Abstract
Purpose of Review
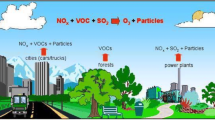
Airway inflammation is a common biological response to many types of environmental exposures and can lead to increased nitric oxide (NO) concentrations in exhaled breath. In recent years, several studies have evaluated airway inflammation using fractional exhaled nitric oxide (FeNO) as a biomarker of exposures to a range of air pollutants. This systematic review aims to summarize the studies that collected personal-level air pollution data to assess the air pollution–induced FeNO responses and to determine if utilizing personal-level data resulted in an improved characterization of the relationship between air pollution exposures and FeNO compared to using only ambient air pollution exposure data.
Recent Findings
Thirty-six eligible studies were identified. Overall, the studies included in this review establish that an increase in personal exposure to particulate and gaseous air pollutants can significantly increase FeNO. Nine out of the 12 studies reported statistically significant FeNO increases with increasing personal PM2.5 exposures, and up to 11.5% increase in FeNO per IQR increase in exposure has also been reported between FeNO and exposure to gas-phase pollutants, such as ozone, NO2, and benzene. Furthermore, factors such as chronic respiratory diseases, allergies, and medication use were found to be effect modifiers for air pollution–induced FeNO responses. About half of the studies that compared the effect estimates using both personal and ambient air pollution exposure methods reported that only personal exposure yielded significant associations with FeNO response.
Summary
The evidence from the reviewed studies confirms that FeNO is a sensitive biomarker for air pollutant-induced airway inflammation. Personal air pollution exposure assessment is recommended to accurately assess the air pollution–induced FeNO responses. Furthermore, comprehensive adjustments for the potential confounding factors including the personal exposures of the co-pollutants, respiratory disease status, allergy status, and usage of medications for asthma and allergies are recommended while assessing the air pollution–induced FeNO responses.


Similar content being viewed by others
Data Availability
Data will be available upon request.
References
Papers of particular interest, have been highlighted as: • Of major importance
Munakata M. Exhaled nitric oxide (FeNO) as a non-invasive marker of airway inflammation. Allergol Int. 2012;61:365–72. https://doi.org/10.2332/ALLERGOLINT.12-RAI-0461.
Henriksen AM, Sue-Chu M, Lingaas Holmen T, Langhammer A, Bjermer L. Exhaled and nasal NO levels in allergic rhinitis: relation to sensitization, pollen season and bronchial hyperresponsiveness. Eur Respir J. 1999;13:301–6. https://doi.org/10.1034/J.1399-3003.1999.13B14.X.
Taylor DR, Pijnenburg MW, Smith AD, De Jongste JC. Exhaled nitric oxide measurements: clinical application and interpretation. Thorax. 2006;61:817–27. https://doi.org/10.1136/THX.2005.056093.
• Fan Z, Pun VC, Chen XC, Hong Q, Tian L, Ho SSH, et al. Personal exposure to fine particles (PM25) and respiratory inflammation of common residents in Hong Kong. Environ Res. 2018;164:24–31. https://doi.org/10.1016/J.ENVRES.2018.02.009. One of the studies reporting that only personal air pollution exposure yielded a significant association with FeNO response, while ambient exposure did not.
• Jiang Y, Niu Y, Xia Y, Liu C, Lin Z, Wang W, et al. Effects of personal nitrogen dioxide exposure on airway inflammation and lung function. Environ Res. 2019;177:108620. https://doi.org/10.1016/J.ENVRES.2019.108620. One of the few studies suggesting NOS2A hypomethylation and ARG2 hypermethylation may enhance NO production after certain air pollution exposures.
Kharitonov SA, Gonio F, Kelly C, Meah S, Barnes PJ. Reproducibility of exhaled nitric oxide measurements in healthy and asthmatic adults and children. Eur Respir J. 2003;21:433–8. https://doi.org/10.1183/09031936.03.00066903A.
Khatri SB, Iaccarino JM, Barochia A, Soghier I, Akuthota P, Brady A, et al. Use of fractional exhaled nitric oxide to guide the treatment of asthma: an Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2021;2021(24):97–110. https://doi.org/10.1164/RCCM.202109-2093ST.
Warke TJ, Fitch PS, Shields MD, Brown V, Ennis M, Taylor R, et al. Exhaled nitric oxide correlates with airway eosinophils in childhood asthma. Thorax. 2002;57:383–7. https://doi.org/10.1136/THORAX.57.5.383.
Berlyne GS, Parameswaran K, Kamada D, Efthimiadis A, Hargreave FE. A comparison of exhaled nitric oxide and induced sputum as markers of airway inflammation. J Allergy Clin Immunol. 2000;106:638–44. https://doi.org/10.1067/mai.2000.109622.
Strunk RC, Szefler SJ, Phillips BR, Zeiger RS, Chinchilli VM, Larsen G, et al. Relationship of exhaled nitric oxide to clinical and inflammatory markers of persistent asthma in children. J Allergy Clin Immunol. 2003;2003(112):883–92. https://doi.org/10.1016/j.jaci.2003.08.014.
Payne DNR, Adcock IM, Wilson NM, Oates T, Scallan M, Bush A. Relationship between exhaled nitric oxide and mucosal eosinophilic inflammation in children with difficult asthma, after treatment with oral prednisolone. Am J Respir Crit Care Med. 2012;164:1376–81. https://doi.org/10.1164/AJRCCM.164.8.2101145.
Uematsu M, Saito J, Sato S, Fukuhara A, Suzuki Y, Rikimaru M, et al. Usefulness of diurnal variation of fractional exhaled nitric oxide for predicting early therapeutic response to asthma treatment. J Asthma. 2022;59:2039–50.
Bălă GP, Râjnoveanu RM, Tudorache E, Motișan R, Oancea C. Air pollution exposure—the (in)visible risk factor for respiratory diseases. Environ Sci Pollut Res. 2021;28:19615–28. https://doi.org/10.1007/s11356-021-13208-x.
Faustini A, Stafoggia M, Colais P, Berti G, Bisanti L, Cadum E, et al. Air pollution and multiple acute respiratory outcomes. Eur Respir J. 2013;42:304–13. https://doi.org/10.1183/09031936.00128712.
Kelly FJ, Fussell JC. Air pollution and airway disease. Clin Exp Allergy. 2011;41:1059–71. https://doi.org/10.1111/J.1365-2222.2011.03776.X.
Dockery DW, Pope CA. Acute respiratory effects of particulate air pollution. Annu Rev Public Health. 2003;15:107–32. https://doi.org/10.1146/ANNUREV.PU.15.050194.000543.
Özkaynak H, Baxter LK, Dionisio KL, Burke J. Air pollution exposure prediction approaches used in air pollution epidemiology studies. J Eposure Sci Environ Epidemiol. 2013;23:566–72. https://doi.org/10.1038/jes.2013.15.
Setton E, Marshall JD, Brauer M, Lundquist KR, Hystad P, Keller P, et al. The impact of daily mobility on exposure to traffic-related air pollution and health effect estimates. J Eposure Sci Environ Epidemiol. 2011;21:42–8. https://doi.org/10.1038/jes.2010.14.
Levy Zamora M, Pulczinski JC, Johnson N, Garcia-Hernandez R, Rule A, Carrillo G, Zietsman J, et al. Maternal exposure to PM2.5 in south Texas, a pilot study. Sci Total Environ. 2018;628:1497–507. https://doi.org/10.1016/J.SCITOTENV.2018.02.138.
Anand A, Phuleria HC. Modeling indoor exposure to PM2.5 and black carbon in densely populated urban slums. Build Environ. 2021;200:107940. https://doi.org/10.1016/J.BUILDENV.2021.107940.
Buonanno G, Fuoco FC, Russi A, Stabile L. Individual exposure of women to fine and coarse PM. Environ Eng Manag J. 2015;14:827–36. https://doi.org/10.30638/EEMJ.2015.092.
Strak M, Boogaard H, Meliefste K, Oldenwening M, Zuurbier M, Brunekreef B, et al. Respiratory health effects of ultrafine and fine particle exposure in cyclists. Occup Environ Med. 2010;67:118–24. https://doi.org/10.1136/OEM.2009.046847.
Buonanno G, Stabile L, Morawska L. Personal exposure to ultrafine particles: the influence of time-activity patterns. Sci Total Environ. 2014;468:903–7. https://doi.org/10.1016/J.SCITOTENV.2013.09.016.
Buehler C, Xiong F, Levy Zamora M, Skog KM, Kohrman-Glaser J, Colton S, et al. Stationary and portable multipollutant monitors for high-spatiotemporal-resolution air quality studies including online calibration. Atmos Meas Tech. 2020;14:995–1013. https://doi.org/10.5194/AMT-14-995-2021.
• Chen G, Liu S, Lu Y, Xiang H. The association between short-term exposure to ambient air pollution and fractional exhaled nitric oxide level: a systematic review and meta-analysis of panel studies. Environ Pollut. 2020;265:114833. https://doi.org/10.1016/J.ENVPOL.2020.114833. Review of the studies investigating associations between ambient air pollution exposures and FeNO responses.
Liu Q, Gu X, Deng F, Mu L, Baccarelli AA, Guo X, et al. Ambient particulate air pollution and circulating C-reactive protein level: a systematic review and meta-analysis. Int J Hyg Environ Health. 2019;222:756–64. https://doi.org/10.1016/j.ijheh.2019.05.005.
Xu T, Hou J, Cheng J, Zhang R, Yin W, Huang C, et al. Estimated individual inhaled dose of fine particles and indicators of lung function: a pilot study among Chinese young adults. Environ Pollut. 2018;235:505–13. https://doi.org/10.1016/J.ENVPOL.2017.12.074.
• Chen T, Chen F, Wang K, Ma X, Wei X, Wang W, et al. Acute respiratory response to individual particle exposure (PM1.0, PM2.5 and PM10) in the elderly with and without chronic respiratory diseases. Environ Pollut. 2021;271:116329. https://doi.org/10.1016/J.ENVPOL.2020.116329. One of the studies assessing the role of size distribution in the association of personal PM exposure with FeNO response.
• Shang J, Khuzestani RB, Huang W, An J, Schauer JJ, Fang D, et al. Acute changes in a respiratory inflammation marker in guards following Beijing air pollution controls. Sci Total Environ. 2018;624:1539–49. https://doi.org/10.1016/J.SCITOTENV.2017.12.109. One of the few studies assessing the effect of various air pollution sources on FeNO response using specific source marker elements.
• Delfino RJ, Staimer N, Gillen D, Tjoa T, Sioutas C, Fung K, et al. Personal and ambient air pollution is associated with increased exhaled nitric oxide in children with asthma. Environ Health Perspect. 2006;114:1736–43. https://doi.org/10.1289/EHP.9141. One of the studies reporting that medications used for asthma may suppress the inflammatory response to air pollution exposures.
Maestrelli P, Canova C, Scapellato ML, Visentin A, Tessari R, Bartolucci GB, et al. Personal exposure to particulate matter is associated with worse health perception in adult asthma. J Investig Allergol Clin Immunol. 2011;21:120–8.
Tung NT, Lai CH, Pan CH, Chen WL, Wang CC, Liang CW, et al. Associations of PM2.5 with chronic obstructive pulmonary disease in shipyard workers: a cohort study. Aerosol Air Qual Res. 2022;22:210272. https://doi.org/10.4209/AAQR.210272.
Benka-Coker ML, Clark ML, Rajkumar S, Young BN, Bachand AM, Balmes JR, et al. Exposure to household air pollution from biomass cookstoves and levels of fractional exhaled nitric oxide (FeNO) among Honduran women. Int J Environ Res Public Health. 2018;15(11):2544. https://doi.org/10.3390/IJERPH15112544.
Maikawa CL, Weichenthal S, Wheeler AJ, Dobbin NA, Smargiassi A, Evans G, et al. Particulate oxidative burden as a predictor of exhaled nitric oxide in children with asthma. Environ Health Perspect. 2016;124:1616–22. https://doi.org/10.1289/EHP175.
Niu Y, Chen R, Xia Y, Cai J, Lin Z, Liu C, et al. Personal ozone exposure and respiratory inflammatory response: the role of DNA methylation in the arginase-nitric oxide synthase pathway. Environ Sci Technol. 2018;52:8785–91. https://doi.org/10.1021/ACS.EST.8B01295.
Zhang X, Staimer N, Gillen DL, Tjoa T, Schauer JJ, Shafer MM, et al. Associations of oxidative stress and inflammatory biomarkers with chemically-characterized air pollutant exposures in an elderly cohort. Environ Res. 2016;150:306–19. https://doi.org/10.1016/J.ENVRES.2016.06.019.
• He L, Li Z, Teng Y, Cui X, Barkjohn KK, Norris C, et al. Associations of personal exposure to air pollutants with airway mechanics in children with asthma. Environ Int. 2020;138:105647. https://doi.org/10.1016/J.ENVINT.2020.105647. Study finding significant association between personal PM2.5 exposure and FeNO response among only participants with non-eosinophilic asthma, but not with eosinophilic asthma.
Douwes J, Gibson P, Pekkanen J, Pearce N. Non-eosinophilic asthma: importance and possible mechanisms. Thorax. 2002;57:643–8. https://doi.org/10.1136/thorax.57.7.643.
Walford HH, Doherty TA. Diagnosis and management of eosinophilic asthma: a US perspective. J Asthma Allergy. 2014;7:53–65. https://doi.org/10.2147/JAA.S39119.
Jung KH, Goodwin KE, Perzanowski MS, Chillrud SN, Perera FP, et al. Personal exposure to black carbon at school and levels of fractional exhaled nitric oxide in New York City. Environ Health Perspect. 2021;129:097005. https://doi.org/10.1289/EHP8985.
Koenig JQ, Mar TF, Allen RW, Jansen K, Lumley T, Sullivan JH, et al. Pulmonary effects of indoor- and outdoor-generated particles in children with asthma. Environ Health Perspect. 2005;113:499. https://doi.org/10.1289/EHP.7511.
Braniš M, Kolomazníková J. Monitoring of long-term personal exposure to fine particulate matter (PM2.5). Air Qual Atmos Health. 2010;3:235–43.
Buonanno G, Fuoco FC, Russi A, Stabile L. Individual exposure of women to fine and coarse PM. Environ Eng Manag J 2015: 14.
Adgate JL, Ramachandran G, Pratt GC, Waller LA, Sexton K. Spatial and temporal variability in outdoor, indoor, and personal PM2.5 exposure. Atmos Environ. 2002;36:3255–65.
Sharma JN, Al-Omran A, Parvathy SS. Role of nitric oxide in inflammatory diseases. Inflammopharmacology. 2007;15:252–9. https://doi.org/10.1007/s10787-007-0013-x.
Munakata M. Exhaled nitric oxide (FeNO) as a non-invasive marker of airway inflammation. Allergol Int. 2012;61:365–72. https://doi.org/10.2332/allergolint.12-RAI-0461.
Heaney LG, Perez de Llano L, Al-Ahmad M, Backer V, Busby J, Canonica GW, et al. Eosinophilic and noneosinophilic asthma: an expert consensus framework to characterize phenotypes in a global real-life severe asthma cohort. Chest. 2021;160:814–30. https://doi.org/10.1016/j.chest.2021.04.013.
Jung KH, Lovinsky-Desir S, Yan B, Torrone D, Lawrence J, Jezioro JR, et al. Effect of personal exposure to black carbon on changes in allergic asthma gene methylation measured 5 days later in urban children: importance of allergic sensitization. Clin Epigenetics. 2017;9:1–11. https://doi.org/10.1186/S13148-017-0361-3.
Kan H. The smaller, the worse? Lancet Planet Health. 2017;1:e210ee211. https://doi.org/10.1016/s2542-5196(17)30095-5.
Ji N, Fang M, Baptista A, Cepeda C, Greenberg M, Mincey IC, et al. Exposure to traffic-related air pollution and changes in exhaled nitric oxide and DNA methylation in arginase and nitric oxide synthase in children with asthma. Environ Health: Glob Access Sci Source. 2021;20:1–11. https://doi.org/10.1186/S12940-020-00678-8.
Lovinsky-Desir S, Miller RL, Chillrud SN, Perzanowski MS, Jung KH. Associations of timing and mode of commuting with in-transit black carbon exposure and airway inflammation: a pilot study. Ann Am Thorac Soc. 2019;16:923–7. https://doi.org/10.1513/ANNALSATS.201810-668RL.
Guilbert A, De Cremer K, Heene B, Demoury C, Aerts R, Declerck P, et al. Personal exposure to traffic-related air pollutants and relationships with respiratory symptoms and oxidative stress: a pilot cross-sectional study among urban green space workers. Sci Total Environ. 2019;649:620–8. https://doi.org/10.1016/J.SCITOTENV.2018.08.338.
Fan Y, Han Y, Liu Y, Wang Y, Chen X, Chen W, et al. Biases arising from the use of ambient measurements to represent personal exposure in evaluating inflammatory responses to fine particulate matter: evidence from a panel study in Beijing, China. Environ Sci Technol Lett. 2020;7:746–52. https://doi.org/10.1021/acs.estlett.0C00478.
• Godri Pollitt KJ, Maikawa CL, Wheeler AJ, Weichenthal S, Dobbin NA, Liu L, et al. Trace metal exposure is associated with increased exhaled nitric oxide in asthmatic children. Environ Health: Glob Access Sci Source. 2016;15:1–11. https://doi.org/10.1186/S12940-016-0173-5. One of the few studies assessing the effect of various air pollution sources on FeNO response using specific source marker elements.
Li T, Wang Y, Hou J, Zheng D, Wang G, Hu C, et al. Associations between inhaled doses of PM2.5-bound polycyclic aromatic hydrocarbons and fractional exhaled nitric oxide. Chemosphere. 2019;218:992–1001. https://doi.org/10.1016/J.CHEMOSPHERE.2018.11.196.
Jiang X, Han Y, Qiu X, Chai Q, Zhang H, Chen X, et al. Organic components of personal PM2.5 exposure associated with inflammation: evidence from an untargeted exposomic approach. Environ Sci Technol. 2021;55:10589–96. https://doi.org/10.1021/ACS.EST.1C02023.
Delfino RJ, Staimer N, Tjoa T, Gillen DL. Relations of exhaled nitric oxide and FEV1 to personal endotoxin exposure in schoolchildren with asthma. Occup Environ Med. 2015;2015(72):830–6. https://doi.org/10.1136/OEMED-2014-102651.
Chambers L, Finch J, Edwards K, Jeanjean A, Leigh R, Gonem S. Effects of personal air pollution exposure on asthma symptoms, lung function and airway inflammation. Clin Exp Allergy. 2018;48:798–805. https://doi.org/10.1111/CEA.13130.
• Weichenthal S, Kulka R, Bélisle P, Joseph L, Dubeau A, Martin C, et al. Personal exposure to specific volatile organic compounds and acute changes in lung function and heart rate variability among urban cyclists. Environ Res. 2012;118:118–23. https://doi.org/10.1016/J.ENVRES.2012.06.005. One of the studies reporting significant change in the effect of a pollutant on FeNO response after accounting the confounding by personal exposure of co-pollutants.
Koenig JQ, Jansen K, Mar TF, Lumley T, Kaufman J, Trenga CA, et al. Measurement of offline exhaled nitric oxide in a study of community exposure to air pollution. Environ Health Perspect. 2003;111:1625. https://doi.org/10.1289/EHP.6160.
Lovinsky-Desir S, Jung KH, Rundle AG, Hoepner LA, Bautista JB, Perera FP, et al. Physical activity, black carbon exposure and airway inflammation in an urban adolescent cohort. Environ Res. 2016;151:756–62. https://doi.org/10.1016/J.ENVRES.2016.09.005.
Chen XC, Chuang HC, Ward TJ, Tian L, Cao JJ, Ho SSH, et al. Indoor, outdoor, and personal exposure to PM2.5 and their bioreactivity among healthy residents of Hong Kong. Environ Res. 2020;188:109780. https://doi.org/10.1016/J.ENVRES.2020.109780.
Andersson L, Bryngelsson IL, Hedbrant A, Persson A, Johansson A, Ericsson A, et al. Respiratory health and inflammatory markers - exposure to respirable dust and quartz and chemical binders in Swedish iron foundries. PLoS ONE. 2019;14:e0224668. https://doi.org/10.1371/JOURNAL.PONE.0224668.
Allen RW, Mar T, Koenig J, Liu LJS, Gould T, Simpson C, et al. Changes in lung function and airway inflammation among asthmatic children residing in a woodsmoke-impacted urban area. Inhalation Toxicol. 2008;20:423–33. https://doi.org/10.1080/08958370801903826.
Laeremans M, Dons E, Avila-Palencia I, Carrasco-Turigas G, Orjuela JP, Anaya E, et al. Short-term effects of physical activity, air pollution and their interaction on the cardiovascular and respiratory system. Environ Int. 2018;117:82–90. https://doi.org/10.1016/J.ENVINT.2018.04.040.
Tungu AM, Bratveit M, Mamuya SH, Moen BE. Cross-shift reduction in fractional exhaled nitric oxide among cement workers. Occupational Medicine & Health Affairs. 2016;4:1000249. https://doi.org/10.4172/2329-6879.1000249.
Westerlund J, Phil L, Bryngelsson IL, Fornander L, Löfstedt H, Graff P. Occupational exposure to trichloramine and endotoxins: adverse health effects among personnel in adventure and rehabilitation swimming pool facilities. J Occup Environ Med. 2022;64:361–9. https://doi.org/10.1097/JOM.0000000000002483.
Xu J, Zhang N, Zhang G, Zhang Y, Wang Z, Lu P, et al. Short-term effects of the toxic component of traffic-related air pollution (TRAP) on lung function in healthy adults using a powered air purifying respirator (PAPR). Environ Res. 2022;214:113745. https://doi.org/10.1016/J.ENVRES.2022.113745.
Acknowledgements
E. C. acknowledges the UConn Health Research Program and the UConn Office of Undergraduate Research for their support and resources. The authors thank Ms. Tony Vella for her assistance in reviewing the biological mechanisms of FeNO production.
Funding
M. L. Z. is supported by the National Institute of Environmental Health Sciences of the National Institutes of Health under award number R00ES029116.
Author information
Authors and Affiliations
Contributions
A.A. and M.L.Z. wrote the main manuscript text and E.C. prepared Table 1. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Anand, A., Castiglia, E. & Zamora, M.L. The Association Between Personal Air Pollution Exposures and Fractional Exhaled Nitric Oxide (FeNO): A Systematic Review. Curr Envir Health Rpt 11, 210–224 (2024). https://doi.org/10.1007/s40572-024-00430-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40572-024-00430-1