Abstract
Little is known about the role of folate and polymorphisms associated with folate metabolism on prostate cancer risk in populations of African origin. We examined the relationship between serum folate and prostate cancer and whether any association was modified by genetic polymorphisms for folate metabolism. The study was case–control in design and consisted of 218 men 40–80 years old with newly diagnosed, histologically confirmed prostate cancer and 236 cancer-free men attending the same urology clinics in Jamaica, March 2005–July 2007. Serum folate was measured by an immunoassay method and genomic DNA evaluated for MTHR (C677T and A1298C), MTRR A66G, and MTR A2756G polymorphisms. Mean serum folate concentration was higher among cases (12.3 ± 4.1 nmol/L) than controls (9.7 ± 4.2 nmol/L). Serum folate concentration showed a positive association with prostate cancer (OR, 4.41; CI, 2.52–7.72 per 10 nmol/L) regardless of grade. No interactions were observed between genotype and folate concentration, but a weak gene effect was observed for MTHFR A1298C and low-grade prostate cancer. Larger studies to investigate the role of gene–gene/gene–diet interactions in Black men are needed.
Similar content being viewed by others
Introduction
Globally, prostate cancer is the second most commonly diagnosed solid malignancy in men; however, the incidence varies widely, with highest rates occurring in developed countries (Australia/New Zealand, 104.2 per 100,000) and lowest in south-central Asia (4.1 per 100,000) (Ferlay et al. 2010). Mortality rates are highest among populations of African descent (Caribbean, 26.3 per 100,000). In Jamaica, the prostate is the leading cancer site and the principal cause of cancer mortality among males (Gibson et al. 2010). Studies suggest that disparities observed among regions may be related to both genetic and environmental factors (such as diet) that play an important role in the development of prostate cancer (Hsing and Chokkalingam 2006).
Circulating folate is largely determined by dietary intakes (Selhub et al. 1999), and there is evidence that low circulating concentrations of folate increase the risk of cancers of the colon, breast, and pancreas (Ulrich 2007), whereas a high concentration may increase the risk for other cancers (Stolzenberg-Solomon et al. 2006). Genetic polymorphisms in folate metabolism also appear to increase the risk of cancer (Ulrich 2007), and it is, therefore, not surprising that gene–nutrient interactions have been implicated in prostate cancer (Rowland et al. 2011; Wright et al. 2009) and other neoplasms (Ma et al. 1997; Ulrich et al. 1999; Ulvik et al. 2001). These studies highlight the complex relationship between folate status and carcinogenesis. Folate functions as a donor in the one-carbon metabolism pathway, an essential process in DNA synthesis, repair and methylation and dysregulation of the metabolic pathway could result in carcinogenesis (Choi and Mason 2000).
Studies relating prostate cancer incidence to circulating folate (Collin et al. 2010), dietary intake (Stevens et al. 2006; Weinstein et al. 2003), and genetic polymorphisms (Collin et al. 2009; Johansson et al. 2007; Stevens et al. 2006; Weinstein et al. 2003) have shown inconsistent findings. Collin et al.’s meta-analysis of circulating folate showed a positive association of folate with prostate cancer (OR, 1.18; CI, 1.00–1.40 per 10 nmol/L) when the prostate testing for cancer and treatment (ProtecT) study of PSA screen-detected cases were excluded (Collin et al. 2010). In a meta-analysis of folate pathway genes and risk of prostate cancer, Collin et al. reported that known common folate pathway single nucleotide polymorphisms methionine synthase (MTR) A2756G and serine hydroxymethyltransferase (SHMT1) C1420T were positively associated with prostate cancer. However, in this meta-analysis, 13 out of the 14 studies involved 91–100 % Caucasian study participants and only one study included 33 % African-American participants (Collin et al. 2009). Methylenetetrahydrofolate reductase (MTHFR), methionine synthase reductase (MTRR), and MTR are genes that encode enzymes involved in the folate metabolic pathway and are critical in the DNA synthesis and methylation process (Kim 2005). Studies have suggested that polymorphisms in these genes may be related to cancer development (Jokic et al. 2011; Marchal et al. 2008).
Despite the high incidence and mortality rates of prostate cancer in blacks, there are limited studies of the nutrigenics of prostate carcinogenesis in these populations. If the relationship of inherited polymorphisms and diet, in particular folate metabolism, increases the risk of prostate cancer, identification of a population at very high risk would allow disease prevention efforts to be more targeted. In this report, we examine for the first time the association of serum folate and MTHFR, MTRR, and MTR as genetic polymorphisms in pathway genes and further investigate the gene–nutrient interactions with risk of prostate cancer in a case–control study in Afro-Caribbean men.
Materials and methods
Study population
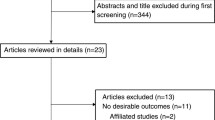
Men with incident prostate cancer were recruited from urology clinics at the 2 main tertiary hospitals and from private practitioners in the Kingston Metropolitan area in Jamaica. The men were referred from primary care clinics, hospitals, and private practitioners throughout the country for diagnostic conformation and treatment of urological disorders. Cases and controls were recruited between March 2005 and July 2007 at the time of their first visit to the clinic—243 men with prostate cancer and 273 controls. The study was approved by the Ethics committee of the University of the West Indies, and subjects gave written informed consent prior to participation in the study.
Selection of cases and controls
Cases
Cases were men 40–80 years old attending the clinics for the first time during the recruitment period. Cases were newly diagnosed prostate cancer that were histologically confirmed and classified by histologic grade using the Gleason system (Gleason and Mellinger 1974).
Controls
Controls were subjects attending the same urology outpatient clinics. Similar to cases, controls were enrolled consecutively in the study. Control subjects presented with diagnostic conditions that were primarily related to lower urinary tract symptoms secondary to BPH and urinary stones. To a lesser extent, patients were referred for investigation and treatment of other suspected genitourinary malignancies or disorders (e.g., male-factor infertility); there were few reports of erectile dysfunction or decreased libido as the primary complaint. Subjects were assigned as controls based on a digital rectal examination (DRE) and total PSA concentration. Controls were initially defined as men with a total PSA < 2 μg/dl but subsequently men with total PSA < 4.0 μg/L and free/total PSA > 0.15 were also recruited to this group.
Exclusion criteria
The following persons were excluded from the study: men (1) with previous prostate surgery, (2) on hormonal treatment, or (3) taking Finasteride.
Data collection
All men who agreed to participate in the study were interviewed at the time of their initial visit to the urologist before their cancer status was known. A standardized questionnaire was administered. Variables collected included demographics, medical history, lifestyle factors (cigarette smoking, vitamin/mineral, and alcohol use) and sexual behavior.
Dietary assessment
Dietary intake was assessed using a validated food frequency questionnaire (FFQ) (Jackson et al. 2011). In addition to frequency of consumption for each food item, subjects were asked to estimate the portion size typically consumed by using food models, commonly used household utensils, measuring cups, and a measuring tape. The FFQ was interviewer-administered.
We excluded from analyses subjects who provided incomplete information on the FFQ (n = 45) or whose reported intakes were outside the range of 800 to 5,000 kcal (n = 36). Men with missing FFQ data were similar in demographic characteristics to the sample providing dietary information. A total of 193 cases and 244 controls were used for analyses of diet.
Anthropometry
Anthropometric measurements were made by trained staff on subjects without shoes wearing light clothing. Weight was measured to the nearest 0.1 kg on an electronic digital scale and height with a portable stadiometer fitted with a spirit level to 0.1 of a centimeter. Body mass index (BMI) was calculated from weight in kilograms divided by the square of the height in meters, and the World Health Organization’s classification of BMI—overweight (BMI > 25.0–29.9 kg/m2) or obese (BMI ≥ 30.0 kg/m2)—was used.
Serum folate analysis
Blood samples, drawn from non-fasting subjects and collected in the mornings, were placed on ice packs in a cooler before being taken to a central laboratory that afternoon. Whole blood aliquots of 5.0 ml were taken and the remaining blood samples were centrifuged at 800×g for 10 min and separated into aliquots of serum and buffy coat fractions. Aliquots were stored at −70 °C.
Folate in serum was measured on an Immulite analyzer by a competitive chemiluminescent immunoassay method in which folate in the sample was released from the serum bonding proteins and competed with a ligand-labeled folate analogue for binding to folate-binding protein (FBP). Bound FBP was then reacted with alkaline phosphatase which resulted in hydrolysis of the chemiluminescent substrate. Measurement of serum folate was carried out at the Chemical Pathology laboratory of the University of the West Indies. (Inter-assay coefficient of variations (CVs) for folate was 7.4 %.) Laboratory personnel were blinded to the status of the samples, and samples from cases and controls were analyzed together to reduce the effect of inter-assay variability.
DNA analysis
Genotyping was performed for rs1801133(MTHFR (C677T)), rs1801131(MTHFR (A1298C)), rs1801394(MTRR A66G), and rs1805087(MTR A2756G) using the Taqman SNP genotyping assays (Applied Biosystems). Briefly, each sample was tested using a 384-well plate and PCR amplification was performed by real-time PCR. For each respective assay, reaction plates were set up to include two non-template controls as well as DNA controls with known genotype at the SNP of interest. Allelic discrimination post-read was performed using the sequence detection system (SDS) software. The SDS software uses the fluorescence measurements from the reaction probe signals from each well to plot fluorescence (Rn) values. The plotted fluorescence values indicate which alleles are in each sample.
Statistical analysis
Chi-square statistics or Fisher’s exact test was used to examine the differences between cases and controls for categorical variables, and the Mann–Whitney U, t test and analysis of variance used for continuous data. Serum folate was measured in nmol/L and dietary intake of folate as μg/day. Serum folate levels according to genotype were reported after adjusting for vitamin use. A non-parametric test for trend was used to look for differences in folate levels by genotype. For each polymorphism, deviation from Hardy–Weinberg equilibrium for the genotype distribution was evaluated in controls only, using an exact test. All genotypes were found to be in Hardy–Weinberg equilibrium.
Adjusted mean serum folate concentrations for cases and controls were calculated independently using a multiple linear regression model (covariates included serum folate, genotype, and vitamin intake). The “adjust” post-estimation command in STATA reports the linear prediction means (×b) and standard errors according to genotype after setting each covariate to the sample mean. Subjects were classified into tertiles according to serum concentration and dietary intakes based on the distribution of the controls. Adjusted binary logistic regression analyses were performed to test the independent and joint association of serum folate and SNPs with prostate cancer. In all multivariable models, adjustments were made for potential confounders that included age, education (as a measure of socioeconomic status), family history of prostate cancer in first-degree relatives, smoking, BMI, and alcohol intake. To test for linear trends across tertiles of serum and dietary intake variables, the median of the variable within each category was determined and used as a continuous variable. We adjusted for age given the suggestion that age influences folate metabolism (Center for Disease Control 2012). The regression coefficients for serum folate are presented for a 10 mmol/L difference in value.
All analyses were performed using STATA 10.1 (College Park, TX) and the Statistical Package for Social Sciences (SPSS) version 17.
Results
The study population consisted of 218 prostate cancer cases and 236 controls. Men diagnosed with prostate cancer were older, shorter, and were less likely to have secondary or higher education than controls (Table 1). Cases and controls had similar mean BMI, and the proportion of current smokers and reported alcohol consumption was not different. Sixteen percent of cases and 11 % of controls reported a family history of prostate cancer. Mean serum folate concentration was higher among men with prostate cancer (12.3 ± 4.1 nmol/L) than cancer-free men (9.7 ± 4.2 nmol/L).
Comparisons between the observed frequencies in our study population controls and reported frequencies in African-American controls were performed using NCBI-dbSNP database: HapMAP data. When HapMAP data were not available, SNP500Cancer data were used. For MTHFR C677T and MTHFR A1298C, the variant frequencies in Jamaican men were not significantly different from African-Americans (C/T + T/T: 20.4 vs. 14.3 %, p = 0.195; A/C + C/C: 27.5 vs. 34.7 %, p = 0.194, respectively). For MTR A2756G, the variant frequency in Jamaican men was significantly higher than that of African-Americans (A/G + G/G: 52.9 vs. 29.2 %, p = 0.003), whereas MTRR A66G variant frequency in Jamaican men was significantly lower than that of African-Americans (A/G + G/G: 40.81 vs. 62.5 %, p = 0.006). Mean serum folate concentrations were lower for cases and controls with the CT and TT variants of MTHFR C677T, but did not attain statistical significance (Table 2). There were no differences in mean serum folate concentrations for the MTR and MTRR polymorphisms.
Table 3 displays age- and multivariable-adjusted associations of serum folate concentrations with prostate cancer. Age-adjusted estimates and multivariable models suggested that increasing serum folate was associated with a higher risk of prostate cancer. Similar patterns were observed for low- and high-grade prostate cancer. Table 3 also displays age- and multivariable-adjusted estimates for serum folate as a continuous variable. Serum folate was positively related to total prostate cancer (OR, 4.41; CI, 2.52–7.72 per 10 nmol/L) and subgrades of disease. In the subset of the population with useful data on folate intake, high intakes of dietary folate also showed a similar association with prostate cancer (Table 4).
Joint effects of genetic polymorphisms and serum folate concentrations on prostate cancer
Table 5 summarizes the joint effects of folate concentration and MTHFR A1298C, MTHFR C677T, MTRR A66G, and MTR A2756G polymorphisms on the odds of prostate cancer. For all of these polymorphisms, men with high folate concentrations and with variant genotypes had increased odds for total prostate compared to men with low folate concentrations and with wild-type genotypes. Similar associations were observed for total-, low-, and high-grade prostate cancer (data not shown). Increased risk was also observed for men with high folate concentrations and wild-type variants versus those with low folate concentration and wild-type variants. Although the risk associated was somewhat attenuated than it was for patients with variant genotypes, there were no significant interactions observed. Similarly, there was no interaction observed for low- and high-grade cancers (data not shown). Regression models without interaction terms for each SNP with total-, low-, and high-grade cancer were calculated to determine the genotype effect on prostate cancer risk. Although not statistically significant, an almost twofold increase in risk was associated with the MTHFR A1298C genotype and low-grade prostate cancer (OR, 1.85; CI, 0.95–3.61) but showed no association with total- or high-grade prostate cancer. There were no genetic effects on total-, low-, or high-grade cancer for any other polymorphisms (data not shown).
Discussion
In this report, we have for the first time presented evidence of a positive relationship between serum folate and incident prostate cancer and showed a dose–response relationship among men of predominantly African origin. For MTHFR A1298C, MTHFR C677T, MTRR A66G, and MTR A2756G polymorphisms, men with high folate concentrations and with variant genotypes showed greater likelihood for total prostate cancer compared to men with low folate concentrations and with wild-type genotypes.
We found a dose–response relationship with serum folate and prostate cancer. Our data suggested a fourfold increased risk of prostate cancer for a 10 nmol/L difference in serum folate. These estimates are higher than Collin et al.’s meta-analysis which included predominantly Caucasian men (7 % men enrolled in the Aspirin/Folic Acid Polyp Prevention trial). These differences in risk may be related to the ethnicity of the populations studied. Jamaica is a predominantly black population (91.6 %) (Statistical Institute of Jamaica 2003) and the contribution of African ancestry is recognized. We did not evaluate vitamin B12 or homocysteine which is important in folate metabolism, particularly DNA methylation and prostate carcinogenesis. Hultdin et al. showed that whereas in univariate analyses, higher folate concentrations increased the risk of prostate cancer, with adjustment for the nutrients and other potential confounders, the effects of folate lost significance (Hultdin et al. 2005). It is possible, therefore, that additional control for vitamin B12 and homocysteine are likely to attenuate the estimate of association observed between circulating folate and prostate cancer.
Folate intake was comparably higher than levels reported in the USA (Vanderwall et al. 2012) and Australia (Bassett et al. 2012). In Jamaica, flour is fortified with folic acid; however, we were unable to account for the contribution of fortification. The major sources of dietary folate were cereals (flour products), legumes, avocado, green leafy vegetables, and fruits. On the other hand, serum folate concentrations in our study while comparable to that reported in some European countries (Collin et al. 2010) were substantially lower than men in the USA, including non-Hispanic blacks (Center for Disease Control 2012), and other countries (Figueiredo et al. 2009; Tomaszewski et al. 2011). Our findings suggest that there may be factors such as genetic or environmental factors that modulate folate status.
We also found that prostate cancer-free men had lower serum folate than men with disease. It is possible that the positive association between serum folate and prostate cancer could be explained by protective effects of lower levels of folate concentrations rather than detrimental effects of high serum folate concentrations. Animal studies show that mild dietary folate depletion appears to arrest prostate cancer progression in the TRAMP mice in which tumorigenesis is prostate-specific and aggressive (Bistulfi et al. 2011). Other animal studies report the tumor-promoting potential of folic acid highlighting that folate deficiency inhibits the incidence and rate of appearance of mammary tumors in rats (Kotsopoulos et al. 2003). It is postulated that folate may facilitate the growth of cancer cells by up-regulating member transporters that mediate folate uptake (Kelemen 2006); such a mechanism might better enable tumor-bearing prostates to extract folate from serum (Tomaszewski et al. 2011).
Although numerous studies have evaluated the role of genetic polymorphisms in folate pathway genes, we are not aware of any studies that have investigated the joint effects between these polymorphisms and serum or plasma folate concentrations on prostate cancer risk. In our study, the MTHFR A1298C, MTHFR C677T, MTRR A66G, and MTR A2756G variants do not appear to attenuate the risk associated with serum folate concentration. Furthermore, there does not appear to be any noted effects of genetics on the increased risk of prostate cancer observed for men with high folate concentration and this was irrespective of low- or high-grade disease.
For the first time, we also evaluated the association of the folate metabolic pathway genes in a Caribbean (Jamaican) population of African ancestry. In our study population, variants of MTHFR C677T, MTHFR A1298C, MTRR A66G, or MTR A2756G were not associated with serum folate and did not increase the risk of prostate cancer. There are a limited number of studies of the potential role of the MTHFR, MTR, and MTRR genotypes on prostate cancer risk. In Asian studies, no associations were found between these genotypes and prostate cancer (Cai et al. 2010; Wu et al. 2010). In the Jamaican population, polymorphisms alone [MTHFR (C677T and A1298C), MTRR A66G, MTHFR A1298C, and MTR A2756G] showed no relationship to total prostate cancer and the findings did not vary by clinical grade except for an increase risk associated with the MTHFR A1298C and low-grade prostate cancer. The meta-analysis by Collin et al. reported an association between the MTR A2756G and prostate cancer, but no difference in the association between localized and advanced disease. We did not observe a genotype effect on prostate cancer risk, and it is possible that our relatively small study was underpowered to detect an association. Notwithstanding, our findings suggest that once circulating folate concentrations increase beyond a certain threshold, the effect of genetics may no longer be important. Investigation of a larger sample is needed to validate our findings.
Strengths/limitations
To our knowledge, this is the first study conducted in a predominantly black Caribbean population that has examined the role of serum and genetic factors on prostate cancer risk. Most other studies have been conducted on Caucasians (Collin et al. 2009, 2010). Data were collected from participants prior to their knowledge of their cancer status and excluded persons who had metastatic cancer which might have affected dietary intake or metabolism. Dietary assessment of folate intake was estimated from FFQ, an instrument prone to measurement errors and reflected in low correlations between dietary and serum concentrations of the nutrient (Jackson et al. 2011; Weinstein et al. 2006), although metabolic effects may also contribute to variations in circulating concentrations. This case–control design does not allow the temporal relationships between folate and prostate cancer to be determined. Residual confounding is also possible due to unexamined confounders. One limitation of our study is the sample size which only allowed us to evaluate single gene–folate concentration interactions. To further explain the differences in the joint effects of genetic polymorphisms in folate metabolic genes and circulating folate concentrations, gene–gene interactions in combination with folate concentrations should be considered in future studies.
Conclusions
Our results suggest that for African-Caribbean men, higher circulating folate concentrations may increase the risk of total prostate cancer and low- and high-grade disease in a dose-dependent manner; there were no interactions between folate pathway polymorphisms and folate levels. Larger studies that further investigate the role of gene–diet interactions on prostate cancer risk in black populations need to be performed.
References
Bassett JK, Severi G, Hodge AM, Baglietto L, Hopper JL, English DR, Giles GG (2012) Dietary intake of B vitamins and methionine and prostate cancer incidence and mortality. Cancer Causes Control 23:855–863
Bistulfi G, Foster BA, Karasik E, Gillard B, Miecznikowski J, Dhiman VK, Smiraglia DJ (2011) Dietary folate deficiency blocks prostate cancer progression in the TRAMP model. Cancer Prev Res (Phila) 4:1825–1834
Cai D, Ning L, Pan C, Liu X, Bu R, Chen X, Wang K, Cheng Y, Wu B (2010) Association of polymorphisms in folate metabolic genes and prostate cancer risk: a case-control study in a Chinese population. J Genet 89:263–267
Center for Disease Control. Second National Report on Biochemical Indicators of Diet and Nutrition in the U.S. Population. 2012. 2012
Choi SW, Mason JB (2000) Folate and carcinogenesis: an integrated scheme. J Nutr 130:129–132
Collin SM, Metcalfe C, Zuccolo L, Lewis SJ, Chen L, Cox A, Davis M, Lane JA, Donovan J, Smith GD, Neal DE, Hamdy FC, Gudmundsson J, Sulem P, Rafnar T, Benediktsdottir KR, Eeles RA, Guy M, Kote-Jarai Z, Morrison J, Al Olama AA, Stefansson K, Easton DF, Martin RM (2009) Association of folate-pathway gene polymorphisms with the risk of prostate cancer: a population-based nested case-control study, systematic review, and meta-analysis. Cancer Epidemiol Biomarkers Prev 18:2528–2539
Collin SM, Metcalfe C, Refsum H, Lewis SJ, Zuccolo L, Smith GD, Chen L, Harris R, Davis M, Marsden G, Johnston C, Lane JA, Ebbing M, Bonaa KH, Nygard O, Ueland PM, Grau MV, Baron JA, Donovan JL, Neal DE, Hamdy FC, Smith AD, Martin RM (2010) Circulating folate, vitamin B12, homocysteine, vitamin B12 transport proteins, and risk of prostate cancer: a case-control study, systematic review, and meta-analysis. Cancer Epidemiol Biomarkers Prev 19:1632–1642
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM (2010) Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 127:2893–2917
Figueiredo JC, Grau MV, Haile RW, Sandler RS, Summers RW, Bresalier RS, Burke CA, McKeown-Eyssen GE, Baron JA (2009) Folic acid and risk of prostate cancer: results from a randomized clinical trial. J Natl Cancer Inst 101:432–435
Gibson TN, Hanchard B, Waugh N, McNaughton D (2010) Age-specific incidence of cancer in Kingston and St. Andrew, Jamaica, 2003–2007. West Indian Med J 59:456–464
Gleason DF, Mellinger GT (1974) Prediction of prognosis for prostatic adenocarcinoma by combined histological grading and clinical staging. J Urol 111:58–64
Hsing AW, Chokkalingam AP (2006) Prostate cancer epidemiology. Front Biosci 11:1388–1413
Hultdin J, Van Guelpen B, Bergh A, Hallmans G, Stattin P (2005) Plasma folate, vitamin B12, and homocysteine and prostate cancer risk: a prospective study. Int J Cancer 113:819–824
Jackson MD, Walker SP, Younger NM, Bennett FI (2011) Use of a food frequency questionnaire to assess diets of Jamaican adults: validation and correlation with biomarkers. Nutr J 10:28
Johansson M, Van Guelpen B, Hultdin J, Wiklund F, Adami HO, Balter K, Gronberg H, Stattin P (2007) The MTHFR 677C –>T polymorphism and risk of prostate cancer: results from the CAPS study. Cancer Causes Control 18:1169–1174
Jokic M, Brcic-Kostic K, Stefulj J, Ivkovic TC, Bozo L, Gamulin M, Kapitanovic S (2011) Association of MTHFR, MTR, MTRR, RFC1, and DHFR gene polymorphisms with susceptibility to sporadic colon cancer. DNA Cell Biol 30:771–776
Kelemen LE (2006) The role of folate receptor alpha in cancer development, progression and treatment: cause, consequence or innocent bystander? Int J Cancer 119:243–250
Kim YI (2005) 5,10-Methylenetetrahydrofolate reductase polymorphisms and pharmacogenetics: a new role of single nucleotide polymorphisms in the folate metabolic pathway in human health and disease. Nutr Rev 63:398–407
Kotsopoulos J, Sohn KJ, Martin R, Choi M, Renlund R, McKerlie C, Hwang SW, Medline A, Kim YI (2003) Dietary folate deficiency suppresses N-methyl-N-nitrosourea-induced mammary tumorigenesis in rats. Carcinogenesis 24:937–944
Ma J, Stampfer MJ, Giovannucci E, Artigas C, Hunter DJ, Fuchs C, Willett WC, Selhub J, Hennekens CH, Rozen R (1997) Methylenetetrahydrofolate reductase polymorphism, dietary interactions, and risk of colorectal cancer. Cancer Res 57:1098–1102
Marchal C, Redondo M, Reyes-Engel A, Perea-Milla E, Gaitan MJ, Machuca J, Diaz F, Caballero J, Carnero J (2008) Association between polymorphisms of folate-metabolizing enzymes and risk of prostate cancer. Eur J Surg Oncol 34:805–810
Rowland GW, Schwartz GG, John EM, Ingles SA (2011) Calcium intake and prostate cancer among African Americans: effect modification by vitamin D receptor calcium absorption genotype. J Bone Miner Res. doi:10.1002/jbmr.505
Selhub J, Jacques PF, Rosenberg IH, Rogers G, Bowman BA, Gunter EW, Wright JD, Johnson CL (1999) Serum total homocysteine concentrations in the third National Health and Nutrition Examination Survey (1991–1994): population reference ranges and contribution of vitamin status to high serum concentrations. Ann Intern Med 131:331–339
Statistical Institute of Jamaica. Population Census 2001: Jamaica. 2003. 2003, Statistical Institute of Jamaica
Stevens VL, Rodriguez C, Pavluck AL, McCullough ML, Thun MJ, Calle EE (2006) Folate nutrition and prostate cancer incidence in a large cohort of US men. Am J Epidemiol 163:989–996
Stolzenberg-Solomon RZ, Chang SC, Leitzmann MF, Johnson KA, Johnson C, Buys SS, Hoover RN, Ziegler RG (2006) Folate intake, alcohol use, and postmenopausal breast cancer risk in the prostate, lung, colorectal, and ovarian cancer screening trial. Am J Clin Nutr 83:895–904
Tomaszewski JJ, Cummings JL, Parwani AV, Dhir R, Mason JB, Nelson JB, Bacich DJ, O’Keefe DS (2011) Increased cancer cell proliferation in prostate cancer patients with high levels of serum folate. Prostate 71:1287–1293
Ulrich CM (2007) Folate and cancer prevention: a closer look at a complex picture. Am J Clin Nutr 86:271–273
Ulrich CM, Kampman E, Bigler J, Schwartz SM, Chen C, Bostick R, Fosdick L, Beresford SA, Yasui Y, Potter JD (1999) Colorectal adenomas and the C677T MTHFR polymorphism: evidence for gene-environment interaction? Cancer Epidemiol Biomarkers Prev 8:659–668
Ulvik A, Evensen ET, Lien EA, Hoff G, Vollset SE, Majak BM, Ueland PM (2001) Smoking, folate and methylenetetrahydrofolate reductase status as interactive determinants of adenomatous and hyperplastic polyps of colorectum. Am J Med Genet 101:246–254
Vanderwall CM, Tangney CC, Kwasny MJ, Gustashaw KA (2012) Examination of circulating folate levels as a reflection of folate intakes among older adult supplement users and nonusers in the National Health and Nutrition Examination Survey 2003–2004. J Acad Nutr Diet 112:285–290
Weinstein SJ, Hartman TJ, Stolzenberg-Solomon R, Pietinen P, Barrett MJ, Taylor PR, Virtamo J, Albanes D (2003) Null association between prostate cancer and serum folate, vitamin B(6), vitamin B(12), and homocysteine. Cancer Epidemiol Biomarkers Prev 12:1271–1272
Weinstein SJ, Stolzenberg-Solomon R, Pietinen P, Taylor PR, Virtamo J, Albanes D (2006) Dietary factors of one-carbon metabolism and prostate cancer risk. Am J Clin Nutr 84:929–935
Wright ME, Peters U, Gunter MJ, Moore SC, Lawson KA, Yeager M, Weinstein SJ, Snyder K, Virtamo J, Albanes D (2009) Association of variants in two vitamin e transport genes with circulating vitamin e concentrations and prostate cancer risk. Cancer Res 69:1429–1438
Wu HC, Chang CH, Tsai RY, Lin CH, Wang RF, Tsai CW, Chen KB, Yao CH, Chiu CF, Bau DT, Lin CC (2010) Significant association of methylenetetrahydrofolate reductase single nucleotide polymorphisms with prostate cancer susceptibility in Taiwan. Anticancer Res 30:3573–3577
Acknowledgments
This work was supported by the National Health Fund [HSF19], CHASE Fund, and the Planning Institute of Jamaica [77/854]. This study was supported also in part by grants from the National Cancer Institute (R13CA130596A) and an appropriation from the Commonwealth of Pennsylvania to Fox Chase Cancer Center (CA006927) awarded to CR. The authors thank the study participants, project staff, Rita Michielli, from the Fox Chase Cancer Center Genomics Facility, Elizabeth Blackman and Denise Gibbs from the Ragin laboratory for supporting this study.
Conflict of interest
No potential conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jackson, M.D., Tulloch-Reid, M.K., McFarlane-Anderson, N. et al. Complex interaction between serum folate levels and genetic polymorphisms in folate pathway genes: biomarkers of prostate cancer aggressiveness. Genes Nutr 8, 199–207 (2013). https://doi.org/10.1007/s12263-012-0321-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12263-012-0321-7