Abstract
Background
Triggering receptor expressed on myeloid cells-1 (TREM-1) has emerged as an important inflammatory marker of immune response associated with severity and mortality outcomes in infection diseases, including viral pneumonias.
Aim
(1) To evaluate the expression of TREM-1 in patients with COVID-19 and other viral pneumonias compared to healthy individuals; and (2) to analyze the levels of these biomarkers according to disease severity.
Materials and methods
This review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline. Searches were performed in PubMed, Scopus, Embase, and Google Scholar. Studies were considered eligible if they were observational studies that provided data on the levels of TREM-1 in humans with viral pneumonia compared to healthy controls. The results of the meta-analysis were expressed as standardized mean difference (SMD) and an effect size of 0.8 was considered a large effect. A subgroup analysis was performed according to the disease severity.
Results
Seven studies were included in this systematic review. Four studies included patients with COVID-19 and three analyzed patients with different viruses. The meta-analysis was performed only with patients with COVID-19, which showed increased levels of soluble form of TREM-1 (sTREM-1) among patients with COVID-19 compared to healthy controls (SMD 1.53; 95% CI 0.53–2.52; p < 0.01). No differences were found between patients with mild-to-moderate COVID-19 and healthy controls, but higher levels of sTREM-1 were shown among patients with severe COVID-19 (SMD 1.83; 95% CI 0.77–2.88; p < 0.01). All three studies including patients with other viral pneumonias showed that TREM-1 levels were significantly elevated in infected patients compared with controls.
Conclusion
These findings may provide evidence on the pro-inflammatory role of TREM-1 in these infections, contributing to the inflammatory profile and disease progression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Viral pneumonias are one of the most causes of morbidity and mortality worldwide. Currently, there is an emergence of new respiratory viral pathogens including influenza A virus, hantavirus, avian H5N1 influenza, and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) associated with the coronavirus disease-2019 (COVID-19) (Hodgens and Gupta 2022). In clinical practice, a wide range of biomarkers has been used to assess disease severity and mortality. In the last years, several studies have suggested that the Triggering Receptor Expressed on Myeloid Cells-1 (TREM-1) is an important biomarker in the diagnosis and prognosis of viral respiratory diseases (Ye et al. 2014; de Nooijer et al. 2021).
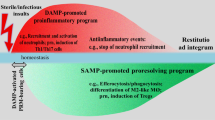
The TREM-1 consists of an innate immune system receptor expressed on innate immune cells and is present in two forms, as a membrane-bound receptor (mTREM-1) and as a soluble protein (sTREM-1) (Bouchon et al. 2000; Kerget et al. 2021). The mTREM-1 has three domains in its structure: one that resembles Ig responsible for binding the ligand, one transmembrane-bound, and a cytoplasmic portion that associates with the DAP12 protein (Colonna 2003; Tammaro et al. 2017). This complex, when activated, increases the expression of pro-inflammatory cytokines including IL-6, IL-8, IL-1β, and TNF-α (de Oliveira Matos et al. 2020), promotes cell survival through the inactivation of pro-apoptotic factors (Yuan et al. 2016; Tammaro et al. 2017), and blocks the synthesis of anti-inflammatory cytokines, such as IL-10 (Dubar et al. 2018).
The soluble form of TREM-1 may originate from the proteolytic cleavage of mTREM-1 through the action of metalloproteinases (Gómez-Piña et al. 2007) or from the translation of an alternative splicing of TREM-1 mRNA (Gingras et al. 2002). Studies have shown that sTREM-1 negatively regulates mTREM-1 signaling by neutralizing its ligands (Yuan et al. 2016; Du et al. 2016). The sTREM-1 has been measured in body fluids, including serum, cerebrospinal fluid, and bronchoalveolar lavage fluid from patients with various inflammatory conditions (de Sá Resende et al, 2021). It has been found that increased levels of sTREM-1 are associated with poor clinical outcomes in infectious and non-infectious diseases (Gibot 2005; Bomfim et al. 2017; de Oliveira Matos et al. 2020).
Some studies have suggested that the broad spectrum of clinical symptoms in viral diseases reflects increased activation of the immune system, characterized by elevated levels of inflammatory cytokines (Martins-Filho et al. 2020; Yang et al. 2020). Although sTREM-1 is a promising inflammatory biomarker (Bellos et al. 2018; de Sá Resende et al. 2021), there is no systematic evidence comparing the levels of this biomarker between patients with viral pneumonia and healthy controls. Thus, the aim of this systematic review and meta-analysis was (1) to evaluate the expression of mTREM-1 and its soluble form in patients with COVID-19 and other viral pneumonias compared to healthy individuals; and (2) to analyze the levels of these biomarkers according to disease severity.
Methods
This review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline (Moher et al. 2010).
Search strategy
Searches were performed in PubMed, Scopus, Embase, and Google Scholar, and were limited to studies published in full-text versions, without language restriction. The reference lists of all eligible studies and reviews were scanned to identify additional studies for inclusion. The main keywords used in the search strategies were as follows: ‘triggering receptor expressed on myeloid cells-1’, ‘soluble triggering receptor expressed on myeloid cells-1’, ‘TREM-1’, ‘sTREM-1’, ‘respiratory tract infections’, ‘viral pneumonia’, ‘COVID-19’, ‘SARS-CoV-2’, ‘coronavirus’, ‘respiratory distress syndrome’, and ‘severe acute respiratory syndrome’. Search strategies were adapted for each database (Supplementary Table 1) and were performed on December 1, 2021.
Eligibility criteria
Studies were considered eligible if they were observational studies that provided data on the levels of TREM-1 in humans with viral pneumonia [respiratory syncytial virus, influenza, parainfluenza, adenovirus, severe acute respiratory syndrome coronavirus (SARS-CoV), severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), Middle East respiratory syndrome coronavirus (MERS-CoV), metapneumovirus, rhinovirus, bocavirus, and parechovirus] compared to healthy controls. We excluded co-infections with bacteria and studies that did not provide clear information about the microorganisms involved in the infections.
Reviews, letters, correspondences, editorials, commentaries, expert opinions, case reports, conference abstracts, and in vitro or animal experiments were also excluded. In addition, authors were contacted via e-mail or using the ResearchGate for missing data in potentially eligible studies. The response time for the requested data was 3 weeks, and those who did not respond were excluded.
Study selection and risk of bias assessment
Two investigators (Y. L. M. O. and A. S. R.) independently screened the search results based on title and abstracts. Relevant studies were read in full and selected according to the eligibility criteria. Disagreements were resolved by a third reviewer (P. R. M-F.).
The Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies of the National Institutes of Health (NIH) (https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools) was used to grade the quality of included studies by two investigators (Y. L. M. O. and A. S. R.).
Data extraction
Two independent investigators (Y. L. M. O. and A. S. R.) extracted the following data: author’s name, year of publication, journal, country, study design, information about eligibility criteria, clinical setting, groups, sample size, age, sex distribution, diagnosis of viral pneumonia and microorganisms involved, disease severity, and TREM-1 values. When TREM-1 values were not reported in tables or text and authors could not be reached, data were extracted using the WebPlotDigitizer (Web Plot Digitizer, V.3.11. Texas, USA: Ankit Rohatgi 2017). If the means and standard deviations were also not reported in the article, indirect methods of extracting estimates were used (Hozo et al. 2005; Wan et al. 2014).
Data analysis
The results of the meta-analysis were expressed as standardized mean difference (SMD). An effect size of 0.2 was considered a small effect, a value of 0.5 a medium effect, and a value of 0.8 a large effect (Colen et al. 2018). We used either a fixed or random-effects model to pool the results of individual studies depending on the presence of heterogeneity. Statistical heterogeneity was quantified by the I2 index using the following interpretation: 0%, no between-study heterogeneity; < 50%, low heterogeneity; 50–75%, moderate heterogeneity; > 75%, high heterogeneity (Higgins and Thompson 2002). In the case of heterogeneity, we used the random-effects model, otherwise, the fixed-effects model was used.
A subgroup analysis was performed according to the disease severity. Although funnel plots may be useful tools in investigating small study effects in meta-analyses, they have limited power to detect such effects when there are few studies (Simmonds 2015). Therefore, because we had a small number of studies included, we did not perform a funnel plot analysis. Forest plots were used to present the effect sizes and 95% confidence interval (CI), and p < 0.05 was used to determine significance. Analyses were conducted using Review Manager, version 5.3 (Cochrane IMS).
Results
Study selection
The search strategy retrieved 285 records and 72 duplicates were deleted. Two additional records were identified in the gray literature. After screening titles and abstracts, 54 full-text articles were assessed for eligibility, and seven (Rohde et al. 2012; Arriaga-Pizano et al. 2015; Zhong and Zhao 2016; Yaşar et al. 2021; de Nooijer et al. 2021; Youngs et al. 2021; Kerget et al. 2021) studies were finally included in this systematic review (Fig. 1).
Study characteristics
The included studies were published from 2012 to 2021 and the main characteristics are listed in Table 1. Three studies were conducted in Europe (Rohde et al. 2012; de Nooijer et al. 2021; Youngs et al. 2021), two studies in Turkey (Yaşar et al. 2021; Kerget et al. 2021), one study in Asia (Zhong and Zhao 2016), and one study in Latin America (Arriaga-Pizano et al. 2015). Only one study was conducted including the pediatric population (Zhong and Zhao 2016).
Four studies included patients with COVID-19 (Yaşar et al. 2021; de Nooijer et al. 2021; Youngs et al. 2021; Kerget et al. 2021) and three studies analyzed patients with different viruses (Rohde et al. 2012; Arriaga-Pizano et al. 2015; Zhong and Zhao 2016). All studies reported that viral infections were confirmed by polymerase chain reaction (PCR). All studies presented a healthy control group consisting of individuals with similar age and sex distribution.
Data synthesis
Due to the small number of studies and the clinical heterogeneity in the study population, the meta-analysis was performed only with patients with COVID-19. All studies including patients with COVID-19 provided data on disease severity. Results from studies including patients with other viral pneumonias were reported descriptively.
SARS-CoV-2 infection and TREM-1
This meta-analysis included 366 individuals, 246 individuals with COVID-19, and 120 healthy controls. Among the COVID-19 patients, 135 were men and 111 were women with a mean age between 51 and 65 years. Among the infected patients, 103 were diagnosed with mild-to-moderate COVID-19 and 143 with severe COVID-19. All four studies have measured the soluble form of TREM-1 in serum (Yaşar et al. 2021; de Nooijer et al. 2021; Youngs et al. 2021; Kerget et al. 2021).
The overall results of the meta-analysis showed increased levels of sTREM-1 among patients with COVID-19 compared to healthy controls (SMD 1.53; 95% CI 0.53– 2.52; p < 0.01; I2 = 93%) and the effect size was considered very large (Fig. 2). In the subgroup analysis evaluating sTREM-1 expression according to disease severity, no differences were found between patients with mild-to-moderate COVID-19 and healthy controls (SMD 1.17; 95% CI −0.61 to 2.95; p = 0.20; I2 = 97%), but higher levels of sTREM-1 were shown among patients with severe COVID-19 (SMD 1.83; 95% CI 0.77–2.88; p < 0.01; I2 = 91%) (Fig. 3).
Table 2 shows the quality assessment tool that resulted in a moderate-to-high risk of bias. Although research question and outcome measures were clearly stated in all studies, important questions on the study design were not clearly described, such as exposure measures of the control group, sample size justification, blinding of outcome assessors, and adjustment for confounders.
Other viral pneumonias and TREM-1
Three studies have investigated differences in TREM-1 levels among patients with other viral pneumonias and healthy individuals. Only one study evaluated TREM-1 expression on monocytes (Arriaga-Pizano et al. 2015), while two studies have analyzed the soluble form of TREM-1 (Rohde et al. 2012; Zhong and Zhao 2016). Zhong and Zhao (2016) included children in the study population and Rohde et al. (2012) have focused on adults with smoking habits. All three studies showed that TREM-1 levels were significantly elevated in infected patients compared with controls.
Discussion
Viral respiratory infections are a burden on the public health system due to their rapid transmissibility among people and poor capacity for control and recovery. Since the outbreak of the SARS-CoV-2 infection in December 2019, there is urgency in identifying biomarkers of severity to improve diagnosis and predict the clinical course of patients (de Nooijer et al. 2021; Kerget et al. 2021). In this context, systematic reviews have consistently demonstrated an association between high levels of sTREM-1 and worse clinical outcomes in patients with infectious diseases. However, these studies have summarized the available evidence based on infections caused by different microorganisms, which limits the understanding of the role of TREM-1 in specific infections (Jiyong et al. 2009; Ye et al. 2014; Su et al. 2016). Thus, to the best of our knowledge, this is the first meta-analysis performed to assess the levels of TREM-1 in viral infections of lower respiratory tract, especially from COVID-19 patients.
Diagnosis in the early stages of infection can be challenging due to the lack of specificity of clinical features and the limited effectiveness of conventional inflammatory markers, such as C-reactive protein (CRP) (Ansar and Ghosh 2016). In viral infections, including COVID-19, the patient can progress to a critical condition called cytokine storm, which is characterized by a significant elevation of inflammatory markers that can lead to hyperinflammation and multiple organ failure (Tang et al. 2020; Luo et al. 2021). In this regard, TREM-1 is early activated on the surface of myeloid cells, including neutrophils and monocytes, to promptly trigger the innate immune response. These cells, in turn, release various cytokines and inflammatory proteins to prevent the spread of the virus, improve its elimination, and recruit more immune cells. However, flaws in TREM-1 suppression mechanisms may contribute to the cytokine storm.
As a feedback mechanism, surface-bound TREM-1 is cleaved in its soluble form sTREM-1, which is suggested to act as a regulator of the inflammatory status. Soluble TREM-1 originates through proteolysis by metalloproteinases or alternative splicing (Gao et al. 2019) after stimulation of TREM-1 by inflammatory molecules (Van Singer et al. 2021). Elevated sTREM-1 levels, mainly as a result of neutrophil activation, correlate with other inflammatory mediators, such as IL-6 and TNF-α, and indicate the occurrence of cell damage associated with the inflammatory process and the release of proteinases by necrotic cells or pathogens (Dubar et al. 2018). In our meta-analysis, we found an increase in sTREM-1 in infected patients compared to healthy individuals, demonstrating the involvement of this inflammatory biomarker in COVID-19. In the subgroup analysis, we found evidence that patients with severe COVID-19 have higher levels of sTREM-1 than patients with mild or moderate disease. In addition, individual results have shown elevated levels of TREM-1 in other viral respiratory-tract infections. These results indicate that TREM-1 may be useful in predicting clinical outcomes in patients with viral pneumonia.
A few studies have investigated whether TREM-1 can be a sensitive and specific biomarker of general infections to predict mortality (Su et al. 2016; Jedynak et al. 2018; Wright et al. 2020). Considering respiratory infections, a meta-analysis by Su et al. (2016) demonstrated a sensitivity of 0.75 (95% CI 0.61–0.86) and specificity of 0.66 (95% CI 0.54–0.75) suggesting a moderate prognostic value of sTREM-1 to predict mortality. However, the between-study heterogeneity was high mainly due to variability in the type of infections, including cases of sepsis. Although it was not possible to measure the sensitivity and specificity of sTREM-1 in the present meta-analysis, our study showed the behavior of sTREM-1 in viral pneumonias including COVID-19. Despite these findings, further studies are needed to confirm the prognostic value and clinical significance of TREM-1 in viral infections.
Our study has some major limitations: (1) relatively small number of studies that evaluated TREM-1 function in respiratory viral infections; (2) different methods of TREM-1 detection; and (3) difficulty in summarizing TREM-1 levels in patients with other viral infections due to heterogeneity between studies. Although these limitations, this is the first study to synthesize the available evidence on TREM-1 levels in patients with COVID-19 and other viral pneumonias. These findings may provide evidence on the pro-inflammatory role of TREM-1 in these infections, contributing to the inflammatory profile and disease progression.
Data availability
Data were directly retrieved from published original articles or by authors upon request by the reviewers.
References
Ansar W, Ghosh S (2016) Inflammation and inflammatory diseases, markers, and mediators: role of CRP in some inflammatory diseases. Biology of C reactive protein in health and disease. Springer India, New Delhi, pp 67–107. https://doi.org/10.1007/978-81-322-2680-2_4
Arriaga-Pizano L, Ferat-Osorio E, Rodríguez-Abrego G et al (2015) Differential immune profiles in two pandemic influenza A(H1N1)pdm09 virus waves at pandemic epicenter. Arch Med Res 46:651–658. https://doi.org/10.1016/j.arcmed.2015.12.003
Bellos I, Fitrou G, Daskalakis G et al (2018) Soluble TREM-1 as a predictive factor of neonatal sepsis: a meta-analysis. Inflamm Res 67:571–578. https://doi.org/10.1007/s00011-018-1149-4
Bomfim LGS, Magalhães LS, Santos-Filho MAA et al (2017) Leishmania infantum induces the release of sTREM-1 in visceral leishmaniasis. Front Microb. https://doi.org/10.3389/fmicb.2017.02265
Bouchon A, Dietrich J, Colonna M (2000) Cutting edge: inflammatory responses can be triggered by TREM-1, a novel receptor expressed on neutrophils and monocytes. J Immunol 164:4991–4995. https://doi.org/10.4049/jimmunol.164.10.4991
Colen CG, Ramey DM, Cooksey EC, Williams DR (2018) Racial disparities in health among nonpoor African Americans and Hispanics: the role of acute and chronic discrimination. Soc Sci Med 199:167–180. https://doi.org/10.1016/j.socscimed.2017.04.051
Colonna M (2003) TREMs in the immune system and beyond. Nat Rev Immunol 3:445–453. https://doi.org/10.1038/nri1106
de Nooijer AH, Grondman I, Lambden S et al (2021) Increased sTREM-1 plasma concentrations are associated with poor clinical outcomes in patients with COVID-19. Biosci Rep. https://doi.org/10.1042/BSR20210940
de Oliveira Matos A, dos Santos Dantas PH, Figueira Marques Silva-Sales M, Sales-Campos H (2020) The role of the triggering receptor expressed on myeloid cells-1 (TREM-1) in non-bacterial infections. Crit Rev Microb 46:237–252. https://doi.org/10.1080/1040841X.2020.1751060
de Sá Resende A, de Oliveira YLM, de Moura TR, Martins-Filho PR (2021) Potential role of triggering receptor expressed on myeloid cells-1 (Trem-1) in sars-cov-2 infection: first insights. EXCLI J 20:722–723
Du Y, Wu T, Zhou XJ et al (2016) Blockade of CD354 (TREM-1) ameliorates anti-GBM-induced nephritis. Inflammation 39:1169–1176. https://doi.org/10.1007/s10753-016-0351-1
Dubar M, Carrasco K, Gibot S, Bisson C (2018) Effects of porphyromonas gingivalis LPS and LR12 peptide on TREM-1 expression by monocytes. J Clin Periodontol 45:799–805. https://doi.org/10.1111/jcpe.12925
Gao S, Yi Y, Xia G et al (2019) The characteristics and pivotal roles of triggering receptor expressed on myeloid cells-1 in autoimmune diseases. Autoimmun Rev 18:25–35. https://doi.org/10.1016/j.autrev.2018.07.008
Gibot S (2005) Clinical review: role of triggering receptor expressed on myeloid cells-1 during sepsis. Crit Care 9:485–489. https://doi.org/10.1186/cc3732
Gingras MC, Lapillonne H, Margolin JF (2002) TREM-1, MDL-1, and DAP12 expression is associated with a mature stage of myeloid development. Mol Immunol 38:817–824. https://doi.org/10.1016/S0161-5890(02)00004-4
Gómez-Piña V, Soares-Schanoski A, Rodríguez-Rojas A et al (2007) Metalloproteinases shed TREM-1 ectodomain from lipopolysaccharide-stimulated human monocytes. J Immunol 179:4065–4073. https://doi.org/10.4049/jimmunol.179.6.4065
Higgins JPT, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558. https://doi.org/10.1002/sim.1186
Hodgens A, Gupta V (2022) Severe acute respiratory syndrome. http://www.ncbi.nlm.nih.gov/pubmed/32644403. Accessed 20 Dec 2021
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13. https://doi.org/10.1186/1471-2288-5-13
Jedynak M, Siemiatkowski A, Mroczko B et al (2018) Soluble TREM-1 serum level can early predict mortality of patients with sepsis, severe sepsis and septic shock. Arch Immunol Ther Exp (warsz) 66:299–306. https://doi.org/10.1007/s00005-017-0499-x
Jiyong J, Tiancha H, Wei C, Huahao S (2009) Diagnostic value of the soluble triggering receptor expressed on myeloid cells-1 in bacterial infection: a meta-analysis. Intensive Care Med 35:587–595. https://doi.org/10.1007/s00134-008-1333-z
Kerget F, Kerget B, İba Yılmaz S, Kızıltunç A (2021) Evaluation of the relationship between TREM-1/TREM-2 ratio and clinical course in COVID-19 pneumonia. Int J Clin Pract. https://doi.org/10.1111/ijcp.14697
Luo X, Zhu Y, Mao J, Du R (2021) T cell immunobiology and cytokine storm of COVID-19. Scand J Immunol. https://doi.org/10.1111/sji.12989
Martins-Filho PR, Tavares CSS, Santos VS (2020) Factors associated with mortality in patients with COVID-19. a quantitative evidence synthesis of clinical and laboratory data. Eur J Intern Med 76:97–99. https://doi.org/10.1016/j.ejim.2020.04.043
Moher D, Liberati A, Tetzlaff J, Altman DG (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8:336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Rohde G, Radsak MP, Borg I et al (2012) Levels of soluble triggering receptor expressed on myeloid cells 1 in infectious exacerbations of chronic obstructive pulmonary disease. Respiration 83:133–139. https://doi.org/10.1159/000328413
Simmonds M (2015) Quantifying the risk of error when interpreting funnel plots. Syst Rev 4:24. https://doi.org/10.1186/s13643-015-0004-8
Su L, Liu D, Chai W et al (2016) Role of sTREM-1 in predicting mortality of infection: a systematic review and meta-analysis. BMJ Open 6:e010314. https://doi.org/10.1136/bmjopen-2015-010314
Tammaro A, Derive M, Gibot S et al (2017) TREM-1 and its potential ligands in non-infectious diseases: from biology to clinical perspectives. Pharm Ther 177:81–95. https://doi.org/10.1016/j.pharmthera.2017.02.043
Tang L, Yin Z, Hu Y, Mei H (2020) Controlling cytokine storm is vital in COVID-19. Front Immunol. https://doi.org/10.3389/fimmu.2020.570993
Van Singer M, Brahier T, Ngai M et al (2021) COVID-19 risk stratification algorithms based on sTREM-1 and IL-6 in emergency department. J Allergy Clin Immunol 147:99-106.e4. https://doi.org/10.1016/j.jaci.2020.10.001
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135. https://doi.org/10.1186/1471-2288-14-135
Wright SW, Lovelace-Macon L, Hantrakun V et al (2020) sTREM-1 predicts mortality in hospitalized patients with infection in a tropical, middle-income country. BMC Med 18:159. https://doi.org/10.1186/s12916-020-01627-5
Yang L, Liu S, Liu J et al (2020) COVID-19: immunopathogenesis and Immunotherapeutics. Signal Transduct Target Ther 5:128. https://doi.org/10.1038/s41392-020-00243-2
Yaşar Ş, Çolak C, Yoloğlu S (2021) Artificial intelligence-based prediction of Covid-19 severity on the results of protein profiling. Comput Methods Progr Biomed 202:105996. https://doi.org/10.1016/j.cmpb.2021.105996
Ye W, Hu Y, Zhang R, Ying K (2014) Diagnostic value of the soluble triggering receptor expressed on myeloid cells-1 in lower respiratory tract infections: a meta-analysis. Respirology 19:501–507. https://doi.org/10.1111/resp.12270
Youngs J, Provine NM, Lim N et al (2021) Identification of immune correlates of fatal outcomes in critically ill COVID-19 patients. Plos Pathog 17:e1009804. https://doi.org/10.1371/journal.ppat.1009804
Yuan Z, Syed M, Panchal D et al (2016) TREM-1-accentuated lung injury via miR-155 is inhibited by LP17 nanomedicine. Am J Physiol Cell Mol Physiol 310:L426–L438. https://doi.org/10.1152/ajplung.00195.2015
Zhong MF, Zhao JM (2016) Diagnostic values of plasma CD64 and sTREM-1 for pediatric pneumonia. Zhongguo Dang Dai Er Ke Za Zhi 18:599–602. https://doi.org/10.7499/j.issn.1008-8830.2016.07.006
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
YLMO and ASR: conceptualization, methodology, investigation, writing, and original draft preparation. PRMF: methodology, statistical analysis, manuscript review, and editing. TRM: conceptualization, methodology, supervision, manuscript review, and editing. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no competing interest. All authors have approved the manuscript for submission.
Ethical approval
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
de Oliveira, Y.L.M., de Sá Resende, A., Martins-Filho, P.R. et al. Role of triggering receptor expressed on myeloid cells-1 (TREM-1) in COVID-19 and other viral pneumonias: a systematic review and meta-analysis of clinical studies. Inflammopharmacol 30, 1037–1045 (2022). https://doi.org/10.1007/s10787-022-00972-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-022-00972-6