Abstract
Patients recovering from COVID-19 often report symptoms of exhaustion, fatigue and dyspnoea and present with exercise intolerance persisting for months post-infection. Numerous studies investigated these sequelae and their possible underlying mechanisms using cardiopulmonary exercise testing. We aimed to provide an in-depth discussion as well as an overview of the contribution of selected organ systems to exercise intolerance based on the Wasserman gears. The gears represent the pulmonary system, cardiovascular system, and periphery/musculature and mitochondria. Thirty-two studies that examined adult patients post-COVID-19 via cardiopulmonary exercise testing were included. In 22 of 26 studies reporting cardiorespiratory fitness (herein defined as peak oxygen uptake—VO2peak), VO2peak was < 90% of predicted value in patients. VO2peak was notably below normal even in the long-term. Given the available evidence, the contribution of respiratory function to low VO2peak seems to be only minor except for lung diffusion capacity. The prevalence of low lung diffusion capacity was high in the included studies. The cardiovascular system might contribute to low VO2peak via subnormal cardiac output due to chronotropic incompetence and reduced stroke volume, especially in the first months post-infection. Chronotropic incompetence was similarly present in the moderate- and long-term follow-up. However, contrary findings exist. Peripheral factors such as muscle mass, strength and perfusion, mitochondrial function, or arteriovenous oxygen difference may also contribute to low VO2peak. More data are required, however. The findings of this review do not support deconditioning as the primary mechanism of low VO2peak post-COVID-19. Post-COVID-19 sequelae are multifaceted and require individual diagnosis and treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Exercise intolerance post-COVID-19 may likely have several causes and is not solely explained by deconditioning. |
Peripheral followed by cardiovascular factors as well as lung diffusion limitations are central for long-term sequelae. |
This work will improve the understanding of possible underlying mechanisms of low cardiorespiratory fitness post-COVID-19 and at the same time promote cardiopulmonary exercise testing as a valuable diagnostic tool in patients post-COVID-19. Based on this, more targeted rehabilitation programmes could be developed in the future. |
1 Introduction
Coronavirus disease 2019 (COVID-19) constitutes a tremendous burden for health care systems worldwide. Despite great research efforts and state-of-the-art treatment, approximately 15% of patients post-COVID-19 present with physiological and psychological symptoms of exhaustion (i.e. dyspnoea, fatigue, dizziness) persisting for several months post-infection [1]. These sequelae may be less frequent in individuals that received at least two doses of a two-dose COVID-19 vaccine regimen [2]. Cardiorespiratory fitness (CRF, herein defined as peak oxygen uptake—\(\dot{V}\)O2peak), a powerful predictor of mortality and risk factor for the development of numerous diseases [3], is commonly below normal in these patients, even up to 9 months post-infection [4,5,6]. Simultaneously, \(\dot{V}\)O2peak is inversely associated with the risk of severe COVID-19 and hospitalisation [7].
\(\dot{V}\)O2peak represents the maximal oxidative metabolic capacity or maximal oxygen supply dependent on the aerobic fitness and health status of an individual [8, 9]. \(\dot{V}\)O2peak relies on the interplay between the three gears—pulmonary system, cardiovascular system, and periphery/skeletal musculature system and mitochondria [8, 9]. The Gear system was originally introduced by Wasserman describing the interdependency of these three gears that together determine \(\dot{V}\)O2peak. It also helps to explain the origin of impaired \(\dot{V}\)O2peak (see Fig. 1).
The figure illustrates leverage points through which COVID-19 could directly and/or indirectly induce low \(\dot{V}\)O2peak and exercise intolerance in patients post-COVID-19. Parameters on the left side of the figure reflect the status quo of the gears (i.e. pulmonary system, cardiovascular system and periphery) and are indicative of organ limitations. The original concept of the gear system explaining determinants of \(\dot{V}\)O2peak is available in Wasserman [9]. a-vO2 diff arteriovenous oxygen difference. CO cardiac output, COVID-19 coronavirus disease 2019, CRF cardiorespiratory fitness, FEV1 forced expiratory volume in 1 s, FVC forced vital capacity, Hb haemoglobin, HR heart rate, SV stroke volume, \(\dot{V}\)O2peak peak oxygen uptake
Recent studies have focused on uncovering potential underlying mechanisms of short- to long-term consequences of COVID-19 for \(\dot{V}\)O2peak. However, to the best of our knowledge, there is no review providing an in-depth overview for researchers, clinicians, and healthcare professionals.
Thus, this narrative review aims to fill this research gap. Furthermore, the aim was to discuss the contribution of the three gears as well as their alterations to low \(\dot{V}\)O2peak.
2 Methods
A narrative review with a systematic approach was chosen as the study design because the aim was to primarily improve the understanding of COVID-19-related sequelae for \(\dot{V}\)O2peak and possible underlying mechanisms, while secondarily constituting an exhaustive summary of pertinent literature. In systematic reviews, the focus is usually on the latter.
The databases Medline, EMBASE (on Ovid) and Covid-19 L.OVE by Epistemonikos were searched using the search strategies presented in Online Resource 1 (see electronic supplementary material [ESM]) through January 2022 to identify key publications. Furthermore, backwards and forwards citation tracking was done for all included studies. Relevant articles had to assess \(\dot{V}\)O2peak by cardiopulmonary exercise testing (CPET) in adults. There were no language restrictions. Case studies/series and conference abstracts were excluded. For this review, we defined short term as up to 1 month, moderate term as > 1 to 5 months, and long term as > 5 months after COVID-19 diagnosis or hospital discharge [10].
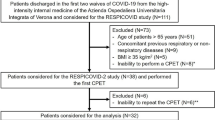
The searches yielded a total of 139 studies. After deduplication in EndNote X9.3.3 (Clarivate, Philadelphia, USA), 106 studies were screened for eligibility. The Rayyan web application [11] was used to document the decision of inclusion or exclusion. Twenty studies fulfilled the inclusion criteria. Citation tracking produced 12 additional studies. After applying the eligibility criteria, we ultimately included 32 studies in this review. Of those, 29 studies included patients hospitalised due to COVID-19 (at least moderate COVID-19) [12]. Three studies examined elite athletes. These are presented in Table 1 but not discussed explicitly as they are not representative of the general population (i.e. considerably higher \(\dot{V}\)O2peak, better health status, lower median age) [13,14,15]. The total number of patients with CPET data was 1817. Four studies provided longitudinal data [13, 16,17,18].
3 Results and Discussion
3.1 Cardiorespiratory Fitness
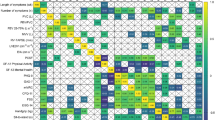
In 22 out of 26 studies (two studies are counted twice as they reported a second measurement point) examining patients post-COVID-19, \(\dot{V}\)O2peak of patients was < 90% of predicted. Figure 2A illustrates that \(\dot{V}\)O2peak is markedly low shortly after hospital discharge. Furthermore, it is remarkable that even in the long term \(\dot{V}\)O2peak is noticeably low. Interestingly, there seems to be no change in \(\dot{V}\)O2peak from mid- to long-term follow-up, which could be due to the following reasons: (i) inactivity-related effects during the hospital stay [19, 20], (ii) direct COVID-19-related sequelae [21, 22], (iii) side effects of drug treatment [23, 24], and (iv) pre-morbid \(\dot{V}\)O2peak may have been low. Regardless of whether \(\dot{V}\)O2peak is low due to a past COVID-19 infection or if patients with lower \(\dot{V}\)O2peak are more likely to have more severe disease progression, improving \(\dot{V}\)O2peak will most likely reduce the risk of all-cause mortality as well as the risk for non-communicable diseases in these patients in the future [3]. The following sections will discuss the contribution of the three gears to low \(\dot{V}\)O2peak.
Medians of \(\dot{V}\)O2peak (A), DLCO (B) and V̇E/V̇CO2 (C) weighted by sample size of respective studies or study visits in case a cohort was tested several times. Bubble area represents the sample size of studies. Bubble colour reflects COVID-19 severity of the majority of patients in the respective study (yellow = mild, dark red = critical). Grey bubbles: classification according to COVID-19 severity not possible. DLCO lung diffusion capacity using carbon monoxide, LT long term, MT medium term, ST short term, V̇E/V̇CO2 ventilatory efficiency, \(\dot{V}\)O2peak peak oxygen uptake
3.2 Pulmonary System (Gear 1)
The pulmonary system is a central component in the supply chain of oxygen delivery to the working muscles [9]. While the pulmonary system usually is not the limiting factor of \(\dot{V}\)O2peak in healthy individuals at sea level [8], it may well be in certain patient populations such as chronic obstructive pulmonary disease patients [25]. Ventilatory disorders are traditionally diagnosed using spirometry at rest measuring forced expiratory volume in 1 s (FEV1), forced vital capacity (FVC) and the ratio of the two (FEV1/FVC) [26]. Using CPET, ventilatory and pulmonary-vascular limitations are recognised by a reduced ventilatory capacity (breathing reserve at peak exercise), an abnormal ventilatory response, ventilatory inefficiency, or ventilation/perfusion mismatching (panels 1, 4, 6, 7, 9 in the original Wasserman 9-panel graph) [27].
A recent meta-analysis included 894 patients recovering from COVID-19 and presenting with abnormalities in lung function [28]. The prevalences of low total lung capacity, low FVC and low FEV1 were 14%, 12% and 7%, respectively [28]. These findings are in line with the studies summarised in Tables 1, 2, 3 that reported low \(\dot{V}\)O2peak [4, 5, 17, 29,30,31,32,33,34,35,36,37,38,39]. On the day of hospital discharge, impaired lung function has been reported in only two studies [24, 40]. Overall, within the first months post-infection, restrictive lung disease does not seem to be responsible for low \(\dot{V}\)O2peak [5, 18, 29,30,31, 41,42,43,44]. A German cohort study performed body plethysmography in 443 mainly non-hospitalised patients at a median of 10 months post-infection as well as in healthy controls [45]. Patients showed somewhat lower total lung capacity (99.1% vs 102.4% of predicted; p = 0.014) and higher airway resistance (77.3% vs 69.8% of predicted; p = 0.001) than controls [45]. Lung capacity, in contrast to airway resistance, however, is unlikely to affect \(\dot{V}\)O2peak due to the overcapacity of human lungs [8, 46]. In addition, impairments in lung function cannot be ruled out by solely comparing them to normative data. Thus, pre-infection data are needed.
In brief, the prevalence of restrictive lung disease seems to decrease with progressing recovery [4, 5, 17, 29,30,31,32,33,34,35,36,37,38,39]. The presented evidence indicates a negligible role of respiratory limitations detectable via spirometry to low \(\dot{V}\)O2peak, which is true for healthy individuals as well as patients recovering from COVID-19 (see Tables 1, 2, 3). Nonetheless, routine spirometry assessments may benefit patients with persistent restrictive lung disease and/or pre-existing respiratory disorders. Lung diffusion capacity measured by a single breath of carbon monoxide (DLCO) is of interest as a marker of diffusive limitations [17, 47]. DLCO may provide additional information on pulmonary-vascular limitations in the gear system [17, 27, 47]. As apparent from Fig. 2B, DLCO seems to recover slowly. Within the first 4 months post-infection, DLCO ranged between 69 and 84% of predicted [5, 16, 29, 32, 33, 42, 43]. Yet, even in the two studies showing higher mean values in DLCO (84% and 82%), 20% and 40% of patients were diagnosed with mild to moderate alterations [5, 43]. A longitudinal study examining patients 1.6 months and 6 months post-infection demonstrated that more than half of those patients without prolonged post-COVID-19 syndrome still had impaired DLCO [17]. Finally, at 6 and 9 months after hospital discharge, DLCO was around 90% of predicted [38, 39]. The combined evidence indicates that impairments in DLCO are more prevalent than restrictive lung disease in patients. This is supported by two meta-analyses in patients post-COVID-19 [28, 48], which showed that 6 months after discharge, 43% of patients still had a DLCO < 80% of predicted [48]. Considering this great fraction of patients with markedly low DLCO, impaired lung diffusion capacity may contribute to low \(\dot{V}\)O2peak in some patients [49]. The association between \(\dot{V}\)O2peak and DLCO is reported elsewhere [49].
As DLCO is a mathematical product of alveolar carbon monoxide uptake efficiency and alveolar volume, impairments may be due to either one or both of these parameters [50]. Limitations in alveolar carbon monoxide uptake efficiency may be explained by COVID-19-induced alveolar capillary damage, microvascular involvement or anaemia [51]. Restrictions in alveolar volume may be caused by microvascular injuries followed by the development of alveolar abnormalities with gradual loss of alveolar spaces [50]. Future studies might consider determining lung diffusion capacity by DLCO and additionally using nitric oxide (DLNO). DLNO has been suggested to be more sensitive than DLCO for detecting alterations in gas transport in patients post-COVID-19 [47, 52]. Gas transport abnormalities were proposed to be due to loss of alveolar units with alveolar membrane damage but relatively preserved capillary volume [47]. These may only be detected using nitric oxide [47]. Hyperpolarised xenon magnetic resonance imaging is a method that has lately been applied in some studies on COVID-19 [53]. Grist et al. [53] found impaired pulmonary gas transfer in seven of eleven non-hospitalised patients post-COVID-19 on average 287 days post-infection. The patients had normal CT scans [53]. These results and the strong correlation with DLCO findings suggest that hyperpolarised xenon magnetic resonance imaging may be a useful method to identify potentially undetected lung abnormalities in patients post-COVID-19 [53].
A normal to increased breathing reserve during exercise was commonly seen in studies with short-term [24, 40, 54], middle-term [4, 5, 16, 17, 29, 31,32,33, 43, 55], and long-term follow-up [6, 34,35,36, 38, 39] of patients post-COVID-19. This argues against respiratory limitations to V̇O2peak but does not rule out impaired lung diffusion capacity.
The ventilatory equivalent (measured as \(\dot{V}\)E/\(\dot{V}\)CO2) is a widely studied parameter of CPET [56] and a marker for ventilatory efficiency. A \(\dot{V}\)E/\(\dot{V}\)CO2 > 35 is often considered an indicator of ventilatory inefficiency which is a hallmark of pulmonary arterial hypertension (although not specific to this condition) [56]. \(\dot{V}\)E/\(\dot{V}\)CO2 has thus been suggested as a valuable marker of early cardiovascular disease [56]. Notably, ventilatory inefficiency does not correspond well with reduced breathing reserve [57]. Ventilatory inefficiency may thus be present even with normal breathing reserve [57].
As apparent in Tables 1, 2, 3, the prevalence of ventilatory inefficiency up to 3 months post-hospital discharge ranged between 15 and 32% [32, 43], and remained around 10–29% thereafter [32,33,34, 38, 55, 58]. However, in 94% of studies, the mean of \(\dot{V}\)E/\(\dot{V}\)CO2 was < 35 (see Table 1 and Fig. 2C). We hypothesise that one of the mechanisms leading to ventilatory inefficiency may be induced by impaired pulmonary endothelial function and not respiratory limitations per se [56]. The thereby elicited changes such as pulmonary arterial obstruction, increased mean pulmonary arterial pressure, as well as a reduced capillary bed, may, in turn, lead to ventilation/perfusion mismatching [56]. This may ultimately result in dyspnoea and reduced \(\dot{V}\)O2peak [56]. Consequently, examinations of ventilatory perfusion would provide valuable information regarding the involvement of the pulmonary vasculature.
Dysfunctional breathing is another aspect that should be discussed in light of the prevalence of ventilatory inefficiency as a potential contributing factor to exercise intolerance as well as post-COVID-19 symptoms such as dyspnoea or fatigue [42]. Skjørten et al. [5] found 3 months post-discharge that in those with ventilatory inefficiency (15% of the cohort), around 45% of cases could be attributed to dysfunctional breathing followed by circulatory (38%) and ventilatory limitations (17%). Motiejunaite et al. [43] likewise reported exercise hyperventilation as the main limitation in 16% of patients and a potential cause of dyspnoea. These studies show that dysfunctional breathing deserves investigation in patients post-COVID-19.
3.3 Cardiovascular System (Gear 2)
The cardiovascular system is essential for the supply of oxygenated haemoglobin in the blood to the working muscles. Cardiovascular limitations can be identified via CPET by maximum heart rate being below the lower limit of normal, an abnormal increase of oxygen uptake or O2-pulse in relation to work rate, reduced ventilatory threshold 1 (VT1), or an abnormal heart rate/\(\dot{V}\)O2 slope (panels 2, 3, 4, 5 in the original Wasserman 9-panel graph) [27].
The supply capacity of O2 by the cardiovascular system is aside from the haemoglobin concentration in the blood reflected by cardiac output (stroke volume [SV] × heart rate) in Fick’s equation [9]. The majority of included studies reported O2-pulse as an estimate for SV calculated as oxygen uptake/heart rate at that stage [59]. Importantly, O2-pulse is equal to SV × arteriovenous oxygen difference [27]. It thus needs to be considered that in contrast to SV, O2-pulse may be altered by changes in the O2-carrying capacity of the blood, O2 uptake or heart rate when interpreting this parameter [59]. O2 uptake and heart rate can therefore directly impact the calculation of O2-pulse. A better capability of the mitochondria to utilise O2 would raise oxygen uptake and thereby lead to a higher O2-pulse, although SV may be indeed unaltered. Similarly, a lower maximum heart rate (e.g. as a consequence of COVID-19 or exercise training) would impact the calculation. It is thus not entirely clear whether the lower O2-pulse truly reflects a decreased SV or if it may be due to either chronotropic incompetence (failing to increase heart rate proportionately to work rate) [60], changes in the oxygen-carrying capacity and thus lower haemoglobin mass, or peripheral changes (i.e. arteriovenous oxygen difference) [59].
Up to 4 months post-infection, there were six studies [5, 16, 31, 33, 42, 44] reporting normal O2-pulse, of which three found at least mild chronotropic incompetence (see Tables 1, 2). Another study additionally performed stress-echocardiography, an indirect imaging method to obtain more precise estimates of cardiac output compared with O2-pulse [24]. Intriguingly, cardiac output did not differ between patients (n = 18) and controls despite lower O2-pulse and mild chronotropic incompetence in patients [24]. However, this was accompanied by a lower arterial blood O2-content than in controls [24]. While this demonstrates the difficulty of using O2-pulse as an estimate of SV, it shows that SV may indeed be (super-)normal since heart rate was below normal but cardiac output was similar to controls. The authors speculated that potentially persisting autonomic imbalance [24, 61] associated with suboptimal distribution of cardiac output to the working musculature could have led to low peripheral oxygen extraction [24]. This might, in turn, impair \(\dot{V}\)O2peak [24]. These findings should, however, be interpreted with caution due to the small sample size. In contrast, lower estimated mean SV was seen in five studies between hospital discharge and 3.5 months post-infection by calculating O2-pulse [17, 24, 32, 43, 54]. While in Jahn et al. [31], O2-pulse was normal in the full sample, it was significantly lower when comparing patients stratified by low versus ‘normal’ \(\dot{V}\)O2peak (defined as \(\dot{V}\)O2peak > 82% of predicted). Moreover, one study assessed cardiac function by using stress-echocardiography 3 months after symptom onset [4]. Szekely et al. [4] observed lower left ventricular end-diastolic volume and ejection fraction, lower SV and lower cardiac output at all stages of exertion in patients compared with controls. In addition, the prevalence of chronotropic incompetence in this study was much higher in patients than in risk factor-matched controls (75% vs 8%) [4]. Following 4 months post-infection, SV and O2-pulse had normalised in most studies (see Table 2). The reversibility of low O2-pulse was further demonstrated by one longitudinal study [17], which showed that mean O2-pulse significantly improved from 91 to 95% of predicted up to 6 months post-infection. These findings are in line with a study by Vannini et al. [35] in patients with mild and severe COVID-19-induced pneumonia as well as acute respiratory distress syndrome, showing normal to supernormal cardiac output values at 6 months post-infection. Lastly, 11 months post-infection, cardiac output and peak oxygen delivery (calculated as arterial O2 content × cardiac output) were normal in a cohort with mainly mild COVID-19 but unexplained dyspnoea (n = 10) [58]. Apart from that, lower biventricular filling pressures, arguing against cardiovascular deconditioning, were apparent [58]. The authors concluded that cardiac limitations were absent and pointed toward the periphery as the main reason for impaired \(\dot{V}\)O2peak [58]. Noticeable in this study was the pronounced reduction in \(\dot{V}\)O2peak (70% of predicted) [58] compared with other studies ranging between 81 and 88% of predicted. However, small sample sizes and the choice of O2-pulse as an outcome measure might have been an issue in these studies. The Hamburg City Health Study (n = 443 patients post-COVID-19) found a slightly lower left-ventricular ejection fraction determined by echocardiography that was accompanied by higher levels of cardiac biomarkers in mostly non-hospitalised patients compared with controls at 10 months post-infection [45]. However, this difference was not present in cardiac MRI measures [45]. Interpretation of these results may therefore require some caution. In combination with low \(\dot{V}\)O2peak, another study reported 46% of patients being below 80% of predicted O2-pulse at 6 months post-discharge [37]. Because no heart rate data or information on arteriovenous oxygen difference were presented, it is unclear if the low O2-pulse was solely due to low SV [37]. Additionally to a low SV, a reduced maximum heart rate could impact the calculation of O2-pulse. These studies argue against SV-related long-term cardiac sequelae. Nonetheless, high-quality studies collecting data > 1 year post-infection using cardiac MRI or echocardiography may be valuable.
Importantly, not only SV but also maximum heart rate needs to be considered as a potential limitation of \(\dot{V}\)O2peak. At least mild chronotropic incompetence was present in ten studies (one study with two measurement points) with follow-ups exceeding 4 months [4, 6, 16, 32, 33, 36, 38, 39, 55, 58]. While chronotropic incompetence could directly impact O2 supply to the muscle, it is also an independent predictor of major cardiovascular events and mortality [60]. Interestingly, chronotropic incompetence is also associated with low \(\dot{V}\)O2peak in patients with chronic fatigue syndrome [62]. These findings might thus have implications for patients post-COVID-19.
The \(\dot{V}\)O2/work rate slope is often abnormal in patients with cardiovascular diseases, thus reflecting limitations in the supply and/or metabolism of oxygen [27, 63]. Five studies reported \(\dot{V}\)O2/work rate slope [6, 32, 34, 44, 64]. Considering 10–11 mL min−1 W−1 as normal [63], results were inconsistent. In one study, \(\dot{V}\)O2/work rate slope was markedly reduced 3 months post-discharge (5.6 mL min−1 W−1, moderate and severe COVID-19) [44]. In the other studies, this parameter was only slightly below normal or normal (9.3, 9.9, 11.8 and 9.7 mL min−1 W−1 at 3 months to 9 months post-discharge) [6, 32, 34, 43]. Although most studies reported a \(\dot{V}\)O2/work rate slope that was slightly below the lower limit of the normal range, it was abnormal at least in a fraction of patients. This supports the findings of the above-presented parameters suggesting a potential contribution of cardiovascular factors to low \(\dot{V}\)O2peak. Again, the reader should be aware that \(\dot{V}\)O2/work rate slope may also be impacted by peripheral factors (discussed in Sect. 3.4) [27, 63].
VT1 is the point of exercise \(\dot{V}\)O2 at which the contribution of anaerobic pathways to energy production increases and, in turn, metabolic acidosis leads to a greater breathing stimulus [65]. VT1 is characterised by a change of slope of \(\dot{V}\)CO2 in relation to \(\dot{V}\)O2 or the inflection point of the \(\dot{V}\)E/\(\dot{V}\)O2 curve in relation to work rate [16]. It provides an indication of O2 supply limitations in the form of cardiac output, anaemia, pulmonary-vascular or peripheral-vascular factors, or a combination of those [65]. However, VT1 is not specific for deconditioning (see also Sect. 3.4) [65]. Eighteen studies presented data on VT1 reported as percentage of \(\dot{V}\)O2peak or percentage of predicted \(\dot{V}\)O2peak [4,5,6, 14,15,16,17, 29, 32,33,34, 37,38,39, 42, 54, 55, 66]. It needs to be emphasised that the unit reported has important implications for the interpretation of results. In a patient with a low \(\dot{V}\)O2peak, VT1 as percentage of \(\dot{V}\)O2peak may be normal but VT1 as percentage of predicted \(\dot{V}\)O2peak is reduced simply because of the lower measured \(\dot{V}\)O2peak. Alternatively, a reduced VT1 as percentage of \(\dot{V}\)O2peak would always be accompanied by a reduced VT1 as percentage of predicted \(\dot{V}\)O2peak independent of the level of \(\dot{V}\)O2peak. Most studies reported normal VT1 that was on average above 40% of \(\dot{V}\)O2peak. This also seemed to be the case for studies that reported VT1 as percentage of predicted \(\dot{V}\)O2peak considering their actual \(\dot{V}\)O2peak [4, 14,15,16, 29, 34, 38]. Yet, several studies reported abnormally low VT1 in 15–42% of patients up to 3 months post-infection [5, 32, 42] and in 19% and 20% of patients at 6 months post-discharge [37, 66]. This is again in line with the cardiovascular parameters discussed earlier, pointing towards a limitation in this organ system in a fraction of patients. The underlying mechanisms for these potential changes in cardiovascular parameters are still unclear. The harmful consequences of physical inactivity and especially bed rest during hospitalisation are extensively described in the literature [19, 20]. Cardiac performance reflected by SV and cardiac output has been shown to decline while heart rate increased, with the recovery of these parameters being delayed following bed rest [19]. Lower plasma volume, impaired vascular regulation, and cardiac atrophy may be responsible for these changes [19, 67]. Medications administered during the hospital stay such as steroidal treatment might lead to myopathic changes [23, 24]. Keeping the delayed recovery of cardiac output in mind, it seems suggestive that low \(\dot{V}\)O2peak, particularly in the first months post-infection, may at least partly be explained by deconditioning and treatment-related aspects affecting the cardiovascular system. The fact that at 4 months post-infection the SV is commonly reported to be close to normal (see Table 3) strongly suggests that the effect of deconditioning on \(\dot{V}\)O2peak via reduced SV diminishes within a rather short time frame of 4 months. Because low \(\dot{V}\)O2peak is prevalent up to 1 year post-infection, deconditioning alone is unlikely to be the only reason for low \(\dot{V}\)O2peak after COVID-19. Nonetheless, it should be noted that deconditioning may also have peripheral manifestations [68].
Endothelial involvement caused by COVID-19-induced chronic inflammation could be another potential cause for the persisting limited cardiovascular function [21]. A recent review described the development of chronic inflammation months after acute COVID-19 infection that accompanies prolonged symptoms [21]. High levels of systemic inflammation, in turn, create a high risk for multi-organ damage [69, 70], potentially mediated by endothelial damage [71, 72]. It has been hypothesised that acute endothelialitis in the pulmonary circulation could extend into the systemic circulation, leading to myocardial injury as well as impaired function [72]. This impaired function might become apparent during CPET by reduced SV and/or chronotropic incompetence. Because none of the previous studies included an adequate measure of vascular function, such as flow-mediated dilation [73], this cannot be answered yet and warrants further investigation.
In conclusion, the contribution of the cardiovascular system to low \(\dot{V}\)O2peak is unclear and the results are inconsistent. It seems that within the first few months post-infection a limited cardiac function contributes to low \(\dot{V}\)O2peak in a considerable fraction of patients. In other patients, it appears that the main limitation lies in the periphery.
3.4 Periphery/Musculature and Mitochondria (Gear 3)
Peripheral limitations are indicated by an abnormal response in respiratory exchange ratio, abnormal \(\dot{V}\)CO2 kinetics throughout exercise, a shallower increase of \(\dot{V}\)O2/work rate ratio, or reduced VT1 during CPET (panels 3, 5, 8 in the original Wasserman 9-panel graph) [27].
As discussed earlier on, \(\dot{V}\)O2/work rate ratio was abnormal at 3 months post-infection [44] and only slightly reduced or normal between 3 and 9 months post-infection (see Sect. 3.3) [6, 32, 34, 43]. VT1 was, on average, normal in most studies. However, as mentioned in Sect. 3.3, abnormal VT1 was documented in a fraction of patients up to 6 months post-infection [5, 32, 37, 42, 66]. Abnormal \(\dot{V}\)O2/work rate ratio and VT1 suggest a possible contribution of peripheral factors (i.e. peripheral-vascular or mitochondrial components) to low \(\dot{V}\)O2peak in some patients. \(\dot{V}\)O2/work rate ratio and VT1, however, seem too unspecific to quantify the contribution of peripheral factors to low \(\dot{V}\)O2peak. It is also not possible to attribute abnormalities in these parameters to deconditioning or inflammation-induced changes that have distinct aetiologies, for example. However, several studies infer deconditioning due to abnormalities in \(\dot{V}\)O2/work rate ratio and VT1 [5, 31, 32]. Also, in some studies definitions for deconditioning seem to differ. Skjørten et al. [5] define deconditioning as the absence of ventilatory and cardiac exercise limitations, whereas in Rinaldo et al. [32] the definition also seems to include virus-induced alterations in muscle tissue. Consistent definitions thus need to be used in the future to obtain a better understanding of the underlying factors of low \(\dot{V}\)O2peak.
In the absence of O2 supply limitations, arteriovenous oxygen difference (a-vO2-diff) reflects the metabolic oxidative capacity, which is the ability of the mitochondria to utilise oxygen [9]. Measuring a-vO2-diff directly is complex [74] and thus is usually calculated using Fick’s equation, which was done in two of the three studies included in this review (both used stress echocardiography to determine cardiac output) [4, 24]. Because determining a-vO2-diff from solving Fick’s equation has severe limitations, such as errors introduced by indirect estimates of SV or the lag in \(\dot{V}\)O2 during incremental exercise [65], the results of these studies need to be interpreted with restraint. One study measured this outcome directly in patients with preserved cardiac output and in controls at 1 year post-infection. Patients showed a lower a-vO2-diff and peripheral oxygen extraction at peak exercise as compared with age- and sex-matched controls with exercise intolerance unrelated to COVID-19 [58]. These results indicate that peripheral alterations may contribute to low \(\dot{V}\)O2peak even 1 year after discharge. In addition, Clavario et al. [29] evaluated maximal muscular strength using the dominant leg extension exercise. Based on the finding of muscular strength being independently associated with \(\dot{V}\)O2peak, the authors concluded that muscle impairment might be responsible for most of the functional diminishing [29]. However, as mentioned before, COVID-19-induced inflammation might also contribute to muscle loss [21]. Thus, it is questionable that the author’s data support the conclusion that deconditioning is the sole explanation for functional diminishing. Piotrowicz et al. [22] recently discussed the pathophysiology of post-COVID-19 acute sarcopenia. In their work, it becomes apparent that the structural and functional changes associated with sarcopenia also impact \(\dot{V}\)O2peak [22]. This is in line with the proposed mechanisms by Singh et al. [58], likewise suggesting systemic microvascular dysfunction and a skeletal muscle myopathic process (i.e. sarcopenia) to be involved. To differentiate between inactivity- and COVID-19-related causes of muscle loss, biomarkers of inflammation and protein degradation may be helpful [75]. Muscle loss as a consequence of inactivity is commonly not accompanied by increased inflammation or muscle protein degradation as opposed to disease-induced changes [75]. For more details, the reader is referred to the review by Evans [75].
Based on the body of evidence, it is probable that both COVID-19-induced and inactivity-induced changes may lead to increased mitochondrial dysfunction, myofibrillar breakdown, reduced mitochondrial biogenesis as well as muscle synthesis and ultimately foster low \(\dot{V}\)O2peak [22]. Given the parallels between patients with chronic fatigue syndrome and those with post-COVID-19, evidence on mitochondrial involvement in the former group of patients [76, 77] might be valuable. Although it is unlikely the primary cause of disease, mitochondrial dysfunction via immune-inflammatory and oxidative pathways is documented in chronic fatigue syndrome and closely related to exercise intolerance [76, 77]. These data may therefore support the conclusions regarding a peripheral contribution to low \(\dot{V}\)O2peak in post-COVID-19. The effects of inactivity/bed rest on skeletal musculature are described elsewhere [68]. Considering that several studies suggested an underlying peripheral limitation, it seems to be important to bear these possible mechanisms of action in mind for further research as well as rehabilitation. Nonetheless, the extent of peripheral involvement in respect to the time post-infection, exact mechanisms and factors predisposing peripheral involvement are yet to be determined.
3.5 Limitations
This review has some limitations. Raman et al. [78] highlighted that the heterogeneity in patient selection and factors such as virus variants, vaccines and choice of controls might have added to the variability in reported prevalence estimates. Indeed, infection with newly emerging SARS-CoV-2 variants such as Omicron might cause different post-COVID-19 sequelae and possibly a differential influence on \(\dot{V}\)O2peak [79]. Also, within some of the studies included in this review, there was a wide heterogeneity in regard to the severity of COVID-19 in patients. Thus, the data shown in Fig. 2 could have led to an overestimation of the levels of \(\dot{V}\)O2peak in severe COVID-19 and an underestimation in mild COVID-19 severity. COVID-19 vaccination status of patients might also affect \(\dot{V}\)O2peak. We previously demonstrated that physical activity, an important moderator of \(\dot{V}\)O2peak, differed between unvaccinated and fully vaccinated adults [80]. Finally, different methods to determine \(\dot{V}\)E/\(\dot{V}\)CO2 are available [56, 81]. However, the exact methods used were often not reported. Thus, we pooled \(\dot{V}\)E/\(\dot{V}\)CO2 data in Fig. 2C irrespective of the method used. This may have led to imprecision [81] but we believe this figure still provides a valuable overview of the data. The reader should be aware of these aspects.
Furthermore, there are limitations of the individual studies per se that need to be considered when interpreting the results. Firstly, the time at which the examinations were conducted was usually provided as either time since infection or since hospital discharge. This could have led to imprecision in our attempt to categorise studies into short, moderate, or long term as infection and hospital discharge may be separated by weeks or months. Secondly, all studies used an observational research design without pre-infection data. This makes it difficult to disentangle the contributions of pre-existing chronic conditions before the COVID-19 infection and lifestyle factors to low \(\dot{V}\)O2peak. Thirdly, as recently shown, individuals with low \(\dot{V}\)O2peak seem to be more prone to greater COVID-19 severity than those with high \(\dot{V}\)O2peak [7]. Simultaneously, the data from this review suggested a detrimental effect of COVID-19 on \(\dot{V}\)O2peak. Based on the available data, both are likely true, but it is unclear to which extent each factor contributes to low \(\dot{V}\)O2peak. Fourthly, most studies used normative data or historical controls for comparisons with cases. This introduces bias since the comparison was not subject to the potential influence of COVID-19 pandemic-related restrictions and their substantial impact on physical activity [82], a key determinant of \(\dot{V}\)O2peak [19, 20]. Fifthly, the source of reference values remains unknown in nearly all studies, making it impossible for the reader to evaluate the generalisability of the results and compare the data across studies. Regarding \(\dot{V}\)O2peak, considerable differences between reference values have been shown recently [83]. Sixthly, most studies included hospitalised patients and/or those with persistent symptoms, limiting the generalisability to hospitalised patients with moderate to critical COVID-19. Seventhly, many studies focused exclusively on single gears, making it difficult to draw conclusions about potentially limiting factors on \(\dot{V}\)O2peak. Studies incorporating all parts of the gear system are thus needed to better understand the interplay of the three gears on low \(\dot{V}\)O2peak. To conclude, it is understandable that at an early stage of a pandemic, available clinical data are used to provide insights into potential sequelae quickly. However, to date, high-quality studies are missing.
4 Conclusion
In patients post-COVID-19, as in healthy subjects, respiratory function seems to contribute in only a minor way to low \(\dot{V}\)O2peak. However, traditional spirometry parameters are measured at rest and may thus not reflect lung function during exercise. In contrast, the prevalence of low lung diffusion capacity, measured by DLCO, is markedly high in patients post-COVID-19, which might contribute to low \(\dot{V}\)O2peak [49]. Future studies need to examine lung function during maximum performance and should include the combined measurement of DLNO-DLCO.
The cardiovascular system might contribute to low \(\dot{V}\)O2peak via subnormal cardiac output due to chronotropic incompetence and lower SV, especially in the first months post-infection. At least mild chronotropic incompetence was similarly present at moderate- and long-term follow-up. Nonetheless, contrary findings exist. Larger cohort studies applying adequate methods to measure SV and consequently CO such as Doppler echocardiography or pulse contour devices are needed [84].
The fact that studies using CPET report the absence of major pulmonary or cardiac limitations suggests that the periphery, including the vasculature as well as musculature, might be central to impaired \(\dot{V}\)O2peak. To confirm this hypothesis, future studies using CPET need to determine muscle mass, muscle strength, muscle perfusion, mitochondrial function as well as a-vO2 diff.
The evidence presented in this review strongly suggests that it is not justified to declare deconditioning as the sole mechanism of low \(\dot{V}\)O2peak as most studies have done (see Tables 1, 2 and 3). While deconditioning certainly explains part of the reductions, there are most likely other factors involved. A combination of COVID-19-induced and inactivity-induced processes might be responsible for the alterations in cardiac, vascular and muscular but also pulmonary function [21, 71, 72]. In addition, psychological factors may contribute substantially to the prolonged symptoms fostering exercise intolerance [85]. Schaeffer et al. [86], for instance, found lower \(\dot{V}\)O2peak in patients with post-COVID-19 fatigue than in those without fatigue. This was accompanied by greater dyspnoea during exercise [86]. Psychological factors should thus not be disregarded in research, diagnosis or therapy/treatment.
The short- and long-term sequelae of COVID-19 are multifaceted and require diagnosis and treatment specific to the individual. This aligns well with recently proposed subtypes of post-COVID-19 syndrome that differ in terms of systematic manifestations as well as pathophysiological mechanisms [87]. Thorough testing with particular focus given to all three gear systems is required to receive a comprehensive understanding of the underlying causes of low \(\dot{V}\)O2peak post-COVID-19. Such understanding would facilitate decision making in terms of diagnosis and treatment decisions. Thus, CPET is of paramount importance.
References
Gebhard CE, Sütsch C, Bengs S, Deforth M, Buehler KP, Hamouda N, et al. Sex- and gender-specific risk factors of post-COVID-19 Syndrome: a population-based cohort study in Switzerland. medRxiv. 2021:2021.06.30.21259757.
Kuodi P, Gorelik Y, Zayyad H, Wertheim O, Wiegler KB, Jabal KA, et al. Association between vaccination status and reported incidence of post-acute COVID-19 symptoms in Israel: a cross-sectional study of patients infected between March 2020 and November 2021. medRxiv. 2022:2022.01.05.22268800.
Korpelainen R, Lamsa J, Kaikkonen KM, Korpelainen J, Laukkanen J, Palatsi I, et al. Exercise capacity and mortality—a follow-up study of 3033 subjects referred to clinical exercise testing. Ann Med. 2016;48(5):359–66.
Szekely Y, Lichter Y, Sadon S, Lupu L, Taieb P, Banai A, et al. Cardiorespiratory abnormalities in patients recovering from coronavirus disease 2019. J Am Soc Echocardiogr. 2021;2021.
Skjørten I, Ankerstjerne OAW, Trebinjac D, Brønstad E, Rasch-Halvorsen Ø, Einvik G, et al. Cardiopulmonary exercise capacity and limitations 3 months after COVID-19 hospitalisation. Eur Respir J. 2021;58(2):2100996.
Mancini DM, Brunjes DL, Lala A, Trivieri MG, Contreras JP, Natelson BH. Use of cardiopulmonary stress testing for patients with unexplained dyspnea post-coronavirus disease. JACC Heart Fail. 2021;9(12):927–37.
Brawner CA, Ehrman JK, Bole S, Kerrigan DJ, Parikh SS, Lewis BK, et al. Inverse relationship of maximal exercise capacity to hospitalization secondary to coronavirus disease 2019. Mayo Clin Proc. 2021;96(1):32–9.
Wagner PD. New ideas on limitations to VO2max. Exerc Sport Sci Rev. 2000;28(1):10–4.
Wasserman K. The Dickinson W. Richards lecture. New concepts in assessing cardiovascular function. Circulation. 1988;78(4):1060–71.
Groff D, Sun A, Ssentongo AE, Ba DM, Parsons N, Poudel GR, et al. Short-term and long-term rates of postacute sequelae of SARS-CoV-2 infection: a systematic review. JAMA Netw Open. 2021;4(10):e2128568-e.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210.
World Health Organization. Clinical management of COVID-19: interim guidance, 27 May 2020. Geneva: World Health Organization; 2020. https://apps.who.int/iris/handle/10665/332196. Accessed 28 July 2022.
Csulak E, Petrov A, Kovats T, Tokodi M, Lakatos B, Kovacs A, et al. The impact of COVID-19 on the preparation for the Tokyo Olympics: a comprehensive performance assessment of top swimmers. Int J Environ Res Public Health. 2021;18(18):16.
Anastasio F, Rossi G, D'Abbondanza M, Curcio R, Vaudo G, et al. Mid-term impact of mild-moderate COVID-19 on cardiorespiratory fitness in elite athletes. J Sports Med Phys Fit. 2021. https://doi.org/10.23736/S0022-4707.21.13226-8.
Cavigli L, Frascaro F, Turchini F, Mochi N, Sarto P, Bianchi S, et al. A prospective study on the consequences of SARS-CoV-2 infection on the heart of young adult competitive athletes: implications for a safe return-to-play. Int J Cardiol. 2021;336:130–6.
Joris M, Minguet P, Colson C, Joris J, Fadeur M, Minguet G, et al. Cardiopulmonary exercise testing in critically ill coronavirus disease 2019 survivors: evidence of a sustained exercise intolerance and hypermetabolism. Crit Care Explor. 2021;3(7): e0491.
Cassar MP, Tunnicliffe EM, Petousi N, Lewandowski AJ, Xie C, Mahmod M, et al. Symptom persistence despite improvement in cardiopulmonary health—insights from longitudinal CMR, CPET and lung function testing post-COVID-19. EClinicalMedicine. 2021;20: 101159.
Everaerts S, Heyns A, Langer D, Beyens H, Hermans G, Troosters T, et al. COVID-19 recovery: benefits of multidisciplinary respiratory rehabilitation. BMJ Open Respir Res. 2021;8(1):09.
Spaak J, Montmerle S, Sundblad P, Linnarsson D. Long-term bed rest-induced reductions in stroke volume during rest and exercise: cardiac dysfunction vs. volume depletion. J Appl Physiol. 2005;98(2):648–54.
Mitchell JH, Levine BD, McGuire DK. The Dallas bed rest and training study. Circulation. 2019;140(16):1293–5.
Hirschenberger M, Hunszinger V, Sparrer KM. Implications of innate immunity in post-acute sequelae of non-persistent viral infections. Cells. 2021;10(8):2134.
Piotrowicz K, Gąsowski J, Michel JP, Veronese N. Post-COVID-19 acute sarcopenia: physiopathology and management. Aging Clin Exp Res. 2021;33(10):2887–98.
Chen F, Hao L, Zhu S, Yang X, Shi W, Zheng K, et al. Potential adverse effects of dexamethasone therapy on COVID-19 patients: review and recommendations. Inf Dis Ther. 2021;10(4):1907–31.
Baratto C, Caravita S, Faini A, Perego GB, Senni M, Badano LP, et al. Impact of COVID-19 on exercise pathophysiology: a combined cardiopulmonary and echocardiographic exercise study. J Appl Physiol. 2021;130(5):1470–8.
Casaburi R, Rennard SI. Exercise limitation in chronic obstructive pulmonary disease. The O’Donnell threshold. Am J Respir Crit Care Med. 2015;191(8):873–5.
Schwarz S, Lehnigk B, Schwittai W. Lungenfunktionsdiagnostik und Spiroergometrie. 2nd ed. Stuttgart: Georg Thieme Verlag KG; 2022.
Wasserman K. Diagnosing cardiovascular and lung pathophysiology from exercise gas exchange. Chest. 1997;112(4):1091–101.
Long Q, Li J, Hu X, Bai Y, Zheng Y, Gao Z. Follow-ups on persistent symptoms and pulmonary function among post-acute COVID-19 patients: a systematic review and meta-analysis. Front Med. 2021;8: 702635.
Clavario P, De Marzo V, Lotti R, Barbara C, Porcile A, Russo C, et al. Cardiopulmonary exercise testing in COVID-19 patients at 3 months follow-up. Int J Cardiol. 2021;340:113–8.
Johnsen S, Sattler SM, Miskowiak KW, Kunalan K, Victor A, Pedersen L, et al. Descriptive analysis of long COVID sequelae identified in a multidisciplinary clinic serving hospitalised and non-hospitalised patients. ERJ Open Res. 2021;7(3):00205–2021.
Jahn K, Sava M, Sommer G, Schumann DM, Bassetti S, Siegemund M, et al. Exercise capacity impairment after COVID-19 pneumonia is mainly caused by deconditioning. Eur Respir J. 2022;59(1):2101136.
Rinaldo RF, Mondoni M, Maria Parazzini E, Pitari F, Brambilla E, Luraschi S, et al. Deconditioning as main mechanism of impaired exercise response in COVID-19 survivors. Eur Respir J. 2021;58(2):2100870.
Mohr A, Dannerbeck L, Lange TJ, Pfeifer M, Blaas S, Salzberger B, et al. Cardiopulmonary exercise pattern in patients with persistent dyspnoea after recovery from COVID-19. Multidiscip Respir Med. 2021;16(1):732.
Dorelli G, Braggio M, Gabbiani D, Busti F, Caminati M, Senna G, et al. Importance of cardiopulmonary exercise testing amongst subjects recovering from COVID-19. Diagnostics. 2021;11(3):507.
Vannini L, Quijada-Fumero A, Martín MPR, Pina NC, Afonso JSH. Cardiopulmonary exercise test with stress echocardiography in COVID-19 survivors at 6 months follow-up. Eur J Intern Med. 2021;94:101–4.
Debeaumont D, Boujibar F, Ferrand-Devouge E, Artaud-Macari E, Tamion F, Gravier F-E, et al. Cardiopulmonary exercise testing to assess persistent symptoms at 6 months in people with COVID-19 who survived hospitalization: a pilot study. Phys Ther. 2021;101(6):pzab099.
Xiao K, Yang H, Liu B, Pang X, Du J, Liu M, et al. Antibodies can last for more than 1 year after SARS-CoV-2 infection: a follow-up study from survivors of COVID-19. Front Med. 2021;8: 684864.
Aparisi Á, Ybarra-Falcón C, García-Gómez M, Tobar J, Iglesias-Echeverría C, Jaurrieta-Largo S, et al. Exercise ventilatory inefficiency in post-COVID-19 syndrome: insights from a prospective evaluation. J Clin Med. 2021;10(12):2591.
Alba GA, Ziehr DR, Rouvina JN, Hariri LP, Knipe RS, Medoff BD, et al. Exercise performance in patients with post-acute sequelae of SARS-CoV-2 infection compared to patients with unexplained dyspnea. EClinicalMedicine. 2021;39: 101066.
Blokland IJ, Ilbrink S, Houdijk H, Dijkstra JW, van Bennekom CAM, Fickert R, et al. Exercise capacity after mechanical ventilation because of COVID-19: Cardiopulmonary exercise tests in clinical rehabilitation. Ned Tijdschr Geneeskd. 2020;164:D5253.
Kersten J, Baumhardt M, Hartveg P, Hoyo L, Hull E, Imhof A, et al. Long COVID: distinction between organ damage and deconditioning. J Clin Med. 2021;10(17):24.
Raman B, Cassar MP, Tunnicliffe EM, Filippini N, Griffanti L, Alfaro-Almagro F, et al. Medium-term effects of SARS-CoV-2 infection on multiple vital organs, exercise capacity, cognition, quality of life and mental health, post-hospital discharge. EClinicalMedicine. 2021;31: 100683.
Motiejunaite J, Balagny P, Arnoult F, Mangin L, Bancal C, Vidal-Petiot E, et al. Hyperventilation as one of the mechanisms of persistent dyspnoea in SARS-CoV-2 survivors. Eur Respir J. 2021;58(2):2101578.
Acar RD, Sarıbaş E, Güney PA, Kafkas Ç, Aydınlı D, Taşçı E, et al. COVID-19: the new cause of dyspnoea as a result of reduced lung and peripheral muscle performance. J Breath Res. 2021. https://doi.org/10.1088/1752-7163/ac22bb.
Petersen EL, Goßling A, Adam G, Aepfelbacher M, Behrendt C-A, Cavus E, et al. Multi-organ assessment in mainly non-hospitalized individuals after SARS-CoV-2 infection: the Hamburg City Health Study COVID programme. Eur Heart J. 2022;43(11):1124–37.
Hidaka T, Utsunomiya H, Mitsuba N, Ishibashi K, Kitagawa T, Dohi Y, et al. Abnormal airway resistance and reactance limit exercise capacity in patients with chronic heart failure. J Card Fail. 2013;19(10):S115.
Barisione G, Brusasco V. Lung diffusing capacity for nitric oxide and carbon monoxide following mild-to-severe COVID-19. Physiol Rep. 2021;9(4): e14748.
Guo T, Jiang F, Liu Y, Zhao Y, Li Y, Wang Y. Respiratory outcomes in patients following COVID-19-related hospitalization: a meta-analysis. Front Mol Biosci. 2021;8: 750558.
Zavorsky GS, Smoliga JM. The association between cardiorespiratory fitness and pulmonary diffusing capacity. Respir Physiol Neurobiol. 2017;241:28–35.
Nusair S. Abnormal carbon monoxide diffusion capacity in COVID-19 patients at time of hospital discharge. Eur Respir J. 2020;56(1):2001832.
Chen R, Gao Y, Chen M, Jian W, Lei C, Zheng J, et al. Impaired pulmonary function in discharged patients with COVID-19: more work ahead. Eur Respir J. 2020;56(1):2002194.
Laveneziana P, Straus C, Meiners S. How and to what extent immunological responses to SARS-CoV-2 shape pulmonary function in COVID-19 patients. Front Physiol. 2021;12: 628288.
Grist JT, Collier GJ, Walters H, Kim M, Chen M, Eid GA, et al. Lung abnormalities depicted with hyperpolarized xenon MRI in patients with long COVID. Radiology. 2022:220069.
Gao Y, Chen R, Geng Q, Mo X, Zhan C, Jian W, et al. Cardiopulmonary exercise testing might be helpful for interpretation of impaired pulmonary function in recovered COVID-19 patients. Eur Respir J. 2021;57(1):2004265.
Vonbank K, Lehmann A, Bernitzky D, Gysan MR, Simon S, Schrott A, et al. Predictors of prolonged cardiopulmonary exercise impairment after COVID-19 infection: a prospective observational study. Front Med. 2021;8: 773788.
Weatherald J, Philipenko B, Montani D, Laveneziana P. Ventilatory efficiency in pulmonary vascular diseases. Eur Respir Rev. 2021;30(161): 200214.
Neder JA, Berton DC, Marillier M, Bernard A-C, O’Donnell DE. Inspiratory constraints and ventilatory inefficiency are superior to breathing reserve in the assessment of exertional dyspnea in COPD. COPD: J Chron Obstruct Pulmon Dis. 2019;16(2):174–81.
Singh I, Joseph P, Heerdt PM, Cullinan M, Lutchmansingh DD, Gulati M, et al. Persistent exertional intolerance after COVID-19: insights from invasive cardiopulmonary exercise testing. Chest. 2021;161(1):54–63.
Accalai E, Vignati C, Salvioni E, Pezzuto B, Contini M, Cadeddu C, et al. Non-invasive estimation of stroke volume during exercise from oxygen in heart failure patients. Eur J Prev Cardiol. 2020;28(3):280–6.
Brubaker PH, Kitzman DW. Chronotropic Incompetence. Circulation. 2011;123(9):1010–20.
Caravita S, Baratto C, Di Marco F, Calabrese A, Balestrieri G, Russo F, et al. Haemodynamic characteristics of COVID-19 patients with acute respiratory distress syndrome requiring mechanical ventilation. An invasive assessment using right heart catheterization. Eur J Heart Fail. 2020;22(12):2228–37.
Davenport TE, Lehnen M, Stevens SR, VanNess JM, Stevens J, Snell CR. Chronotropic intolerance: an overlooked determinant of symptoms and activity limitation in myalgic encephalomyelitis/chronic fatigue syndrome? Front Pediatr. 2019;7:82.
Statement on cardiopulmonary exercise testing in chronic heart failure due to left ventricular dysfunction: recommendations for performance and interpretation Part I: Definition of cardiopulmonary exercise testing parameters for appropriate use in chronic heart failure. Eur J Cardiovasc Prev Rehabil. 2006;13(2):150–64.
Motiejunaite J, Balagny P, Arnoult F, Mangin L, Bancal C, d’Ortho MP, et al. Hyperventilation: a possible explanation for long-lasting exercise intolerance in mild COVID-19 survivors? Front Physiol. 2020;11: 614590.
Wasserman K. The anaerobic threshold measurement to evaluate exercise performance. Am Rev Respir Dis. 1984;129(2 Pt 2):S35-40.
Liu M, Lv F, Huang Y, Xiao K. Follow-up study of the chest CT characteristics of COVID-19 survivors seven months after recovery. Front Med. 2021;8(212): 636298.
Perhonen MA, Franco F, Lane LD, Buckey JC, Blomqvist CG, Zerwekh JE, et al. Cardiac atrophy after bed rest and spaceflight. J Appl Physiol. 2001;91(2):645–53.
Di Girolamo FG, Fiotti N, Milanović Z, Situlin R, Mearelli F, Vinci P, et al. The aging muscle in experimental bed rest: a systematic review and meta-analysis. Front Nutr. 2021;8: 633987.
Azkur AK, Akdis M, Azkur D, Sokolowska M, van de Veen W, Brüggen MC, et al. Immune response to SARS-CoV-2 and mechanisms of immunopathological changes in COVID-19. Allergy. 2020;75(7):1564–81.
Hu B, Huang S, Yin L. The cytokine storm and COVID-19. J Med Virol. 2021;93(1):250–6.
Goshua G, Pine AB, Meizlish ML, Chang CH, Zhang H, Bahel P, et al. Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study. Lancet Haematol. 2020;7(8):e575–82.
Vrints CJM, Krychtiuk KA, Van Craenenbroeck EM, Segers VF, Price S, Heidbuchel H. Endothelialitis plays a central role in the pathophysiology of severe COVID-19 and its cardiovascular complications. Acta Cardiol. 2021;76(2):109–24.
Königstein K, Wagner J, Frei M, Knaier R, Klenk C, Carrard J, et al. Endothelial function of healthy adults from 20 to 91 years of age: prediction of cardiovascular risk by vasoactive range. J Hypertens. 2021;39(7):1361–9.
Kiel JW, Shepherd AP. Continuous measurement of arteriovenous oxygen difference and VO2 by microcomputer. Am J Physiol. 1983;245(1):H178–82.
Evans WJ. Skeletal muscle loss: cachexia, sarcopenia, and inactivity. Am J Clin Nutr. 2010;91(4):1123S-S1127.
Morris G, Maes M. Mitochondrial dysfunctions in myalgic encephalomyelitis/chronic fatigue syndrome explained by activated immuno-inflammatory, oxidative and nitrosative stress pathways. Metab Brain Dis. 2014;29(1):19–36.
Holden S, Maksoud R, Eaton-Fitch N, Cabanas H, Staines D, Marshall-Gradisnik S. A systematic review of mitochondrial abnormalities in myalgic encephalomyelitis/chronic fatigue syndrome/systemic exertion intolerance disease. J Transl Med. 2020;18(1):290.
Raman B, Bluemke DA, Lüscher TF, Neubauer S. Long COVID: post-acute sequelae of COVID-19 with a cardiovascular focus. Eur Heart J. 2022;43(11):1157–72.
Peralta Santos A, Pinto Leite P, Casaca P, Fernandes E, Freire Rodrigues E, Moreno J, et al. Omicron (BA.1) SARS-CoV-2 variant is associated with reduced risk of hospitalization and length of stay compared with Delta (B.1.617.2). medRxiv. 2022:2022.01.20.22269406.
Schwendinger F, Boeck HT, Infanger D, Faulhaber M, Tegtbur U, Schmidt-Trucksäss A. COVID-19 vaccination status is associated with physical activity in German-speaking countries: the COR-PHYS-Q cohort study. medRxiv. 2022:2022.01.01.21268576.
Lamotte M, Chaumont M, Forton K, Gillet A, Strapart J. Influence of the method of calculating the Ve / VCO2 slope on its value in a cohort of 700 successive Cardiopulmonary exercise testing. Eur J Prev Cardiol 2022;29(Issue Supplement_1):zwac056.013.
Stockwell S, Trott M, Tully M, Shin J, Barnett Y, Butler L, et al. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ Open Sport Exerc Med. 2021;7(1): e000960.
Wagner J, Knaier R, Infanger D, Königstein K, Klenk C, Carrard J, et al. Novel CPET reference values in healthy adults: associations with physical activity. Med Sci Sports Exerc. 2021;53(1):26–37.
Geerts BF, Aarts LP, Jansen JR. Methods in pharmacology: measurement of cardiac output. Br J Clin Pharmacol. 2011;71(3):316–30.
Dhawan RT, Gopalan D, Howard L, Vicente A, Park M, Manalan K, et al. Beyond the clot: perfusion imaging of the pulmonary vasculature after COVID-19. Lancet Respir Med. 2021;9(1):107–16.
Schaeffer MR, Cowan J, Milne KM, Puyat JH, Voduc N, Corrales-Medina V, et al. Cardiorespiratory physiology, exertional symptoms, and psychological burden in post-COVID-19 fatigue. Respir Physiol Neurobiol. 2022;302: 103898.
Yong SJ, Liu S. Proposed subtypes of post-COVID-19 syndrome (or long-COVID) and their respective potential therapies. Rev Med Virol. 2022;32(4): e2315.
Liu M, Lv F, Zheng Y, Xiao K. A prospective cohort study on radiological and physiological outcomes of recovered COVID-19 patients 6 months after discharge. Quant Imaging Med Surg. 2021;11(9):4181–92.
Acknowledgements
The authors thank Thomas Angst for proofreading the manuscript. We acknowledge the use of graphics provided by SERVIER MEDICAL ART (www.smart.servier.com) and the Centers for Disease Control and Prevention on Unsplash (www.unsplash.com) in Fig. 1.
Funding
Open access funding provided by University of Basel.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Fabian Schwendinger, Raphael Knaier, Thomas Radtke and Arno Schmidt-Trucksäss declare that they have no conflicts of interest relevant to the content of this review.
Funding
No external sources of funding were used to assist in the preparation of this article. RK was funded by the Swiss National Science Foundation (Grant P2BSP3_191755).
Author contributions
FS conceptualised the study, performed the literature search, interpreted the data, and wrote the original draft of the manuscript. RK, TR and AST contributed to data interpretation and revised the manuscript. All authors read and approved the final version of the manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schwendinger, F., Knaier, R., Radtke, T. et al. Low Cardiorespiratory Fitness Post-COVID-19: A Narrative Review. Sports Med 53, 51–74 (2023). https://doi.org/10.1007/s40279-022-01751-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-022-01751-7