Abstract
Background
One-carbon metabolism genes are linked to several cancers, but the association with prostate cancer (PCa) is less clear. Studies examining the relationship have not accounted for obesity, a risk factor for advanced PCa and altered methylation patterns. We hypothesized that obesity could moderate the association between one-carbon metabolism genes and PCa outcomes.
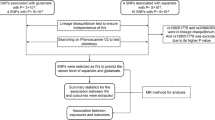
Methods
We conducted secondary data analyses of the Study of Clinical Outcomes, Risk and Ethnicity. Obesity was included as a primary exposure and modifier (interacting with genetic polymorphisms) in the analytic models. We used logistic regression to determine associations of common one-carbon metabolism genotypes with odds of high stage (T3/T4) and high grade (Gleason score ≥ 7). We used Cox regression to examine associations of genotypes with biochemical recurrence.
Results
There were 808 patients (632 White and 176 Black.) Among White men, we observed associations of TCN2_R259P with increased odds of high stage (OR = 0.64, 95% CI = 0.41–1.00), but no significant interactions with obesity. Among Black men, the SCL19A1_61bpdel and CBS_68bpINS variants were associated with high grade (OR = 2.61, 95% CI = 1.39–4.89 and OR = 0.29, 95% CI = 0.09–0.91, respectively.) Both the CBS_68bpINS and MTHFR_E429A variants interacted with obesity in Black men, where the highest risk for biochemical failure and odds of high grade, respectively, occurred among obese patients with variants.
Conclusions
We observed associations of one-carbon metabolism genes with different associations by race. We also observed interactions with obesity related to PCa outcomes in Black men only. Therefore, the involvement of one-carbon metabolism on PCa was dependent upon obesity status for Black men. These novel results could help identify patients that might benefit from effective weight management targeting one-carbon metabolism effects.



Similar content being viewed by others
Data Availability
Data can be obtained by contacting the corresponding author or director of the SCORE Study, Dr. Timothy Rebbeck (Harvard University).
References
ACS: Cancer facts and figures 2019. In. Atlanta: American Cancer Society; 2019. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-factsfigures-2019.html. Accessed 2020
Cancer Stat facts: lung and bronchus cancer https://seer.cancer.gov/statfacts/html/lungb.html. Accessed 2020
Wu Y, Sarkissyan M, Vadgama JV. Epigenetics in breast and prostate cancer. Methods Mol Biol. 2015;1238:425–66.
Singh S, Plaga A, Shukla GC. Racial disparities: disruptive genes in prostate carcinogenesis. Front Biosci. 2017;9:244–53.
Freedland SJ, Isaacs WB. Explaining racial differences in prostate cancer in the United States: sociology or biology? Prostate. 2005;62(3):243–52.
Zhang S, Lin J, Jiang J, Chen Y, Tang W, Liu L. Association between methylenetetrahydrofolate reductase tagging polymorphisms and susceptibility of hepatocellular carcinoma: a case-control study. Biosci Rep. 2019. https://doi.org/10.1042/BSR20192517.
Figueiredo JC, Levine AJ, Crott JW, Baurley J, Haile RW. Folate-genetics and colorectal neoplasia: what we know and need to know next. Mol Nutr Food Res. 2013;57(4):607–27.
Kim YI. Role of the MTHFR polymorphisms in cancer risk modification and treatment. Future Oncol. 2009;5(4):523–42.
Luo WP, Li B, Lin FY, Yan B, Du YF, Mo XF, et al. Joint effects of folate intake and one-carbon-metabolizing genetic polymorphisms on breast cancer risk: a case-control study in China. Sci Rep. 2016;6:29555.
Stevens VL, Rodriguez C, Sun J, Talbot JT, Thun MJ, Calle EE. No association of single nucleotide polymorphisms in one-carbon metabolism genes with prostate cancer risk. Cancer Epidemiol Biomark Prev. 2008;17(12):3612–4.
Abedinzadeh M, Zare-Shehneh M, Neamatzadeh H, Abedinzadeh M, Karami H. Association between MTHFR C677T polymorphism and risk of prostate cancer: evidence from 22 studies with 10,832 cases and 11,993 controls. Asian Pac J Cancer Prev. 2015;16(11):4525–30.
Fard-Esfahani P, Mohammadi Torbati P, Hashemi Z, Fayaz S, Golkar M. Analysis of relation between C677T genotype in MTHFR gene and prostatic cancer in Iranian males. Acta Med Iran. 2012;50(10):657–63.
Jackson MD, Tulloch-Reid MK, McFarlane-Anderson N, Watson A, Seers V, Bennett FI, et al. Complex interaction between serum folate levels and genetic polymorphisms in folate pathway genes: biomarkers of prostate cancer aggressiveness. Genes Nutr. 2013;8(2):199–207.
Herman M, Raman J, Dong S, Samadi D, Scherr D. Increasing body mass index negatively impacts outcomes following robotic radical prostatectomy. J Soc Laparoendosc Surg. 2007;11:438–42.
Calle E, Kaaks R. Overweight, Obesity and Cancer: epidemiological evidence and proposed mechanisms. Nat Rev. 2004;4:579–91.
Demark-Wahnefried W, Rais-Bahrami S, Desmond RA, Gordetsky JB, Hunter GR, Yang ES, et al. Presurgical weight loss affects tumour traits and circulating biomarkers in men with prostate cancer. Br J Cancer. 2017;117(9):1303–13.
Rodriguez C, Freedland S, Deka A, Jacobs E, McCullough M, Patel A, et al. Body mass index, weight change, and risk of prostate cancer in the Cancer Prevention Study II Nutrition Cohort. Cancer Epidemiol Biomark Prev. 2007;161(1):63–9.
Spangler E, Zeigler-Johnson C, Coomes M, Malkowicz S, Wein A, Rebbeck T. Association of obesity with tumor characteristics and treatment failure of prostate cancer in African-American and European American men. J Urol. 2007;178:1939–45.
Amling C, Riffenburgh R, Sun L, Moul J, Lance R, Kusuda L, et al. Pathologic variables and recurrence rates as related to obesity and race in men with prostate cancer undergoing radical prostatectomy. J Clin Oncol. 2004;22(3):439–45.
Freedland S, Terris M, Presti J Jr, Amling C, Kane C, Trock B, et al. Obesity and biochemical outcome following radical prostatectomy for organ confined disease with negative surgical margins. J Urol. 2004;172(2):520–4.
Zeigler-Johnson C, Spangler E, Jalloh M, Gueye S, Rennert H, Rebbeck T. Genetic susceptibility to prostate cancer in men of African descent: implications for global disparities in incidence and outcomes. Can J Urol. 2007;15(1):3872–82.
Bassett W, Cooperberg M, Sadetsky N, Silvia S, DuChane J, Pasta D, et al. Impact of obesity on prostate cancer recurrence after radical prostatectomy: Data from CaPSURE. Urology. 2005;66:1060–5.
Rebbeck TR, Weber AL, Walker AH, Stefflova K, Tran TV, Spangler E, et al. Context-dependent effects of genome-wide association study genotypes and macroenvironment on time to biochemical (prostate specific antigen) failure after prostatectomy. Cancer Epidemiol Biomark Prev. 2010;19(9):2115–23.
Zeigler-Johnson C, Morales KH, Spangler E, Chang BL, Rebbeck TR. Relationship of early-onset baldness to prostate cancer in African-American men. Cancer Epidemiol Biomark Prev. 2013;22(4):589–96.
Chen XL, Wang YM, Zhao F, Chen Z, Yang X, Sun C, et al. Methylenetetrahydrofolate reductase polymorphisms and colorectal cancer prognosis: a meta-analysis. J Gene Med. 2019;21(9):e3114.
Collin SM, Metcalfe C, Zuccolo L, Lewis SJ, Chen L, Cox A, et al. Association of folate-pathway gene polymorphisms with the risk of prostate cancer: a population-based nested case-control study, systematic review, and meta-analysis. Cancer Epidemiol Biomark Prev. 2009;18(9):2528–39.
Collin SM. Folate and B12 in prostate cancer. Adv Clin Chem. 2013;60:1–63.
Qu YY, Zhou SX, Zhang X, Zhao R, Gu CY, Chang K, et al. Functional variants of the 5-methyltetrahydrofolate-homocysteine methyltransferase gene significantly increase susceptibility to prostate cancer: results from an ethnic Han Chinese population. Sci Rep. 2016;6:36264.
Zhang X, Tang J, Shen N, Ren K. A single-nucleotide polymorphism (rs1805087) in the methionine synthase (METH) gene increases the risk of prostate cancer. Aging. 2018;10(10):2741–54.
Lin VC, Lu TL, Yin HL, Yang SF, Lee YC, Liu CC, et al. Prognostic relevance of methylenetetrahydrofolate reductase polymorphisms for prostate cancer. Int J Mol Sci. 2016;17(12). https://doi.org/10.3390/ijms17121996.
Tsai MY, Bignell M, Schwichtenberg K, Hanson NQ. High prevalence of a mutation in the cystathionine beta-synthase gene. Am J Hum Genet. 1996;59(6):1262–7.
Romano M, Marcucci R, Buratti E, Ayala YM, Sebastio G, Baralle FE. Regulation of 3′ splice site selection in the 844ins68 polymorphism of the cystathionine Beta -synthase gene. J Biol Chem. 2002;277(46):43821–9.
Tsai MY, Yang F, Bignell M, Aras O, Hanson NQ. Relation between plasma homocysteine concentration, the 844ins68 variant of the cystathionine beta-synthase gene, and pyridoxal-5′-phosphate concentration. Mol Genet Metab. 1999;67(4):352–6.
Levine AJ, Siegmund KD, Ervin CM, Diep A, Lee ER, Frankl HD, et al. The methylenetetrahydrofolate reductase 677C-->T polymorphism and distal colorectal adenoma risk. Cancer Epidemiol Biomark Prev. 2000;9(7):657–63.
Lopez-Cortes A, Cabrera-Andrade A, Salazar-Ruales C, Zambrano AK, Guerrero S, Guevara P, et al. Genotyping the high altitude mestizo ecuadorian population affected with prostate cancer. Biomed Res Int. 2017;2017:3507671.
Friedman G, Goldschmidt N, Friedlander Y, Ben-Yehuda A, Selhub J, Babaey S, et al. A common mutation A1298C in human methylenetetrahydrofolate reductase gene: association with plasma total homocysteine and folate concentrations. J Nutr. 1999;129(9):1656–61.
Kwabi-Addo B, Wang S, Chung W, Jelinek J, Patierno SR, Wang BD, et al. Identification of differentially methylated genes in normal prostate tissues from African American and Caucasian men. Clin Cancer Res. 2010;16(14):3539–47.
Wang S, Dorsey TH, Terunuma A, Kittles RA, Ambs S, Kwabi-Addo B. Relationship between tumor DNA methylation status and patient characteristics in African-American and European-American women with breast cancer. PLoS One. 2012;7(5):e37928.
Devaney JM, Wang S, Funda S, Long J, Taghipour DJ, Tbaishat R, et al. Identification of novel DNA-methylated genes that correlate with human prostate cancer and high-grade prostatic intraepithelial neoplasia. Prostate Cancer Prostatic Dis. 2013;16(4):292–300.
Gohlke JH, Lloyd SM, Basu S, Putluri V, Vareed SK, Rasaily U, et al. Methionine-homocysteine pathway in African-American prostate cancer. JNCI Cancer Spectr. 2019;3(2):pkz019.
Gross M, Ramirez C, Luthringer D, Nepomuceno E, Vollmer R, Burchette J, et al. Expression of androgen and estrogen related proteins in normal weight and obese prostate cancer patients. Prostate. 2009;69:520–7.
Freedland S, Banez L, Sun L, Fitzsimons N, Moul J. Obese men have higher-grade and larger tumors: an analysis of the Duke Prostate Center database. Prostate Cancer Prostatic Dis. 2009;12:259–63.
Al-Bayyari N, Hamadneh J, Hailat R, Hamadneh S. Total homocysteine is positively correlated with body mass index, waist-to-hip ratio, and fat mass among overweight reproductive women: a cross-sectional study. Nutr Res. 2017;48:9–15.
Fowke JH, Motley SS. Statin use linked with a decrease in the conversion from high-grade prostatic intraepithelial neoplasia (HGPIN) to prostate cancer. Carcinogenesis. 2018;39(6):819–25.
Acknowledgments
We would like to thank Dr. Timothy R. Rebbeck (Dana Farber Cancer Institute) for providing access to data from the SCORE study.
Funding
This study was funded by the Pennsylvania (PA) Department of Health. However, the PA Department of Health did not play a role in the study design, analysis, interpretation of results, or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
SK assisted with drafting the manuscript, data analysis and interpretation, and manuscript revisions.
BKA contributed to the manuscript draft and revisions.
CZJ acquired data, was responsible for the study concept/design, analysis, and interpretation, and drafted the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethics Approval and Consent to Participate
This observational study based upon secondary data analysis of the Study of Clinical Outcomes, Risk and Ethnicity (SCORE) was approved by the Institutional Review Board (IRB) at Thomas Jefferson University (Philadelphia, PA). The IRB reference number is 16S.256. Informed consent was waived by the review board.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Code Availability
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Keith, S.W., Kwabi-Addo, B. & Zeigler-Johnson, C. Interactions Between Obesity and One-Carbon Metabolism Genes in Predicting Prostate Cancer Outcomes Among White and Black Patients. J. Racial and Ethnic Health Disparities 9, 305–314 (2022). https://doi.org/10.1007/s40615-020-00958-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-020-00958-6