Abstract
Introduction
There is inadequate information on blood pressure (BP) and FBG (Blood pressure and Fasting blood glucose) control among adult hypertensive patients in Southern Ethiopia.
Aim
To determine the level and factors associated with poor BP and FBG control among adult hypertensive patients on regular follow-up at three public hospitals
Results
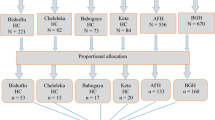
We included 406 adult hypertensives with mean age of 55.87 ± 11.03 years. Mean systolic BP was 134.46 ± 13.44 mmHg; and mean diastolic BP was 82.10 ± 9.44 mmHg. More than eight out of 205 (86.2%) of patients did not achieve BP and FBG target level. Having body mass index 18–24.9 kg/m2, Adjusted odds ratio (AOR) = 0.317 (95% C.I. for AOR, 0.135–0.740, p = 0.008); having no comorbidity, AOR = 0.425 (95% C.I. for AOR, 0.232–0.779, p = 0.006); physically activity, AOR = 0.303 (95% C.I., 0.110–0.829, p = 0.020); having low perceived health risk, AOR = 0.095 (95% C.I., 0.014–0.632, p = 0.015); taking monotherapy, AOR = 3.34 (95% C.I. for AOR, 1.121–10.524, p = 0.033); and history of hospitalization, AOR = 7.048 (95% C.I. for AOR, 2.486–19.954, p = 0.000) were associated with poor BP and FBG control.
Conclusions
The level of BP and FBG control was low. Improving screening of hypertensive patients for diabetes; addressing obesity and mental health; strengthening healthy life style interventions and enhancing appropriate dose intensification of prescribed anti-hypertensives by responsible bodies are critical to improve BP and FBG control.




Similar content being viewed by others
References
WHO. Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2016. Geneva: WHO; 2018.
Oti SO, van de Vijver SJM, Lange J. A community-based intervention for primary prevention of cardiovascular diseases in the slums of Nairobi: the SCALE UP study protocol for a prospective quasi-experimental community-based trial. Trials. 2013;14:409.
Plante TB, Koh I, Judd SE, Howard G, Howard VJ, Zakai NA, et al. Life’s Simple 7 and incident hypertension: the REGARDS study. J Am Heart Assoc. 2020;9:e016482.
Volpe M, Gallo G, Battistoni A, Tocci G. Implications of guidelines for hypertension management in Europe. Circ Res. 2019;124(7):972–4.
Region WSEA. Special Issue on Blood Pressure-take control. India2013 World Health Day.
Shiferaw F, Letebo M, Misganaw A, Feleke Y, Gelibo T, Getachew T, et al. Non-communicable Diseases in Ethiopia: disease burden, gaps in health care delivery and strategic directions. Ethiopian J Health Dev. 2018;32:3.
WHO. Health profile: Ethiopia. World Health Rankings: [Internet]. 2017. https://www.worldlifeexpectancy.com/country-health-profile/ethiopia.
Collaborators. GRF. Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 84 behavioral, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1923-94.
Cappuccio FP, Miller MA. Cardiovascular disease and hypertension in sub-Saharan Africa: burden, risk and interventions. Intern Emerg Med. 2016;11(3):299–305.
Ataklte F, Erqou S, Kaptoge S. 147 burden of undiagnosed hypertension in Sub-Saharan Africa: a systematic review and meta-analysis. Heart. 2015;101(Suppl 4):A84-A.
Institute. EPH. Ethiopia steps report on risk factors for chronic non-communicable diseases and prevalence of selected NCDs. 2016.
Organization WH. Global action plan for the prevention and control of noncommunicable diseases 2013-2020: World Health Organization; 2013.
Olsen MH, Angell SY, Asma S, Boutouyrie P, Burger D, Chirinos JA, et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the Lancet Commission on hypertension. Lancet. 2016;388(10060):2665–712.
McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–45.
Beaglehole R, Bonita R, Ezzati M, Alleyne G, Dain K, Kishore SP, et al. NCD Countdown 2025: accountability for the 25× 25 NCD mortality reduction target. Lancet. 2014;384(9938):105–7.
Norheim OF, Baltussen R, Johri M, Chisholm D, Nord E, Brock D, et al. Guidance on priority setting in health care (GPS-Health): the inclusion of equity criteria not captured by cost-effectiveness analysis. Cost Eff Resour Alloc. 2014;12:18.
World Health Organization. It’s time to walk the talk: WHO independent high-level commission on noncommunicable diseases final report. Geneva: World Health Organization; 2019. Licence: CC BY-NC-SA 3.0 IGO. 2019.
Ruhil R. The Changing Wealth of Nations 2018. Building a Sustainable Future. By Glenn-Marie Lange, Quentin Wodon and Kevin Carey; Washington DC: World Bank Group.© World Bank. IASSI-Quarterly. 2018;37(1):135–7.
Feyissa YM, Hanlon C, Emyu S, Cornick RV, Fairall L, Gebremichael D, Teka T, Shiferaw S, Walelgne W, Mamo Y, Segni H, Ayehu T, Wale M, Eastman T, Awotiwon A, Wattrus C, Picken SC, Ras C-J, Anderson L, Doherty T, Prince MJ, Tegabu D. Using a mentorship model to localize the Practical Approach to Care Kit (PACK): from South Africa to Ethiopia. BMJ Glob Health. 2019;3:e001108.
Muluneh AT, Tessema F, Alemseged F, Woldemichael K, Asefa M, et al. Population based survey of chronic non-communicable diseases at gilgel gibe field research center, southwest Ethiopia. Ethiop J Health Sci. 2012;22(Special Issue):7–18.
Elzinga G, Jerene D, Mesfin G, Negussie S. Human resources for health implications of scaling up for universal access to HIV/AIDS prevention, treatment, and care: Ethiopia Rapid Situational Analysis. Group GHWATW, editor Addis Ababa, Ethiopia. 2010.
Getachew T, Bekele A, Amenu K, Defar A, Teklie H, Taye G, et al. Service availability and readiness for major non-communicable diseases at health facilities in Ethiopia. Ethiopian J Health Dev. 2017;31(1):384–90.
Pascal Geldsetzer JG, Marcus ME, Ebert C, Zhumadilov Z, Wesseh CS, Tsabedze L, Supiyev A, Sturua L, Bahendeka SK, Sibai AM, Quesnel-Crooks S, Norov B, Mwangi KJ, Mwalim O, Wong-McClure R, Mayige MT, Martins JS, Jaacks LM. The state of hypertension care in 44 low-income and middle-income countries: a cross-sectional study of nationally representative individual-level data from 1·1 million adults. Lancet. 2019;6736(19):30955–9.
Katsarou A, Panagiotakos D, Zafeiropoulou A, Vryonis M, Skoularigis I, Tryposkiadis F, et al. Validation of a Greek version of PSS-14; a global measure of perceived stress. Cent Eur J Public Health. 2012;20(2):104–9.
Almadi T, Cathers I, Mansour AMH, Chow CM. An Arabic version of the Perceived Stress Scale: translation and validation study. Int J Nurs Stud. 2012;49(1):84–9.
Roberti JW, Harrington LN, Storch EA. Further psychometric support for the 10-item version of the perceived stress scale. J Coll Couns. 2006;9(2):135–47.
Löwe B, Kroenke K, Herzog W, Gräfe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). J Affect Disord. 2004;81(1):61–6.
Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. CMAJ. 2012;184(3):E191–6.
Gierveld JDJ, Tilburg TV. A 6-item scale for overall, emotional, and social loneliness: confirmatory tests on survey data. Res Aging. 2006;28(5):582–98.
Kriston L, Scholl I, Hölzel L, Simon D, Loh A, Härter M. The 9-item Shared Decision Making Questionnaire (SDM-Q-9). Development and psychometric properties in a primary care sample. Patient Educ Couns. 2010;80(1):94–9.
Cockcroft DW, Gault H. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16(1):31–41.
Coresh J, Stevens L. Kidney function estimating equations: where do we stand? Curr Opin Nephrol Hypertens. 2006;15(3):276–84.
Vouri SM, Shaw RF, Waterbury NV, Egge JA, Alexander B. Prevalence of achievement of A1c, blood pressure, and cholesterol (ABC) goal in veterans with diabetes. J Manag Care Pharm. 2011;17(4):304–12.
Whelton PKCR, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–115.
Federal Democratic Republic of Ethiopia Ministry of Health. Guidelines on Clinical and Programmatic Management of Major Non Communicable Diseases. 2016.
Association AD. 6 Glycemic targets: standards of medical care in diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S66.
Buse JB, Wexler DJ, Tsapas A, Rossing P, Mingrone G, Mathieu C, et al. 2019 update to: Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2020;63(2):221–8.
Volpe M, Gallo G, Modena MG, Ferri C, Desideri G, Tocci G, et al. Updated Recommendations on Cardiovascular Prevention in 2022: an Executive Document of the Italian Society of Cardiovascular Prevention. High Blood Press Cardiovasc Prevent. 2022;29(2):91–102.
Smith SC Jr, Jackson R, Pearson TA, Fuster V, Yusuf S, Faergeman O, et al. Principles for national and regional guidelines on cardiovascular disease prevention: a scientific statement from the World Heart and Stroke Forum. Circulation. 2004;109(25):3112–21.
Price AJ, Crampin AC, Amberbir A, Kayuni-Chihana N, Musicha C, Tafatatha T, et al. Prevalence of obesity, hypertension, and diabetes, and cascade of care in sub-Saharan Africa: a cross-sectional, population-based study in rural and urban Malawi. Lancet Diabetes Endocrinol. 2018;6(3):208–22.
Goverwa TP, Masuka N, Tshimanga M, Gombe NT, Takundwa L, Bangure D, et al. Uncontrolled hypertension among hypertensive patients on treatment in Lupane District, Zimbabwe, 2012. BMC Res Notes. 2014;7(1):703.
Sintayehu MTM, Legese C, Desta A. Blood pressure control and its determinants among diabetes mellitus comorbid hypertensive patients at Jimma University medical center, South West Ethiopia. Clin Hypertension. 2017;3:29.
Gebrewahd Bezabh G. Uncontrolled hypertension and associated factors among adult hypertensive patients in Ayder comprehensive specialized hospital, Tigray, Ethiopia, 2018. BMC Cardiovasc Disord. 2019;19:121.
Yazie DSW, Alebachew M, Berha AB. Assessment of Blood Pressure Control among Hypertensive Patients in Zewditu Memorial Hospital, Addis Ababa, Ethiopia: a cross-sectional study. J Bioanal Biomed. 2018;10:80–7.
Berhe DF, Taxis K, Haaijer-Ruskamp FM, Mulugeta A, Mengistu YT, Mol PGM. Hypertension treatment practices and its determinants among ambulatory patients: retrospective cohort study in Ethiopia. BMJ Open. 2017;7(8): e015743.
Rachlis B, Naanyu V, Wachira J, Genberg B, Koech B, Kamene R, et al. Community Perceptions of Community Health Workers (CHWs) and Their Roles in Management for HIV, Tuberculosis and Hypertension in Western Kenya. PLoS ONE. 2016;11(2):e0149412.
Woldegebriel AS, Gudina EK, Alemu DT. Assessment of blood pressure control among hypertensive patients in southwest Ethiopia. PLoS ONE. 2016;11(11):e0166432.
Muleta S, Melaku T, Chelkeba L, Assefa D. Blood pressure control and its determinants among diabetes mellitus co-morbid hypertensive patients at Jimma University medical center, South West Ethiopia. Clin Hypertens. 2017;23:29.
Teshome DFDA, Zeleke BM. Determinants of blood pressure control amongst hypertensive patients in Northwest Ethiopia. PLoS ONE. 2018;13(5):e0196535.
Gareth Beevers GYHL, O'Brien E. ABC of Hypertension, 6th edn. Series A, editor 2014.
Arnett DKBR, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd-Jones D, McEvoy JW, Michos ED, Miedema MD, Muñoz D, Smith SC Jr, Virani SS, Williams KA Sr, Yeboah J, Ziaeian B. ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140:e563–95.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International society of hypertension global hypertension practice guidelines. Hypertension. 2020;75(00):1–25.
Lee HS, Park YM, Han K, Yang JH, Kim SR. Impact of overweight and obesity in prevalence and management of hypertension. Circulation. 2017. https://doi.org/10.1161/circ.135.suppl_1.p268.
Yusuf S, Hawken S, Ôunpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–52.
O'donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. The Lancet. 2010;376(9735):112-23.
Drawz PE, Alper AB, Anderson AH, Brecklin CS, Charleston J, Chen J, et al. Masked hypertension and elevated nighttime blood pressure in CKD: prevalence and association with target organ damage. Clin J Am Soc Nephrol. 2016;11(4):642–52.
Di Palo KE, Barone NJ. Hypertension and heart failure: prevention, targets, and treatment. Heart Fail Clin. 2020;16(1):99–106.
Farsang C, Kiss I, Tykarski A, Narkiewicz K. Treatment of hypertension in patients with chronic obstructive pulmonary disease (COPD). Eur Soc Hypertens Sci Newslett. 2016;17:62.
Marathe PH, Gao HX, Close KL. American D iabetes A ssociation S tandards of M edical C are in D iabetes 2017. J Diabetes. 2017;9(4):320–4.
Sever PS, Poulter NR, Dahlöf B, Wedel H, Collins R, Beevers G, et al. Reduction in cardiovascular events with atorvastatin in 2,532 patients with type 2 diabetes: Anglo-Scandinavian Cardiac Outcomes Trial–lipid-lowering arm (ASCOT-LLA). Diabetes Care. 2005;28(5):1151–7.
Agca R, Heslinga S, Rollefstad S, Heslinga M, McInnes I, Peters M, et al. EULAR recommendations for cardiovascular disease risk management in patients with rheumatoid arthritis and other forms of inflammatory joint disorders: 2015/2016 update. Ann Rheum Dis. 2017;76(1):17–28.
Patten SB, Williams JV, Lavorato DH, Campbell NR, Eliasziw M, Campbell TS. Major depression as a risk factor for high blood pressure: epidemiologic evidence from a national longitudinal study. Psychosom Med. 2009;71(3):273–9.
Noh J, Kim HC, Shin A, Yeom H, Jang S-Y, Lee JH, et al. Prevalence of Comorbidity among People with Hypertension: The Korea National Health and Nutrition Examination Survey 2007–2013. Korean Circ J. 2016;46(5):672–80.
Ose D, Miksch A, Urban E, Natanzon I, Szecsenyi J, Kunz CU, et al. Health related quality of life and comorbidity. A descriptive analysis comparing EQ-5D dimensions of patients in the German disease management program for type 2 diabetes and patients in routine care. BMC Health Serv Res. 2011;11(1):179.
Valderas JM, Starfield B, Sibbald B, Salisbury C, Roland M. Defining comorbidity: implications for understanding health and health services. Ann Family Med. 2009;7(4):357–63.
Chokshi NP, Grossman E, Messerli FH. Blood pressure and diabetes: vicious twins. Heart. 2013;99(8):577.
Achwoka D, Waruru A, Chen TH, Masamaro K, Ngugi E, Kimani M, et al. Noncommunicable disease burden among HIV patients in care: a national retrospective longitudinal analysis of HIV-treatment outcomes in Kenya, 2003–2013. BMC Public Health. 2019;19(1):372.
Belaunzaran-Zamudio PF, Caro-Vega Y, Giganti MJ, Castilho JL, Crabtree-Ramirez BE, Shepherd BE, et al. Frequency of non-communicable diseases in people 50 years of age and older receiving HIV care in Latin America. PLoS ONE. 2020;15(6):e0233965.
Chireshe R, Naidoo K, Nyamakura R. Hypertension among human immunodeficiency virus infected patients on treatment at Parirenyatwa Hospital: a descriptive study. African J Primary Health Care Family Med. 2019;11(1):e1–8.
Gerin WCW, Schwartz JE, et al. Sustained blood pressure increase after an acute stressor: the effects of the 11 September 2001 attack on the New York City World Trade Center. J Hypertens. 2005;23:279–84.
Dimsdale JEZM, Mills P. Renin correlates with blood pressure reactivity to stressors. Neuropschopharmacology. 1990;3:237–42.
Scalco AZ, Scalco MZ, Azul JBS, Lotufo NF. Hypertension and depression. Clinics. 2005;60(3):241–50.
Kretchy IA, Owusu-Daaku FT, Danquah SA. Mental health in hypertension: assessing symptoms of anxiety, depression and stress on anti-hypertensive medication adherence. Int J Mental Health Syst. 2014;8(1):25.
Sandström YK, Ljunggren G, Wändell P, Wahlström L, Carlsson AC. Psychiatric comorbidities in patients with hypertension—a study of registered diagnoses 2009–2013 in the total population in Stockholm County, Sweden. J Hypertens. 2016;34(3):414–20.
Biondi-Zoccai G, Mazza M, Roever L, van Dixhoorn J, Frati G, A. A. Evidence-Based Psychotherapy in Ischemic Heart Disease: Umbrella Review and Updated Meta-Analysis. In: Roncella A., C P, editors. Psychotherapy for Ischemic Heart Disease: Springer, Cham; 2016. p. 131–58.
Organization. WH. Global action plan for the prevention and control of non-communicable diseases 2013–2020. 2013.
Cicero AFG, Veronesi M, Fogacci F. Dietary intervention to improve blood pressure control: beyond salt restriction. High Blood Press Cardiovasc Prev. 2021;28(6):547–53.
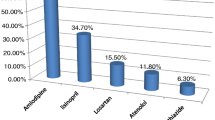
Busser D, Yarlagadda R, Ahmed SM. Assessment of Antihypertensive Drugs Utilization Pattern in Butajira Zonal Hospital, Butajira Town, South Ethiopia. Int J Pharm Sci Res. 2016;7(10):4028.
Fufa F, Mirkano D, Tipathi R. Prescription Pattern and Potential Drug-Drug Interactions of Antihypertensive Drugs in a General Hospital, South Ethiopia. Cukurova Med J. 2015;40:698–706.
Jarari N, Rao N, Peela JR, Ellafi KA, Shakila S, Said AR, et al. A review on prescribing patterns of antihypertensive drugs. Clin Hypertens. 2016;22(1):7.
Catić T, Begović B. Outpatient antihypertensive drug utilization in Canton Sarajevo during five years period (2004–2008) and adherence to treatment guidelines assessment. Bosn J Basic Med Sci. 2011;11(2):97–102.
Suchard MA, Schuemie MJ, Krumholz HM, You SC, Chen R, Pratt N, et al. Comprehensive comparative effectiveness and safety of first-line antihypertensive drug classes: a systematic, multinational, large-scale analysis. Lancet. 2019;394(10211):1816–26.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42(9):1235–481.
Acknowledgements
We would like to thank all patients participated in this study for their valuable dedication to provide information, We would also like to thank Arba Minch University college of medicine and health sciences and Tehran University medical sciences, department of pharmacoeconomics and Pharmaceutical Administration staffs for their technical and material support during this manuscript development.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
There is no funding source for the study.
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
The study was approved by Tehran University of medical sciences, Faculty of pharmacy, department of pharmacoeconomics, and pharmaceutical administration ethical review board with Approval ID: IR.TUMS.MEDICINE.REC.1399.674 and Arba Minch University College of medicine and health sciences Institutional review board with Reference number: IRB/T10/2012. After clarifying the study objective and confidentiality of the information; verbal informed consent was obtained from each respective hospital before data collection.
Consent for publication
All authors read the full version of this manuscript and agreed to publish.
Availability of data and materials
All the data reported in the manuscript are publicly available up on official request of principal investigator upon acceptance of the manuscript.
Code availability
Not applicable.
Authors’ contributions
All Authors read and approved the manuscript. MM conceived the research, framed the format design and developed the manuscript for publication; MD participated in data analysis and reviewed the manuscript and AK reviewed the manuscript and write-up process; NS and TS, participated in literature review and polished the language of the manuscript.
Rights and permissions
About this article
Cite this article
Sorato, M.M., Davari, M., Kebriaeezadeh, A. et al. Blood Pressure and Blood Glucose Control and Associated Factors Among Adults with Hypertension at Three Public Hospitals in Southern Ethiopia. High Blood Press Cardiovasc Prev 29, 287–304 (2022). https://doi.org/10.1007/s40292-022-00516-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-022-00516-7