Abstract
Idiopathic inflammatory myopathies (IIMs) are autoimmune disorders characterized by symmetric proximal muscle weakness and chronic inflammation, with an increased risk of morbidity and mortality. The current standard of care includes traditional immunosuppressive pharmacotherapies; however, some patients cannot tolerate or do not adequately respond to these therapies, highlighting the need for alternative treatments for refractory disease. Acthar® Gel (repository corticotropin injection) is a naturally sourced mixture of adrenocorticotropic hormone analogs and other pituitary peptides that has been approved by the US Food and Drug Administration since 1952 for use in patients with two subgroups of IIMs, dermatomyositis (DM) and polymyositis (PM). However, it has not been routinely used in the treatment of IIMs. While Acthar may induce steroidogenesis, it also has a steroid-independent mechanism of action by exerting immunomodulatory effects through the activation of melanocortin receptors on immune cells, such as macrophages, B cells, and T cells. Recent clinical trials, retrospective analyses, and case reports add to the growing evidence suggesting that Acthar may be effective in patients with DM and PM. Here we review the current evidence supporting the safety and efficacy of Acthar for the treatment of refractory DM and PM.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
This review describes the current clinical evidence supporting the safety and efficacy of Acthar® Gel (repository corticotropin injection) for the treatment of two subgroups of idiopathic inflammatory myopathies, dermatomyositis (DM) and polymyositis (PM). |
Acthar is a naturally sourced mixture of adrenocorticotropic hormone analogs and other pituitary peptides with a unique immunomodulatory mechanism of action through activating melanocortin receptors on immune cells. |
Recent clinical trials, retrospective analyses, and case reports suggest that Acthar may be effective in patients with DM and PM and is generally safe and well tolerated. |
Acthar may provide an alternative treatment for patients who cannot tolerate the side effects or are unresponsive to standard therapies for DM and PM. |
Introduction
Idiopathic inflammatory myopathies (IIMs) are a group of relatively rare systemic autoimmune disorders with an estimated global prevalence of 2.9 to 34 per 100,000 individuals [1]. IIMs have traditionally been classified into five major subgroups based on their clinicopathologic characteristics: dermatomyositis (DM), polymyositis (PM), immune-mediated necrotizing myopathy (IMNM), anti-synthetase syndrome (ASyS), and inclusion-body myositis [2]. Most of the IIMs are characterized by symmetric proximal muscle weakness and chronic inflammation [1, 2]. DM is typically accompanied by characteristic skin manifestations, such as heliotrope rash and Gottron’s sign or papules [3]. Extramuscular manifestations include dysphagia, arthritis [4], interstitial lung disease (ILD) [5], cardiovascular effects (e.g., myocarditis) [6], and Raynaud’s syndrome [7]. In addition, myositis-specific autoantibodies are present in approximately 50–70% of patients with DM and PM [8, 9].
Classification criteria have been accepted by the American College of Rheumatology (ACR)/European League Against Rheumatism (EULAR) that allow clinicians to distinguish IIM from conditions with similar phenotypes and to subclassify patients into the major IIM subgroups [10]. However, there remains a lack of standardized therapeutic guidelines [11, 12], and some patients cannot tolerate or do not adequately respond to standard-of-care therapies. Further, some specific manifestations refractory to standard immunosuppressive therapies are a significant challenge for clinicians, including calcinosis universalis, aphagia, rapidly progressive interstitial lung disease, and chronic intestinal pseudo-obstruction [12]. This complicates the disease landscape and highlights the need for alternative therapies for these patients with refractory disease.
Here we present the clinical evidence for the safety and efficacy of Acthar® Gel (repository corticotropin injection) and how it may be considered as an alternative treatment of DM and PM. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Epidemiology, Diagnosis, and Pathophysiology of DM and PM
DM and PM are associated with increased risk of morbidity and mortality [13]. The most common causes of death are cancer, infection, profound effects of muscle weakness, and cardiovascular disease [14]. Both DM and PM have been shown to be more prevalent in female and Black/African-American patients [15,16,17,18].
The diagnoses of DM and PM are based on clinical signs and symptoms, muscle biopsies to identify inflammatory features, electromyography for evaluating myopathic vs. neuropathic causes of weakness, magnetic resonance imaging to identify active inflammation in muscle or fascia, and serum levels of muscle-derived enzymes (e.g., creatine kinase) [2]. Myositis-specific autoantibodies are generally mutually exclusive and can be associated with specific disease manifestations that help guide classification, prognosis, and disease management [8, 9].
DM is characterized by perimysial and perivascular inflammation and muscle fiber atrophy (Fig. 1) [2]. It begins when putative antibodies directed against endothelial cells of the endomysial capillaries activate the classical complement cascade. This results in the formation and deposition of the membrane attack complex (MAC) on capillaries surrounding the muscle fibers and leads to endothelial cell death and ischemic muscle fiber damage [19,20,21]. Complement activation also leads to the release of proinflammatory cytokines and chemokines that upregulate the expression of adhesion molecules on the endothelial cell membrane, facilitating the transmigration of activated CD4+ T cells, B cells, and macrophages to the endomysial tissue [19,20,21]. Perivascular, perimysial, and perifascicular inflammation, along with perifascicular atrophy and reduced capillaries, are characteristic of the muscle biopsy in DM [2]. This, along with the skin manifestations of heliotrope rash, Gottron’s papules, or Gottron’s sign, provides the basis for DM diagnosis [22, 23].
Pathophysiology of dermatomyositis. Muscle fiber atrophy begins when putative antibodies directed against endothelial cells of the endomysial capillaries activate the classical complement cascade. The membrane attack complex (MAC) is deposited on capillaries surrounding the muscle fibers and leads to endothelial cell death and ischemic muscle fiber damage. Complement activation also leads to the release of proinflammatory cytokines and chemokines that upregulate the expression of adhesion molecules (VCAM-1, ICAM-1) on the endothelial cell membrane, facilitating the transmigration of activated CD4+ T cells, B cells, and macrophages to the endomysial tissue. Figure created with BioRender.com. C1 indicates complement component 1; C3, complement component 3; C3b, complement component 3b; ICAM-1, intercellular adhesion molecule 1; LFA-1, lymphocyte function-associated antigen 1; MAC, membrane attack complex; Mac-1, macrophage-1 antigen; pDC, plasmacytoid dendritic cell; VCAM-1, vascular cell adhesion protein 1; VLA-4, very late antigen-4
PM is characterized by endomysial inflammation [2] and muscle fiber degeneration [1]; however, the mechanism by which this occurs is not well established. Muscle biopsies from individuals with PM show an overexpression of major histocompatibility complex (MHC) class 1 antigens on muscle fibers, infiltration of CD8+ T cells, and muscle fiber necrosis (Fig. 2) [2, 19]. Muscle fiber death occurs when an antigen-specific CD8+ T cell binds to its corresponding MHC-1 expressing antigen on a muscle fiber, activating the CD8+ T cell to release perforin and granzyme granules that ultimately result in cell death [2]. Pro-inflammatory cytokines (e.g., interferon-γ, tumor necrosis factor-α) released by the activated T cells may also enhance MHC-1 upregulation and the cytotoxic effect of T cells [2]. B cells and terminally differentiated plasma cells are also found in the muscle tissue of patients with PM; however, their role in muscle inflammation has not been fully elucidated [24].
Pathophysiology of polymyositis. Polymyositis is characterized by an overexpression of major histocompatibility complex (MHC) class 1 antigens on muscle fibers and the infiltration of CD8+ T cells from the periphery into the endomysium. Muscle fiber death occurs when an antigen-specific CD8+ T cell binds its corresponding MHC-1 expressing antigen on a muscle fiber, activating the CD8+ T cell to release perforin and granzyme granules and resulting in necrosis. Pro-inflammatory cytokines (e.g., interferon-γ, tumor necrosis factor-α) released by the activated T cells may also enhance MHC-1 upregulation and the cytotoxic effect of T cells. Figure created with BioRender.com. CD40 indicates cluster of differentiation 40; CD40L, cluster of differentiation 40 ligand; CD80, cluster of differentiation 80; CTLA-4, cytotoxic T lymphocyte associated protein 4; ICAM-1, intercellular adhesion molecule 1; ICOS, inducible costimulator; ICOS-L, inducible costimulator-ligand; LFA-1, lymphocyte function-associated antigen 1; MHC, major histocompatibility complex; TCR, T cell receptor; VCAM-1, vascular cell adhesion protein 1; VLA-4, very late antigen-4
The discovery of myositis-specific antibodies has allowed the identification of new subgroups of IIMs with distinct clinical and muscle histopathologic features, including IMNM and ASyS [1]. Muscle biopsies from patients with autoantibodies against aminoacyl transfer RNA synthetases, a hallmark of patients with ASyS, exhibit perifascicular necrosis [25] and endomysial infiltration by clonally expanded T cells [26]. In addition, patients with ASyS have a higher incidence of pulmonary involvement and may have glucocorticoid-resistant myositis or ILD [27]. Patients with IMNM most often have autoantibodies to 3-hydroxy-3-methylglutaryl-coenzyme A reductase (HMGCR) or the signal recognition particle (SRP), which are highly correlated with muscle weakness and elevated creatine kinase levels [1]. Although muscle biopsies show increased macrophages and deposits of MAC on the sarcolemma, IMNM-specific autoantibodies do not appear to be complement-fixing [28], and the pathophysiological mechanism of muscle damage remains uncertain [1].
Current Standard of Care
Current clinical practice guidelines indicate the use of physical therapy and sun protection (in patients with DM) in addition to traditional immunosuppressive pharmacotherapies [12]. It is generally agreed that glucocorticoids should be the first-line therapy for DM and PM [11, 12, 29, 30], with the addition of methotrexate or azathioprine for moderate-to-severe disease or to control disease flares when tapering glucocorticoids (Fig. 3) [1, 11, 29, 30]. Unfortunately, glucocorticoids are not an optimal long-term treatment option due to a high rate of adverse events (AEs) and other complications [11, 29] (e.g., diabetes, hypertension, dyslipidemia, osteoporosis, weight gain, gastric intolerance, mood changes, infections, cataracts, and glaucoma) [31]. Despite these side effects, drugs such as methotrexate, azathioprine, mycophenolate mofetil (MMF), and intravenous immunoglobulin (IVIg) are recommended for their steroid-sparing abilities. Typically, 30–40% of patients have disease that is refractory to glucocorticoids, with fewer than 50% of patients achieving a complete response and many experiencing significant side effects. Further, glucocorticoid tapering is often associated with disease flare, and most patients will require an additional immunosuppressive agent [13, 14].
Current standard of care therapies for the management of idiopathic inflammatory myopathies. Reproduced from Oddis CV, Aggarwal R. Treatment in myositis. Nat Rev Rheumatol. 2018;14(5):279–289. doi: https://doi.org/10.1038/nrrheum.2018.42. IVIg indicates intravenous immunoglobulin; MMF, mycophenolate mofetil
MMF is typically used as a second-line therapy, except in patients with moderate-to-severe myositis associated with ILD and refractory DM rashes for whom it can be used as a first-line therapy [1, 11]. The calcineurin inhibitors cyclosporine and tacrolimus are also considered second-line therapies; however, they are typically reserved for refractory myositis with either muscle weakness or associated ILD due to toxicity concerns [1, 11, 30]. Third-line therapies include cyclophosphamide and biologic agents such as rituximab [1, 32,33,34]. Owing to the toxic effects and increased risk of malignancy at high cumulative doses of cyclophosphamide, its use is limited to severe refractory muscle weakness, rapidly progressive ILD, or systemic vasculitis [1, 30].
IVIg therapy is approved by the US Food and Drug Administration (FDA) for DM in adults and is considered safe and effective in combination with or after failure of glucocorticoids or other immunosuppressive drugs. However, IVIg treatment is associated with increased health care resource utilization due to administration in an outpatient setting [35]. In addition, it has a long administration time and potential side effects and is contraindicated in patients with a high risk of thromboembolism, so it is not routinely used as a first-line therapy unless there are features such as dysphagia [36], anti-HMGCR-related IMNM [37], active infection, severe disease, pregnancy, cancer, or ILD [1, 11, 12, 29, 30, 38].
Most current treatments are associated with toxicities that require careful monitoring [29]. In addition, many patients are unable to tolerate the side effects or are unresponsive to standard therapies [39], which poses a significant therapeutic challenge to clinicians.
Acthar Gel
Acthar has been FDA-approved for use in patients with DM and PM since 1952 [40]; however, it is not routinely used in the treatment of IIMs [1]. Acthar is a naturally sourced complex mixture of adrenocorticotropic hormone (ACTH) analogs (a major component of which is ACTH1-39) and other pituitary peptides with a unique mechanism of action from standard of care therapies used to treat DM and PM [40]. It was originally thought that the anti-inflammatory effects of Acthar were mediated through glucocorticoid production (via activation of melanocortin receptor [MCR] 2 on adrenocortical cells), but recent studies have shown that glucocorticoid release from the adrenal cortex is relatively low with Acthar in both animals and humans, suggesting that it has a steroid-independent anti-inflammatory mechanism of action [41,42,43].
MCR agonists provide substantial anti-inflammatory and immunomodulatory effects. MCR activation inhibits nuclear factor-kappa B (NF-κB), which in turn functionally controls the expression of hundreds of genes including those that encode cytokines and their receptors, growth factors, and chemokines [44]. MC1R, MC3R, and MC5R are expressed in macrophages, B cells, and T cells and mediate anti-inflammatory and immunomodulatory properties of MCR agonists (Fig. 4) [41, 44,45,46]. Acthar has also been shown to have a direct immunomodulatory effect [41, 47, 48] via activation of MCRs, some of which are expressed on immune cells [41]. Acthar has been shown to inhibit antibody production and B cell proliferation [47] as well as inhibit inflammatory cytokine production from macrophages and T cells [48, 49].
Proposed mechanism of action of Acthar. Reproduced from Mirsaeidi M, Baughman RP. Repository corticotropin injection for the treatment of pulmonary sarcoidosis: a narrative review. Pulm Ther. 2022;8(1):43–55. doi:https://doi.org/10.1007/s41030-022-00181-0. under CC BY-NC 4.0 license terms. MCR indicates melanocortin receptor
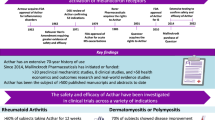
Although there have been no active-controlled studies comparing the efficacy of glucocorticoids to Acthar in DM or PM, some recent clinical trials, retrospective analyses, and case reports add to the growing body of evidence suggesting that Acthar may be effective in patients with DM and PM (Table 1). In a retrospective case review examining five patients with either DM or PM disease exacerbation who were unable to tolerate the side effects of previous therapies or in whom those therapies failed, patients received 80 U Acthar either twice weekly (n = 4) or once weekly (n = 1) for 12 weeks [50]. Improvements were observed in all patients, including increased muscle strength, decreased pain, and resolution of skin rashes in the patients with DM [50]. The success of Acthar in this small retrospective case review prompted the creation of the Acthar in Dermatomyositis and Polymyositis Treatment (ADAPT) registry in order to determine dosing, AEs, and efficacy of Acthar in patients with refractory DM or PM. An interim analysis (n = 24) showed that 58.3% of patients responded to Acthar treatment (80 IU twice weekly) as shown by improvement in inflammatory neuropathy cause and treatment (INCAT) score, manual muscle testing (MMT) scores, or Myositis Activity Profile (MAP) scores. Interestingly, the concomitant use of MMF was associated with 100% response rate (n = 5) [51].
The efficacy of Acthar (80 IU twice weekly) was also examined in a retrospective case series of four patients with DM or PM that was refractory to corticosteroids or other disease-modifying agents. Most patients experienced improvements in clinical laboratory measures, muscle strength, and pain. All patients were able to either decrease or stop glucocorticoid treatment following Acthar therapy [52]. In yet another retrospective analysis (n = 8) of Acthar use with doses varying between 40 IU once daily to 80 IU once a week up to 12 months in patients with DM and PM, 66.7% of patients improved based on physicians’ assessment of efficacy [53].
In a larger retrospective analysis of patients with rheumatologic diseases, Nelson et al. examined the medical records of 254 patients with either DM or PM [54]. They found that each patient used an average of 2.9 medications before initiation of Acthar therapy. Twenty-one percent of these patients received Acthar as a bridge to new therapy. The mean number of hospital admissions and hospitalization days was lower following Acthar administration, and the number of outpatient visits decreased by 26%. Of the patients who had information about medication access in their records, 26% faced obstacles to obtaining Acthar that were mostly insurance-related [54]. An economic US claims data analysis of patients with DM or PM between 2009 and 2014 found that total mean nonmedication costs were significantly lower in those receiving Acthar compared with IVIg (US $2126 vs. US $3964; p < 0.001), rituximab (US $2008 vs. US $2607; p = 0.018), or IVIg-rituximab (US $1234 vs. US $4858; p < 0.001) [35].
Ten patients with refractory DM or PM in whom glucocorticoids and/or ≥ 1 immunosuppressive agent failed and who had active disease completed the first open-label clinical trial to evaluate the efficacy, safety, and tolerability of Acthar [55]. All patients received 80 U Acthar twice weekly and were evaluated every 4 weeks for 24 weeks. Seventy percent of patients met the primary endpoint of the International Myositis Assessment and Clinical Studies (IMACS) definition of improvement as well as the ACR/EULAR response criteria, thus demonstrating a clinically significant response to Acthar (Fig. 5A and B). The addition of Acthar led to a reduction in prednisone dose (including in two patients with IMNM), and half of the patients were able to discontinue prednisone completely (Fig. 5C) [55]. Eight patients were included in a 6-month follow-up to the open-label clinical trial of Acthar. Four patients remained stable without additional therapy (including one patient who remained on Acthar following the trial), and four experienced a flare an average of 4.1 months after stopping Acthar. Three of the patients experiencing a flare required increases in prednisone, and one restarted Acthar at 5.5 months [56].

Reproduced from Aggarwal R, Marder G, Koontz DC, Nandkumar P, Qi Z, Oddis CV. Efficacy and safety of adrenocorticotropic hormone gel in refractory dermatomyositis and polymyositis. Ann Rheum Dis. 2018;77(5):720–727. DOI indicates definition of improvement
Primary outcome results as definition of improvement (DOI) A and secondary outcome results as 2016 American College of Rheumatology/European League Against Rheumatism myositis response criteria B. Changes in prednisone dose at baseline and 6-month follow-up C.
The most common and standard dose of Acthar that is used in myositis is 80 IU subcutaneously (SC), twice per week. This was based on previous studies on exacerbations of multiple sclerosis and nephrotic syndrome [57, 58]. There are no clear evidence or guidelines to follow for duration of therapy. The duration of Acthar therapy in the myositis studies ranged from 2 to 27 months [50,51,52,53,54,55,56]. The time needed to respond is highly variable and influenced by a variety of known and unknown factors, which may include disease type, severity, and concomitant therapy. Once a patient commits to treatment with Acthar, it should be continued for at least 3 months before considering it an efficacy failure. The interim analysis from the ADAPT registry reported that most patients responded within a mean of 90 days, and the patients who terminated therapy before this may have benefitted from continuation of their treatment [51]. Further studies delineating dose–response and duration relationships are required to consolidate the currently available evidence.
Regarding the steroid-sparing effects of Acthar, in the first case series of five patients, the mean (SD) reduction in dose of prednisone was –51.25 mg (37 mg) for four of the patients, two of whom were completely weaned off of steroids [50]. The fifth patient had only received 1 g intravenous methylprednisolone (IVMP) per week for 8 weeks prior to starting Acthar therapy and was able to be maintained off of IVMP [50]. In another series, two of the four patients were able to be weaned off of steroids, with a mean reduction in steroid dose from before Acthar therapy to after of –27.5 mg [52]. In the prospective trial, the mean prednisone dose significantly decreased from a baseline of 18.5 mg to a last follow-up dose of 2.3 mg (p < 0.01), with almost half of the patients weaned off of prednisone [50].
An open-label, randomized, crossover trial comparing IVMP with Acthar illustrated the different pharmacodynamic effects of the two drugs [59]. The study population, which included only healthy adults with no contraindications to steroid use, were randomized to receive either Acthar at 80 IU SC or 1 g of IVMP for a total of five consecutive days, followed by a washout period of 30 days, before crossing over to the other arm of the trial. The two drugs were considered equivalent at the given doses based on their use and similar efficacy in the treatment of multiple sclerosis flares [58]. Acthar at the given dose had a much lower serum cortisol-equivalent exposure and was deemed to be equivalent to 3% of 1 g IVMP. The effects on total peripheral lymphocyte and neutrophil count also mirror this discrepancy, with Acthar causing a lower decrease in lymphocyte counts and a lower increase in neutrophil count compared with IVMP [59]. This supports the possibility that Acthar acts via non-steroidogenic mechanisms to decrease inflammatory responses.
In all the studies mentioned, Acthar was generally safe and well tolerated. None of the five patients in the retrospective case series by Levine (2012) experienced any significant side effects from the treatment, including no changes in hemoglobin A1c (HbA1c) [50]. Patel et al. (2016) noted that Acthar did not exacerbate any of the patients' comorbidities, and there were no significant changes in blood pressure, weight, or glycemic control. However, one patient experienced mild weight gain, and one patient experienced blurry vision that resolved while on treatment [52]. In the retrospective medical record analysis by Ho-Mahler et al. (2020), one patient experienced bruising and red or bloodshot eyes and one patient experienced shortness of breath [53]. Also, 41.7% of patients from the ADAPT registry experienced mild-to-moderate AEs, the most common of which were increased HbA1c levels and edema [51]. In the open-label clinical trial, AEs were similar to those seen with glucocorticoids; however, significant weight gain, diabetes, or cushingoid features were not observed, and these are typically associated with long-term high steroid doses [55]. In the longitudinal follow-up study, the AEs remained mild to moderate and were consistent with previous reports [56].
Conclusions
Due to its unique immunomodulatory mechanism of action through the activation of MCRs, Acthar may provide an alternative treatment for patients who are unable to tolerate the side effects or are unresponsive to standard therapies for DM and PM. The retrospective analyses and open-label trial of Acthar suggest that it may be a safe and effective treatment for refractory DM and PM. Along with the fact that Acthar is already FDA-approved for use in patients with DM and PM, the favorable efficacy and safety profiles suggest that Acthar may be considered an alternative treatment for DM and PM.
References
Lundberg IE, Fujimoto M, Vencovsky J, Aggarwal R, Holmqvist M, Christopher-Stine L, et al. Idiopathic inflammatory myopathies. Nat Rev Dis Primers. 2021;7(1):86.
Dalakas MC. Inflammatory Muscle Diseases. N Engl J Med. 2015;373(4):393–4.
Muro Y, Sugiura K, Akiyama M. Cutaneous manifestations in dermatomyositis: key clinical and serological features-a comprehensive review. Clin Rev Allergy Immunol. 2016;51(3):293–302.
Klein M, Mann H, Vencovsky J. Arthritis in idiopathic inflammatory myopathies. Curr Rheumatol Rep. 2019;21(12):70.
Kiely PD, Chua F. Interstitial lung disease in inflammatory myopathies: clinical phenotypes and prognosis. Curr Rheumatol Rep. 2013;15(9):359.
Schwartz T, Diederichsen LP, Lundberg IE, Sjaastad I, Sanner H. Cardiac involvement in adult and juvenile idiopathic inflammatory myopathies. RMD Open. 2016;2(2): e000291.
Manfredi A, Sebastiani M, Cassone G, Pipitone N, Giuggioli D, Colaci M, et al. Nailfold capillaroscopic changes in dermatomyositis and polymyositis. Clin Rheumatol. 2015;34(2):279–84.
McHugh NJ, Tansley SL. Autoantibodies in myositis. Nat Rev Rheumatol. 2018;14(5):290–302.
Betteridge Z, McHugh N. Myositis-specific autoantibodies: an important tool to support diagnosis of myositis. J Intern Med. 2016;280(1):8–23.
Lundberg IE, Tjarnlund A, Bottai M, Werth VP, Pilkington C, Visser M, et al. 2017 European league against rheumatism/american college of rheumatology classification criteria for adult and juvenile idiopathic inflammatory myopathies and their major subgroups. Ann Rheum Dis. 2017;76(12):1955–64.
Barsotti S, Lundberg IE. Current treatment for myositis. Curr Treatm Opt Rheumatol. 2018;4(4):299–315.
Meyer A, Scire CA, Talarico R, Alexander T, Amoura Z, Avcin T, et al. Idiopathic inflammatory myopathies: state of the art on clinical practice guidelines [corrected]. RMD Open. 2018;4(Suppl 1): e000784.
Airio A, Kautiainen H, Hakala M. Prognosis and mortality of polymyositis and dermatomyositis patients. Clin Rheumatol. 2006;25(2):234–9.
Lundberg IE, Forbess CJ. Mortality in idiopathic inflammatory myopathies. Clin Exp Rheumatol. 2008;26(5 Suppl 51):S109–14.
Cox S, Limaye V, Hill C, Blumbergs P, Roberts-Thomson P. Idiopathic inflammatory myopathies: diagnostic criteria, classification and epidemiological features. Int J Rheum Dis. 2010;13(2):117–24.
Chinniah KJ, Mody GM. The spectrum of idiopathic inflammatory myopathies in South Africa. Clin Rheumatol. 2021;40(4):1437–46.
Essouma M, Noubiap JJ, Singwe-Ngandeu M, Hachulla E. Epidemiology of idiopathic inflammatory myopathies in Africa: a contemporary systematic review. J Clin Rheumatol. 2021. https://doi.org/10.1097/RHU.0000000000001736.
Smoyer-Tomic KE, Amato AA, Fernandes AW. Incidence and prevalence of idiopathic inflammatory myopathies among commercially insured, Medicare supplemental insured, and Medicaid enrolled populations: an administrative claims analysis. BMC Musculoskelet Disord. 2012;13:103.
Dalakas MC. Pathophysiology of inflammatory and autoimmune myopathies. Presse Med. 2011;40(4 Pt 2):e237–47.
Yang SH, Chang C, Lian ZX. Polymyositis and dermatomyositis - challenges in diagnosis and management. J Transl Autoimmun. 2019;2: 100018.
Dalakas MC, Hohlfeld R. Polymyositis and dermatomyositis. Lancet. 2003;362(9388):971–82.
Bottai M, Tjarnlund A, Santoni G, Werth VP, Pilkington C, de Visser M, et al. EULAR/ACR classification criteria for adult and juvenile idiopathic inflammatory myopathies and their major subgroups: a methodology report. RMD Open. 2017;3(2): e000507.
Lundberg IE, Miller FW, Tjarnlund A, Bottai M. Diagnosis and classification of idiopathic inflammatory myopathies. J Intern Med. 2016;280(1):39–51.
Franco C, Gatto M, Iaccarino L, Ghirardello A, Doria A. Lymphocyte immunophenotyping in inflammatory myositis: a review. Curr Opin Rheumatol. 2021;33(6):522–8.
Mescam-Mancini L, Allenbach Y, Hervier B, Devilliers H, Mariampillay K, Dubourg O, et al. Anti-Jo-1 antibody-positive patients show a characteristic necrotizing perifascicular myositis. Brain. 2015;138(Pt 9):2485–92.
Montagne JM, Zheng XA, Pinal-Fernandez I, Milisenda JC, Christopher-Stine L, Lloyd TE, et al. Ultra-efficient sequencing of T cell receptor repertoires reveals shared responses in muscle from patients with myositis. EBioMedicine. 2020;59: 102972.
Witt LJ, Curran JJ, Strek ME. The diagnosis and treatment of antisynthetase syndrome. Clin Pulm Med. 2016;23(5):218–26.
Dalakas MC, Alexopoulos H, Spaeth PJ. Complement in neurological disorders and emerging complement-targeted therapeutics. Nat Rev Neurol. 2020;16(11):601–17.
Oddis CV. Update on the pharmacological treatment of adult myositis. J Intern Med. 2016;280(1):63–74.
Oddis CV, Aggarwal R. Treatment in myositis. Nat Rev Rheumatol. 2018;14(5):279–89.
Hoes JN, Jacobs JW, Boers M, Boumpas D, Buttgereit F, Caeyers N, et al. EULAR evidence-based recommendations on the management of systemic glucocorticoid therapy in rheumatic diseases. Ann Rheum Dis. 2007;66(12):1560–7.
Oddis CV, Reed AM, Aggarwal R, Rider LG, Ascherman DP, Levesque MC, et al. Rituximab in the treatment of refractory adult and juvenile dermatomyositis and adult polymyositis: a randomized, placebo-phase trial. Arthritis Rheum. 2013;65(2):314–24.
Moghadam-Kia S, Aggarwal R, Oddis CV. Biologics for idiopathic inflammatory myopathies. Curr Opin Rheumatol. 2017;29(6):645–51.
Moghadam-Kia S, Oddis CV, Aggarwal R. Modern therapies for idiopathic inflammatory myopathies (IIMS): role of biologics. Clin Rev Allergy Immunol. 2017;52(1):81–7.
Philbin M, Niewoehner J, Wan GJ. Clinical and economic evaluation of repository corticotropin injection: a narrative literature review of treatment efficacy and healthcare resource utilization for seven key indications. Adv Ther. 2017;34(8):1775–90.
Giannini M, Fiorella ML, Tampoia M, Girolamo F, Fornaro M, Amati A, et al. Long-term efficacy of adding intravenous immunoglobulins as treatment of refractory dysphagia related to myositis: a retrospective analysis. Rheumatology (Oxford). 2021;60(3):1234–42.
Lim J, Eftimov F, Verhamme C, Brusse E, Hoogendijk JE, Saris CGJ, et al. Intravenous immunoglobulins as first-line treatment in idiopathic inflammatory myopathies: a pilot study. Rheumatology (Oxford). 2021;60(4):1784–92.
Aggarwal R, Charles-Schoeman C, Schessl J, Dimachkie MM, Beckmann I, Levine T. Prospective, double-blind, randomized, placebo-controlled phase III study evaluating efficacy and safety of octagam 10% in patients with dermatomyositis (“ProDERM Study”). Medicine (Baltimore). 2021;100(1): e23677.
Ytterberg SR. Treatment of refractory polymyositis and dermatomyositis. Curr Rheumatol Rep. 2006;8(3):167–73.
Acthar Gel [package insert]. Bedminster (NJ): Mallinckrodt ARD LLC; 2021.
Huang YJ, Galen K, Zweifel B, Brooks LR, Wright AD. Distinct binding and signaling activity of Acthar Gel compared to other melanocortin receptor agonists. J Recept Signal Transduct Res. 2021;41(5):425–33.
Wang X, Pham L, Poola N, Brooks LR, Due B. Comparison of steroidogenic exposure following the administration of repository corticotropin injection with a synthetic ACTH1-24 depot and methylprednisolone in healthy subjects. Clin Pharmacol Drug Dev. 2021;10(7):777–88.
Poola N, Due B, Wright D, Brooks LR, Zaman F. Pharmacokinetics and pharmacodynamics of repository corticotropin injection compared with synthetic ACTH1–24 depot and methylprednisolone in healthy subjects. Clin Pharmacol Drug Dev. 2021. https://doi.org/10.1002/cpdd.1020.
Catania A, Lonati C, Sordi A, Carlin A, Leonardi P, Gatti S. The melanocortin system in control of inflammation. ScientificWorldJournal. 2010;10:1840–53.
Catania A, Gatti S, Colombo G, Lipton JM. Targeting melanocortin receptors as a novel strategy to control inflammation. Pharmacol Rev. 2004;56(1):1–29.
Ahmed TJ, Montero-Melendez T, Perretti M, Pitzalis C. Curbing inflammation through endogenous pathways: focus on melanocortin peptides. Int J Inflam. 2013;2013: 985815.
Olsen NJ, Decker DA, Higgins P, Becker PM, McAloose CA, Benko AL, et al. Direct effects of HP Acthar Gel on human B lymphocyte activation in vitro. Arthritis Res Ther. 2015;17:300.
Wright D, Zweifel B, Sharma P, Galen K, Fitch R. Reduced steroidogenic activity of repository corticotropin injection (RCI) induces a distinct cytokine response following T cell activation in vivo (Abstract AB0082). Ann Rheum Dis. 2019;78:1504.
Healy LM, Jang JH, Lin YH, Rao V, Antel JP, Wright D. Melanocortin receptor mediated anti-inflammatory effect of repository corticotropin injection on human monocyte-derived macrophages. Multiple Sclerosis Journal. 2017;23(3_suppl):680–975.
Levine T. Treating refractory dermatomyositis or polymyositis with adrenocorticotropic hormone gel: a retrospective case series. Drug Des Devel Ther. 2012;6:133–9.
Levine T, Malone J, Efthimiou P, Tandan R, Dikranian A, Levine A, et al. HP Acthar® Gel in dermatomyositis and polymyositis treatment registry: an interim analysis. J Neurol Disord. 2016. https://doi.org/10.4172/2329-6895.1000292.
Patel A, Seely G, Aggarwal R. Repository corticotropin injection for treatment of idiopathic inflammatory myopathies. Case Rep Rheumatol. 2016;2016:9068061.
Ho-Mahler N, Turner B, Eaddy M, Hanke ML, Nelson WW. Treatment with repository corticotropin injection in patients with rheumatoid arthritis, systemic lupus erythematosus, and dermatomyositis/polymyositis. Open Access Rheumatol. 2020;12:21–8.
Nelson WW, Philbin MJ, Gallagher JR, Heap K, Carroll S, Wan GJ. A Retrospective medical record review of utilization patterns and medical resource use associated with repository corticotropin injection among patients with rheumatologic diseases in the united states. Rheumatol Ther. 2017;4(2):465–74.
Aggarwal R, Marder G, Koontz DC, Nandkumar P, Qi Z, Oddis CV. Efficacy and safety of adrenocorticotropic hormone gel in refractory dermatomyositis and polymyositis. Ann Rheum Dis. 2018;77(5):720–7.
Saygin D, Oddis CV, Marder G, Moghadam-Kia S, Nandkumar P, Neiman N, et al. Follow-up results of myositis patients treated with H. P Acthar gel Rheumatology (Oxford). 2020;59(10):2976–81.
Tumlin J, Galphin C, Santos R, Rovin B. Safety and efficacy of combination Acthar gel and tacrolimus in treatment-resistant focal segmental glomerulosclerosis and membranous glomerulopathy. Kidney Int Rep. 2017;2(5):924–32.
Wynn D, Goldstick L, Bauer W, Zhao E, Tarau E, Cohen JA, et al. Results from a multicenter, randomized, double-blind, placebo-controlled study of repository corticotropin injection for multiple sclerosis relapse that did not adequately respond to corticosteroids. CNS Neurosci Ther. 2022;28(3):364–71.
Lal R, Bell S, Challenger R, Hammock V, Nyberg M, Decker D, et al. Pharmacodynamics and tolerability of repository corticotropin injection in healthy human subjects: a comparison with intravenous methylprednisolone. J Clin Pharmacol. 2016;56(2):195–202.
Acknowledgements
Funding
This review paper and the journal’s Rapid Service Fee were funded by Mallinckrodt Pharmaceuticals, Hampton, NJ, USA.
Medical Writing/Editorial Assistance
Professional writing and editorial support were provided by Jennifer Ayala, PhD, of MedLogix Communications, LLC, Itasca, Illinois, under the direction of the authors and were funded by Mallinckrodt Pharmaceuticals.
Author Contributions
Tanya Chandra and Rohit Aggarwal both meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article and contributed to the conception or design of the work; acquisition, analysis, or interpretation of data; drafting or critically revising the work for important intellectual content; and final approval of the manuscript.
Disclosures
Tanya Chandra has no competing interests to declare. Rohit Aggarwal has received contracts for consultancy from Actigraph, Alexion, Argenx, AstraZeneca, Beigene, Bristol Myers Squibb, Boehringer Ingelheim, CSL Behring, Corbus, EMBD Serono, Galapagos, Horizontal Therapeutics, Janssen, Kezar, Kyverna, Mallinckrodt Pharmaceuticals, Merck, Octapharma, Pfizer, Roivant, Scipher, and Teva. He has also received research grants from Bristol Myers Squibb, EMD, Serono, Mallinckrodt Pharmaceuticals, Pfizer, and Q32.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Chandra, T., Aggarwal, R. A Narrative Review of Acthar Gel for the Treatment of Myositis. Rheumatol Ther 10, 523–537 (2023). https://doi.org/10.1007/s40744-023-00545-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-023-00545-1