Abstract
Background
Resistance training (RT) and nutritional supplementation are recommended for the management of sarcopenia in older adults. However, optimal RT intensity for the treatment of sarcopenia has not been well investigated.
Methods
This network meta-analysis aims to determine the comparative effectiveness of interventions for sarcopenia, taking RT intensity into consideration. RT intensity was classified into light-to-moderate intensity RT(LMRT), moderate intensity RT(MRT), and moderate-to-vigorous intensity RT(MVRT) based on percentage of one repetition maximum (%1RM) and/or rating of perceived exertion.
Results
A total of 50 RCTs (N = 4,085) were included after screening 3,485 articles. The results confirmed that RT with or without nutrition was positively associated with improved measures of muscle strength and physical performance. Regarding RT intensity, LMRT only demonstrated positive effects on hand grip (aerobic training + LMRT + nutrition: mean difference [MD] = 2.88; 95% credential intervals [CrI] = 0.43,5.32). MRT provided benefits on improvement in the 30-s chair stand test (repetitions) (MRT: MD = 2.98, 95% CrI = 0.35,5.59), timed up and go test (MRT: MD = -1.74, 95% CrI: = -3.34,-0.56), hand grip (MRT: MD = 2.44; 95% CrI = 0.03,5.70), and leg press (MRT: MD = 8.36; 95% CrI = 1.87,13.4). MVRT also improved chair stand test repetitions (MVRT: MD = 5.64, 95% CrI = 0.14,11.4), gait speed (MVRT + nutrition: MD = 0.21, 95% CrI = 0.003,0.48), appendicular skeletal muscle index (MVRT + nutrition: MD = 0.25, 95% CrI = 0.01,0.5), and leg press (MVRT: MD = 14.7, 95% CrI: 5.96,22.4; MVRT + nutrition: MD = 17.8, 95% CrI: 7.55,28.6).
Conclusion
MVRT had greater benefits on muscle mass, lower extremity strength, and physical performance compared to MRT. Increasing RT intensity may be recommended for sarcopenic older adults.
Similar content being viewed by others
Introduction
Sarcopenia, an age-related condition characterized by progressive decrease in muscle mass, strength, and function, currently affects an estimated 10–40% of community-dwelling older adults [1, 2]. Additionally, sarcopenia is associated with increased risk of falls by 60%, increased fractures by 84%, and adverse health outcomes such as functional decline, decreased quality of life, mortality, and increased healthcare costs [1, 3, 4].
Modifiable risk factors including low physical activity and protein intake have been targeted for the prevention and treatment of sarcopenia [5]. In 2018, the International Conference on Sarcopenia and Frailty Research (ICSFR) guideline for the management of sarcopenia recommended progressive resistance training (RT) and a protein-rich diet or protein supplementation [6]. Recent systematic reviews and meta-analyses have demonstrated desirable effects of various forms of exercise with or without nutrition interventions on muscle strength and physical performance, as measured by gait speed (GS) or short physical performance battery (SPPB) [7,8,9]. However, the evidence for increasing muscle mass is less consistent. One meta-analysis focusing on sarcopenic older adults found no improvement after exercise, nutrition, and mixed exercise (aerobic training (AT) plus RT) and nutrition [8], while another meta-analysis published in the same year determined that mixed exercise with nutrition resulted in significantly increased muscle mass among people with sarcopenia [10]. Discrepancies in study results may be due to varied inclusion criteria, different definitions of sarcopenia used, and inconsistent exercise protocols in exercise type, frequency, intensity, and duration.
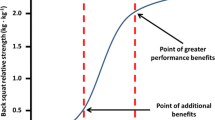
More importantly, exercise intensity, especially for RT, has not been fully taken into consideration in previous systematic reviews and meta-analyses. ACSM guidelines suggest moderate-to-vigorous RT intensity (60–80% one-repetition maximum, 60–80%1RM) of resistance exercise for older adults [11]. Recent systematic reviews and meta-analyses suggest that progressive RT may reduce mortality and produce greater gains in muscle strength in a linear fashion among older adults in general [12,13,14]. On the other hand, one meta-analysis focusing on older adults reported that high-load RT only produced marginal gains in muscle mass and insignificant improvements in muscle strength [15]. According to Csapo et al. because muscle hypertrophy plateaus above a certain point in high intensity training, high frequency low intensity training may be required to continue increasing muscle mass [15]. Additionally, high-intensity exercise might decrease adherence and lead to decline in total exercise [16]. Thus, clarification of the effects of RT intensity on muscle mass, strength, and physical performance is needed to make precise exercise prescriptions for older adults with sarcopenia.
The objective of this study is to compare the effectiveness of interventions for sarcopenia, with a particular focus on determining the optimal intensity of RT for older adults with sarcopenia. We conducted a network meta-analysis of randomized controlled trials (RCTs) in older adults with sarcopenia and pooled data of intervention effects on muscle mass (appendicular skeletal muscle, leg muscle mass, and skeletal muscle mass), muscle strength (handgrip strength (HG), chest press, and leg press), and physical function (5 times sit to stand (5TSTS), number of repetitions done in the 30-s chair stand test, timed up and go test (TUG), SPPB, GS, and 6-min walk test).
Methods
This network meta-analysis was performed according to the standards described in the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) statement [17]. The study was registered in PROSPERO under the ID CRD42021287114.
Search strategy and selection process
Using Pubmed, Embase, Central Register of Controlled Trials (CENTRAL), and ClinicalTrials (Clinicaltrials.gov), we identified RCTs on sarcopenia from database inception until October 20, 2022. The keywords used for the search were “sarcopenia” or “sarcopeni*” and “randomized controlled trial.” To identify pertinent studies, we utilized the search terms: “train*”, “physical activity”, “exercise”, “diet”, “nutr*”, and “drug therapy”. Additionally, we incorporated the associated MeSH terms: “sarcopenia”, “exercise”, “diet, food, and nutrition”, “nutrition therapy”, and “drug therapy”. "We integrated the search terms using the Boolean operators “AND” and “OR”. The complete search terms and search string can be found in Supplementary S1. To ensure comprehensive inclusion of potentially relevant articles, we refrained from applying filters related to publication type, age, or language. Additional studies were identified by reviewing the reference lists of papers found through the database search. Study protocol paper and conference abstracts were not included. The inclusion criteria for studies were: (1) community-dwelling adults aged over 18 years, (2) participants diagnosed with either sarcopenia (characterized by low muscle mass and low muscle strength, and/or reduced physical performance) or dynapenia (manifested as low muscle strength and/or reduced physical performance but with normal muscle mass) [18, 19], and (3) RCT. Since severe illness such as cancer, liver cirrhosis, or end stage renal failure could induce cachexia and decrease physical function, studies involving patients with these comorbidities were excluded.
During the initial selection process, two independent authors reviewed the title, abstract, and full text of each reference to determine its suitability for inclusion. In cases of uncertainty regarding the study’s relevance, a third author was consulted to achieve consensus. When multiple studies on the same population were conducted by the same research group and reported identical outcomes of interest, we only chose the results from the study with the longest follow-up duration. The process of selection is detailed in Fig. 1. Finally, the included studies underwent a comprehensive assessment of bias risk using the Cochrane Risk of Bias Tool 2.0 (RoB 2.0) [20], accessible at https://methods.cochrane.org/risk-bias-2. This tool evaluates each study’s susceptibility to potential bias across multiple domains, including randomization procedures, adherence to intended interventions, handling of missing outcome data, measurement of outcome variables, and selection bias. We categorized the overall risk of bias in each domain as “Low risk of bias,” “Some concerns,” or “High risk of bias.”
Data extraction
RCTs with at least one intervention (e.g., nutrition, exercise, whole body electrical muscle stimulation [WB-EMS], whole body vibration [WBV], electrical puncture, Taichi, global sensorimotor training, focused vibrational therapy, and drug treatment [bimagrumab, MK-0773, perindopril, oxytocin]) were included. One researcher entered the following data for each paper into a standardized table: authors, publication year, location of study, number of participants, baseline characteristics of participants, inclusion criteria, exclusion criteria, intervention(s), comparison group, duration of intervention, intensity of resistance exercise, and outcomes of interest. Outcome measures included 5TSTS, number of repetitions done in the 30-s chair stand test, TUG, SPPB, GS, 6-min walk test, appendicular skeletal muscle index (ASMI), leg muscle mass, skeletal muscle mass, HG, chest press, leg press. Since the quality of life (QOL), as measured by either the Short Form 36 or Short Form 12, is divided into physical and mental components, the combined QOL is represented using overall, physical, and psychological scores.
Grading of exercise intensity
Exercise was initially classified as either AT or RT. According to ACSM guidelines, the intensity of RT was categorized into five levels: very light, light, moderate, vigorous, and near-maximal to maximal intensity, based on repetition maximum (RM) and/or rating of perceived exertion (RPE) [11]. The term “1RM” refers to the maximum weight an individual can lift for a single repetition. Relative intensity, indicated as percentage of 1RM (%1RM), was calculated by converting from the repetition numbers implemented in the RT program [21]. The Borg RPE is a subjective scale and reliable measure of RT intensity [22]. However, the sarcopenia management guidelines advocate for RT of at least moderate intensity [23]. Accordingly, we stratified RT intensity into 3 distinct levels: light-to-moderate (LMRT), moderate (MRT), and moderate-to-vigorous intensity RT (MVRT). Specifically, LMRT corresponds to scores of 6–11 on the Borg RPE scale (whose full range is 6–20), 0–4 on the Modified Borg’s scale (with a complete range of 0–10), or less than 49% of 1RM [11]. MRT is represented by ratings of 12–13 on the Borg RPE scale, 5–6 on the Modified Borg’s scale, or 50% ~ 69% of 1RM [11]. MVRT is characterized by scores of 14–17 on the Borg RPE scale, 7–8 on the Modified Borg’s scale, or 70% ~ 84% of 1RM [11]. To ensure accuracy, both a sports medicine physician and a geriatrician meticulously reviewed all included studies. They then determined the RT intensity through mutual consensus.
AT primarily focuses on augmenting cardiovascular endurance and efficiency. Nonetheless, it also leads to discernible enhancements in muscular strength and endurance [24]. Given that 50% of 1RM is roughly equivalent to an average of 26 repetitions [25], AT, which typically involves over 100 repetitive movements, can be categorized as LMRT. Thus, the effects of AT on muscular strength and endurance might be more subtle compared to those elicited by RT. Consequently, we opted not to further classify AT.
Statistical analysis
Network meta-analysis was performed using changes in mean and standard deviation (SD) from baseline. 95% two-tailed credible intervals (CrI) were calculated, with p < 0.05 indicating statistical significance. When studies only reported 25% and 75% percentile of outcome values, we estimated SD based on interquartile range (IQR = 1.349*SD) [26]. If changes in SD were not available, it was estimated using the following equation: [SDpre2 + SDpost2-2 × CC × SDpre × SDpost]0.5 [9, 27]. SDpre represented the SD at baseline and SDpost was the SD after the intervention. CC was the correlation coefficient between baseline and post-intervention values for the same individual. If the correlation was not reported, CC was designated as 0.5. Network plots visually represented the number of study participants according to the size of nodes and the number of trials conducted according to the thickness of connecting lines. Forest plots depicted the intervention effects compared to the control group. Effectiveness of the interventions were ordered by rank probability and determined using the surface under the cumulative ranking curve (SUCRA), where larger surface areas equaled greater treatment effects [28].
We used the web‐based software MetaInsight V4.0.0 powered by Rshiny for network meta-analysis combining direct and indirect comparisons and figure plotting [29, 30]. All Bayesian statistical calculations were performed using R package gemtc [28]. Random effects model by heterogeneity consideration was employed because results under random effects model in all analyses demonstrated better fitting with lower deviance information criterion values when compared to fixed effects model [31]. Bayesian rank probabilities were visualized with (cumulative) Rank-O-Grams. Publication bias was examined by Egger’s regression [32]. The consistency of network meta-analysis was assessed using the node-splitting models to compare the results between direct and indirect comparisons [33]. Several sensitivity and subgroup analyses were conducted to ensure consistency and stability of results. Analyses were repeatedly performed by (1) sequentially excluding each trial and (2) omitting studies with a high risk of bias.
Results
Study selection
The PRISMA flow diagram (Fig. 1) shows the study selection process and provides reasons for study exclusion. A total of 3,846 publications were identified from 4 databases and hand search, of which 1,681 duplicate records were removed. After screening titles and abstracts based on the pre-specified criteria, the full text of 311 records were assessed for eligibility. After full-text review, 55 records were retained. Five more articles were removed due to lack of data. Therefore, a final total of 50 RCTs were included in quantitative network meta-analysis. The results of risk of bias assessments using ROB2 are shown in Table S1.
Study characteristics
Table 1 shows characteristics and details of the included studies. The 50 studies included (N = 4,085, mean age range:55.0 ± 9.6 to 89.5 ± 4.4 years) were published between 2012–2022 and were conducted around the globe, mostly in Asia (7 studies in Taiwan, 4 in South Korea, 3 in China, and 2 in Japan). Three studies were conducted cross-nationally in Europe and North America. There were 14 studies involving RT, 5 studies involving AT + RT, 7 studies involving nutritional intervention, 1 study involving AT + nutritional intervention, 9 studies involving RT + nutritional intervention, and 4 studies involving AT + RT + nutritional intervention, and 6 studies involving WB-EMS and WBV. Adherence rates to the exercise intervention ranged from 74 to 100%, with no apparent correlation to exercise intensity. Details of the included trials are shown in Table S2.
Regarding sarcopenia outcome measures, 23 studies examined muscle mass, 26 studies examined handgrip strength (including one study on upper body strength), 16 studies examined lower leg strength, 23 studies examined gait speed, and 25 studies examined physical performance, including TUG, SPPB, single leg stance, and chair stand tests. Network plots of trials with each outcome are shown in Fig S1a-1 m.
Results of network meta-analysis
Physical performance
5 times sit to stand
Studies measuring this outcome included a total of 108 subjects receiving RT, 40 subjects receiving AT + RT, 314 subjects receiving nutritional interventions, 139 subjects receiving RT and nutritional interventions, 36 subjects receiving AT + RT and nutritional interventions, 48 subjects receiving whole body EMS, 24 subjects practicing Taichi, 115 subjects receiving Bimagrumab, and 522 subjects in the control group (Table 1). The results showed that the time taken to complete 5TSTS decreased significantly in the RT group (mean difference[MD]: -1.59 s; 95% CrI: -2.78, -0.44; SUCRA = 68.7%), RT + nutritional intervention group (MD:-1.57 s; 95% CrI: -2.57, -0.48; SUCRA = 67.8%), and AT + RT + nutritional intervention group (MD:-2.28 s; 95% CrI: -4.23, -0.29; SUCRA = 84.9%) (Fig S2a, S3a). A favorable trend was found in AT + RT group but did not reach statistical significance (Fig S2a).
Regarding RT intensity, neither LMRT, MRT nor MVRT was associated with improvement in 5TSTS (Fig. 2a). In the subgroup analysis, no differences were found for all interventions done on women and participants with low muscle mass.
Forest plot comparing the effects of LMRT, MRT, and MVRT on physical performance. An asterisk denotes statistical significance. a 5 times sit to stand (5TSTS). b 30-s chair stand test (repetitions). c timed up and go test (TUG). d short physical performance battery (SPPB). e gait speed. f six min walk test
30-s chair stand test (repetitions)
A total of 95, 25, 15, and 93 older adults in the RT, AT + RT, RT + nutrition, and placebo group, respectively, were included for comparison (Table 1). RT had the greatest effect (SUCRA = 79.15%) on the number of repetitions done in the 30-s chair stand test with a MD of 3.72 (95% CrI: 1.23, 7.31) (Fig S2b, S3b). Regarding RT intensity, MRT (MD:2.98; 95% CrI:0.35, 5.59; SUCRA = 98.32%) and MVRT (MD:5.64; 95% CrI:0.14, 11.4; SUCRA = 81.19%) were both associated with dose-responsive improvement in the 30-s chair stand test (Fig. 2b).
In the subgroup analysis, RT remained effective in women, resulting in a MD of 3.69 (95% CrI: 1.22, 7.27; SUCRA = 85.94%).
Timed up and go test
A total of 143 older adults using RT, 86 adults using nutrition supplements, 98 adults using RT + nutrition, 12 adults using oxytocin, 28 adults practicing Taichi, 44 adults using whole body EMS, and 194 adults in the placebo group were included for comparison (Table 1). RT demonstrated greater improvement than other interventions (SUCRA = 65.52%) on TUG with a MD of -0.85 (95% CrI: -1.69, -0.1) (Fig S2c, S3c). The effect was mainly attributable to MRT (MD: -1.74; 95% CrI: -3.34, -0.56; SUCRA = 99.18%) instead of MVRT (Fig. 2c).
There were no differences in subgroup analysis on TUG among all interventions done on women, men, the low muscle mass group, and the sarcopenic obesity group.
Short physical performance battery (SPPB)
We included 391 (placebo), 29 (RT), 16 (AT + RT), 289 (nutrition), 73 (AT + nutrition), 51 (RT + nutrition), 66 (MK-0773), and 12 (oxytocin) older adults for comparison (Table 1). No significant differences were found among all interventions in all participants (Fig S2d, S3d), MVRT group (Fig. 2d) and women.
Gait speed
A total of 227 participants in the RT group, 81 participants in the AT + RT group, 465 participants in the nutritional intervention group, 62 participants in the RT + nutrition group, 36 participants in the AT + RT + nutrition group, 106 participants in the whole body EMS group, 24 participants in the Taichi group, 115 participants in the Bimagrumab group, 25 participants in the whole body EMS + nutrition group, 66 participants in the MK-0773 group, and 794 participants in the placebo group were included for comparison (Table 1). RT + nutrition increased GS with a MD of 0.17 (95% CrI: 0.01, 0.34) (SUCRA = 85.6%) (Fig S2e, S3e). Regarding RT intensity, MVRT + nutrition was associated with improvement in GS (MD:0.21; 95% CrI: 0.003, 0.48; SUCRA = 84.87%), but LMRT and MRT produced no significant differences (Fig. 2e).
There was no improvement on GS among all interventions in women, those with dynapenia, and those with sarcopenic obesity.
Six min walk test
We included 27 adults from the RT group, 65 adults from the AT + RT group, 33 adults from the nutrition group, 15 adults from the RT + nutrition group, 36 adults from the AT + RT + nutrition group, 115 adults from the Bimagrumab group, and 182 adults from the placebo group for analysis (Table 1). No significant differences were found in each group compared to placebo (Fig S2f, S3f). There were also no significant effects of any interventions in the MVRT group (Fig. 2f).
Muscle mass
Appendicular skeletal muscle index (ASMI)
Twenty-four adults in the AT group, 305 adults in the RT group, 127 adults in the AT + RT group, 271 adults in the nutrition group, 175 adults in the RT + nutrition group, 95 adults in the AT + RT + nutrition group, 25 adults in the Whole body EMS group, 23 adults in the electrical acupuncture group, 58 adults in the whole body EMS + nutrition group, and 608 adults in the placebo group were compared (Table 1). RT + nutrition (MD:0.24; 95% CrI: 0.1, 0.38; SUCRA = 78.67%), RT (MD:0.19; 95% CrI: 0.08, 0.3; SUCRA = 65.74%), and nutrition (MD:0.15; 95% CrI: 0.04, 0.26; SUCRA = 53.49%) significantly increased ASMI (Fig S2g, S3g). Although LMRT and MRT were not associated with changes in ASMI, MVRT + nutrition was positively associated with increased ASMI (MD:0.25; 95% CrI: 0.01, 0.5; SUCRA = 68.21%) (Fig. 3a).
None of the interventions influenced ASMI in men, women, low muscle mass group, and sarcopenic obesity group.
Leg muscle mass
A total of 97 participants in the RT group, 40 participants in the AT + RT group, 142 participants in the nutrition group, 90 participants in the RT + nutrition group, 36 participants in the whole body EMS group, and 272 participants in the placebo group were included for comparing leg muscle mass (Table 1). No significant differences were found in each pairwise comparison with placebo among all participants and the MVRT group (Fig S2h, S3h, and Fig. 3b).
Skeletal muscle mass
Studies with skeletal muscle mass as an outcome included 24 participants in the AT group, 298 participants in the RT group, 122 participants in the AT + RT group, 280 participants in the nutrition group, 243 participants in the RT + nutrition group, 59 participants in the AT + RT + nutrition group, 61 participants in the whole body EMS group, 24 participants in the Taichi group, 115 participants in the Bimagrumab group, 65 participants in the MK-0773 group, 12 participants in the oxytocin group, and 655 participants in the placebo group (Table 1). Bimagruab (MD:1.94; 95% CrI: 0.81, 3.07; SUCRA = 91.21%), MK-0773 (MD:1.37; 95% CrI: 0.37, 2.40; SUCRA = 79.58%), RT + nutrition (MD:0.82; 95% CrI: 0.31, 1.32; SUCRA = 57.05%), RT (MD:0.58; 95% CrI: 0.11, 1.04; SUCRA = 41.72%), and nutrition (MD:0.51; 95% CrI: 0.06, 0.97; SUCRA = 36.73%) increased skeletal muscle mass significantly (Fig S2i, S3i). However, LMRT, MRT, and MVRT were not associated with enhanced skeletal muscle mass (Fig. 3c).
Muscle strength
Handgrip strength
We included 43 older adults in the AT group, 267 older adults in the RT group, 152 older adults in the AT + RT group, 553 older adults in the nutrition group, 73 older adults in the AT + nutrition group, 172 older adults in the RT + nutrition group, 95 older adults in the AT + RT + nutrition group, 53 older adults in the whole body EMS group, 24 older adults in the Taichi group, 58 older adults in the whole body EMS + nutrition group, and 1,063 older adults in the placebo group for comparison (Table 1). AT + RT + nutrition (MD:3.25; 95% CrI: 1.12, 5.4; SUCRA = 87.12%), AT + RT(MD:2.43; 95% CrI: 0.69, 4.11; SUCRA = 87.12%), RT + nutrition (MD:2.48; 95% CrI: 0.98, 4; SUCRA = 73.27%), AT + RT (MD:2.43; 95% CrI: 0.69, 4.11; SUCRA = 70.45%), RT (MD:2.21; 95% CrI: 1.18, 3.34; SUCRA = 66%), and nutrition (MD:1.73; 95% CrI: 0.76, 2.74; SUCRA = 50.33%) significantly improved handgrip strength (Fig S2j, S3j).
For RT intensity, AT + LMRT + nutrition (MD:2.88; 95% CrI: 0.43, 5.32; SUCRA = 93.01%) and MRT (MD:2.44; 95% CrI: 0.03, 5.70; SUCRA = 77.87%) were positively associated with gains in HG (Fig. 4a), whereas MVRT was not associated with changes in HG.
For women, RT was associated with HG improvement (MD:1.97; 95% CrI: 0.2, 4.12; SUCRA = 62.5%). There was no influence on HG among all interventions in men, low muscle mass group, and sarcopenic obesity group.
Chest press
A total of 24 adults in the RT group, 17 adults in the nutrition group, 36 adults in the RT + nutrition group, and 29 adults in the placebo group were included for comparing changes in chest press strength (Table 1). No significant differences among interventions were found in all participants and the MVRT group (Fig S2k, S3k, Fig. 4b).
Leg press
Studies examining leg press strength included a total of 43 older adults in the AT group, 267 older adults in the RT group, 152 older adults in the AT + RT group, 553 older adults in the nutrition group, 73 older adults in the AT + nutrition group, 172 older adults in the RT + nutrition group, 36 older adults in the RT + nutrition group, 95 older adults in the AT + RT + nutrition group, 53 older adults in the whole body EMS group, 24 older adults in the Taichi group, 58 older adults in the whole body EMS + nutrition group, and 1,063 older adults in the placebo group (Table 1). RT + nutrition (MD:12.3; 95% CrI: 5.59, 18.9; SUCRA = 88.33%) and RT (MD:8.24; 95% CrI: 3.78, 12.7; SUCRA = 70.81%) were significantly associated with gains in leg press strength (Fig S2l, S3l).
With respect to RT intensity, MRT (MD:8.36; 95% CrI: 1.87, 13.4; SUCRA = 80.5%) was positively associated with improvements in leg press strength. MVRT (MD:14.7; 95% CrI: 5.96, 22.4; SUCRA = 77.59%) and MVRT + nutrition (MD:17.8; 95% CrI: 7.55, 28.6; SUCRA = 89.71%) demonstrated even greater benefits in leg press strength (Fig. 4c). There was no influence on leg press among all interventions in subgroup analysis of men, women, and sarcopenic obesity group.
Quality of life
In total, 19 participants in the AT group, 34 participants in the RT group, 33 participants in the nutrition group, and 76 participants in the placebo group were included for comparing overall QOL. For comparing physical QOL, we examined 75 participants in the AT group, 67 participants in the RT group, 40 participants in the AT + RT group, 63 participants in the nutrition group, 74 participants in the AT + nutrition group, 69 participants in the RT + nutrition group, 36 participants in the AT + RT + nutrition group, and 215 participants in the placebo group. Additionally, 40 participants in the AT + RT group, 63 participants in the nutrition group, 69 participants in the RT + nutrition group, 36 participants in the AT + RT + nutrition group, and 159 participants in the placebo group were compared for psychological QOL (Table 1). No significant differences among interventions were found in all participants and the MVRT group (Fig S2m, S3m, Fig. 5).
Sensitivity analysis
When reanalyzing data with the sequential exclusion of each study, the results remained consistent with the original analysis. Additionally, after excluding four studies that were assessed to have a high risk of bias assessed using ROB2 [35, 44, 69, 70], the rankings remained unchanged. Node-splitting model showed no inconsistency between direct and indirect comparisons (Table S3a-S3j). Egger’s test revealed no obvious publication bias except in studies involving leg muscle mass, HG, leg press, and QOL (Table S4). After removing a study done on patients with Alzheimer’s disease [73], the intervention effects were consistent except that RT + nutrition lost its significant effect on GS and HG, whereas whole body EMS + nutrition lost its significant effect on HG. After removing two studies involving post-operative patients [74, 75], the results were consistent except that RT + nutrition lost its significant effect on GS and HG, and whole body EMS + nutrition lost its significant effect on HG.
Discussion
For community-dwelling older adults with sarcopenia, our systematic review and network meta-analysis confirmed that a combination of exercise and nutrition were associated with improved sarcopenia parameters, including 5TSTS, 30-s chair stand test (repetitions), TUG, GS, ASMI, skeletal muscle mass, HG, and leg press. Regarding RT intensity, LMRT only demonstrated desired effects on HG. MRT provided improvements in the 30-s chair stand test, TUG, HG, and leg press. MVRT had additional benefits on the 30-s chair stand test, GS, ASMI, and leg press.
Our study is the first network meta-analysis to investigate exercise effects on patients with sarcopenia according to RT intensity. The results revealed that boosting RT intensity to the moderate-vigorous level had significantly greater positive effects on physical function, lower body strength, and muscle mass. RT has been proven to be essential for the management of sarcopenia because it preferentially increases the cross-sectional area of type II muscle fibers that are replaced by slow type I muscle fibers and fatty tissue during the aging process [84,85,86,87]. Additionally, research has shown that adaptive responses including increasing myofibrillar protein synthesis, satellite cell count, myonuclei count, glycolytic function, mitochondrial volume, and mitochondrial protein synthesis in skeletal muscle occur following RT [88]. More importantly, relative RT intensity (%1RM) was associated with 18–35% of the variance for the muscle hypertrophy response [89]. More type II muscle units and associated muscle fibers were recruited with higher RT intensity in a dose–response manner, resulting in larger muscle size and greater force [90]. Therefore, with appropriate instruction and supervision before, during, and after exercise, moderate-to-vigorous RT intensity may be suggested for older adults with sarcopenia [11].
Surprisingly, MVRT was not associated with additional benefits compared to MRT in terms of TUG, which is a measure of overall functional mobility, including locomotion, static balance, and dynamic balance. Most MVRT trials increased intensity by elevating %1RM, but used the original exercise type, such as body weight workout and elastic band exercise, which mainly build limb strength. To improve agility and balance, power resistance training may provide benefits in addition to muscle power and physical performance. A 12-week RCT reported that high-speed RT program may bring greater improvement in walking sprint, 8-foot up-and-go test, and sit-to-stand test [91]. Another randomized within-subject trial demonstrated that power resistance training generated more increases in muscle power and movement velocity [92]. Considering the significance of rate-dependent mobility for fall prevention and functional maintenance in older adults [93, 94], velocity-based power training should be introduced and integrated into traditional RT programs.
According to our results, MVRT was not associated with greater gains in HG compared to MRT. Similarly, most MVRT programs tended to focus on reinforcing lower limb strength because gait and balance were more pertinent to all-cause mortality, activities of daily living (ADL) decline, and instrumental activities of daily living (IADL) worsening [95, 96]. Compared to gait and balance, HG has been proven to be equivalently essential in the concept of intrinsic capacity developed by the WHO [97]. In addition, grip strength was related to cognitive performance, mental health, and quality of life cross-sectionally and longitudinally [98], and grip training has been reported to improve cognitive function through increasing the local efficiency of brain white matter connectivity in minor acute ischemic stroke patients [99]. Because most RT programs target large muscle groups (e.g., chest press and squat), training focusing on handgrip strength, like the lateral pulldown and reverse fly, may be incorporated when intensifying exercise is warranted.
Management of sarcopenia based on strong evidence of treatment effectiveness is required. Our findings suggest that adding nutritional support to exercise interventions can amplify the effects on sarcopenia. Specifically, when nutrition is combined with RT, the improvements in outcome measures, such as HG and leg press, are more pronounced than with RT alone. Although electrical muscle stimulation, electrical acupuncture, whole body vibration, and Taichi have been introduced to manage sarcopenia, our pooled analysis showed no promising evidence of these interventions having favorable effects on sarcopenia parameters [9]. Novel agents such as bimagrumab (human monoclonal antibody targeting activin type 2 receptors) [100] and MK0733 (selective androgen receptor modulator) [36] have the potential to improve skeletal muscle mass, but our results show no benefit on muscle function and physical performance. Recent studies suggested that dysfunctions at the neuromuscular junction and within mitochondria may contribute to the deterioration of muscle function [101]. Engaging in physical activity has the potential to modify gene expression of acetylcholine receptor subunits and optimize mitochondrial dynamics, including fusion, fission, and autophagy, thereby supporting muscle function and preserving muscle strength [102]. Notably, sarcopenic patients with low muscle strength may benefit more from exercise interventions than those without strength deficits [103].
Future clinical trials are encouraged to investigate the impact of exercise intensity on sarcopenia outcomes, focusing on patients with low muscle strength and those with severe sarcopenia, characterized by reduced muscle mass, compromised physical performance, and diminished strength.
The strength of our study is the robust evidence from the network meta-analysis of currently available clinical trials. Indirect comparison allows for estimation of intervention effects even if there are no head-to-head trials. Similar results among direct and indirect comparisons reinforce and support our conclusions. However, this study also has several limitations. First, inconsistent sarcopenia criteria among studies compromised the generalizability of the findings. Second, heterogenous interventional protocols of exercise (e.g., exercise type, intensity, duration, and frequency) and diverse nutritional support might make clinical application difficult. Lack of detailed information about exercise protocols in some studies might lead to misclassification bias. Universal reporting of exercise interventions with FITT-VP (frequency, intensity, time, type, volume, and progression) information should be encouraged in future studies [11]. Third, many studies have failed to report on exercise adherence, potentially leading to an underestimation of the true effects of exercise interventions. Fourth, discordant advice on usual diet habits, lifestyle, and physical activity in control groups among studies might obscure the intervention effects.
Fifth, given the variety of metrics used to evaluate exercise, comparing results across different studies can be challenging. The ACSM recommends a holistic approach to evaluating exercise intensity, encompassing metrics such as 1-RM, VO2 max, and RPE. This approach offers both an objective measure and a subjective assessment of effort, streamlining the standardization of exercise intensity across various studies [11]. Detailed reporting on exercise intervention protocols should be emphasized in future studies.
Conclusions
This network meta-analysis suggests that RT with or without nutritional supplementation improves physical performance, ASMI, and handgrip strength in older adults suffering from sarcopenia. Higher RT intensity potentially generates more benefits on lower body strength and muscle mass compared to lower RT intensity. Further investigation is necessary to clarify the advantages and disadvantages of intensifying RT and give insight to future exercise program modifications.
Availability of data and materials
The datasets used and/or during the current study are available from the corresponding author on reasonable request.
References
Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. 2019;393(10191):2636–46.
Yeung SSY, Reijnierse EM, Pham VK, Trappenburg MC, Lim WK, Meskers CGM, Maier AB. Sarcopenia and its association with falls and fractures in older adults: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle. 2019;10(3):485–500.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(4):601.
Mayhew AJ, Amog K, Phillips S, Parise G, McNicholas PD, de Souza RJ, Thabane L, Raina P. The prevalence of sarcopenia in community-dwelling older adults, an exploration of differences between studies and within definitions: a systematic review and meta-analyses. Age Ageing. 2019;48(1):48–56.
Coll PP, Phu S, Hajjar SH, Kirk B, Duque G, Taxel P. The prevention of osteoporosis and sarcopenia in older adults. J Am Geriatr Soc. 2021;69(5):1388–98.
Dent E, Morley JE, Cruz-Jentoft AJ, Arai H, Kritchevsky SB, Guralnik J, Bauer JM, Pahor M, Clark BC, Cesari M, et al. International Clinical Practice Guidelines for Sarcopenia (ICFSR): Screening, Diagnosis and Management. J Nutr Health Aging. 2018;22(10):1148–61.
Beaudart C, Dawson A, Shaw SC, Harvey NC, Kanis JA, Binkley N, Reginster JY, Chapurlat R, Chan DC, Bruyere O, et al. Nutrition and physical activity in the prevention and treatment of sarcopenia: systematic review. Osteoporos Int. 2017;28(6):1817–33.
Wu PY, Huang KS, Chen KM, Chou CP, Tu YK. Exercise, nutrition, and combined exercise and nutrition in older adults with sarcopenia: a systematic review and network meta-analysis. Maturitas. 2021;145:38–48.
Lai CC, Tu YK, Wang TG, Huang YT, Chien KL. Effects of resistance training, endurance training and whole-body vibration on lean body mass, muscle strength and physical performance in older people: a systematic review and network meta-analysis. Age Ageing. 2018;47(3):367–73.
Negm AM, Lee J, Hamidian R, Jones CA, Khadaroo RG. Management of sarcopenia: a network meta-analysis of randomized controlled trials. J Am Med Dir Assoc. 2022;23(5):707–14.
Pollock ML, Gaesser GA, Butcher J, Després JP, Dishman RK, Franklin BA, Garber CE. ACSM position stand: the recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc. 1998;30(6).
Latham NK, Bennett DA, Stretton CM, Anderson CS. Systematic review of progressive resistance strength training in older adults. J Gerontol A Biol Sci Med Sci. 2004;59(1):48–61.
Peterson MD, Rhea MR, Sen A, Gordon PM. Resistance exercise for muscular strength in older adults: a meta-analysis. Ageing Res Rev. 2010;9(3):226–37.
Hupin D, Roche F, Gremeaux V, Chatard JC, Oriol M, Gaspoz JM, Barthélémy JC, Edouard P. Even a low-dose of moderate-to-vigorous physical activity reduces mortality by 22% in adults aged ≥60 years: a systematic review and meta-analysis. Br J Sports Med. 2015;49(19):1262–7.
Csapo R, Alegre LM. Effects of resistance training with moderate vs heavy loads on muscle mass and strength in the elderly: a meta-analysis. Scand J Med Sci Sports. 2016;26(9):995–1006.
Perri MG, Anton SD, Durning PE, Ketterson TU, Sydeman SJ, Berlant NE, Kanasky WF Jr, Newton RL Jr, Limacher MC, Martin AD. Adherence to exercise prescriptions: effects of prescribing moderate versus higher levels of intensity and frequency. Health Psychol. 2002;21(5):452–8.
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, Ioannidis JP, Straus S, Thorlund K, Jansen JP, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–84.
Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, Jang HC, Kang L, Kim M, Kim S, et al. Asian working group for sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020;21(3):300-307 e302.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16–31.
Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA. Assessing risk of bias in a randomized trial. Cochrane handbook for systematic reviews of interventions. 2019:205–228.
Haff GG, Triplett NT. Essentials of strength training and conditioning 4th edition: Human kinetics. 2015.
Chen MJ, Fan X, Moe ST. Criterion-related validity of the Borg ratings of perceived exertion scale in healthy individuals: a meta-analysis. J Sports Sci. 2002;20(11):873–99.
Negm AM, Lee J, Hamidian R, Jones CA, Khadaroo RG: Management of Sarcopenia: A Network Meta-analysis of Randomized Controlled Trials. Journal of the American Medical Directors Association. 2022.
Shiotsu Y, Yanagita M. Comparisons of low-intensity versus moderate-intensity combined aerobic and resistance training on body composition, muscle strength, and functional performance in older women. Menopause. 2018;25(6):668–75.
Nuzzo JL, Pinto MD, Nosaka K, Steele J: Maximal Number of Repetitions at Percentages of the One Repetition Maximum: A Meta-Regression and Moderator Analysis of Sex, Age, Training Status, and Exercise. Sports Med. 2023.
Ialongo C. Confidence interval for quantiles and percentiles. Biochem Med (Zagreb). 2019;29(1):010101.
Follmann D, Elliott P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. J Clin Epidemiol. 1992;45(7):769–73.
Shim SR, Kim SJ, Lee J, Rücker G. Network meta-analysis: application and practice using R software. Epidemiol Health. 2019;41:e2019013.
Owen RK, Bradbury N, Xin Y, Cooper N, Sutton A. MetaInsight: an interactive web-based tool for analyzing, interrogating, and visualizing network meta-analyses using R-shiny and netmeta. Research Synthesis Methods. 2019;10(4):569–81.
Hu D, O’Connor AM, Wang C, Sargeant JM, Winder CB. How to Conduct a Bayesian Network Meta-Analysis. Front Vet Sci. 2020;7:271.
Dias S, Sutton AJ, Ades AE, Welton NJ. Evidence synthesis for decision making 2: a generalized linear modeling framework for pairwise and network meta-analysis of randomized controlled trials. Med Decis Making. 2013;33(5):607–17.
Lin L, Chu H. Quantifying publication bias in meta-analysis. Biometrics. 2018;74(3):785–94.
Higgins JP, Jackson D, Barrett JK, Lu G, Ades AE, White IR. Consistency and inconsistency in network meta-analysis: concepts and models for multi-arm studies. Res Synth Methods. 2012;3(2):98–110.
Alemán-Mateo H, Macías L, Esparza-Romero J, Astiazaran-García H, Blancas AL. Physiological effects beyond the significant gain in muscle mass in sarcopenic elderly men: evidence from a randomized clinical trial using a protein-rich food. Clin Interv Aging. 2012;7:225–34.
Bellomo RG, Iodice P, Maffulli N, Maghradze T, Coco V, Saggini R. Muscle strength and balance training in sarcopenic elderly: a pilot study with randomized controlled trial. Eur J Inflamm. 2013;11(1):193–201.
Papanicolaou DA, Ather SN, Zhu H, Zhou Y, Lutkiewicz J, Scott BB, Chandler J. A phase IIA randomized, placebo-controlled clinical trial to study the efficacy and safety of the selective androgen receptor modulator (SARM), MK-0773 in female participants with sarcopenia. J Nutr Health Aging. 2013;17(6):533–43.
Liu CK, Leng X, Hsu FC, Kritchevsky SB, Ding J, Earnest CP, Ferrucci L, Goodpaster BH, Guralnik JM, Lenchik L, et al. The impact of sarcopenia on a physical activity intervention: the Lifestyle Interventions and Independence for Elders Pilot Study (LIFE-P). J Nutr Health Aging. 2014;18(1):59–64.
Bauer JM, Verlaan S, Bautmans I, Brandt K, Donini LM, Maggio M, McMurdo ME, Mets T, Seal C, Wijers SL, et al. Effects of a vitamin D and leucine-enriched whey protein nutritional supplement on measures of sarcopenia in older adults, the PROVIDE study: a randomized, double-blind, placebo-controlled trial. J Am Med Dir Assoc. 2015;16(9):740–7.
Zdzieblik D, Oesser S, Baumstark MW, Gollhofer A, König D. Collagen peptide supplementation in combination with resistance training improves body composition and increases muscle strength in elderly sarcopenic men: a randomised controlled trial. Br J Nutr. 2015;114(8):1237–45.
Cramer JT, Cruz-Jentoft AJ, Landi F, Hickson M, Zamboni M, Pereira SL, Hustead DS, Mustad VA. Impacts of high-protein oral nutritional supplements among malnourished men and women with sarcopenia: a multicenter, randomized, double-blinded, controlled trial. J Am Med Dir Assoc. 2016;17(11):1044–55.
Kemmler W, Teschler M, Weissenfels A, Bebenek M, von Stengel S, Kohl M, Freiberger E, Goisser S, Jakob F, Sieber C, et al. Whole-body electromyostimulation to fight sarcopenic obesity in community-dwelling older women at risk. Resultsof the randomized controlled FORMOsA-sarcopenic obesity study. Osteoporos Int. 2016;27(11):3261–70.
Kim H, Kim M, Kojima N, Fujino K, Hosoi E, Kobayashi H, Somekawa S, Niki Y, Yamashiro Y, Yoshida H. Exercise and nutritional supplementation on community-dwelling elderly japanese women with sarcopenic obesity: a randomized controlled trial. J Am Med Dir Assoc. 2016;17(11):1011–9.
Maltais ML, Ladouceur JP, Dionne IJ. The effect of resistance training and different sources of postexercise protein supplementation on muscle mass and physical capacity in sarcopenic elderly men. J Strength Cond Res. 2016;30(6):1680–7.
Maltais ML, Perreault K, Courchesne-Loyer A, Lagacé JC, Barsalani R, Dionne IJ. Effect of resistance training and various sources of protein supplementation on body fat mass and metabolic profile in sarcopenic overweight older adult men: a pilot study. Int J Sport Nutr Exerc Metab. 2016;26(1):71–7.
Maruya K, Asakawa Y, Ishibashi H, Fujita H, Arai T, Yamaguchi H. Effect of a simple and adherent home exercise program on the physical function of community dwelling adults sixty years of age and older with pre-sarcopenia or sarcopenia. J Phys Ther Sci. 2016;28(11):3183–8.
Rondanelli M, Klersy C, Terracol G, Talluri J, Maugeri R, Guido D, Faliva MA, Solerte BS, Fioravanti M, Lukaski H, et al. Whey protein, amino acids, and vitamin D supplementation with physical activity increases fat-free mass and strength, functionality, and quality of life and decreases inflammation in sarcopenic elderly. Am J Clin Nutr. 2016;103(3):830–40.
Vasconcelos KS, Dias JM, Araújo MC, Pinheiro AC, Moreira BS, Dias RC. Effects of a progressive resistance exercise program with high-speed component on the physical function of older women with sarcopenic obesity: a randomized controlled trial. Braz J Phys Ther. 2016;20(5):432–40.
Chen HT, Chung YC, Chen YJ, Ho SY, Wu HJ. Effects of different types of exercise on body composition, muscle strength, and IGF-1 in the elderly with sarcopenic obesity. J Am Geriatr Soc. 2017;65(4):827–32.
Huang SW, Ku JW, Lin LF, Liao CD, Chou LC, Liou TH. Body composition influenced by progressive elastic band resistance exercise of sarcopenic obesity elderly women: a pilot randomized controlled trial. Eur J Phys Rehabil Med. 2017;53(4):556–63.
Kemmler W, Weissenfels A, Teschler M, Willert S, Bebenek M, Shojaa M, Kohl M, Freiberger E, Sieber C, von Stengel S. Whole-body electromyostimulation and protein supplementation favorably affect sarcopenic obesity in community-dwelling older men at risk: the randomized controlled FranSO study. Clin Interv Aging. 2017;12:1503–13.
Liao CD, Tsauo JY, Lin LF, Huang SW, Ku JW, Chou LC, Liou TH. Effects of elastic resistance exercise on body composition and physical capacity in older women with sarcopenic obesity: a CONSORT-compliant prospective randomized controlled trial. Medicine (Baltimore). 2017;96(23):e7115.
Park J, Kwon Y, Park H. Effects of 24-week aerobic and resistance training on carotid artery intima-media thickness and flow velocity in elderly women with sarcopenic obesity. J Atheroscler Thromb. 2017;24(11):1117–24.
Sammarco R, Marra M, Di Guglielmo ML, Naccarato M, Contaldo F, Poggiogalle E, Donini LM, Pasanisi F. Evaluation of hypocaloric diet with protein supplementation in middle-aged sarcopenic obese women: a pilot study. Obes Facts. 2017;10(3):160–7.
Wei N, Pang MY, Ng SS, Ng GY. Optimal frequency/time combination of whole-body vibration training for improving muscle size and strength of people with age-related muscle loss (sarcopenia): a randomized controlled trial. Geriatr Gerontol Int. 2017;17(10):1412–20.
Wei N, Pang MY, Ng SS, Ng GY. Optimal frequency/time combination of whole body vibration training for developing physical performance of people with sarcopenia: a randomized controlled trial. Clin Rehabil. 2017;31(10):1313–21.
von Berens Å, Fielding RA, Gustafsson T, Kirn D, Laussen J, Nydahl M, Reid K, Travison TG, Zhu H, Cederholm T, et al. Effect of exercise and nutritional supplementation on health-related quality of life and mood in older adults: the VIVE2 randomized controlled trial. BMC Geriatr. 2018;18(1):286.
Chen HT, Wu HJ, Chen YJ, Ho SY, Chung YC. Effects of 8-week kettlebell training on body composition, muscle strength, pulmonary function, and chronic low-grade inflammation in elderly women with sarcopenia. Exp Gerontol. 2018;112:112–8.
Kemmler W, Grimm A, Bebenek M, Kohl M, von Stengel S. Effects of Combined Whole-Body Electromyostimulation and Protein Supplementation on Local and Overall Muscle/Fat Distribution in Older Men with Sarcopenic Obesity: The Randomized Controlled Franconia Sarcopenic Obesity (FranSO) Study. Calcif Tissue Int. 2018;103(3):266–77.
Liao CD, Tsauo JY, Huang SW, Ku JW, Hsiao DJ, Liou TH. Effects of elastic band exercise on lean mass and physical capacity in older women with sarcopenic obesity: a randomized controlled trial. Sci Rep. 2018;8(1):2317.
Piastra G, Perasso L, Lucarini S, Monacelli F, Bisio A, Ferrando V, Gallamini M, Faelli E, Ruggeri P. Effects of two types of 9-month adapted physical activity program on muscle mass, muscle strength, and balance in moderate sarcopenic older women. Biomed Res Int. 2018;2018:5095673.
Tsekoura M, Billis E, Tsepis E, Dimitriadis Z, Matzaroglou C, Tyllianakis M, Panagiotopoulos E, Gliatis J: The effects of group and home-based exercise programs in elderly with sarcopenia: a randomized controlled trial. J Clin Med. 2018;7(12).
Zhou X, Xing B, He G, Lyu X, Zeng Y. The effects of electrical acupuncture and essential amino acid supplementation on sarcopenic obesity in male older adults: a randomized control study. Obes Facts. 2018;11(4):327–34.
Amasene M, Besga A, Echeverria I, Urquiza M, Ruiz JR, Rodriguez-Larrad A, Aldamiz M, Anaut P, Irazusta J, Labayen I. Effects of leucine-enriched whey protein supplementation on physical function in post-hospitalized older adults participating in 12-Weeks of resistance training program: a randomized controlled trial. Nutrients. 2019;11(10).
Bo Y, Liu C, Ji Z, Yang R, An Q, Zhang X, You J, Duan D, Sun Y, Zhu Y, et al. A high whey protein, vitamin D and E supplement preserves muscle mass, strength, and quality of life in sarcopenic older adults: a double-blind randomized controlled trial. Clin Nutr. 2019;38(1):159–64.
Mafi F, Biglari S, Ghardashi Afousi A, Gaeini AA. Improvement in Skeletal Muscle Strength and Plasma Levels of Follistatin and Myostatin Induced by an 8-Week Resistance Training and Epicatechin Supplementation in Sarcopenic Older Adults. J Aging Phys Act. 2019;27(3):384–91.
Nabuco HCG, Tomeleri CM, Fernandes RR, Sugihara Junior P, Cavalcante EF, Cunha PM, Antunes M, Nunes JP, Venturini D, Barbosa DS, et al. Effect of whey protein supplementation combined with resistance training on body composition, muscular strength, functional capacity, and plasma-metabolism biomarkers in older women with sarcopenic obesity: A randomized, double-blind, placebo-controlled trial. Clin Nutr ESPEN. 2019;32:88–95.
Vikberg S, Sörlén N, Brandén L, Johansson J, Nordström A, Hult A, Nordström P. Effects of resistance training on functional strength and muscle mass in 70-year-old individuals with pre-sarcopenia: a randomized controlled trial. J Am Med Dir Assoc. 2019;20(1):28–34.
Yamada M, Kimura Y, Ishiyama D, Nishio N, Otobe Y, Tanaka T, Ohji S, Koyama S, Sato A, Suzuki M, et al. Synergistic effect of bodyweight resistance exercise and protein supplementation on skeletal muscle in sarcopenic or dynapenic older adults. Geriatr Gerontol Int. 2019;19(5):429–37.
Zhu LY, Chan R, Kwok T, Cheng KC, Ha A, Woo J. Effects of exercise and nutrition supplementation in community-dwelling older Chinese people with sarcopenia: a randomized controlled trial. Age Ageing. 2019;48(2):220–8.
Zhu YQ, Peng N, Zhou M, Liu PP, Qi XL, Wang N, Wang G, Wu ZP. Tai Chi and whole-body vibrating therapy in sarcopenic men in advanced old age: a clinical randomized controlled trial. Eur J Ageing. 2019;16(3):273–82.
Bagheri R, Moghadam BH, Church DD, Tinsley GM, Eskandari M, Moghadam BH, Motevalli MS, Baker JS, Robergs RA, Wong A. The effects of concurrent training order on body composition and serum concentrations of follistatin, myostatin and GDF11 in sarcopenic elderly men. Exp Gerontol. 2020;133:110869.
Björkman MP, Suominen MH, Kautiainen H, Jyväkorpi SK, Finne-Soveri HU, Strandberg TE, Pitkälä KH, Tilvis RS. Effect of protein supplementation on physical performance in older people with sarcopenia-a randomized controlled trial. J Am Med Dir Assoc. 2020;21(2):226-232.e221.
Chang MC, Lee AY, Kwak S, Kwak SG. Effect of Resistance Exercise on Depression in Mild Alzheimer Disease Patients With Sarcopenia. Am J Geriatr Psychiatry. 2020;28(5):587–9.
Liao CD, Chiu YS, Ku JW, Huang SW, Liou TH. Effects of elastic resistance exercise on postoperative outcomes linked to the ICF core sets for osteoarthritis after total knee replacement in overweight and obese older women with sarcopenia risk: a randomized controlled trial. J Clin Med. 2020;9(7).
Oh MK, Yoo JI, Byun H, Chun SW, Lim SK, Jang YJ, Lee CH. Efficacy of combined antigravity treadmill and conventional rehabilitation after hip fracture in patients with sarcopenia. J Gerontol A Biol Sci Med Sci. 2020;75(10):e173–81.
Rooks D, Swan T, Goswami B, Filosa LA, Bunte O, Panchaud N, Coleman LA, Miller RR, Garcia Garayoa E, Praestgaard J, et al. Bimagrumab vs optimized standard of care for treatment of sarcopenia in community-dwelling older adults: a randomized clinical trial. JAMA Netw Open. 2020;3(10):e2020836.
Espinoza SE, Lee JL, Wang CP, Ganapathy V, MacCarthy D, Pascucci C, Musi N, Volpi E. Intranasal oxytocin improves lean muscle mass and lowers LDL cholesterol in older adults with sarcopenic obesity: a pilot randomized controlled trial. J Am Med Dir Assoc. 2021;22(9):1877-1882.e1872.
Lee YH, Lee PH, Lin LF, Liao CD, Liou TH, Huang SW. Effects of progressive elastic band resistance exercise for aged osteosarcopenic adiposity women. Exp Gerontol. 2021;147:111272.
Li Z, Cui M, Yu K, Zhang XW, Li CW, Nie XD, Wang F. Effects of nutrition supplementation and physical exercise on muscle mass, muscle strength and fat mass among sarcopenic elderly: a randomized controlled trial. Applied physiology, nutrition, and metabolism Physiologie appliquee, nutrition et metabolisme. 2021;46(5):494–500.
Nasimi N, Sohrabi Z, Dabbaghmanesh MH, Eskandari MH, Bedeltavana A, Famouri M, Talezadeh P. A novel fortified dairy product and sarcopenia measures in sarcopenic older adults: a double-blind randomized controlled trial. J Am Med Dir Assoc. 2021;22(4):809–15.
Osuka Y, Kojima N, Sasai H, Wakaba K, Miyauchi D, Tanaka K, Kim H. Effects of exercise and/or β-hydroxy-β-methylbutyrate supplementation on muscle mass, muscle strength, and physical performance in older women with low muscle mass: a randomized, double-blind, placebo-controlled trial. Am J Clin Nutr. 2021;114(4):1371–85.
Seo MW, Jung SW, Kim SW, Lee JM, Jung HC, Song JK. Effects of 16 weeks of resistance training on muscle quality and muscle growth factors in older adult women with sarcopenia: a randomized controlled trial. Int J Environ Res Public Health. 2021;18(13).
Achison M, Adamson S, Akpan A, Aspray T, Avenell A, Band MM, Bashir T, Burton LA, Cvoro V, Donnan PT, et al. Effect of perindopril or leucine on physical performance in older people with sarcopenia: the LACE randomized controlled trial. J Cachexia Sarcopenia Muscle. 2022;13(2):858–71.
von Haehling S, Morley JE, Anker SD. From muscle wasting to sarcopenia and myopenia: update 2012. J Cachexia Sarcopenia Muscle. 2012;3(4):213–7.
Yoo SZ, No MH, Heo JW, Park DH, Kang JH, Kim SH, Kwak HB. Role of exercise in age-related sarcopenia. J Exerc Rehabil. 2018;14(4):551–8.
Tanganelli F, Meinke P, Hofmeister F, Jarmusch S, Baber L, Mehaffey S, Hintze S, Ferrari U, Neuerburg C, Kammerlander C, et al. Type-2 muscle fiber atrophy is associated with sarcopenia in elderly men with hip fracture. Exp Gerontol. 2021;144:111171.
Nilwik R, Snijders T, Leenders M, Groen BB, van Kranenburg J, Verdijk LB, van Loon LJ. The decline in skeletal muscle mass with aging is mainly attributed to a reduction in type II muscle fiber size. Exp Gerontol. 2013;48(5):492–8.
Qaisar R, Bhaskaran S, Van Remmen H. Muscle fiber type diversification during exercise and regeneration. Free Radic Biol Med. 2016;98:56–67.
Fry AC. The role of resistance exercise intensity on muscle fibre adaptations. Sports Med. 2004;34(10):663–79.
Kraemer W, Looney D. Underlying Mechanisms and Physiology of Muscular Power. Strength and Conditioning Journal. 2012;34:13–9.
Ramírez-Campillo R, Castillo A, de la Fuente CI, Campos-Jara C, Andrade DC, Álvarez C, Martínez C, Castro-Sepúlveda M, Pereira A, Marques MC, et al. High-speed resistance training is more effective than low-speed resistance training to increase functional capacity and muscle performance in older women. Exp Gerontol. 2014;58:51–7.
Rodriguez-Lopez C, Alcazar J, Sanchez-Martin C, Baltasar-Fernandez I, Ara I, Csapo R, Alegre LM. Neuromuscular adaptations after 12 weeks of light- vs. heavy-load power-oriented resistance training in older adults. Scand J Med Sci Sports. 2022;32(2):324–37.
Bellumori M, Uygur M, Knight CA. High-Speed Cycling Intervention Improves Rate-Dependent Mobility in Older Adults. Med Sci Sports Exerc. 2017;49(1):106–14.
Bohrer RCD, Pereira G, Beck JK, Lodovico A, Rodacki ALF. Multicomponent training program with high-speed movement execution of ankle muscles reduces risk of falls in older adults. Rejuvenation Res. 2019;22(1):43–50.
Grgic J, Garofolini A, Orazem J, Sabol F, Schoenfeld BJ, Pedisic Z. Effects of resistance training on muscle size and strength in very elderly adults: a systematic review and meta-analysis of randomized controlled trials. Sports Med. 2020;50(11):1983–99.
Liu B, Hu X, Zhang Q, Fan Y, Li J, Zou R, Zhang M, Wang X, Wang J. Usual walking speed and all-cause mortality risk in older people: a systematic review and meta-analysis. Gait Posture. 2016;44:172–7.
Beard JR, Jotheeswaran AT, Cesari M. Araujo de Carvalho I: the structure and predictive value of intrinsic capacity in a longitudinal study of ageing. BMJ Open. 2019;9(11):e026119.
Jiang R, Westwater ML, Noble S, Rosenblatt M, Dai W, Qi S, Sui J, Calhoun VD, Scheinost D. Associations between grip strength, brain structure, and mental health in > 40,000 participants from the UK Biobank. BMC Med. 2022;20(1):286.
Shang X, Meng X, Xiao X, Xie Z, Yuan X. Grip training improves handgrip strength, cognition, and brain white matter in minor acute ischemic stroke patients. Clin Neurol Neurosurg. 2021;209:106886.
Hofbauer LC, Witvrouw R, Varga Z, Shiota N, Cremer M, Tanko LB, Rooks D, Auberson LZ, Arkuszewski M, Fretault N, et al. Bimagrumab to improve recovery after hip fracture in older adults: a multicentre, double-blind, randomised, parallel-group, placebo-controlled, phase 2a/b trial. The Lancet Healthy Longevity. 2021;2(5):e263–74.
Deschenes MR, Oh J, Tufts H: Chapter 2 - The role of the neuromuscular junction in sarcopenia. In: Sarcopenia. Edited by Sakuma K: Elsevier; 2021: 59–80.
Soendenbroe C, Bechshøft CJL, Heisterberg MF, Jensen SM, Bomme E, Schjerling P, Karlsen A, Kjaer M, Andersen JL, Mackey AL. Key Components of Human Myofibre Denervation and Neuromuscular Junction Stability are Modulated by Age and Exercise. Cells. 2020;9(4).
Distefano G, Goodpaster BH. Effects of exercise and aging on skeletal muscle. Cold Spring Harb Perspect Med. 2018;8(3).
Acknowledgements
None.
Funding
This work was supported by the E-DA Hospital (grant number EDAHS111026 and EDAHS112024) and National Science and Technology Council, Taiwan (grant number NSTC 112-2314-B-650 -001 -MY3, EDAHJ112009).
Author information
Authors and Affiliations
Contributions
CHH, YCC and WCC originally conceived and designed the study. CHH, YCC, WCC, CWL, and WYH acquired the data and screened records. CHH, YCC, and WCC extracted, analyzed and interpreted the data. CHH, YCC, and CWL were major contributors in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was registered in PROSPERO under the ID CRD42021287114.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, Y.C., Chen, WC., Liu, CW. et al. Is moderate resistance training adequate for older adults with sarcopenia? A systematic review and network meta-analysis of RCTs. Eur Rev Aging Phys Act 20, 22 (2023). https://doi.org/10.1186/s11556-023-00333-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s11556-023-00333-4