Abstract
Purpose of Review
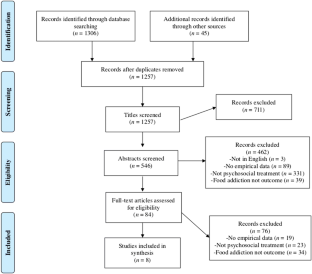
The current systematic review examined the empirical literature on psychosocial interventions for food addiction with the goal of providing recommendations for clinical practice and future research. A PsycINFO and PubMed search of publications was conducted in September 2019. Two authors assessed retrieved titles and abstracts to determine topic relevance and rated the quality of the included studies using an established checklist.
Recent Findings
Eight studies met the study inclusion criteria, and study quality ranged from “poor” to “fair”. Most studies were pilot and feasibility studies with limitations that impact the conclusions that can be drawn.
Summary
There are currently no empirically supported psychosocial interventions for food addiction. Additional research is warranted to develop and test the efficacy of interventions for food addiction. In the meantime, it is recommended that clinicians treating food addiction assess for comorbid eating disorders, and if present, first provide evidence-based treatments for those conditions.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Gordon EL, Ariel-Donges AH, Bauman V, Merlo LJ. What is the evidence for “food addiction”? A systematic review. Nutrients. 2018;12:477. https://doi.org/10.3390/nu10040477.
Fletcher PC, Kenny PJ. Food addiction: a valid concept? Neuropsychopharmacol. 2018;43:2506–13. https://doi.org/10.1038/s41386-018-0203-9.
Naish KR, MacKillop J, Balodis IM. The concept of food addiction: a review of the current evidence. Curr Behav Neurosci Rep. 2018;5:281–94. https://doi.org/10.1007/s40473-018-0169-2.
Ziauddeen H, Fletcher PC. Is food addiction a valid and useful concept? Obes Rev. 2013;14:19–28. https://doi.org/10.1111/j.1467-789X.2012.01046.x.
Gearhardt AN, Corbin WR, Brownell KD. Preliminary validation of the Yale food addiction scale. Appetite. 2009;52:430–6. https://doi.org/10.1016/j.appet.2008.12.003.
Meule A. Back by popular demand: a narrative review on the history of food addiction research. Yale J Biol Med. 2015;88:295.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington: American Psychiatric Publishing; 2013.
Meule A, Gearhardt AN. Five years of the Yale food addiction scale: taking stock and moving forward. Curr Addict Rep. 2014;1:193–205. https://doi.org/10.1007/s40429-014-0021-z.
Meule A, Geardhardt AN. Ten years of the Yale food addiction scale: a review of version 2.0. Curr Addict Rep. 2019;6:218–28. https://doi.org/10.1007/s40429-019-00261-3.
Penzenstadler L, Soares C, Karila L, Khazaal Y. Systematic review of food addiction as measured with the Yale food addiction scale: implications for the food addiction construct. Curr Neuropharmacol. 2019;17:526–38. https://doi.org/10.2174/1570159X16666181108093520.
Pursey KM, Stanwell P, Gearhardt AN, Collins CE, Burrows TL. The prevalence of food addiction as assessed by the Yale food addiction scale: a systematic review. Nutr. 2014;6:4552–90. https://doi.org/10.3390/nu6104552.
Ifland JR, Preuss HG, Marcus MT, Rourke KM, Taylor WC, Burau K, et al. Refined food addiction: a classic substance use disorder. Med Hypotheses. 2009;72:518–26. https://doi.org/10.1016/j.mehy.2008.11.035.
National Institute for Health and Care Excellence. Alcohol-use disorders: diagnosis, assessment, and management of harmful drinking (high-risk drinking) and alcohol dependence [Internet]. NICE; 2011 [updated 2019 July 19; cited 2019 Oct 28]. Available from https://www.nice.org.uk/guidance/cg115
National Institute for Health and Care Excellence. Eating disorders: recognition and treatment [Internet]. NICE; 2017 [updated 2017 May; cited 2019 Oct 28]. Available from https://www.nice.org.uk/guidance/ng69
Schulte EM, Joyner MA, Potenza MN, Grilo CM, Gearhardt AN. Current considerations regarding food addiction. Curr Psychiatry Rep. 2015;17:563. https://doi.org/10.1007/s11920-015-0563-3.
• Schulte EM, Grilo CM, Gearhardt AN. Shared and unique mechanisms underlying binge eating disorder and addictive disorders. Clin Psychol Rev. 2016;44:125–39. https://doi.org/10.1016/j.cpr.2016.02.001. This review paper examines the shared mechanisms and unique aspects of addiction and eating disorders and provides a guiding framework for future research. One recommendation is to evaluate whether treatment approaches for addictive disorders, such as abstinence-based or harm reduction approaches, are beneficial for food addiction.
Wilson GT. Eating disorders, obesity and addiction. Eur Eat Disord Rev. 2010;18:341–51. https://doi.org/10.1002/erv.1048.
•• Treasure J, Leslie M, Chami R, Fernández-Aranda F. Are trans diagnostic models of eating disorders fit for purpose? A consideration of the evidence for food addiction. Eur Eat Disord Rev. 2018;26:83–91. https://doi.org/10.1002/erv.2578. This paper proposes a food addiction model of binge eating behaviour and recommends specific targets for intervention, including reducing access to processed foods, reducing habit-based eating, reducing restriction of healthy foods, and improving emotion regulation.
•• Wiss DA, Brewerton TD. Incorporating food addiction into disordered eating: the disordered eating food addiction nutrition guide (DEFANG). Eat Weight Disord. 2017;22:49–59. https://doi.org/10.1007/s40519-016-0344-y. This paper examines the relationship between eating disorders and addictions and proposes a new model of conceptualizing and treating eating disorders that incorporates the concept of food addiction.
Adams RC, Sedgmond J, Maizey L, Chambers CD, Lawrence NS. Food addiction: implications for the diagnosis and treatment of overeating. Nutr. 2019;11:2086. https://doi.org/10.3390/nu11092086.
Davis C, Carter JC. If certain foods are addictive, how might this change the treatment of compulsive overeating and obesity? Curr Addict Rep. 2014;1:89–95. https://doi.org/10.1007/s40429-014-0013-z.
• Meule A. A critical examination of the practical implications derived from the food addiction concept. Curr Obes Rep. 2019;8:11–7. https://doi.org/10.1007/s13679-019-0326-2. This paper provides a thoughtful analysis of the potential clinical implications that arise from the concept of food addiction. The author suggests that food addiction may be a useful metaphor in the treatment of binge eating disorder, but calls into question the current clinical utility of food addiction.
• Schulte EM, Joyner MA, Schiestl ET, Gearhardt AN. Future directions in “food addiction”: next steps and treatment implications. Curr Addict Rep. 2017;4:165–71. https://doi.org/10.1007/s40429-017-0140-4. This paper discusses potential treatment implications of food addiction, including harm reduction approaches, exposure to food cues, coping skills for managing cravings, and strategies for improving emotion regulation.
• Vella SC, Pai NB. A narrative review of potential treatment strategies for food addiction. Eat Weight Disord. 2017;22:387–93. https://doi.org/10.1007/s40519-017-0400-2. This review article proposes treatment strategies for food addiction that target four key behaviours of the addiction phenotype: cravings, impulsivity, compulsivity, and motivation.
Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–84. https://doi.org/10.1136/jech.52.6.377.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:1–6. https://doi.org/10.1371/journal.pmed.1000097.
Trac MH, McArthur E, Jandoc R, Dixon SN, Nash DM, Hackam DG, et al. Macrolide antibiotics and the risk of ventricular arrhythmia in older adults. Can Med Assoc J. 2016;188:E120–9. https://doi.org/10.1503/cmaj.150901.
Hooper P, Jutai J, Strong G, Russell-Minda E. Age-related macular degeneration and low-vision rehabilitation: a systematic review. Can J Ophthalmol. 2008;43:180–7. https://doi.org/10.3129/i08-001.
Krippendorff K. Content analysis: an introduction to its methodology. Beverly Hills, CA: Sage; 1980.
Mount R, Neziroglu F, Taylor CJ. An obsessive-compulsive view of obesity and its treatment. J Clin Psychol. 1990;46:68–78. https://doi.org/10.1002/1097-4679(199001)46:1<68::AID-JCLP2270460112>3.0.CO;2-V.
Mason AE, Lustig RH, Brown RR, Acree M, Bacchetti P, Moran PJ, et al. Acute responses to opioidergic blockade as a biomarker of hedonic eating among obese women enrolled in a mindfulness-based weight loss intervention trial. Appetite. 2015;91:311–20. https://doi.org/10.1016/j.appet.2015.04.062.
Weinstein A, Zlatkes M, Gingis A, Lejoyeux M. The effects of a 12-step self-help group for compulsive eating on measures of food addiction, anxiety, depression, and self-efficacy. J Groups Addict Recovery. 2015;10:190–200. https://doi.org/10.1080/1556035X.2015.1034825.
Hilker I, Sánchez I, Steward T, Jiménez-Murcia S, Granero R, Gearhardt AN, et al. Food addiction in bulimia nervosa: clinical correlates and association with response to a brief psychoeducational intervention. Eur Eat Disord Rev. 2016;24:482–8. https://doi.org/10.1002/erv.2473.
Sawamoto R, Nozaki T, Nishihara T, Furukawa T, Hata T, Komaki G, et al. Predictors of successful long-term weight loss maintenance: a two-year follow-up. Biopsychosoc Med. 2017;11:14. https://doi.org/10.1186/s13030-017-0099-3.
Vidmar AP, Pretlow R, Borzutzky C, Wee CP, Fox DS, Fink C, et al. An addiction model-based mobile health weight loss intervention in adolescents with obesity. Pediatr Obes. 2019;14:e12464. https://doi.org/10.1111/ijpo.12464.
Webber KH, Mellin L, Mayes L, Mitrovic I, Saulnier M. Pilot investigation of 2 nondiet approaches to improve weight and health. Altern Ther Health Med. 2017;24:16–20.
Miller-Matero LR, Brescacin C, Clark SM, Troncone CL, Tobin ET. Why WAIT? Preliminary evaluation of the weight assistance and intervention techniques (WAIT) group. Psychol Health Med. 2019;24:1029–37. https://doi.org/10.1080/13548506.2019.1587478.
Chambless DL, Hollon SD. Defining empirically supported therapies. J Consul Clin Psychol. 1998;66:7–18.
Tolin DF, McKay D, Forman EM, Klonsky ED, Thombs BD. Empirically supported treatment: recommendations for a new model. Clin Psychol Sci Pract. 2015;22:317–38. https://doi.org/10.1111/cpsp.12122.
Davis CA. A commentary on the associations among ‘food addiction’, binge eating disorder, and obesity: overlapping conditions with idiosyncratic clinical features. Appetite. 2017;115:3–8. https://doi.org/10.1016/j.appet.2016.11.001.
Carter JC, van Wijk M, Rowsell M. Symptoms of ‘food addiction’ in binge eating disorder using the Yale food addiction scale version 2.0. Appetite. 2019;133:362–9. https://doi.org/10.1016/j.appet.2018.11.032.
Cassin SE, von Ranson KM. Is binge eating experienced as an addiction? Appetite. 2007;49:687–90. https://doi.org/10.1016/j.appet.2007.06.012.
Gormally J, Black S, Daston S, Rardin D. The assessment of binge eating severity among obese persons. Addict Behav. 1982;7:47–55. https://doi.org/10.1016/0306-4603(82)90024-7.
Latner JD, Mond JM, Kelly MC, Haynes SN, Hay PJ. The loss of control over eating scale: development and psychometric evaluation. Int J Eat Disord. 2014;47:647–59. https://doi.org/10.1002/eat.22296.
Owen P, Marlatt GA. Should abstinence be the goal for alcohol treatment? Am J Addict. 2001;10:289–95. https://doi.org/10.1080/aja.10.4.289.295.
Saladin ME, Santa Ana EJ. Controlled drinking: more than just a controversy. Curr Opin Psychiatry. 2004;17:175–87. https://doi.org/10.1097/01.yco.0000126547.69286.12.
Sackett DL, Rosenberg WM, Gray JM, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312:71–2. https://doi.org/10.1136/bmj.312.7023.71.
Peterson CB, Becker CB, Treasure J, Shafran R, Bryant-Waugh R. The three-legged stool of evidence-based practice in eating disorder treatment: research, clinical, and patient perspectives. BMC Med. 2016;14:69. https://doi.org/10.1186/s12916-016-0615-5.
Cassin SE, von Ranson KM, Heng K, Brar J, Wojtowicz AE. Adapted motivational interviewing for women with binge eating disorder: a randomized controlled trial. Psychol Addict Behav. 2008;22:417–25. https://doi.org/10.1037/0893-164X.22.3.417.
Knowles L, Anokhina A, Serpell L. Motivational interventions in the eating disorders: what is the evidence? Int J Eat Disord. 2013;46:97–107. https://doi.org/10.1002/eat.22053.
Linardon J, Messer M, Fuller-Tyszkiewicz M. Meta-analysis of the effects of cognitive-behavioral therapy for binge-eating-type disorders on abstinence rates in nonrandomized effectiveness studies: comparable outcomes to randomized, controlled trials? Int J Eat Disord. 2018;51:1303–11. https://doi.org/10.1002/eat.22986.
Linardon J. Rates of abstinence following psychological or behavioral treatments for binge-eating disorder: meta-analysis. Int J Eat Disord. 2018;51:785–97. https://doi.org/10.1002/eat.22897.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Food Addiction
Rights and permissions
About this article
Cite this article
Cassin, S.E., Sijercic, I. & Montemarano, V. Psychosocial Interventions for Food Addiction: a Systematic Review. Curr Addict Rep 7, 9–19 (2020). https://doi.org/10.1007/s40429-020-00295-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-020-00295-y



