Abstract
Background
Aging leads to a number of structural and physiological deficits such as loss of muscle mass and strength. Strength training at ~ 70% of 1 repetition max (RM) is recommended to prevent age-related loss of muscle mass and strength. However, most older adults may not be able to perform 70% of 1RM or higher intensity. An alternative exercise training program combining low intensity resistance exercise with blood flow restriction (BFR) can result in similar acute and chronic benefits to skeletal muscles in older adults.
Main body and short conclusion
The potential mechanisms involved are discussed, and include reactive hyperaemia, metabolic stress, and hypoxia. Key issues and safety with the use of BFR in older adults, especially those with chronic conditions are also discussed. Although there has been no reported evidence to suggest that BFR elevates the risk of clinical complications any more than high intensity exercise, it is recommended for individuals to be medically cleared of any cardiovascular risks, prior to engaging in BFR exercise.
Similar content being viewed by others
Background
Aging is characterised by a number of structural and physiological deficits, for instance, increased arterial stiffness leads to decreased vascular compliance [1] and elevates the risk for developing cardiovascular and metabolic disease. Furthermore, significant loss in skeletal muscle mass and strength starts around the 4th decade in life [2] and accelerates thereafter in men and women [3]. Age-related loss of muscle mass (sarcopenia) and strength contributes to functional decline, thereby increasing the prevalence of frailty, disability, falls and mortality in older adults [4, 5]. The estimated global prevalence of sarcopenia (ranged from 10 to 27%, depending on definition used) [6], imposes significant challenges on the global healthcare systems [7,8,9]. As recommended by the sarcopenia committees around the world, exercise is beneficial to prevent/reduce sarcopenia. It is important for the older population to exercise, to maintain skeletal muscle mass [10, 11].
The American College of Sports Medicine (ACSM) recommends strength training to prevent age-related loss of muscle mass and strength, with prescribed intensities ranging from loads of 65 to 75% of 1 repetition max (RM) for older adults [12]. Several studies have shown that exercising at intensities above 70% of 1RM improves muscle size and strength in older adults [13, 14]. Performing resistance exercise above 70% of 1RM also stimulated muscle protein synthesis, satellite cell activity, and decreased proteolysis when compared with low-intensity resistance exercise [15, 16].
Muscle hypertrophy can be achieved by manipulating exercise intensity (load, repetitions), duration, or both. Some investigators have suggested that the training load may be redundant; exercising to failure with low (~ 30% 1RM) or high loads (~ 80% 1 RM) resulted in similar rates of muscle hypertrophy [17, 18]. A disadvantage in using low loads (~ 30% 1RM) is the longer duration required to reach muscular fatigue. To economize exercise time, it may be prudent to increase the intensity of exercise. Resistance training with heavier loads is necessary to maximize the development of muscle mass and strength [13, 19].
High-intensity resistance exercise stimulates the molecular pathways that regulate protein synthesis/hypertrophy. Skeletal muscle from young adults performing high-intensity resistance exercise (70% 1RM) showed an activation of the mammalian target of rapamycin (mTOR) signalling pathway (Fig. 1): protein kinase B (AKT); ~ 50%, mTOR; ~ 100%, ribosomal protein S6 kinase beta-1 (S6K1); ~ 150%, 4E binding protein 1 (4E-BP1); ~ 50%, extracellular signal-regulated kinase 1/2 (ERK1/2); ~ 300%, ribosomal protein S6 (S6; ~ 200%), and increased protein synthesis (~ 60%) 3 to 24 hours post-exercise [20]. However, older adults performing the same resistance exercise had reduced extent of, or did not achieve significant changes in muscle protein synthesis, or phosphorylation of intramuscular proteins in the mTOR pathway [20], suggesting that aging impairs the anabolic response to acute high-intensity resistance exercise. While inconclusive, the impaired anabolic response in older adults has been suggested to be associated with basal hyperphosphorylation of S6K1 [21] and basal mTOR complex 1 (mTORC1; Fig. 1) [22]. Partial inhibition of mTORC1, using Everolimus, a rapamycin-mimetic (rapalog), counteracted age-associated sarcopenia in aged rat models [23]. Hyperphosphorylation of these intramuscular signalling proteins could reduce AKT phosphorylation and degradation of Insulin receptor substrate 1 (IRS-1) [24]. Therefore, it is possible that chronic phosphorylation of the mTORC1/S6K1 pathway impairs the age-related anabolic response. In support of this viewpoint, it had been demonstrated that mTORC1 is hyperphosphorylated in skeletal muscles of sarcopenic rats [23].
AKT-mTOR signalling pathways in skeletal muscle for protein synthesis. Red “+” sign indicates hyperphosphorylation of protein at baseline with aging. 4E-BP1: 4E binding protein 1; AKT: protein kinase B; eEF2: Eukaryotic elongation factor 2; eIF2Bε: eukaryotic translation initiation factor 4E; ERK/MAPK: extra-cellular signal-regulated kinase; IGF-I: insulin-like growth factor 1; IRS: insulin receptor substrate; MnK1: mitogen-activated protein kinase-interacting kinase 1; mTORC1/2: mammalian target of rapamycin complex 1/2; PI3K: phosphatidylinositol-3 kinase; PIP3: phosphatidylinositol-3,4,5-triphosphate; REDD1: regulated in development and DNA damage responses 1; Rheb: ras-homolog enriched in brain; rpS6: ribosomal protein S6 (S6); S6K1; ribosomal protein S6 kinase beta-1 (p70S6 kinase 1); TSC: tuberous sclerosis complex
A possible solution to overcome the impaired anabolic response in older individuals is to increase the volume of exercise training. Doubling resistance exercise volume, by increasing from 3 to 6 sets of 40% 1RM and 75% 1RM, upregulated intramuscular protein expression (S6K1; ~ 100% and ~ 75% respectively) and muscle protein synthesis (~ 300% and ~ 100% respectively) in older adults, but was not further enhanced in young adults [25]. However, high-intensity load and increased training volume in resistance or aerobic training programs are impractical for older adults with chronic medical conditions, or in older, deconditioned adults. This is primarily because a major barrier for older adults to commit to exercise programs is the perceived time constraint [26]. Therefore, an alternative solution would be needed to recapitulate the benefits of exercise in the older adults.
An alternative exercise training method that combines blood flow restriction (BFR) with low-intensity exercise, both resistance and aerobic, can result in positive physiological adaptations akin to performing high-intensity exercise. For instance, combining BFR with low-intensity resistance training increased intramuscular signaling pathways and the rate of muscle protein synthesis in younger [27] and older adults [28], as compared with low-intensity resistance training alone. In addition, combining BFR with low-intensity exercise was as effective as high-intensity exercise in increasing muscle mass and strength [29,30,31,32].
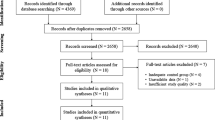
Given that there may be different mechanisms involved with the use of BFR in older adults as compared to younger adults, the purpose of this narrative review is to summarise the short- and long-term effects of combining BFR with resistance exercise on physiological and molecular responses in older adults. The adaptations and potential mechanisms with the use of BFR alone, or with exercise in older adults will be discussed in the next section. Finally, key issues and safety of the use of BFR in older adults will be discussed.
History and origin of BFR
The origins of BFR can be traced as far back as 1966, where Dr. Yoshiaki Sato’s leg became numb after sitting at a Buddhist memorial in a kneeling position [33]. He then started to massage his calf and noticed the swelling and discomfort was similar to performing calf-raise exercises [33]. Dr. Sato then experimented and eventually developed and patented the KAATSU training method [33], which combines BFR with low-intensity resistance exercise (~ 20–50% 1RM). The KAATSU method typically involves applying a tourniquet that occludes up to 200 mmHg of systolic blood pressure (SBP), while performing low-intensity resistance exercise (Table 1).
Benefits of BFR without exercise
Without incorporating exercise, BFR alone reduced disuse atrophy by 9.4% and 9.2% in knee extensors and flexors respectively, compared with control (limb immobilization) [34]. Further, BFR reduced and delayed skeletal muscle atrophy in young healthy adults immobilised with casts after injury [34,35,36], as well as in older adults with chronic disease [37]. These studies suggest that BFR-induced hypoxia and/or hyperaemic reperfusion may preserve muscle mass in age-associated sarcopenia. Apart from improving disuse atrophy, BFR was also effective in mitigating strength reduction during limb immobilisation [35, 36]. Given the paucity of studies investigating the effects of BFR in physiological responses in older adults, future studies should explore whether BFR mitigates changes in muscle strength and size differently between young adults and older adults.
Acute BFR with resistance exercise in older adults
Combining BFR with a single session of resistance exercise in older men increased phosphorylation of proteins involved in skeletal muscle anabolism (mTORC1; ~ 30%, S6K1; 300%, S6 Ser235/236; ~ 1800%, S6 Ser240/244; ~ 500%), and muscle protein synthesis (~ 56%) immediately post-exercise [28]. The concentration of anabolic hormones such as growth hormone (GH), was also increased in systemic circulation 15–30 min after combined BFR and resistance exercise, and returned to resting concentrations 45 mins post-exercise [28]. It is important to note that the increase in systemic concentrations of GH was observed post-BFR with low-intensity resistance exercise but not with low-intensity resistance exercise alone [38]. The reduced systemic GH concentrations in normal aging is associated with reduced muscle mass and strength and slower muscle protein synthesis [39]. Administration of GH in older adults increased muscle protein synthesis and muscle growth, which may be mediated through the insulin-like growth factor 1 (IGF-1) signalling pathway [40, 41]. BFR with resistance exercise also elevated other blood biomarkers such as cortisol [28], lactate [28, 42, 43] and interleukin-6 (IL-6) [38], which are related to exercise-induced metabolic stress and contribute to skeletal muscle adaptations [44, 45]. An elevation of these biomarkers in systemic circulation during a combined session of BFR with resistance exercise would suggest that this exercise mode is sufficient for skeletal muscle adaptations.
BFR with chronic resistance training in older adults
Chronic resistance exercise training improves musculoskeletal health in older adults [43]. Maintaining or enhancing skeletal muscle mass can slow the rate of functional decline with aging [46,47,48], given the strong evidence that regular participation in physical activity improves physical capacity and mobility, while reducing the risk of fall-related injuries by 32–40% in older adults [49].
In older adults, performing 3 to 12 weeks of BFR with low-intensity resistance exercise increased muscle mass and strength (Table 2), compared with low-intensity resistance exercise without BFR [28] or with sedentary controls [50, 51]. The increases in muscle cross-sectional area (CSA) [29, 31, 32, 52,53,54,55], leg press (muscle strength) [30, 54, 55] and leg extension (muscle strength) [29,30,31,32, 53,54,55] in older adults were similar when compared with resistance exercises incorporating heavier loads (≥ 70% 1RM) [29,30,31,32, 52,53,54,55]. In a different study, 12 weeks of combined BFR with resistance exercise resulted in increased muscle size and strength, relative to high-intensity resistance exercise alone [56]. In addition, BFR combined with resistance exercise training improved cardiovascular health in older participants, with decreases in mean arterial pressure (MAP; 11.6%), SBP (11.0%) and diastolic blood pressures (DBP; 12.1%) respectively [57]. Maximal aerobic exercise capacity (V̇O2max; ~ 10%) improved when participants underwent 12 weeks of BFR with low resistance exercise training [29, 31, 32]. It is important, however, to note that these studies included aerobic exercise training. Hence, synergistic V̇O2max adaptations with aerobic training may have occurred. These physiological improvements from combining BFR with resistance exercise also led to improvements in physical function, as measured by walking speed and the chair stand test [50, 54, 58]. Therefore, low-intensity resistance exercise combined with BFR is a viable mode of exercise for older adults.
Potential mechanisms of combining BFR with low-intensity resistance exercise in stimulating muscle hypertrophy in older adults
Intramuscular signaling pathways
Older adults have impaired anabolic responses to high-intensity resistance exercise training, which may partially be attributed to repression of specific molecular signaling involving muscle hypertrophy, for instance, chronic phosphorylation of basal S6K1 [21] and mTORC1 [22]. However, when older adults performed BFR with low-intensity resistance exercise, mTOR, S6K1, S6, mitogen-activated protein kinase-interacting kinase 1 (MnK1), AKT phosphorylation peaked 3 hours post-BFR exercise [28]. In addition, significant increase in muscle protein synthesis was reported [28]. The post-exercise peak in intramuscular signalling pathways and muscle protein synthesis was similar to young adults performing high-intensity resistance exercise [20]. However, a key difference was that skeletal muscle 4E-BP1 was phosphorylated after the BFR exercise in young adults [28] but not in older adults [28]. A depressed protein expression of 4E-BP1 may be relevant for older adults in staving off sarcopenia. In pre-clinical models, 24 month-old, 4E-BP1 knockout mice demonstrated enhanced protein synthesis in skeletal muscle, under basal and stimulated conditions, compared with age-matched wildtype controls [59]. Furthermore, the knockout mice also exhibited increased grip strength and muscle mass, compared with the age-matched wildtype controls. These observations suggest that phosphorylated 4E-BP1 may be a repressor for downstream protein translation and targeting this gene may be a potential prophylactic for treating sarcopenia.
The mechanisms responsible for the hypertrophic response following BFR exercise are still poorly understood, but many mechanisms have been proposed. The sub-section below will briefly discuss some proposed mechanisms as to how combining BFR with low-intensity exercise can have positive adaptations.
Reactive hyperemia (ischemia/reperfusion)
During BFR combined with resistance exercise, blood flow is restricted, creating an ischemic response. Immediately after exercise, the release of the occlusion increases blood flow to the muscles, resulting in reperfusion where blood flow is increased above pre-occlusion levels. Therefore, one of the proposed mechanisms is that reactive hyperemic response with BFR exercise is responsible for muscle hypertrophy. A research study by Gundermann and colleagues [60] showed that BFR resulted in elevated blood flow post-exercise, delivering nutrients (such as glucose and phenylalanine) to skeletal muscles. However, they also found that the enhanced blood flow and nutrient delivery was not the primary mechanism responsible for mTORC1 signaling and muscle protein synthesis after BFR exercise [60], indicating that reactive hyperemia is not the primary mechanism. It is likely that the hypertrophic response following BFR exercise involves other signaling pathways that are yet to be elucidated.
Metabolic stress
Metabolic stress has been reported to be as equally critical as mechanical tension for the induction of muscle growth [61,62,63,64]. To test this hypothesis, Goto and colleagues [65] compared 2 different rest periods, using volume- or intensity-matched resistance exercise, with one protocol having 30 sec rest between sets to minimize metabolite accumulation, while the other protocol did not have rest periods. Results showed that the concentration of blood lactate was significantly higher following the no-rest protocol when compared to the exercise with rest periods [65]. After 12 weeks of training with the same protocol, the protocol without rest resulted in an increase in muscle CSA, relative to pre-exercise, while there was no difference with the rest protocol [65]. This indicates an association between metabolic stress and muscle hypertrophy.
The degree of metabolic stress, such as lactate accumulation, was also observed during and post-BFR resistance exercise in older adults [28, 42, 43]. Indeed, lactate increases satellite cell activity and anabolic signal (phosphorylation of p70S6K and mTOR) for muscle hypertrophy in C2C12 muscle cells [66]. The potential for metabolic stress to stimulate muscle hypertrophy in older adults have been demonstrated by several studies using similar BFR (~above 50% AOP or up to 20 mmHg) with resistance exercise training (~ 20–50% 1RM) protocol over a period of time [29, 31, 32, 50,51,52,53,54,55,56, 67]. BFR with aerobic exercise also resulted in muscle hypertrophy in older adults [68,69,70], but to a smaller extent (~ 3%), compared with combined BFR resistance exercise (~ 4–17%).
Hypoxia
Hypoxia occurs when there is a decrease in oxygen tension. Hypoxia created by BFR may contribute to enhanced metabolic response following resistance exercise. A meta-analysis of nine eligible studies showed that hypoxia resistance training causes an increase in muscle size and strength [71]. BFR walking increased the release of hypoxic inducing factor 1 alpha (HIF-1α) [72], suggesting the potential for HIF-1α to be a stimulus for muscle hypertrophy. However, HIF-1α does not seem necessary for muscle development as the HIF-1α knockout experiment showed no effect on muscle development [73].
Exercising with BFR also stimulates vascular endothelial growth factor (VEGF) release [72, 74]. It was found that VEGF deletion in adult mouse skeletal muscle impaired the skeletal muscle contraction and hypertrophy adaptations [75]. VEGF plays an important role in muscle hypertrophy. The increase in VEGF following BFR may play a role, in part, to improved vascular endothelial function.
It is important to note that these studies were conducted in young adults and not in older adults. More research is required to establish how BFR exercise leads to muscle hypertrophy in older adults, and whether HIF-1α and VEGF are mechanistically involved.
Key issues and safety with the use of BFR
Gender and age can have different prevalence and rates of decline in skeletal muscle mass and strength. However, most studies examining the effect of BFR on the elderly recruited a mixed population of older men and women. An example is sarcopenia, where the prevalence of sarcopenia was reported more frequently in women younger than 70 years, while this was more frequent in men older than 80 years [76, 77]. One key factor affecting this difference is menopause in older women. The reason could be due to the decline in systemic concentrations of estrogen as women enter menopause [78]. The low systemic concentration of estrogen is associated with accelerated loss of skeletal muscle mass and strength [79, 80]. Postmenopausal women who underwent estrogen replacement therapy had systemic concentrations of estrogen that are similar to young women; further, resistance exercise enhanced their sensitivity to anabolic responses such as muscle protein synthesis [81]. In contrast, postmenopausal women who did not undergo estrogen replacement therapy did not observe any anabolic effects such as muscle protein synthesis, from the same exercise [81]. This suggests that the level of estrogen in the blood in postmenopausal women can affect muscle mass. Another factor that affects sarcopenia due to gender difference is testosterone. Testosterone level can predict skeletal muscle mass in the older male population [82]. Testosterone level is also positively associated with muscle strength and function [83], and that testosterone treatment in old hypogonadal men increased handgrip strength [84] and leg strength [85]. While the role of testosterone in older women is limited, low levels of testosterone in older women are often associated with lower skeletal muscle mass and strength [86].
Research design can also underestimate the effects of BFR exercise training. One example is a study by Fahs and colleagues (2014), where the same individual trains their legs with different protocols. Training one leg with BFR and the other leg without BFR may result in a crossover effect within the individual. For example, biomarkers and signalling proteins may differ in the leg training with BFR from the leg without BFR. But since 2 different protocols were performed on the same individual, biomarkers and signalling proteins from both protocols will mix up systematically in the individual, underestimating the effect of both protocols. This may explain the difference in these results, as compared to other studies where participants perform the same training on both legs [56].
Another important factor affecting BFR exercise is the occlusion pressure of the cuff. Some researchers used a standard occlusion pressure across all participants, as such, researchers must take into account cuff width and cuff material [87, 88]. For example, wider cuffs restrict blood pressure at a lower pressure [87]. On the other hand, other researchers have used and recommended the occlusion pressure to be individualized to the percent arterial occlusion pressure (%AOP) during exercise [89, 90]. Using this method accounts for individual blood pressure, cuff width, cuff material and limb width. For example, larger limbs will require a greater cuff pressure to fully restrict arterial blood flow regardless of cuff width [87]. Using %AOP may seem to individualize pressure for all participants, but it requires specialized equipment to measure arterial pressure. Another factor to consider is whether to use a full or partial occlusion pressure, to balance between exercise effectiveness and injury prevention.
Occlusion pressure is an important consideration for clinical conditions such as hypertension and osteoporosis, especially for older adults with these clinical conditions. There are concerns that full occlusion with exercise may cause discomforts, increase the risk of injury and compliance in those with hypertension and osteoporosis, especially in older adults, while partial occlusion with exercise may not achieve the desired musculoskeletal adaptations/benefits [91]. As such, Ilett and colleagues [91] have recommended the cuff pressure of at least 60–80% arterial occlusion pressure for BFR exercise to be effective in young adults. While there is no common consensus, more research is required to further explore this area with the older population.
While there are concerns regarding the use of BFR training for older adults, especially those with chronic conditions, studies have shown that BFR training is safe. Araújo and colleagues [92], reported a hypotensive effect of leg extension exercises with BFR in hypertensive adult women 60 mins after exercise. It is important to take note that the authors used only 2 training sessions. On the other hand, Brand et al. (2013) evaluated the effects of strength training without occlusion and found similar results. They demonstrated that resistance exercise was effective in reducing systolic blood pressure and diastolic blood pressure. It is important to emphasize that Brand and colleagues had used a 48-week strength training program without BFR on hypertensive adults and noted no change in hypertension levels with no adverse effect during training sessions [93]. The effect of acute exercise reduction in blood pressure of hypertensive subjects may last for up to 13 hours [94], whereas the effect of chronic exercise on blood pressure reduction remains to be evaluated. This hypotensive effect after a session of the exercise was also observed in older adults with hypertension [95]. BFR with low-intensity exercise has been recommended for clinical populations, including hypertension due to the lower risk of injury [96] and was reported safe for hypertension individuals [97, 98]. The use of BFR exercise on individuals with hypertension has been reviewed as safe and effective in promoting cardiovascular and musculoskeletal health [97,98,99]. It is also important to note that there were a few cases of discomfort reported [28, 100] and only one study [100] reported knee pain and adverse side effect, out of the 24 studies looking at the effects of BFR with resistance exercise on older adults reported here. Since the number of studies using BFR on older adults remains small, it is recommended that older participants undergo medical clearance prior to participating in BFR training.
Conclusions
The use of BFR with resistance exercise can be a viable and effective method for older adults to maintain musculoskeletal health. Many mechanisms underlying the musculoskeletal and cardiovascular adaptations have been suggested, but the extent to which they contribute is unclear and remains to be elucidated. Despite low mechanical stress from low-intensity exercise, when performed together with BFR, the combined approach can elicit adaptations similar to performing high-intensity exercise. While there are some concerns with the use of BFR on the older adults and clinical populations such as those with hypertension and osteoporosis, there has been no reported evidence to suggest that BFR elevates the risk of clinical complications any more than traditional high-intensity exercise modes. For the use of BFR in the older population, individuals are to be medically cleared of any cardiovascular risks.
Availability of data and materials
Not applicable.
Abbreviations
- CK:
-
Creatine kinase
- CO:
-
Cardiac output
- CSA:
-
Cross sectional area
- DBP:
-
Diastolic blood pressure
- GH:
-
Growth hormone
- IGF-I:
-
Insulin-like growth factor 1
- IL-6:
-
Interleukin-6
- MAP:
-
Mean arterial pressure
- mTOR:
-
Mammalian target of rapamycin
- SBP:
-
Systolic blood pressure
References
Sun Z. Aging, arterial stiffness, and hypertension. Hypertension. 2015;65(2):252–6. https://doi.org/10.1161/HYPERTENSIONAHA.114.03617.
Lexell J, Taylor CC, Sjöström M. What is the cause of the ageing atrophy?: Total number, size and proportion of different fiber types studied in whole vastus lateralis muscle from 15-to 83-year-old men. J Neurol Sci. 1988;84(2):275–94. https://doi.org/10.1016/0022-510X(88)90132-3.
Metter EJ, Conwit R, Tobin J, Fozard JL. Age-associated loss of power and strength in the upper extremities in women and men. J Gerontol Ser A Biol Med Sci. 1997;52(5):B267–76. https://doi.org/10.1093/gerona/52A.5.B267.
Arai H. Aging and homeostasis. Prevention and treatment of sarcopenia and frailty. Clinical calcium. 2017;27(7):1007–11 CliCa170710071011.
Marques A, Queirós C. Frailty, sarcopenia and falls. In: Fragility Fracture Nursing: Springer; 2018. p. 15–26.
Petermann-Rocha F, Balntzi V, Gray SR, Lara J, Ho FK, Pell JP, et al. Global prevalence of sarcopenia and severe sarcopenia: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle. 2022;13(1):86–99. https://doi.org/10.1002/jcsm.12783.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16–31. https://doi.org/10.1093/ageing/afy169.
Chen L-K, Liu L-K, Woo J, Assantachai P, Auyeung T-W, Bahyah KS, et al. Sarcopenia in Asia: consensus report of the Asian working Group for Sarcopenia. J Am Med Dir Assoc. 2014;15(2):95–101. https://doi.org/10.1016/j.jamda.2013.11.025.
Janssen I, Shepard DS, Katzmarzyk PT, Roubenoff R. The healthcare costs of sarcopenia in the United States. J Am Geriatr Soc. 2004;52(1):80–5. https://doi.org/10.1111/j.1532-5415.2004.52014.x.
Yang J. Enhanced skeletal muscle for effective glucose homeostasis. Prog Mol Biol Transl Sci. 2014;121:133–63. https://doi.org/10.1016/B978-0-12-800101-1.00005-3.
Cartee GD, Hepple RT, Bamman MM, Zierath JR. Exercise promotes healthy aging of skeletal muscle. Cell Metab. 2016;23(6):1034–47. https://doi.org/10.1016/j.cmet.2016.05.007.
Willoughby D, Medicine ACoS: resistance training and the older adult. ACSM Current Comment. In.; 2015.
Lambert CP, Evans WJ. Adaptations to aerobic and resistance exercise in the elderly. Rev Endocr Metab Disord. 2005;6(2):137–43. https://doi.org/10.1007/s11154-005-6726-5.
Guizelini PC, de Aguiar RA, Denadai BS, Caputo F, Greco CC. Effect of resistance training on muscle strength and rate of force development in healthy older adults: a systematic review and meta-analysis. Exp Gerontol. 2018;102:51–8. https://doi.org/10.1016/j.exger.2017.11.020.
Harridge SD. Plasticity of human skeletal muscle: gene expression to in vivo function. Exp Physiol. 2007;92(5):783–97. https://doi.org/10.1113/expphysiol.2006.036525.
Louis E, Raue U, Yang Y, Jemiolo B, Trappe S. Time course of proteolytic, cytokine, and myostatin gene expression after acute exercise in human skeletal muscle. J Appl Physiol. 2007;103(5):1744–51. https://doi.org/10.1152/japplphysiol.00679.2007.
Mitchell CJ, Churchward-Venne TA, West DW, Burd NA, Breen L, Baker SK, et al. Resistance exercise load does not determine training-mediated hypertrophic gains in young men. J Appl Physiol. 2012;113(1):71–7. https://doi.org/10.1152/japplphysiol.00307.2012.
Morton RW, Oikawa SY, Wavell CG, Mazara N, McGlory C, Quadrilatero J, et al. Neither load nor systemic hormones determine resistance training-mediated hypertrophy or strength gains in resistance-trained young men. J Appl Physiol. 2016;121(1):129–38. https://doi.org/10.1152/japplphysiol.00154.2016.
Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1435–45. https://doi.org/10.1249/mss.0b013e3180616aa2.
Fry CS, Drummond MJ, Glynn EL, Dickinson JM, Gundermann DM, Timmerman KL, et al. Aging impairs contraction-induced human skeletal muscle mTORC1 signaling and protein synthesis. Skelet Muscle. 2011;1(1):11. https://doi.org/10.1186/2044-5040-1-11.
Guillet C, Prod’homme M, Balage M, Gachon P, Giraudet C, Morin L, et al. Impaired anabolic response of muscle protein synthesis is associated with S6K1 dysregulation in elderly humans. FASEB J. 2004;18(13):1586–7. https://doi.org/10.1096/fj.03-1341fje.
Markofski MM, Dickinson JM, Drummond MJ, Fry CS, Fujita S, Gundermann DM, et al. Effect of age on basal muscle protein synthesis and mTORC1 signaling in a large cohort of young and older men and women. Exp Gerontol. 2015;65:1–7. https://doi.org/10.1016/j.exger.2015.02.015.
Joseph GA, Wang SX, Jacobs CE, Zhou W, Kimble GC, Herman WT, et al. Partial inhibition of mTORC1 in aged rats counteracts the decline in muscle mass and reverses molecular signaling associated with sarcopenia. Mol Cell Biol. 2019;39(19):e00141–19. https://doi.org/10.1128/MCB.00141-19.
Tremblay F, Marette A. Amino acid and insulin signaling via the mTOR/p70 S6 kinase pathway a negative feedback mechanism leading to insulin resistance in skeletal muscle cells. J Biol Chem. 2001;276(41):38052–60. https://doi.org/10.1074/jbc.M106703200.
Kumar V, Atherton PJ, Selby A, Rankin D, Williams J, Smith K, et al. Muscle protein synthetic responses to exercise: effects of age, volume, and intensity. J Gerontol A Biomed Sci Med Sci. 2012;67(11):1170–7. https://doi.org/10.1093/gerona/gls141.
Stutts WC. Physical activity determinants in adults: perceived benefits, barriers, and self efficacy. AAOHN J. 2002;50(11):499–507. https://doi.org/10.1177/216507990205001106.
Fujita S, Abe T, Drummond MJ, Cadenas JG, Dreyer HC, Sato Y, et al. Blood flow restriction during low-intensity resistance exercise increases S6K1 phosphorylation and muscle protein synthesis. J Appl Physiol. 2007;103(3):903–10. https://doi.org/10.1152/japplphysiol.00195.2007.
Fry CS, Glynn EL, Drummond MJ, Timmerman KL, Fujita S, Abe T, et al. Blood flow restriction exercise stimulates mTORC1 signaling and muscle protein synthesis in older men. J Appl Physiol. 2010;108(5):1199–209. https://doi.org/10.1152/japplphysiol.01266.2009.
de Souza TMF, Libardi CA, Cavaglieri CR, Gáspari AF, Brunelli DT, de Souza GV, et al. Concurrent training with blood flow restriction does not decrease inflammatory markers. Int J Sports Med. 2018;40(01):29–36. https://doi.org/10.1055/s-0043-119222.
Karabulut M, Abe T, Sato Y, Bemben MG. The effects of low-intensity resistance training with vascular restriction on leg muscle strength in older men. Eur J Appl Physiol. 2010;108(1):147–55. https://doi.org/10.1007/s00421-009-1204-5.
Libardi C, Chacon-Mikahil M, Cavaglieri C, Tricoli V, Roschel H, Vechin F, et al. Effect of concurrent training with blood flow restriction in the elderly. Int J Sports Med. 2015;36(05):395–9. https://doi.org/10.1055/s-0034-1390496.
Sedghi SS. Effect of combined aerobic and resistance training with blood flow restriction in the elderly women. Sport Sci Pract Asp. 2017;14(1).
Sato Y. The history and future of KAATSU training. Int J KAATSU Train Res. 2005;1(1):1–5. https://doi.org/10.3806/ijktr.1.1.
Takarada Y, Takazawa H, Ishii N. Applications of vascular occlusion diminish disuse atrophy of knee extensor muscles. Med Sci Sports Exerc. 2000;32(12):2035–9. https://doi.org/10.1097/00005768-200012000-00011.
Kubota A, Sakuraba K, Koh S, Ogura Y, Tamura Y. Blood flow restriction by low compressive force prevents disuse muscular weakness. J Sci Med Sport. 2011;14(2):95–9. https://doi.org/10.1016/j.jsams.2010.08.007.
Kubota A, Sakuraba K, Sawaki K, Sumide T, Tamura Y. Prevention of disuse muscular weakness by restriction of blood flow. Med Sci Sports Exerc. 2008;40(3):529–34. https://doi.org/10.1249/MSS.0b013e31815ddac6.
Barbalho M, Rocha AC, Seus TL, Raiol R, Del Vecchio FB, Coswig VS. Addition of blood flow restriction to passive mobilization reduces the rate of muscle wasting in elderly patients in the intensive care unit: a within-patient randomized trial. Clin Rehabil. 2019;33(2):233–40. https://doi.org/10.1177/0269215518801440.
Patterson SD, Leggate M, Nimmo MA, Ferguson RA. Circulating hormone and cytokine response to low-load resistance training with blood flow restriction in older men. Eur J Appl Physiol. 2013;113(3):713–9. https://doi.org/10.1007/s00421-012-2479-5.
Welle S. Growth hormone and insulin-like growth factor-I as anabolic agents. Curr Opin Clin Nutr Metab Care. 1998;1(3):257–62. https://doi.org/10.1097/00075197-199805000-00004.
Giannoulis MG, Jackson N, Shojaee-Moradie F, Nair KS, Sonksen PH, Martin FC, et al. The effects of growth hormone and/or testosterone on whole body protein kinetics and skeletal muscle gene expression in healthy elderly men: a randomized controlled trial. J Clin Endocrinol Metab. 2008;93(8):3066–74. https://doi.org/10.1210/jc.2007-2695.
Brill KT, Weltman AL, Gentili A, Patrie JT, Fryburg DA, Hanks JB, et al. Single and combined effects of growth hormone and testosterone administration on measures of body composition, physical performance, mood, sexual function, bone turnover, and muscle gene expression in healthy older men. J Clin Endocrinol Metab. 2002;87(12):5649–57. https://doi.org/10.1210/jc.2002-020098.
Pinto RR, Karabulut M, Poton R, Polito MD. Acute resistance exercise with blood flow restriction in elderly hypertensive women: haemodynamic, rating of perceived exertion and blood lactate. Clin Physiol Funct Imaging. 2018;38(1):17–24. https://doi.org/10.1111/cpf.12376.
Staunton CA, May AK, Brandner CR, Warmington SA. Haemodynamics of aerobic and resistance blood flow restriction exercise in young and older adults. Eur J Appl Physiol. 2015;115(11):2293–302. https://doi.org/10.1007/s00421-015-3213-x.
de Freitas MC, Gerosa-Neto J, Zanchi NE, Lira FS, Rossi FE. Role of metabolic stress for enhancing muscle adaptations: practical applications. World J Methodol. 2017;7(2):46–54. https://doi.org/10.5662/wjm.v7.i2.46.
Grosicki GJ, Barrett B, Englund D, Liu C, Travison T, Cederholm T, et al. Circulating Interleukin-6 is associated with skeletal muscle strength, quality, and functional adaptation with exercise training in mobility-limited older adults. J Frailty Aging. 2020;9(1):57–63. https://doi.org/10.14283/jfa.2019.30.
Frontera WR, Meredith CN, O'Reilly KP, Knuttgen HG, Evans WJ. Strength conditioning in older men: skeletal muscle hypertrophy and improved function. J Appl Physiol. 1988;64(3):1038–44. https://doi.org/10.1152/jappl.1988.64.3.1038.
Rantanen T, Avela J. Leg extension power and walking speed in very old people living independently. J Gerontol Ser A Biol Med Sci. 1997;52(4):M225–31. https://doi.org/10.1093/gerona/52A.4.M225.
Byrne C, Faure C, Keene DJ, Lamb SE. Ageing, muscle power and physical function: a systematic review and implications for pragmatic training interventions. Sports Med. 2016;46(9):1311–32. https://doi.org/10.1007/s40279-016-0489-x.
Dipietro L, Campbell WW, Buchner DM, Erickson KI, Powell KE, Bloodgood B, et al. Physical activity, injurious falls, and physical function in aging: an umbrella review. Med Sci Sports Exerc. 2019;51(6):1303–13. https://doi.org/10.1249/MSS.0000000000001942.
Yasuda T, Fukumura K, Fukuda T, Uchida Y, Iida H, Meguro M, et al. Muscle size and arterial stiffness after blood flow-restricted low-intensity resistance training in older adults. Scand J Med Sci Sports. 2014;24(5):799–806. https://doi.org/10.1111/sms.12087.
Yasuda T, Fukumura K, Uchida Y, Koshi H, Iida H, Masamune K, et al. Effects of low-load, elastic band resistance training combined with blood flow restriction on muscle size and arterial stiffness in older adults. J Gerontol A Biomed Sci Med Sci. 2015;70(8):950–8. https://doi.org/10.1093/gerona/glu084.
Vechin FC, Libardi CA, Conceição MS, Damas FR, Lixandrão ME, Berton RP, et al. Comparisons between low-intensity resistance training with blood flow restriction and high-intensity resistance training on quadriceps muscle mass and strength in elderly. J Strength Cond Res. 2015;29(4):1071–6. https://doi.org/10.1519/JSC.0000000000000703.
Vechin FC, Libardi CA, Conceição MS, Damas F, Cavaglieri CR, Chacon-Mikahil MPT, et al. Low-intensity resistance training with partial blood flow restriction and high-intensity resistance training induce similar changes in skeletal muscle transcriptome in elderly humans. Appl Physiol Nutr Metab. 2019;44(2):216–20. https://doi.org/10.1139/apnm-2018-0146.
Cook SB, LaRoche DP, Villa MR, Barile H, Manini TM. Blood flow restricted resistance training in older adults at risk of mobility limitations. Exp Gerontol. 2017;99:138–45. https://doi.org/10.1016/j.exger.2017.10.004.
Thiebaud RS, Loenneke JP, Fahs CA, Rossow LM, Kim D, Abe T, et al. The effects of elastic band resistance training combined with blood flow restriction on strength, total bone-free lean body mass and muscle thickness in postmenopausal women. Clin Physiol Funct Imaging. 2013;33(5):344–52. https://doi.org/10.1111/cpf.12033.
Yasuda T, Fukumura K, Tomaru T, Nakajima T. Thigh muscle size and vascular function after blood flow-restricted elastic band training in older women. Oncotarget. 2016;7(23):33595–607. https://doi.org/10.18632/oncotarget.9564.
Cezar MA, De Sá CA, VdS C, Copatti SL, GAGd S, MEdS G. Effects of exercise training with blood flow restriction on blood pressure in medicated hypertensive patients. Motriz Revista de Educação Física. 2016;22(2):9–17. https://doi.org/10.1590/S1980-6574201600020002.
Harber MP, Konopka AR, Undem MK, Hinkley JM, Minchev K, Kaminsky LA, et al. Aerobic exercise training induces skeletal muscle hypertrophy and age-dependent adaptations in myofiber function in young and older men. J Appl Physiol. 2012;113(9):1495–504. https://doi.org/10.1152/japplphysiol.00786.2012.
Le Bacquer O, Combe K, Patrac V, Ingram B, Combaret L, Dardevet D, et al. 4E-BP1 and 4E-BP2 double knockout mice are protected from aging-associated sarcopenia. J Cachexia Sarcopenia Muscle. 2019;10(3):696–709. https://doi.org/10.1002/jcsm.12412.
Gundermann DM, Fry CS, Dickinson JM, Walker DK, Timmerman KL, Drummond MJ, et al. Reactive hyperemia is not responsible for stimulating muscle protein synthesis following blood flow restriction exercise. J Appl Physiol. 2012;112(9):1520–8. https://doi.org/10.1152/japplphysiol.01267.2011.
Takada S, Okita K, Suga T, Omokawa M, Kadoguchi T, Sato T, et al. Low-intensity exercise can increase muscle mass and strength proportionally to enhanced metabolic stress under ischemic conditions. J Appl Physiol. 2012;113(2):199–205. https://doi.org/10.1152/japplphysiol.00149.2012.
Loenneke JP, Pujol TJ. The use of occlusion training to produce muscle hypertrophy. Strength & Conditioning Journal. 2009;31(3):77–84. https://doi.org/10.1519/SSC.0b013e3181a5a352.
Schoenfeld BJ. Potential mechanisms for a role of metabolic stress in hypertrophic adaptations to resistance training. Sports Med. 2013;43(3):179–94. https://doi.org/10.1007/s40279-013-0017-1.
Suga T, Okita K, Morita N, Yokota T, Hirabayashi K, Horiuchi M, et al. Dose effect on intramuscular metabolic stress during low-intensity resistance exercise with blood flow restriction. J Appl Physiol. 2010;108(6):1563–7. https://doi.org/10.1152/japplphysiol.00504.2009.
Goto K, Ishii N, Kizuka T, Takamatsu K. The impact of metabolic stress on hormonal responses and muscular adaptations. Med Sci Sports Exerc. 2005;37(6):955–63.
Oishi Y, Tsukamoto H, Yokokawa T, Hirotsu K, Shimazu M, Uchida K, et al. Mixed lactate and caffeine compound increases satellite cell activity and anabolic signals for muscle hypertrophy. J Appl Physiol. 2015;118(6):742–9. https://doi.org/10.1152/japplphysiol.00054.2014.
Fahs CA, Rossow LM, Thiebaud RS, Loenneke JP, Kim D, Abe T, et al. Vascular adaptations to low-load resistance training with and without blood flow restriction. Eur J Appl Physiol. 2014;114(4):715–24. https://doi.org/10.1007/s00421-013-2808-3.
Ozaki H, Sakamaki M, Yasuda T, Fujita S, Ogasawara R, Sugaya M, et al. Increases in thigh muscle volume and strength by walk training with leg blood flow reduction in older participants. J Gerontol A Biomed Sci Med Sci. 2011;66(3):257–63. https://doi.org/10.1093/gerona/glq182.
Ozaki H, Miyachi M, Nakajima T, Abe T. Effects of 10 weeks walk training with leg blood flow reduction on carotid arterial compliance and muscle size in the elderly adults. Angiology. 2011;62(1):81–6. https://doi.org/10.1177/0003319710375942.
Iida H, Nakajima T, Kurano M, Yasuda T, Sakamaki M, Sato Y, et al. Effects of walking with blood flow restriction on limb venous compliance in elderly subjects. Clin Physiol Funct Imaging. 2011;31(6):472–6. https://doi.org/10.1111/j.1475-097X.2011.01044.x.
Ramos-Campo DJ, Scott BR, Alcaraz PE, Rubio-Arias JA. The efficacy of resistance training in hypoxia to enhance strength and muscle growth: a systematic review and meta-analysis. Eur J Sport Sci. 2018;18(1):92–103. https://doi.org/10.1080/17461391.2017.1388850.
Barjaste A, Mirzaei B, Rahmani-nia F, Haghniyaz R, Brocherie F. Concomitant aerobic-and hypertrophy-related skeletal muscle cell signaling following blood flow-restricted walking. Sci Sports. 2020;36(2):e51–8. https://doi.org/10.1016/j.scispo.2020.03.006.
Yang X, Yang S, Wang C, Kuang S. The hypoxia-inducible factors HIF1α and HIF2α are dispensable for embryonic muscle development but essential for postnatal muscle regeneration. J Biol Chem. 2017;292(14):5981–91. https://doi.org/10.1074/jbc.M116.756312.
Shimizu R, Hotta K, Yamamoto S, Matsumoto T, Kamiya K, Kato M, et al. Low-intensity resistance training with blood flow restriction improves vascular endothelial function and peripheral blood circulation in healthy elderly people. Eur J Appl Physiol. 2016;116(4):749–57. https://doi.org/10.1007/s00421-016-3328-8.
Huey KA. Potential roles of vascular endothelial growth factor during skeletal muscle hypertrophy. Exerc Sport Sci Rev. 2018;46(3):195–202. https://doi.org/10.1249/JES.0000000000000152.
Kirchengast S, Huber J. Gender and age differences in lean soft tissue mass and sarcopenia among healthy elderly. Anthropol Anz. 2009;67(2):139–51. https://doi.org/10.1127/0003-5548/2009/0018.
Cherin P, Voronska E, Fraoucene N, de Jaeger C. Prevalence of sarcopenia among healthy ambulatory subjects: the sarcopenia begins from 45 years. Aging Clin Exp Res. 2014;26(2):137–46. https://doi.org/10.1007/s40520-013-0132-8.
Vina J, Sastre J, Pallardo F, Gambini J, Borras C. Role of mitochondrial oxidative stress to explain the different longevity between genders. Protective effect of estrogens. Free Radic Res. 2006;40(12):1359–65. https://doi.org/10.1080/10715760600952851.
Cooper R, Mishra G, Clennell S, Guralnik J, Kuh D: Menopausal status and physical performance in midlife: findings from a British birth cohort study. Menopause (New York, NY) 2008, 15(6):1079.
Carville SF, Rutherford OM, Newham DJ. Power output, isometric strength and steadiness in the leg muscles of pre-and postmenopausal women; the effects of hormone replacement therapy. Eur J Appl Physiol. 2006;96(3):292–8. https://doi.org/10.1007/s00421-005-0078-4.
Hansen M, Skovgaard D, Reitelseder S, Holm L, Langbjerg H, Kjaer M. Effects of estrogen replacement and lower androgen status on skeletal muscle collagen and myofibrillar protein synthesis in postmenopausal women. J Gerontol A Biomed Sci Med Sci. 2012;67(10):1005–13. https://doi.org/10.1093/gerona/gls007.
Iannuzzi-Sucich M, Prestwood KM, Kenny AM. Prevalence of sarcopenia and predictors of skeletal muscle mass in healthy, older men and women. J Gerontol Ser A Biol Med Sci. 2002;57(12):M772–7. https://doi.org/10.1093/gerona/57.12.M772.
van den Beld AW, de Jong FH, Grobbee DE, Pols HA, Lamberts SW. Measures of bioavailable serum testosterone and estradiol and their relationships with muscle strength, bone density, and body composition in elderly men. J Clin Endocrinol Metab. 2000;85(9):3276–82. https://doi.org/10.1210/jcem.85.9.6825.
Sih R, Morley JE, Kaiser FE, Perry HM III, Patrick P, Ross C. Testosterone replacement in older hypogonadal men: a 12-month randomized controlled trial. J Clin Endocrinol Metab. 1997;82(6):1661–7. https://doi.org/10.1210/jcem.82.6.3988.
Kenny AM, Prestwood KM, Gruman CA, Marcello KM, Raisz LG. Effects of transdermal testosterone on bone and muscle in older men with low bioavailable testosterone levels. J Gerontol Ser A Biol Med Sci. 2001;56(5):M266–72. https://doi.org/10.1093/gerona/56.5.M266.
Häkkinen K, Pakarinen A. Muscle strength and serum testosterone, cortisol and SHBG concentrations in middle-aged and elderly men and women. Acta Physiol Scand. 1993;148(2):199–207. https://doi.org/10.1111/j.1748-1716.1993.tb09549.x.
Loenneke JP, Fahs CA, Rossow LM, Sherk VD, Thiebaud RS, Abe T, et al. Effects of cuff width on arterial occlusion: implications for blood flow restricted exercise. Eur J Appl Physiol. 2012;112(8):2903–12. https://doi.org/10.1007/s00421-011-2266-8.
Rossow LM, Fahs CA, Loenneke JP, Thiebaud RS, Sherk VD, Abe T, et al. Cardiovascular and perceptual responses to blood-flow-restricted resistance exercise with differing restrictive cuffs. Clin Physiol Funct Imaging. 2012;32(5):331–7. https://doi.org/10.1111/j.1475-097X.2012.01131.x.
Patterson SD, Hughes L, Head P, Warmington S, Brandner C. Blood flow restriction training: a novel approach to augment clinical rehabilitation: how to do it. In.: BMJ publishing group ltd and British Association of Sport and Exercise. Medicine. 2017;51(23):1648–9. https://doi.org/10.1136/bjsports-2017-097738.
McEwen JA, Owens JG, Jeyasurya J. Why is it crucial to use personalized occlusion pressures in blood flow restriction (BFR) rehabilitation? J Med Biol Eng. 2019;39(2):173–7. https://doi.org/10.1007/s40846-018-0397-7.
Ilett MJ, Rantalainen T, Keske MA, May AK, Warmington SA. The effects of restriction pressures on the acute responses to blood flow restriction exercise. Front Physiol. 2019;10:1018. https://doi.org/10.3389/fphys.2019.01018.
Araújo JP, Silva ED, Silva JC, Souza TS, Lima EO, Guerra I, et al. The acute effect of resistance exercise with blood flow restriction with hemodynamic variables on hypertensive subjects. J Hum Kinet. 2014;43(1):79–85. https://doi.org/10.2478/hukin-2014-0092.
Brand C, Griebeler LC, Roth MA, Mello FF, Barros TVP, Neu LD. Efeito do treinamento resistido em parâmetros cardiovasculares de adultos normotensos e hipertensos. Rev Bras Cardiol. 2013;26(6):435–41.
Pescatello LS, Fargo AE, Leach CN Jr, Scherzer HH. Short-term effect of dynamic exercise on arterial blood pressure. Circulation. 1991;83(5):1557–61. https://doi.org/10.1161/01.CIR.83.5.1557.
Costa JBY, Gerage AM, Gonçalves CGS, Pina FLC, Polito MD. Influence of the training status on the blood pressure behavior after a resistance training session in hypertensive older females. Rev Bras Med Esporte. 2010;16(2):103–6. https://doi.org/10.1590/S1517-86922010000200005.
Chulvi-Medrano I. Resistance training with blood flow restriction and hypertensive subjects. J Hum Kinet. 2015;46(1):7–8. https://doi.org/10.1515/hukin-2015-0028.
Loenneke J, Wilson J, Wilson G, Pujol T, Bemben M. Potential safety issues with blood flow restriction training. Scand J Med Sci Sports. 2011;21(4):510–8. https://doi.org/10.1111/j.1600-0838.2010.01290.x.
Nakajima T, Kurano M, Iida H, Takano H, Oonuma H, Morita T, et al. Use and safety of KAATSU training: results of a national survey. Int J KAATSU Train Res. 2006;2(1):5–13. https://doi.org/10.3806/ijktr.2.5.
Wong ML, Formiga MF, Owens J, Asken T, Cahalin LP. Safety of blood flow restricted exercise in hypertension: a meta-analysis and systematic review with potential applications in orthopedic care. Tech Orthop. 2018;33(2):80–8. https://doi.org/10.1097/BTO.0000000000000288.
Harper SA, Roberts LM, Layne AS, Jaeger BC, Gardner AK, Sibille KT, et al. Blood-flow restriction resistance exercise for older adults with knee osteoarthritis: a pilot randomized clinical trial. J Clin Med. 2019;8(2):265. https://doi.org/10.3390/jcm8020265.
Pinto RR, Polito MD. Haemodynamic responses during resistance exercise with blood flow restriction in hypertensive subjects. Clin Physiol Funct Imaging. 2016;36(5):407–13. https://doi.org/10.1111/cpf.12245.
Lopes KG, Bottino DA, Farinatti P, MdGC d S, Maranhão PA, CMS d A, et al. Strength training with blood flow restriction–a novel therapeutic approach for older adults with sarcopenia? A Case Report. Clin Interv Aging. 2019;14:1461–9. https://doi.org/10.2147/CIA.S206522.
Patterson SD, Ferguson RA. Enhancing strength and postocclusive calf blood flow in older people with training with blood-flow restriction. J Aging Phys Act. 2011;19(3):201–13. https://doi.org/10.1123/japa.19.3.201.
Ruaro MF, Santana JO, Gusmão N, De França E, Carvalho BN, Farinazo KB, et al. Effects of strength training with and without blood flow restriction on quality of life in the elderly. J Phys Educ Sport. 2019;19:787–94.
Acknowledgements
None.
Authors’ informations
ZXL is a Research Fellow in the Healthy Longevity Translational Research Programme and the Department of Biochemistry, Yong Loo Lin School of Medicine, at the National University of Singapore and the Centre for Healthy Longevity, National University Health System. JG is a Research Assistant Professor in the Healthy Longevity Translational Research Programme and the Department of Physiology, Yong Loo Lin School of Medicine, at the National University of Singapore and the Centre for Healthy Longevity, National University Health System.
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
ZXL and JG conceptualized the manuscript. ZXL performed the literature research, drafted and revised the manuscript. JG gave critical comments and edited the manuscript. ZXL and JG approve of the final version of the manuscript to be published.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Both authors give consent for this manuscript to be published.
Competing interests
The authors declare no competing interests in this work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lim, Z.X., Goh, J. Effects of blood flow restriction (BFR) with resistance exercise on musculoskeletal health in older adults: a narrative review. Eur Rev Aging Phys Act 19, 15 (2022). https://doi.org/10.1186/s11556-022-00294-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s11556-022-00294-0