-based algorithms could provide guidance as decision-making tools in the ED. However prospective randomized controlled trial (with / without the algorithms) must be done to evaluate its safety and impact on the rate of hospital and ICU admission in actual practice.
Data Availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- sTREM-1:
-
soluble triggering receptor expressed on myeloid cells 1
- IL:
-
interleukin
- COVID-19:
-
Coronavirus disease 2019
- ED:
-
Emergency Department
- PASC:
-
post-acute sequelae of COVID-19
- EOC:
-
Ente Ospedaliero Cantonale
- PLR:
-
positive likelihood ratio
- NLR:
-
negative likelihood ratio
- CRT:
-
classification and regression tree analysis
- AUROC:
-
area under the receiver-operating characteristic curve
References
Tanne JH, Hayasaki E, Zastrow M, Pulla P, Smith P, Rada AG. Covid-19: how doctors and healthcare systems are tackling coronavirus worldwide. BMJ [Internet]. 2020. https://doi.org/10.1136/bmj.m1090. [cited 2020 May 27];368.
Emanuel EJ, Persad G, Upshur R, Thome B, Parker M, Glickman A, et al. Fair allocation of Scarce Medical Resources in the time of Covid-19. N Engl J Med. 2020;382:2049–55. https://doi.org/10.1056/NEJMsb2005114.
Ponti G, Maccaferri M, Ruini C, Tomasi A, Ozben T. Biomarkers associated with COVID-19 disease progression. Crit Rev Clin Lab Sci. 2020;57:389–99. https://doi.org/10.1080/10408363.2020.1770685.
Chandna A, Mahajan R, Gautam P, Mwandigha L, Gunasekaran K, Bhusan D, et al. Facilitating Safe Discharge through Predicting Disease Progression in Moderate Coronavirus Disease 2019 (COVID-19): a prospective cohort study to develop and validate a clinical prediction model in resource-limited settings. Clin Infect Dis. 2022;75:e368–79. https://doi.org/10.1093/cid/ciac224.
Van Singer M, Brahier T, Ngai M, Wright J, Weckman AM, Erice C, et al. COVID-19 risk stratification algorithms based on sTREM-1 and IL-6 in emergency department. J Allergy Clin Immunol. 2021;147:99–106e4. https://doi.org/10.1016/j.jaci.2020.10.001.
de Nooijer AH, Grondman I, Lambden S, Kooistra EJ, Janssen NAF, Kox M, et al. Increased sTREM-1 plasma concentrations are associated with poor clinical outcomes in patients with COVID-19. Biosci Rep. 2021;41:BSR20210940. https://doi.org/10.1042/bsr20210940.
Potere N, Batticciotto A, Vecchié A, Porreca E, Cappelli A, Abbate A, et al. The role of IL-6 and IL-6 blockade in COVID-19. Expert Rev Clin Immunol. 2021;17:601–18. https://doi.org/10.1080/1744666x.2021.1919086.
Antoniou KM, Vasarmidi E, Russell A-M, Andrejak C, Crestani B, Delcroix M et al. European respiratory society statement on long COVID follow-up. Eur Respiratory J [Internet]. 2022 [cited 2022 Nov 30];60. https://doi.org/10.1183/13993003.02174-2021.
Leligdowicz A, Conroy AL, Hawkes M, Zhong K, Lebovic G, Matthay MA, et al. Validation of two multiplex platforms to quantify circulating markers of inflammation and endothelial injury in severe infection. PLoS ONE. 2017;12:e0175130. https://doi.org/10.1371/journal.pone.0175130.
Wynants L, Calster BV, Bonten MMJ, Collins GS, Debray TPA, Vos MD, et al. Prediction models for diagnosis and prognosis of covid-19 infection: systematic review and critical appraisal. BMJ [Internet]. 2020. https://doi.org/10.1136/bmj.m1328. [cited 2020 May 18];369.
da Silva-Neto PV, de Carvalho JCS, Pimentel VE, Pérez MM, Toro DM, Fraga-Silva TFC, et al. sTREM-1 predicts Disease Severity and Mortality in COVID-19 patients: involvement of peripheral blood leukocytes and MMP-8 activity. Viruses. 2021;13:2521. https://doi.org/10.3390/v13122521.
de Oliveira YLM, de Sá Resende A, Martins-Filho PR, de Moura TR. Role of triggering receptor expressed on myeloid cells-1 (TREM-1) in COVID-19 and other viral pneumonias: a systematic review and meta-analysis of clinical studies. Inflammopharmacol. 2022;30:1037–45. https://doi.org/10.1007%2Fs10787-022-00972-6.
Dholariya S, Parchwani DN, Singh R, Radadiya M, Katoch CDS. Utility of P-SEP, sTREM-1 and suPAR as novel Sepsis biomarkers in SARS-CoV-2 infection. Indian J Clin Biochem. 2022;37:131–8. https://doi.org/10.1007%2Fs12291-021-01008-6.
Polidoro RB, Hagan RS, de Santis Santiago R, Schmidt NW. Overview: systemic inflammatory response derived from Lung Injury caused by SARS-CoV-2 infection explains severe outcomes in COVID-19. Frontiers in immunology [Internet]. 2020 [cited 2022 Nov 1];11. https://doi.org/10.3389/fimmu.2020.01626.
Aziz M, Fatima R, Assaly R. Elevated interleukin-6 and severe COVID-19: a meta-analysis. J Med Virol. 2020;92:2283–5. https://doi.org/10.1002/jmv.25948.
Dhar SK, Damodar KV, Gujar S, Das S. IL-6 and IL-10 as predictors of disease severity in COVID-19 patients: results from meta-analysis and regression. Heliyon. 2021;7:e06155. https://doi.org/10.1016/j.heliyon.2021.e06155.
Acknowledgements
We thank all the patients who accepted to participate and make this study possible. We thank Professor Carron, head of the emergency department of Lausanne University Hospital, who supported the study. We thank all healthcare workers of the emergency department, internal medicine ward, infectious disease service and intensive care unit of the University Hospital of Lausanne, who managed COVID-19 patients. We thank Hélène Gerhard Donnet and Marie-Josée Brochu Vez for helping in sample collection at the emergency department.
Funding
This work was supported in part by: an academic award of the Leenaards Foundation (to NBB) and by the Foundation of Lausanne University Hospital (to NBB); by an intramural grant of the Cantonal Hospital St. Gallen (Nr. 21/13, WCA) and Ente Ospedaliero Cantonale (EOC); by the Canadian Institutes of Health Research (CIHR) Foundation grant FDN-148439 (KCK), CIHR COVID-19 grant 447092 and VR3-172649 (KCK), National Research Council (NRC-IRAP) No. 947684 (KCK), GeoSentinel Foundation (KCK), FAST grants, Thistledown Foundation (KCK), Slaight Family Foundation (KCK), Tesari Foundation (KCK), and the Canada Research Chair program (KCK).
Open access funding provided by University of Lausanne
Author information
Authors and Affiliations
Contributions
Contribution of authors: NBB, WCA, EB, OH, DVG, TB and MVS were involved in the study conception, study design, data analysis, data interpretation, and manuscript writing. MVS, JK, SP, AW, KZ, TK, AL, AC, and KK were involved for the acquisition of the data and critical review of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The Ethics Committees of the canton of Vaud (CER-VD 2019–02283) and of East Switzerland (BASEC 2020–03059 EKOS 20/244) gave ethical approval and all methods were carried out in accordance with relevant guidelines and regulations (declaration of Helsinki). Informed consent was obtained from all subjects and/or their legal guardian(s).
Consent for publication
not applicable.
Competing interests
Disclosure Statement: WCA received speaker’s fee from A.Vogel AG and participated in advisory boards for Pfizer, MSD, GSK, Sanofi and OM Pharma, with reimbursements paid to his institution; MVS, TB, JK, OH, AMW, KZ, TJK, AL, EB, AC, SP, DVG, KCK and NBB have no relevant conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Van Singer, M., Brahier, T., Koch, J. et al. Validation of sTREM-1 and IL-6 based algorithms for outcome prediction of COVID-19. BMC Infect Dis 23, 630 (2023). https://doi.org/10.1186/s12879-023-08630-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08630-0