Abstract
Context
In preclinical studies, high androgen levels during pregnancy are associated with low birth weight and rapid postnatal weight gain in the offspring. However, human data linking prenatal androgens with birth weight and early life weight gain in the offspring are scarce.
Design
We evaluated 516 mother–child pairs enrolled in the New England birth cohorts of the Collaborative Perinatal Project (1959–1966). We assayed androgen bioactivity in maternal sera during third-trimester using a receptor-mediated luciferase expression bioassay. Age and sex-specific BMI Z-scores (BMIz), defined using established standards, were assessed at birth, 4 months, 1 year, 4 years, and 7 years. We used linear mixed models to evaluate the relation of maternal androgens with childhood BMIz overall and by sex. We examined the association of maternal androgens with fetal growth restriction. The association of weight trajectories with maternal androgens was examined using multinomial logistic regression.
Results
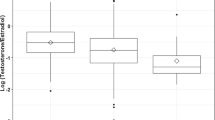
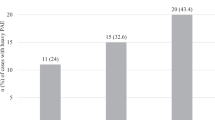
Higher maternal androgen levels associated with lower BMIz at birth (β = − 0.39, 95% CI: − 0.73, − 0.06); this relation was sex-dependent, such that maternal androgens significantly associated with BMIz at birth in girls alone (β = − 0.72, 95% CI: − 1.40, − 0.04). The relation of maternal androgens with fetal growth restriction revealed dose threshold effects that differed by sex. There was no significant association between maternal androgens and weight trajectory overall. However, we found a significant sex interaction (p = 0.01); higher maternal androgen levels associated with accelerated catch-up growth in boys (aOR = 2.14, 95% CI: 1.14, 4.03).
Conclusion
Our findings provide evidence that maternal androgens may have differential effects on the programming of intrauterine growth and postnatal weight gain depending on fetal sex.

Similar content being viewed by others
References
Ozanne SE (2001) Metabolic programming in animals. Br Med Bull 60:143–152
Barker DJ (2004) The developmental origins of chronic adult disease. Acta Paediatr 93(446):26–33
Goldstein JM, Hale T, Foster SL, Tobet SA, Handa RJ (2019) Sex differences in major depression and comorbidity of cardiometabolic disorders: impact of prenatal stress and immune exposures. Neuropsychopharmacology 44(1):59–70. https://doi.org/10.1038/s41386-018-0146-1
Stavreva DA, George AA, Klausmeyer P, Varticovski L, Sack D, Voss TC, Schiltz RL, Blazer VS, Iwanowicz LR, Hager GL (2012) Prevalent glucocorticoid and androgen activity in US water sources. Sci Rep 2:937. https://doi.org/10.1038/srep00937
Cho J, Holditch-Davis D (2014) Effects of perinatal testosterone on infant health, mother-infant interactions, and infant development. Biol Res Nurs 16(2):228–236. https://doi.org/10.1177/1099800413486340
Bruns CM, Baum ST, Colman RJ, Eisner JR, Kemnitz JW, Weindruch R, Abbott DH (2004) Insulin resistance and impaired insulin secretion in prenatally androgenized male rhesus monkeys. J Clin Endocrinol Metab 89(12):6218–6223. https://doi.org/10.1210/jc.2004-0918
Eisner JR, Dumesic DA, Kemnitz JW, Abbott DH (2000) Timing of prenatal androgen excess determines differential impairment in insulin secretion and action in adult female rhesus monkeys. J Clin Endocrinol Metab 85(3):1206–1210. https://doi.org/10.1210/jcem.85.3.6453
Huang G, Cherkerzian S, Loucks EB, Buka SL, Handa RJ, Lasley BL, Bhasin S, Goldstein JM (2018) Sex differences in the prenatal programming of adult metabolic syndrome by maternal androgens. J Clin Endocrinol Metab 103(11):3945–3953. https://doi.org/10.1210/jc.2018-01243
Ong KK, Dunger DB (2002) Perinatal growth failure: the road to obesity, insulin resistance and cardiovascular disease in adults. Best Pract Res Clin Endocrinol Metab 16(2):191–207. https://doi.org/10.1053/beem.2002.0195
Jornayvaz FR, Vollenweider P, Bochud M, Mooser V, Waeber G, Marques-Vidal P (2016) Low birth weight leads to obesity, diabetes and increased leptin levels in adults: the CoLaus study. Cardiovasc Diabetol 15:73. https://doi.org/10.1186/s12933-016-0389-2
Fall CH, Osmond C, Barker DJ, Clark PM, Hales CN, Stirling Y, Meade TW (1995) Fetal and infant growth and cardiovascular risk factors in women. BMJ 310(6977):428–432. https://doi.org/10.1136/bmj.310.6977.428
Lauren L, Jarvelin MR, Elliott P, Sovio U, Spellman A, McCarthy M, Emmett P, Rogers I, Hartikainen AL, Pouta A, Hardy R, Wadsworth M, Helmsdal G, Olsen S, Bakoula C, Lekea V, Millwood I (2003) Relationship between birthweight and blood lipid concentrations in later life: evidence from the existing literature. Int J Epidemiol 32(5):862–876. https://doi.org/10.1093/ije/dyg201
Mi J, Law C, Zhang KL, Osmond C, Stein C, Barker D (2000) Effects of infant birthweight and maternal body mass index in pregnancy on components of the insulin resistance syndrome in China. Ann Intern Med 132(4):253–260. https://doi.org/10.7326/0003-4819-132-4-200002150-00002
Eriksson JG, Forsen T, Tuomilehto J, Jaddoe VW, Osmond C, Barker DJ (2002) Effects of size at birth and childhood growth on the insulin resistance syndrome in elderly individuals. Diabetologia 45(3):342–348. https://doi.org/10.1007/s00125-001-0757-6
Forsen T, Eriksson J, Tuomilehto J, Reunanen A, Osmond C, Barker D (2000) The fetal and childhood growth of persons who develop type 2 diabetes. Ann Intern Med 133(3):176–182. https://doi.org/10.7326/0003-4819-133-3-200008010-00008
Ong KK, Ahmed ML, Emmett PM, Preece MA, Dunger DB (2000) Association between postnatal catch-up growth and obesity in childhood: prospective cohort study. BMJ 320(7240):967–971
Steckler T, Wang J, Bartol FF, Roy SK, Padmanabhan V (2005) Fetal programming: prenatal testosterone treatment causes intrauterine growth retardation, reduces ovarian reserve and increases ovarian follicular recruitment. Endocrinology 146(7):3185–3193. https://doi.org/10.1210/en.2004-1444
Sathishkumar K, Elkins R, Chinnathambi V, Gao H, Hankins GD, Yallampalli C (2011) Prenatal testosterone-induced fetal growth restriction is associated with down-regulation of rat placental amino acid transport. Reprod Biol Endocrinol RB&E 9:110. https://doi.org/10.1186/1477-7827-9-110
Sathishkumar K, Elkins R, Yallampalli U, Balakrishnan M, Yallampalli C (2011) Fetal programming of adult hypertension in female rat offspring exposed to androgens in utero. Early Human Dev 87(6):407–414. https://doi.org/10.1016/j.earlhumdev.2011.03.001
Manikkam M, Crespi EJ, Doop DD, Herkimer C, Lee JS, Yu S, Brown MB, Foster DL, Padmanabhan V (2004) Fetal programming: prenatal testosterone excess leads to fetal growth retardation and postnatal catch-up growth in sheep. Endocrinology 145(2):790–798. https://doi.org/10.1210/en.2003-0478
Wolf CJ, Hotchkiss A, Ostby JS, LeBlanc GA, Gray LE Jr (2002) Effects of prenatal testosterone propionate on the sexual development of male and female rats: a dose-response study. Toxicol Sci Off J Soc Toxicol 65(1):71–86
Sir-Petermann T, Hitchsfeld C, Maliqueo M, Codner E, Echiburu B, Gazitua R, Recabarren S, Cassorla F (2005) Birth weight in offspring of mothers with polycystic ovarian syndrome. Hum Reprod 20(8):2122–2126. https://doi.org/10.1093/humrep/dei009
Bastek JA, Pare E, Wang E, Elovitz MA, Srinivas SK (2009) Limitations of ultrasound in diagnosing intrauterine growth restriction in severe preeclampsia. J Matern-Fetal Neonatal Med Off J Eur Assoc Perinat Med Fed Asia Ocean Perinat Soc Int Soc Perinat Obstet 22(11):1039–1044. https://doi.org/10.3109/14767050903029584
Recabarren SE, Smith R, Rios R, Maliqueo M, Echiburu B, Codner E, Cassorla F, Rojas P, Sir-Petermann T (2008) Metabolic profile in sons of women with polycystic ovary syndrome. J Clin Endocrinol Metab 93(5):1820–1826. https://doi.org/10.1210/jc.2007-2256
Torchen LC, Idkowiak J, Fogel NR, O'Neil DM, Shackleton CH, Arlt W, Dunaif A (2016) Evidence for increased 5alpha-reductase activity during early childhood in daughters of women with polycystic ovary syndrome. J Clin Endocrinol Metab 101(5):2069–2075. https://doi.org/10.1210/jc.2015-3926
Krone N, Wachter I, Stefanidou M, Roscher AA, Schwarz HP (2001) Mothers with congenital adrenal hyperplasia and their children: outcome of pregnancy, birth and childhood. Clin Endocrinol (Oxf) 55(4):523–529. https://doi.org/10.1046/j.1365-2265.2001.01359.x
Remde H, Zopf K, Schwander J, Quinkler M (2016) Fertility and pregnancy in primary adrenal insufficiency in Germany. Horm Metab Res 48(5):306–311. https://doi.org/10.1055/s-0035-1565183
Reisch N (2019) Pregnancy in congenital adrenal hyperplasia. Endocrinol Metab Clin North Am 48(3):619–641. https://doi.org/10.1016/j.ecl.2019.05.011
Lo JC, Schwitzgebel VM, Tyrrell JB, Fitzgerald PA, Kaplan SL, Conte FA, Grumbach MM (1999) Normal female infants born of mothers with classic congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Clin Endocrinol Metab 84(3):930–936. https://doi.org/10.1210/jcem.84.3.5565
Hagenfeldt K, Janson PO, Holmdahl G, Falhammar H, Filipsson H, Frisen L, Thoren M, Nordenskjold A (2008) Fertility and pregnancy outcome in women with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Hum Reprod 23(7):1607–1613. https://doi.org/10.1093/humrep/den118
Reynolds RM, Seckl JR (2012) Antenatal glucocorticoid treatment: are we doing harm to term babies? J Clin Endocrinol Metab 97(10):3457–3459. https://doi.org/10.1210/jc.2012-3201
Takishima S, Nakajima K, Nomura R, Tsuji-Hosokawa A, Matsuda N, Matsubara Y, Ono M, Miyai K, Takasawa K, Morio T, Hasegawa Y, Kashimada K (2016) Lower body weight and BMI at birth were associated with early adiposity rebound in 21-hydroxylase deficiency patients. Endocr J 63(11):983–990. https://doi.org/10.1507/endocrj.EJ16-0194
Kung KTF, Spencer D, Pasterski V, Neufeld SAS, Hindmarsh PC, Hughes IA, Acerini CL, Hines M (2018) Emotional and behavioral adjustment in 4 to 11-year-old boys and girls with classic congenital adrenal hyperplasia and unaffected siblings. Psychoneuroendocrinology 97:104–110. https://doi.org/10.1016/j.psyneuen.2018.07.004
Sathishkumar K, Balakrishnan M, Chinnathambi V, Chauhan M, Hankins GD, Yallampalli C (2012) Fetal sex-related dysregulation in testosterone production and their receptor expression in the human placenta with preeclampsia. J Perinatol 32(5):328–335. https://doi.org/10.1038/jp.2011.101
Susser E, Buka S, Schaefer CA, Andrews H, Cirillo PM, Factor-Litvak P, Gillman M, Goldstein JM, Henry PI, Lumey LH, McKeague IW, Michels KB, Terry MB, Cohn BA, for the EDAH Team (2011) The early determinants of adult health study. J Dev Origins Health Dis 2(6):311–321
Niswander KRG (1972) The collaborative perinatal study of the national institute of neurological diseases and stroke: the women and their pregnancies. Department of health, Education and Welfare, Washington
Goldstein JM, Buka SL, Seidman LJ, Tsuang MT (2010) Specificity of familial transmission of schizophrenia psychosis spectrum and affective psychoses in the New England family study’s high-risk design. Arch Gen Psychiatry 67(5):458–467. https://doi.org/10.1001/archgenpsychiatry.2010.38
Ellman LM, Schetter CD, Hobel CJ, Chicz-Demet A, Glynn LM, Sandman CA (2008) Timing of fetal exposure to stress hormones: effects on newborn physical and neuromuscular maturation. Dev Psychobiol 50(3):232–241. https://doi.org/10.1002/dev.20293
Yeh S, Chang C (1996) Cloning and characterization of a specific coactivator, ARA70, for the androgen receptor in human prostate cells. Proc Natl Acad Sci USA 93(11):5517–5521. https://doi.org/10.1073/pnas.93.11.5517
Chen J, Sowers MR, Moran FM, McConnell DS, Gee NA, Greendale GA, Whitehead C, Kasim-Karakas SE, Lasley BL (2006) Circulating bioactive androgens in midlife women. J Clin Endocrinol Metab 91(11):4387–4394. https://doi.org/10.1210/jc.2006-0284
de Onis M, Habicht JP (1996) Anthropometric reference data for international use: recommendations from a World Health Organization Expert Committee. Am J Clin Nutr 64(4):650–658. https://doi.org/10.1093/ajcn/64.4.650
Grummer-Strawn LM, Reinold C, Krebs NF, Centers for Disease C, Prevention (2010) Use of World Health Organization and CDC growth charts for children aged 0–59 months in the United States. MMWR Recomm Rep 59(RR-9):1–15
Oken E, Kleinman KP, Rich-Edwards J, Gillman MW (2003) A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatr 3:6. https://doi.org/10.1186/1471-2431-3-6
Nagin DS, Odgers CL (2010) Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol 6:109–138. https://doi.org/10.1146/annurev.clinpsy.121208.131413
Nagin DS (2005) Group based modeling of development. Harvard University Press, Cambridge
van de Schoot RSM, Winter SD, Depaoli S, Vermunt JK (2017) The GRoLTS-checklist: guidelines for reporting on latent trajectory studies. Struct Equ Model Multidiscip J 24(3):451–467
Jones BLND, Roeder K (2001) A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res 29:374–393
Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, Mei Z, Curtin LR, Roche AF, Johnson CL (2000) CDC growth charts: United States. Adv Data 314:1–27
de Zegher F, Devlieger H, Eeckels R (1999) Fetal growth: boys before girls. Horm Res 51(5):258–259. https://doi.org/10.1159/000023382
Makieva S, Saunders PT, Norman JE (2014) Androgens in pregnancy: roles in parturition. Human Reprod Update 20(4):542–559. https://doi.org/10.1093/humupd/dmu008
Hotchkiss AK, Lambright CS, Ostby JS, Parks-Saldutti L, Vandenbergh JG, Gray LE Jr (2007) Prenatal testosterone exposure permanently masculinizes anogenital distance, nipple development, and reproductive tract morphology in female Sprague-Dawley rats. Toxicol Sci Off J Soc Toxicol 96(2):335–345. https://doi.org/10.1093/toxsci/kfm002
Serin IS, Kula M, Basbug M, Unluhizarci K, Gucer S, Tayyar M (2001) Androgen levels of preeclamptic patients in the third trimester of pregnancy and six weeks after delivery. Acta Obstet Gynecol Scand 80(11):1009–1013
Salamalekis E, Bakas P, Vitoratos N, Eleptheriadis M, Creatsas G (2006) Androgen levels in the third trimester of pregnancy in patients with preeclampsia. Eur J Obstet Gynecol Reprod Biol 126(1):16–19. https://doi.org/10.1016/j.ejogrb.2005.07.007
Carlsen SM, Jacobsen G, Romundstad P (2006) Maternal testosterone levels during pregnancy are associated with offspring size at birth. Eur J Endocrinol Eur Fed Endocrine Soc 155(2):365–370. https://doi.org/10.1530/eje.1.02200
Voegtline KM, Costigan KA, Kivlighan KT, Henderson JL, DiPietro JA (2013) Sex-specific associations of maternal prenatal testosterone levels with birth weight and weight gain in infancy. J Dev Orig Health Dis 4(4):280–284. https://doi.org/10.1017/S2040174413000135
Padmanabhan V, Veiga-Lopez A, Abbott DH, Recabarren SE, Herkimer C (2010) Developmental programming: impact of prenatal testosterone excess and postnatal weight gain on insulin sensitivity index and transfer of traits to offspring of overweight females. Endocrinology 151(2):595–605. https://doi.org/10.1210/en.2009-1015
Gilman SE, Cherkerzian S, Buka SL, Hahn J, Hornig M, Goldstein JM (2016) Prenatal immune programming of the sex-dependent risk for major depression. Trans Psychiatry 6(5):e822. https://doi.org/10.1038/tp.2016.91
Stettler N, Zemel BS, Kumanyika S, Stallings VA (2002) Infant weight gain and childhood overweight status in a multicenter, cohort study. Pediatrics 109(2):194–199. https://doi.org/10.1542/peds.109.2.194
Eriksson JG, Forsen TJ (2002) Childhood growth and coronary heart disease in later life. Ann Med 34(3):157–161
Holt RI (2002) Fetal programming of the growth hormone-insulin-like growth factor axis. Trends Endocrinol Metab 13(9):392–397. https://doi.org/10.1016/s1043-2760(02)00697-5
Crespi EJ, Steckler TL, Mohankumar PS, Padmanabhan V (2006) Prenatal exposure to excess testosterone modifies the developmental trajectory of the insulin-like growth factor system in female sheep. J Physiol 572(Pt 1):119–130. https://doi.org/10.1113/jphysiol.2005.103929
Carbone DL, Zuloaga DG, Hiroi R, Foradori CD, Legare ME, Handa RJ (2012) Prenatal dexamethasone exposure potentiates diet-induced hepatosteatosis and decreases plasma IGF-I in a sex-specific fashion. Endocrinology 153(1):295–306. https://doi.org/10.1210/en.2011-1601
Hsu TY, Lan KC, Tsai CC, Ou CY, Cheng BH, Tsai MY, Kang HY, Tung YH, Wong YH, Huang KE (2009) Expression of androgen receptor in human placentas from normal and preeclamptic pregnancies. Taiwan J Obstet Gynecol 48(3):262–267. https://doi.org/10.1016/S1028-4559(09)60301-6
Gopalakrishnan K, Mishra JS, Chinnathambi V, Vincent KL, Patrikeev I, Motamedi M, Saade GR, Hankins GD, Sathishkumar K (2016) Elevated testosterone reduces uterine blood flow, spiral artery elongation, and placental oxygenation in pregnant rats. Hypertension 67(3):630–639. https://doi.org/10.1161/HYPERTENSIONAHA.115.06946
Carlson HE (2007) Human adrenal cortex hyperfunction due to LH/hCG. Mol Cell Endocrinol 269(1–2):46–50. https://doi.org/10.1016/j.mce.2006.06.014
Moran FM, Chen J, Gee NA, Lohstroh PN, Lasley BL (2013) Dehydroepiandrosterone sulfate levels reflect endogenous luteinizing hormone production and response to human chorionic gonadotropin challenge in older female macaque (Macaca fascicularis). Menopause 20(3):329–335. https://doi.org/10.1097/GME.0b013e3182698f80
Stroud LR, Solomon C, Shenassa E, Papandonatos G, Niaura R, Lipsitt LP, Lewinn K, Buka SL (2007) Long-term stability of maternal prenatal steroid hormones from the National Collaborative Perinatal Project: still valid after all these years. Psychoneuroendocrinology 32(2):140–150. https://doi.org/10.1016/j.psyneuen.2006.11.008
Furui T, Imai A, Ohno T (2007) Pre-term labour in cases with high maternal testosterone levels. J Obstet Gynaecol J Inst Obstet Gynaecol 27(2):155–156. https://doi.org/10.1080/01443610601113979
von Hippel PT, Nahhas RW (2013) Extending the history of child obesity in the United States: the Fels longitudinal study, birth years 1930–1993. Obesity (Silver Spring) 21(10):2153–2156. https://doi.org/10.1002/oby.20395
Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC (2018) Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics. https://doi.org/10.1542/peds.2017-3459
Phipps SA, Burton PS, Osberg LS, Lethbridge LN (2006) Poverty and the extent of child obesity in Canada, Norway and the United States. Obes Rev 7(1):5–12. https://doi.org/10.1111/j.1467-789X.2006.00217.x
Acknowledgements
We thank Anne Remington for help with project management. We also thank Nancy Gee at U.C. Davis with Dr. Lasley’s laboratory for performing the bioactive androgen assays for this study.
Funding
National Institute of Health/National Heart, Lung, and Blood Institute (NIH/NHLBI) K08 HL132122-02 (Huang, PI); State of Arizona Arizona Biomedical Research Commission (ABRC) ADHS14-00003606 (Handa/Goldstein, PIs), NIMH-NHLBI R01MH074679 (Goldstein, PI), NIA RC2AG036666 (Loucks and Buka, PIs), and NIA R01AG023397 (Buka, PI). Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (Gilman).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Shalender Bhasin (SB) has received research grant support from Abbvie Pharmaceuticals, Transition Therapeutics, and Metro International Biotechnology, LLC for investigator-initiated research unrelated to this study. SB has served as a consultant to AbbVie and Novartis. SB has a financial interest in Function Promoting Therapies, LLC, a company aiming to develop innovative solutions that enhance precision and accuracy in clinical decision-making and facilitate personalized therapeutic choices in reproductive health. SB’s interests were reviewed and are managed by Brigham and Women’s Hospital and Partners HealthCare in accordance with their conflict of interest policies. Dr. Goldstein is on the scientific advisory board for and has equity in Cala Health. However, this study has no relationship to the work in Cala Health. The rest of the authors have no conflicts of interest to disclose.
Ethical approval
The study protocol was approved by the institutional review boards at Partners HealthCare system and Brown University.
Informed consent
All participants provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, G., Aroner, S., Bay, C. et al. Sex-dependent associations of maternal androgen levels with offspring BMI and weight trajectory from birth to early childhood. J Endocrinol Invest 44, 851–863 (2021). https://doi.org/10.1007/s40618-020-01385-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-020-01385-4