Abstract
Estetrol (E4) is the most recently described natural estrogen. It is produced by the human fetal liver during pregnancy and its physiological function remains unclear. E4 is the estrogenic component of a recently approved combined oral contraceptive. It is also in development for use as menopausal hormone therapy. In the context of these developments, the pharmacological activity of E4, alone or in combination with a progestin, has been extensively characterized in preclinical models as well as in clinical studies in women of reproductive age and postmenopausal women. Despite the clinical benefits, the use of oral estrogens for contraception or menopause is also associated with unwanted effects, such as an increased risk of breast cancer and thromboembolic events, due to their impact on non-target tissues. Preclinical and clinical data for E4 point to a tissue-specific activity and a more selective pharmacological profile compared with other estrogens, including a low impact on the liver and hemostasis balance. This review summarizes the characterization of the pharmacological properties of E4 as well as recent advances made in the understanding of the molecular mechanisms of action driving its activity. How the unique mode of action and the different metabolism of E4 might support its favorable benefit–risk ratio is also discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Estetrol presents a more selective pharmacological profile compared with other oral estrogens, suggestive of a better safety profile. |
This includes a low impact on the liver and hemostasis balance. |
1 Introduction
Estetrol (E4) was recently marketed as the estrogenic component of a new combined oral contraceptive (COC) in combination with the progestin drospirenone (DRSP). It is also currently in late stage clinical development for use as a menopausal hormone therapy (MHT). These advancements for E4 in women’s health are the culmination of efforts to characterize the pharmacological activity and safety profile of this natural estrogen. In addition to the primary therapeutic targets, namely the prevention of pregnancy and the alleviation of vasomotor symptoms (VMS), the pharmacological characterization of E4 has been extended to many other tissues and biological responses.
The use of estrogens in the context of contraception and menopause is associated with unwanted effects, including an increased risk of breast cancer and venous thromboembolism (VTE). The role of estrogens and estrogen receptors (ERs) in the breast is well described. Estradiol (E2) physiologically stimulates postnatal mammary gland development [1, 2]. The proliferative rate in normal breast epithelium from women exposed to an estroprogestative combination is significantly higher compared with non-users [3,4,5]. Breast cancer is the most commonly diagnosed cancer [6] and about 70% of breast tumors express ERs. In these cancers, estrogen acts as mitotic agent and growth factor promoting tumor growth. Several epidemiological studies have linked the use of hormonal contraception or MHT to an increased risk of developing breast cancer [7,8,9]. Besides the ER-mediated effects on cell proliferation, the production of highly reactive metabolites has also been described to play a role in estrogen-induced carcinogenesis. The oxidative metabolism of estrogen leads to the formation of catechol and quinone species that can react with the DNA to create adducts that can give rise to mutations and therefore contribute to the development of tumors [10, 11]. This mechanism of breast carcinogenesis is independent of ER. Accumulation of estrogen-DNA adducts was detected in human breast cancer cells [12] and in human samples (breast tumor tissue, urine and serum) [13,14,15,16].
The liver plays a critical role in hemostasis as it is the primary source of the majority of coagulation factors, anticoagulant proteins and constituents of the fibrinolytic system [17]. The VTE risk in hormonal contraception users is a rare but serious adverse effect [18, 19] that is due to the strong impact of estrogens on the liver, and in particular on the synthesis of hepatic coagulation factors triggering a shift towards a prothrombotic state [19]. The estrogen dosage, the nature of the estrogenic and progestogenic components in combined contraceptives, as well as the route of administration are some of the parameters that can influence the risk of VTE associated with hormonal contraception [20,21,22].
Based on the adverse effects reported for other estrogens, special attention was given to deciphering the impact of E4 on the breast and the liver with a particular focus on hemostasis parameters. Preclinical and clinical data suggest that E4 has a more selective pharmacological profile compared with other estrogens. E4 confers adequate estrogenic effects in uterovaginal tissues and bone as well as on cardiovascular and central nervous systems, while it has an overall limited impact on hepatic parameters, including on the hemostasis balance. In addition, data obtained in preclinical models suggest that E4 may have a differential impact on breast proliferation and carcinogenesis compared with other estrogens. From a molecular perspective, the interaction of E4 with the ERs has been extensively characterized.
The focus of the current review is to provide an overview of the work that led to the characterization of the pharmacological properties of E4 as well as an insight into the recent advances made in the understanding of the molecular mechanisms of action driving its tissue-selective activity and ultimately underlying its favorable benefit–risk ratio.
2 Estetrol (E4)
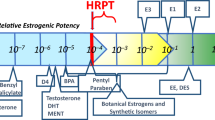
E4 was first discovered and identified by Egon Diczfalusy at the Karolinska Institute in Stockholm in 1965 [23]. E4 belongs to the family of natural estrogens with estrone (E1), estradiol (E2) and estriol (E3). Structurally, E4 has four hydroxyl groups (Fig. 1). E4 is produced by the human fetal liver during pregnancy and reaches the maternal circulation as indicated by increasing E4 concentrations in maternal plasma and urine throughout pregnancy. Different studies have shown a consistent steady rise of E4 in maternal plasma during pregnancy to levels up to 1.2 ng/mL at term. Fetal E4 levels are reported to be over 10 times higher than maternal levels [24, 25]. To date, the physiological function of E4 during pregnancy remains unclear. However, the physiological exposure to relatively high concentrations of E4 during pregnancy suggests a good tolerability of the compound.
After its discovery, preclinical research studies were conducted with E4. The first experimental data described E4 as a weak estrogen compared with the reference estrogen E2, showing a moderate affinity for the ERs [26, 27]. It was also shown that E4 was able to induce a number of biological changes in the rat uterus, revealing its estrogenic activity [28, 29].
The potential use of E4 as an indicator of fetal well-being was investigated in various studies, but due to the large intra- and interindividual variation of maternal E4 levels, this appeared not to be feasible [24, 30, 31], and further research into E4 was subsequently abandoned. In the 2000s, scientific interest in E4 was rekindled with the goal of exploring its potential therapeutic use in women’s health.
In terms of pharmacokinetic properties, E4 has a high oral bioavailability and a long half-life in humans, in contrast to other natural estrogens such as E2 [32]. Metabolism also highly differentiates E4 from other estrogens. In vitro reaction phenotyping studies were conducted to evaluate the role of drug-metabolizing enzymes in the metabolism of E4. Furthermore, to obtain a comprehensive understanding of the metabolic behavior of E4 in humans, metabolite profiling by mass spectrometry was performed, with samples collected during a phase I trial in which participants received an oral dose of radiolabeled-E4. Cytochrome P450 (CYP) enzymes do not play a major role in the metabolism of E4 [33], and, instead, E4 undergoes phase II metabolism with the production of inactive conjugated metabolites. Human metabolite profiling showed that the main metabolites observed in plasma after oral administration are E4-16-glucuronide, E4-3-glucuronide and E4-glucuronide-sulfate. E4 is not converted back into other active estrogens such as E3, E2 or E1 and is therefore considered as a terminal end-product of estrogen metabolism [34].
3 The Pharmacological Profile of E4
In order to gain insight into the pharmacological profile of E4, this compound was tested in a large panel of preclinical in vitro and in vivo models and then in clinical trials involving women of reproductive age as well as postmenopausal women. Current knowledge on the pharmacological activity of E4 includes data on the prevention of pregnancy, as well as the alleviation of menopausal symptoms. The biological responses induced by E4 on uterovaginal tissues, bones, the cardiovascular system, and the breast, and in regard to glucose metabolism, lipid profile, hepatic proteins and hemostasis balance, were also investigated and are presented below.
3.1 Prevention of Pregnancy
While the inhibition of ovulation is primarily induced by the progestin contained in a COC, the estrogenic component assists the progestin in its contraceptive activity and provides an adequate cycle control.
The efficacy of E4 to inhibit ovulation was first assessed and confirmed in rats, showing that the anti-ovulatory effect of E4 was dose-dependent, with two administrations per day of 0.3 mg/kg E4 effectively inhibiting ovulation in cycling rats [35]. In this experiment, the relative potency of E4 was about 18-fold lower than the synthetic estrogen EE. Based on these preclinical data, it was concluded that E4 was a good candidate to be the estrogenic component of a COC.
A phase II dose-finding pilot study was conducted to evaluate the efficacy of different doses of E4 (5–20 mg) in combination with a progestin (levonorgestrel or DRSP) in suppressing the pituitary-ovarian axis and ovulation in healthy premenopausal women for three consecutive cycles. Participants receiving EE 20 µg/DRSP 3 mg served as a reference group. The compounds were well tolerated, and all treatments resulted in inhibition of ovulation. Inhibition of ovarian activity was more pronounced in the highest E4 dose group and was very similar to that observed for the EE/DRSP group [36]. Another published clinical trial that included healthy young women with proven ovulatory cycles further demonstrated the adequate ovulation inhibition and ovarian function suppression for the combination of E4 15 mg/DRSP 3 mg in a 24/4-day regimen for three consecutive cycles. None of the participants using E4/DRSP ovulated during E4/DRSP use, while the subsequent return of ovulation occurred, on average, 15.5 days after treatment discontinuation [37].
Two comparable pivotal phase III clinical studies, conducted in North America (NCT02817841) [38] and Europe/Russia (NCT02817828) [39], assessed the contraceptive efficacy of the combination E4/DRSP. In the trial conducted in North America evaluating 1674 women aged between 16 and 35 years for 13 cycles, the overall and method-failure pregnancy rates were evaluated using the Pearl Index (PI) and life-table analysis. A PI of 2.65, a method-failure PI of 1.43, and a 13-cycle life-table pregnancy rate of 2.1% were reported, indicating that E4/DRSP is an effective method of contraception. The trial conducted in Europe and Russia that included 1353 women aged 18–35 years who used E4/DRSP for 13 cycles also showed a high contraceptive efficacy with a low PI of 0.47 pregnancies/100 woman-years. This PI value is similar to the marketed DRSP-containing COCs such as Yaz® and Yasmin®.
A pooled analysis of both phase III studies further demonstrated that E4/DRSP is an effective oral contraception overall, and, importantly, also across subgroups based on age, contraceptive history and body mass index [40]. The COC consisting of E4 15 mg/DRSP 3 mg is now approved and marketed in different territories, including Europe, Russia, US, Canada and Australia.
3.2 Alleviation of Vasomotor Symptoms
The efficacy of E4 to alleviate hot flushes was investigated in an experimental animal model considered representative for menopausal VMS. This experimental model consists of recording the thermal responses in the tail skin of morphine-dependent ovariectomized rats after morphine withdrawal by administration of naloxone. E4 was efficacious in alleviating hot flushes and suppressed the increase in tail skin temperature in a dose-dependent manner. In this model, the equipotent dose of E4 was 10 times higher than EE, suggesting that the potency of E4 may be lower than EE, although only one dose of EE was tested [41].
A dose-finding phase II clinical trial (E4Relief—NCT02834312) was conducted to select the effective dose of E4 for the treatment of VMS in postmenopausal women. A total of 257 postmenopausal women aged 40–65 years, presenting with at least seven moderate to severe hot flushes per day or at least 50 moderate to severe hot flushes per week received a daily dose of E4 (2.5, 5, 10 or 15 mg) for a period of 12 weeks. During that period, the efficacy of E4 in alleviating VMS was assessed by recording (in an e-diary) the frequency and severity of hot flushes, with statistical analysis performed at weeks 4 and 12. The frequency of hot flushes decreased with all tested E4 doses, with the most pronounced changes observed in the E4 15 mg group. The difference in the percentage change of weekly hot flushes frequency was significant for the E4 15 mg group versus placebo at both week 4 and week 12. The decrease in severity of hot flushes was significantly more pronounced for E4 15 mg than for placebo at both week 4 and week 12. With the other doses having failed to promote statistically significant effects versus placebo, E4 15 mg was considered to be the minimum effective daily oral dose for the treatment of VMS [42].
3.3 Effects of E4 on Uterovaginal Tissues
The ability of E4 to bind to the rat uterine ER, but with a lower binding affinity compared with E2, was originally demonstrated in 1976 [27]. Subsequently, a study in 1979 that evaluated the uterine response to E4 following subcutaneous administration of the compound to immature rats, showed that E4 influenced the uterine weight, luminal fluid volume and protein content [28]. The estrogenic action of E4 in the uterus has been confirmed in more recent preclinical studies [43, 44]. In ovariectomized female rats treated daily orally for 7 days, E4 1 mg/kg/day and 3 mg/kg/day induced a statistically significant increase in uterine wet weight compared with the vehicle group. The potency of E4 was estimated to be approximately 20-fold lower than EE in this rat model [43].
An acute treatment with E4 in ovariectomized mice induced uterotrophic effects and changes in uterine gene expression. Luminal epithelial height and stromal height were significantly increased by subcutaneous administration of E4 1 mg/kg. Accordingly, epithelial proliferation measured by Ki67 staining was also increased in mice treated with E4. The expression of a set of uterine genes known to be regulated by estrogen was evaluated in ovariectomized mice 6 h after a treatment with E4, and this transcriptomic analysis revealed that all E2-responsive genes in the uterus were also modulated by E4. In most cases, a 100-times higher dose of E4 was necessary to mimic the transcriptional effect induced by E2. The gene expression profile and the histological changes induced by concomitant treatment with E2 and E4 was similar to the profile induced by E2 alone [44].
The estrogenic activity of E4 was also shown in the vagina in preclinical models. A modified Allen–Doisy test conducted in ovariectomized female rats showed that E4 induced vaginal cornification in a dose-dependent manner after 5 days of oral treatment (E4 0.1, 0.3, 1 or 3 mg/kg) [43]. In ovariectomized mice, morphological and functional changes in the vagina were observed after chronic treatment with E4 (subcutaneous minipumps releasing 1 or 6 mg/kg/day), including an increase in vaginal weight, an increase in vaginal epithelial proliferation and epithelial height, as well as an increase in vaginal lubrication after cervical vaginal stimulation [45].
The endometrium plays a central role in the uterine bleeding process. One of the purposes of including an estrogen in a COC is to counterbalance the effects of the progestin on the endometrium, thereby providing good cycle stability and an acceptable bleeding pattern. The fact that a reduction of the estrogen dose in COCs or the use of progestin-only pills often results in bleeding irregularities clearly illustrates this role for the estrogenic component [46, 47]. A regular and predictable bleeding profile is an important factor influencing COC choice, acceptability and adherence. Bleeding data from different clinical trials highlight the favorable and highly predictable bleeding pattern with limited unscheduled bleeding/spotting for the combination of E4/DRSP [38, 39, 48, 49]. A pooled analysis of two phase III trials including bleeding data from over 3400 participants showed that the use of the E4 15mg/DRSP 3mg COC in a 24/4-day treatment regimen is associated with a regular and predictable bleeding pattern [48]. This further demonstrates the adequate estrogenic activity of E4 on the endometrium as well as its capacity to counterbalance the effects of the progestin to stabilize the endometrium and offer a good cycle control.
In postmenopausal women receiving oral E4 alone (2.5, 5, 10 or 15 mg) for a period of 12 weeks, the endometrial thickness increased during treatment in a dose-dependent manner. While the mean endometrial thickness at baseline was 2.5 mm and was comparable among groups, a mean endometrial thickness of 3.9 mm (E4 2.5 mg) to 6.2 mm (E4 15 mg) was reported at week 4. The endometrial thickness remained stable until week 12 for all groups except the E4 15 mg group, for which the mean endometrial thickness increased to 7.9 mm. However, no endometrial hyperplasia was observed in any of the treatment groups. The endometrial thickness normalized and returned to baseline levels (3.2 mm) following progestin treatment (10 mg dydrogesterone daily for 14 days) at study completion [42].
In the same trial with postmenopausal women, the effects of oral E4 were also evaluated on vaginal cytology, genitourinary syndrome of menopause, and health-related quality-of-life. The different outcomes included the vaginal epithelial cell maturation index, maturation value, vaginal pH, the genitourinary syndrome of menopause score (vaginal dryness, vaginal pain associated with sexual activity, vaginal irritation/itching, dysuria; reported in an e-diary) and the Menopause Rating Scale (MRS) at baseline and at week 12. Overall, E4 promoted estrogenic effects in the vagina and decreased signs of atrophy, confirming that E4 is a promising treatment option for these menopausal symptoms. Regarding vaginal cytology, a decrease in parabasal and intermediate cells and an increase in superficial cells was observed at week 12 in all E4 groups compared with baseline, indicating improved vaginal estrogenization, with a significant effect in the E4 15 mg group. Additionally, the maturation value was increased in all E4 groups. Vaginal pH decreased in all E4 groups and slightly increased in the placebo group. In terms of self-reported genitourinary symptoms, compared with placebo, the intensity score at week 12 significantly decreased for vaginal dryness (in the E4 15 mg group) and vaginal pain (in the E4 5, 10 and 15 mg groups), while the changes observed for irritation/itching and dysuria were not significant. Of note, this trial was designed with a primary goal of assessing the effect of E4 on VMS as opposed to focusing specifically on genitourinary symptoms. The MRS score decreased in all E4 treatment groups after 4 and 12 weeks of treatment, with the most pronounced effects in the E4 15 mg group, highlighting an improvement in terms of quality of life and well-being [50].
3.4 Effects of E4 on Bone Metabolism
Although an effect on human osteoblastic cell proliferation was not detected in vitro [51], in vivo studies have suggested that E4 may play a beneficial role in the maintenance of bone mass.
A preclinical bone study conducted in ovariectomized female rats (a model of postmenopausal osteoporosis) showed that an oral treatment of E4 (0.1, 0.5 or 2.5 mg/kg/day) for 4 weeks significantly prevented the ovariectomy-related increase in osteocalcin levels, and improved bone mineral density and content, while also increasing bone strength. These bone-sparing effects induced by E4 were dose-dependent, although, similar to other studies, the potency of E4 was lower than for EE [52].
In healthy women of reproductive age using E4/DRSP for three consecutive cycles, no imbalance in bone markers was observed [53]. In line with the preclinical data, in a multiple-rising-dose study with postmenopausal women, E4 treatment induced changes in bone turnover markers, including a substantial dose-dependent decrease in osteocalcin levels, suggesting a preventative effect on bone loss [54].
In the phase II E4Relief trial (NCT02834312), in which postmenopausal women received E4 2.5, 5, 10, 15 mg or placebo daily for 12 weeks, changes in bone turnover markers (osteocalcin and type 1 collagen C-terminal telopeptide [CTX-1]) were evaluated at week 12 compared with baseline and versus placebo. CTX-1 levels significantly decreased from baseline in the E4 5 mg, 10 mg and 15 mg groups. In the analysis versus placebo, the decrease was significant in the E4 10 mg and 15 mg groups. The impact of E4 (5, 10 and 15 mg groups) on osteocalcin after 12 weeks of treatment was not significant from baseline but was significant versus placebo [55]. While this effect is consistent with the role of estrogens in bone remodeling and supports the potential beneficial effect of E4 in osteoporosis, additional clinical data (including long-term bone marker measurements, bone density scan and fracture data) are needed to validate this effect.
Further evidence regarding the benefits of E4 on the bone came from a phase II study evaluating a high dose of E4 (40 mg) in male patients with advanced prostate cancer requiring androgen deprivation therapy (ADT), where E4 was being evaluated as an add-on to ADT to improve the efficacy and adverse effects of ADT, including ADT-induced bone loss. Therefore, the secondary endpoints of the study included the assessment of bone metabolism (osteocalcin and type I collagen telopeptide). While bone metabolism markers increased in the group receiving luteinizing hormone-releasing hormone agonist alone (48% for osteocalcin and 151% for CTX-1) at week 24, those turnover parameters decreased significantly from baseline in the group cotreated with E4 [56].
3.5 Effects of E4 on the Cardiovascular System
It is known that estrogens modulate cardiovascular physiology and function [57], and as such the impact of E4 has been thoroughly assed in preclinical models of different cardiovascular functions including nitric oxide (NO) production, vasodilation, endothelial healing, atherosclerosis, neointimal proliferation and hypertension prevention. To date, the effect of E4 on these cardiovascular functions are limited to preclinical data, with no clinical data available yet.
3.5.1 Nitric Oxide Production and Vasodilation
Endothelial NO is a key player for vascular function and vasodilation and is a known target of estrogens [58]. In vitro, E4 induced rapid NO release and stimulated endothelial NO synthase (eNOS) activation and expression in human umbilical vein endothelial cells (HUVECs). However, E4 was significantly less effective compared with E2. When E4 was combined with E2, E4 antagonized NO synthesis induced by pregnancy-like E2 concentrations. However, E4 did not impede the induction of NO synthesis induced by lower E2 concentrations [59]. These data support that E4 may be a regulator of NO synthesis in human endothelial cells.
In a mouse model of carotid artery, E4 used at different dose levels (0.3, 1 and 6 mg/kg/day) failed to stimulate eNOS activation or endothelial NO production, while E2 was able to promote these two responses. When E4 was used in combination with E2, E4 antagonized the effects induced by E2 in mouse carotid artery. The combination E4+E2 therefore failed to promote eNOS activation and NO production in this experimental model [44].
Based on the antagonistic activity of E4 in the presence of E2 on NO release described above, lower cardiovascular effects (such as vasodilation) could be expected in the presence of E4. Importantly, several studies have confirmed that NO production, which is essential for adequate vasodilation and endothelial function, is controlled by multiple factors besides estrogens. The regulation of vascular tone by endothelium-derived NO is mediated by multiple controlling mechanisms, including physical factors such as an increase in shear stress or reduction in temperature, as well as by neurohumoral mediators through the activation of specific endothelial cell membrane receptors. The main physiological driver of NO production is shear stress [60,61,62] and estrogens are considered to play a limited role in the regulation of endothelial-derived NO production and subsequent physiological vasodilation. The impact of E4 on shear stress, was evaluated in an ex vivo model of flow-mediated vasodilatation. Chronic treatment with E4 promoted the occurrence of flow arteriolar remodeling in ovariectomized mice after an increase in blood flow, demonstrating that the presence of E4 did not impair the NO-mediated vasodilation [63].
Moreover, E4 was shown to induce vasodilation of animal arteries by a specific mechanism distinct from NO production, whereby E4 induced the vasodilation of ewe uterine arteries at high concentrations [64]. It also induced ex vivo relaxing responses in eight different vascular beds: rat uterine, aorta, carotid, mesenteric, pulmonary, renal, middle cerebral and septal coronary arteries. The vasodilation induced by E4 in rat arteries was ER-dependent since it was abrogated by the ER antagonist ICI 182 780. Blockade of eNOS by Nω-nitro-l-arginine methyl ester (an NO synthase inhibitor) blunted the E2-mediated, but not E4-mediated, relaxing response, demonstrating that E2, but not E4, induced vasodilation by stimulating eNOS activity. Overall, this study shows that E4 induced relaxation of precontracted rat arteries via both an endothelium-dependent mechanism and a guanylate cyclase mechanism [65].
In conclusion, NO production is not the only mechanism eliciting the beneficial impact of estrogens on vasculature. The lack of E4-induced eNOS activity and NO release observed in some but not all experimental models should not be associated with any vascular safety concerns.
3.5.2 Endothelial Healing
The preclinical model of endothelial healing is usually used to assess the vascular protective effects of a compound. The acceleration of endothelial healing by estrogens is considered as a vasculo-protective action. A recent study demonstrated that chronic treatment with E4 (subcutaneous pellet) was able to accelerate endothelial healing after carotid artery injury in ovariectomized mice. The quantitative analysis of re-endothelialized areas, performed 5 days after endovascular injury, showed an increase of 30% of endothelial regeneration in control mice compared with day 0, and an increase of about 80% in mice treated with E4 [66].
It was previously reported in another study published by the same group that E4 was not able to promote endothelial healing in the mouse carotid artery model [44]. In the experimental model used for that study, both the artery media and endothelium were injured by electrocoagulation (perivascular injury) and the endothelial regeneration process was evaluated 3 days post-injury by the quantification of the re-endothelialized area. In these conditions, no effect was observed with E4, regardless of the dose levels used (0.3, 1 or 6 mg/kg/day) [44]. Davezac et al. showed that in contrast, a model of specific endothelial destruction of the carotid artery, preserving smooth muscle cells, does not lead to the same results [66]. When the injury is limited to the artery endothelium and when the underlining layer of vascular smooth muscle cells stays intact, E4 is able to accelerate the endothelial healing (re-endothelialization) after artery injury, highlighting that smooth muscle cells are necessary for E4 to mediate this endothelial function in mice. These conflicting results, at first glance, illustrate the crucial importance of the preclinical models and experimental conditions when interpreting data.
A recent study evaluating the impact of estrogens used in oral contraceptives on human endothelial function showed that E4 (10−9 to 10−7 M) significantly enhanced migration of HUVECs using scratch and Boyden chamber assays. The effect of E4 on endothelial migration was comparable with the effect of EE, suggesting comparable vascular remodeling and regeneration capacity [67].
3.5.3 Atherosclerosis Prevention
The impact of E4 on the prevention of atheroma was assessed in low-density lipoprotein receptor-deficient (LDLr−/−) mice fed a high-cholesterol diet, a well-described model to investigate the atheroprotective effects of estrogens.
E4 used at 0.6 or 6 mg/kg/day in the diet for 12 weeks prevented lipid deposition and reduced atheroma deposits in the aortic sinus in ovariectomized LDLr−/− mice up to almost 80% in a dose-dependent manner. E4 also decreased the total plasma cholesterol in these mice [44, 68].
3.5.4 Neointimal Hyperplasia Prevention
Neointimal hyperplasia refers to post-intervention (e.g. after mechanical atherosclerosis treatment), pathological, vascular remodeling due to the proliferation and migration of vascular muscle cells into the tunica intima layer. Neointimal hyperplasia can ultimately result in vascular wall thickening and in a reduction of the lumen diameter, which in turn leads to vascular insufficiency and restenosis.
In a mouse model of femoral artery mechanical injury, E4 prevented neointimal hyperplasia by a direct inhibitory effect on the proliferation and migration of vascular smooth muscle cells but not by acting on endothelial cells. Morphometric analysis showed that 28 days after the injury, the mice treated with E4 exhibited a reduced neointima/media ratio [69].
3.5.5 Hypertension Prevention and Arteriolar Remodeling Promotion
Additional vasculoprotective actions were described after chronic treatment with E4, including the prevention of angiotensin II-induced hypertension, which is a major risk factor of cardiovascular diseases, and the restoration of arteriolar flow-mediated remodeling, which has a major role in the homeostasis of tissue perfusion [63]. In that study, flow-mediated remodeling was evaluated in mesenteric arteries isolated from ovariectomized mice treated with vehicle or E4 over 2 weeks. The arterial diameter was measured in response to stepwise increases in pressure in mesenteric arteries submitted to high flow or to normal flow. The effect of E4 on angiotensin II treatment was evaluated in ovariectomized female mice implanted with osmotic minipumps delivering angiotensin II or a combination of angiotensin II and E4 for 1 month, with systolic blood pressure being measured weekly. E4 prevented angiotensin II-induced hypertension and favored flow-mediated remodeling [63].
3.6 Effects of E4 on the Breast
Sex steroids promote the growth of certain hormone-dependent tissues and tumors. Efforts have been made to characterize the impact of E4 on breast epithelial cell proliferation and breast cancer growth in preclinical models and preliminary clinical trials.
3.6.1 Normal Breast Epithelial Cell Proliferation
In vitro exposure of normal human breast epithelial cells for 96 h with 10 nM E2 elicited a maximal cell proliferation increase of about 60%. At the same concentration, E4 did not increase human breast epithelial cell proliferation. A 100 times higher concentration of E4 (1 µM) was necessary to stimulate the proliferation to the same extent as E2 [70].
To evaluate the effect of E4 on mammary gland, prepubertal ovariectomized mice were treated orally with different dose levels of E4 (0.3, 1, 3 or 10 mg/kg/day) or with E2 (1 mg/kg/day) for 14 days, after which mammary glands were collected and epithelial cells isolated. The level of epithelial proliferation assessed by the expression of cyclin D1 and Ki67 mRNA was significantly lower in mice treated by E4 (at any dose levels) compared with mice treated with E2, suggesting a lower proliferative effect for E4 [70].
3.6.2 Breast Cancer Growth
E4 also exhibits a lower potency than E2 to induce human breast cancer cell growth. Liu et al. investigated the impact of different estrogens, including E2 and E4, on proliferation of the ER-positive breast cancer cell line ZR 75-1 in vitro. All estrogens tested caused a significant stimulation of cell proliferation. At the lowest concentration (10−10 M), E4 had a significantly lower stimulatory effect than E2, while at higher concentrations (≥10−9 M), E2 and E4 stimulated cell proliferation to the same extent [71]. In another assay using MCF-7 cells transfected with PGRMC1, E4 was also significantly less active than E2 in promoting cell proliferation. At 10−10 M, E2 increased the proliferation rate by about 160%, while E4 induced an increase of only 50% compared with the control condition. At higher concentrations (≥10−9 M), the same proliferative effect (about +160%) was elicited by E2 and E4 [71].
In another study, a 1000 times higher concentration of E4 was needed to promote MCF-7 and MCF-7/BOS cell growth in vitro to the same extent as E2, confirming the weaker potency of E4 to induce human breast cancer cell growth compared with E2 in vitro [72].
An estrogen supplementation is necessary for the growth of MCF-7 and the formation of tumor in vivo. To determine if E4 could achieve the same effect as E2 in this model, ovariectomized immunodeficient mice implanted with MCF-7 cells received a daily oral treatment of E4 (0.5, 1, 3 or 10 mg/kg/day) or E2 (3 mg/kg/day). After 5 weeks of treatment, E2 promoted tumor growth, with tumor weights being fivefold higher compared with the untreated group. No significant difference was observed between the untreated control group and mice treated with E4 0.5 mg/kg/day. Indeed, E4 was as efficient as E2 in promoting tumor growth only at the highest dose level of 10 mg/kg/day, confirming the lower potency of E4 to induce breast cancer growth compared with E2 in vivo [72].
The effect of a combined treatment with E2 and E4 on MCF-7 tumor growth was also analyzed, whereby ovariectomized mice implanted with MCF-7 cells and with a subcutaneous E2 pellet received a daily oral treatment of E4 (1, 3 or 10 mg/kg/day) for 5 weeks. In these conditions, E4 attenuated E2-induced tumor growth in a dose-dependent manner. Exposure to the combination of E2 + E4 decreased the tumor volume and tumor weight by approximately 50% compared with mice exposed to E2 alone. This antagonistic effect of E4 in the presence of E2 was also observed for MCF-7 cell proliferation in vitro. This effect became maximal when E4 was at least 100 times more concentrated than E2 [72].
In a broader preclinical study combining genetically engineered mouse models, human cell line xenografts and hormone-dependent authentic breast tumor patient-derived xenografts, the authors showed a limited effect of E4 on breast cancer growth in vivo when used at doses similar to the therapeutic levels required for contraception or menopause [73].
3.6.3 Breast Cancer Migration and Invasion
Breast cancer cell movement requires a remodeling of the actin cytoskeleton, involving estrogen-mediated signaling pathways. Interestingly, it has been demonstrated that E4 acts as a weak estrogen on breast cancer cell migration and invasion. The effects of E4 on its own or in the presence of E2 were tested on T47-D breast cancer cell migration and invasion of three-dimensional matrices. Exposure of T47-D cells to E4 weakly stimulated migration and invasion in comparison with E2. In addition, E4 decreased the extent of movement and invasion induced by E2 [74].
3.6.4 Clinical Data
The effect of 14 days of preoperative treatment with E4 20 mg/day on tumor proliferation markers was investigated in a preoperative window trial in 30 pre- and postmenopausal women with ER+ early breast cancer. E4 had a significant proapoptotic effect on tumor tissue, whereas Ki67 expression (a marker of cell proliferation) remained unchanged in both pre- and postmenopausal women [75]. The efficacy of high doses of E4 in postmenopausal patients with pretreated, locally advanced, and/or metastatic ER+/HER2− breast cancer was assessed in a phase IB/IIA, dose-escalation study in which successive cohorts of three patients received E4 20, 40 or 60 mg/day for 12 weeks by oral administration. Five of nine patients completing 12 weeks of E4 treatment showed objective antitumor effects, as evaluated by computer tomography scanning according to the Response Evaluation Criteria in Solid Tumors (RECIST) criteria, with stabilization of the disease in four patients and one complete response. The complete response was seen with the 20 mg dose, and stabilization of the disease was observed in one patient in the 20 mg group and three patients treated with 40 mg [76].
3.7 Lipid Profile, Carbohydrate Metabolism and Metabolic Disorders
The use of hormone therapy can impact metabolic markers such as total cholesterol, low-density lipoprotein cholesterol (LDLc), high-density lipoprotein cholesterol (HDLc), triglycerides and glucose levels.
The effect of E4 on the pathophysiological consequences of a Western diet (42% kcal fat, 0.2% cholesterol) was evaluated in mice. Weekly body weight measurements showed that chronic treatment with E4 reduced body weight gain and protected mice against Western diet-induced obesity. After 7 weeks of Western diet feeding, E4 improved glucose tolerance in mice. At the end of the protocol, fasting glucose levels were significantly lower in mice treated with E4. A reduced accumulation of subcutaneous, perigonadal and mesenteric adipose tissue was also observed in the E4-treated group. In addition, disorders associated with obesity, such as atherosclerosis and steatosis, were prevented in mice fed a Western diet and treated with E4. Furthermore, E4 induced a lower accumulation of lipids in the liver. Accordingly, the expression of genes involved in lipid metabolism, including cholesterol metabolism and lipoprotein assembly, was decreased in the liver of E4-treated mice compared with control mice. The study demonstrated that E4 prevents Western-induced obesity by increasing locomotor activity and energy expenditure [68].
In postmenopausal women receiving E4 2.5, 5, 10 or 15 mg daily for 12 weeks in the E4Relief trial (NCT02834312), absolute changes from baseline in triglyceride levels were minimal in all study groups and were not significant when compared with placebo. HDLc increased from baseline in all E4 groups, while no increase was observed in the placebo group. An increase from baseline was observed for LDLc in the E4 2.5 and 5 mg groups and for total cholesterol in the E4 2.5, 5 and 10 mg groups. None of these changes were significantly different when compared with placebo. Regarding glucose metabolism, no significant change in fasting glucose level was observed from baseline. A significant decrease was seen in insulin resistance and hemoglobin A1c in the E4 10 and 15 mg groups, respectively, suggesting an improved glucose tolerance [55].
The impact of E4 in combination with a progestin on lipid metabolism was evaluated in healthy women. Participants (healthy women aged between 18 and 35 years) received E4/DRSP, E4/LNG or EE/DRSP as a comparator for three consecutive cycles. Minor effects on lipoproteins were observed in the E4 groups and the effects on triglycerides in the E4 groups were significantly lower compared with the EE group, demonstrating that E4-containing COCs have a limited effect on lipid metabolism [53].
The effect of the combination of E4 15 mg/DRSP 3 mg on metabolic parameters, including lipid profile and carbohydrate metabolism, after six treatment cycles was then evaluated in healthy subjects [77]. The study included two frequently used EE-containing COCs as comparators, one with LNG and one with DRSP, to validate changes related to the estrogen component. E4/DRSP had a minimal impact on lipid parameters; the largest effect was observed for triglycerides (+24.0%), which was less compared with EE/LNG (+28.0%) and EE/DRSP (+65.5%). With E4/DRSP, no significant changes from baseline were observed for LDL-C, total cholesterol, the HDL-C/LDL-C ratio, and lipoprotein A. Carbohydrate parameters, including fasting insulin and glucose, C-peptide and HbA1c, remained relatively stable in all treatment groups. Oral glucose tolerance test (OGTT) glucose and insulin concentrations varied substantially with no remarkable treatment differences. Changes in carbohydrate parameters were minimal, pointing towards a negligible impact on glycemic control [77].
Taken together, these data tend to demonstrate a low impact of E4 on lipids and carbohydrate metabolism. The COC with E4 15 mg/DRSP 3 mg is associated with a favorable effect on body weight control [78, 79].
3.8 Effects of E4 on Liver Proteins and Hemostasis Balance
Sex hormone binding globulin (SHBG) is an estrogen-responsive protein produced by the liver that reflects the overall estrogenic impact of a compound on the liver [80, 81]. Moreover, the plasma levels of SHBG can modify the plasma distribution of natural steroid ligands.
The effect of E4 on the production of SHBG has been evaluated in vitro in human HepG2 cells and human Hep89 cells overexpressing ERα and was compared with the effect of other estrogens. Exposure to E4 (0.1–1000 nM) during 24, 48 or 72 h did not stimulate the production of SHBG in either cell lines. In contrast, a significant dose-dependent increase in SHBG production was observed after exposure to other estrogens such as EE, E2 and E3 [82]. These in vitro data may indicate that E4 is less likely to modulate the plasma levels of SHBG.
In a clinical trial including 49 postmenopausal women, treatment with escalating doses of E4 (2–40 mg) for 28 days induced a dose-dependent increase of SHBG levels. When looking at the different doses of E4, only the 10 mg E4 group elicited a similar increase in SHBG levels as the 2 mg E2-valerate group (59% and 62%, respectively), suggesting a lower potency of E4 on the production of SHBG [54]. In the E4Relief trial (NCT02834312) conducted in postmenopausal women, a dose-dependent increase in SHBG levels compared with baseline was also observed in E4-treated groups (+10.3%, +23.3%, +61.8% and +99.4% for E4 2.5, 5, 10 and 15 mg, respectively) [55]. Moreover, the combination E4/DRSP given to healthy women during six cycles had significantly less impact (+55%) than the combination EE/DRSP (+251%) on SHBG production [83]. In conclusion, although an effect on SHBG production is noted after oral treatment with E4 in clinical trials, in contrast to the absence of effect reported in in vitro assays, the effect of E4 stayed small compared with other estrogens, suggesting a lower estrogenic effect on the liver.
Preclinical studies in relation to coagulation risks, showed that chronic E4 treatment in ovariectomized female mice exhibited a prolonged tail-bleeding time and were protected from arterial and venous thrombosis in vivo. In addition, E4 treatment decreased ex vivo thrombus growth on collagen under arterial flow conditions [84].
To assess the effects of the COC containing E4 on hemostasis parameters, healthy women received the combination E4/DRSP, EE/LNG or EE/DRSP as comparators, during six cycles.
Activated protein C resistance is observed in COC users [85] and this functional assay is used to assess the thrombogenicity potential of COCs [86]. The median change of endogenous thrombin potential (ETP)-based activated protein C sensitivity resistance (APCr) at cycle 6 was +30% for E4/DRSP, +165% for EE/LNG, and +219% for EE/DRSP. Changes in hemostasis parameters, including anticoagulant proteins and fibrinolytic proteins, after treatment with six cycles of E4/DRSP, were smaller or similar to those observed for EE/LNG. However, much more pronounced changes were observed with EE/DRSP [83]. Absolute changes from baseline for hemostasis parameters were also minimal in postmenopausal women receiving E4 alone for 12 weeks [55].
The thrombin generation coagulation assay is used as a marker of hypercoagulability and risk of VTE [87]. A comparative assessment of the impact of E4/DRSP and EE/LNG or EE/DRSP on thrombin generation was conducted. Data were collected from trial NCT02957630, in which thrombograms and thrombin generation parameters were extracted for each subject at baseline and after six cycles of treatment. It was shown that E4 in combination with DRSP does not have any impact on thrombin generation in contrast to EE-containing products that induce the production of procoagulant factors, a decrease in the synthesis of anticoagulant factors, and therefore induce a shift towards a prothrombotic state [21, 88]. It can therefore be concluded that EE-containing products induce a prothrombotic environment while E4 exhibits a neutral profile on hemostasis (Fig. 2).

Source: Morimont et al. [21]
Thrombin generation curves in the absence and presence of APC in healthy pooled plasma (blue) and women using different combined oral contraceptives. The area under the curve represents the ETP parameter. In the presence of APC, ETP is higher with the use of combined oral contraceptives (e.g. EE/DRSP, EE/DSG) compared with HPP, leading to a resistance towards APC. APC activated protein C, DRSP drospirenone, DSG desogestrel, EE ethinylestradiol, ETP endogenous thrombin potential, E4 estetrol, HPP healthy pooled plasma, LNG levonogestrel.
Pooled analysis of data from two phase III trials including 3417 participants showed that the combination of E4/DRSP is associated with an overall favorable safety profile. A single case of VTE was reported, which resolved without sequelae after anticoagulant treatment [89].
While available hemostasis data described above suggest that the E4/DRSP COC may be associated with a lower VTE risk, this will need to be demonstrated in a larger population in postauthorization safety studies.
4 Molecular Mechanism of Action
4.1 Estrogen Signaling Pathways
The pleiotropic effects of estrogens are mainly mediated by ER alpha (ERα) and beta (ERβ), each encoded by separate genes, ESR1 and ESR2, respectively, located on different chromosomes.
ERα and ERβ belong to the nuclear receptors protein family and mainly function as ligand-dependent transcription factors. ERs contain two transactivation functional domains AF-1 and AF-2. After ligand binding to ERs, an ordered sequence of events takes place to regulate the transcription of estrogen-responsive genes. The binding of estrogen to the ligand-binding domain (LBD) of the ER induces conformational changes in the receptor. After the dimerization and recruitment of coregulators, the estrogen/ER complexes translocate into the nucleus and directly bind to the estrogen-responsive element (ERE) in the promoter region of target genes to directly modulate their transcription. This ERE-dependent process is referred to as the classical genomic pathway.
Distinctly, ERs can also regulate the transcription of genes without any direct interaction with the DNA. In this case, ERs act as co-activators for other DNA-binding transcription factors, leading to the indirect binding of ERs to regulatory DNA sequences, such as AP-1 or Sp1 sequences. This mechanism of action enables the transcription of genes that do not harbor ERE sequences in their promoter region. This pathway is referred to as the non-classical genomic pathway.
Aside from genomic signaling, estrogens can elicit non-genomic events, also commonly referred as extranuclear or membrane-initiated signaling. The non-genomic effects of estrogens are mediated via a pool of ERs present at the plasma membrane or in the cytoplasm. The membrane-bound ERα undergoes a post-translational palmitoylation on cysteine 447 (451 in mice). This modification is necessary for ERα localization at the cell membrane, where it is associated with caveolin-1. The ligand binding to membrane ER leads to rapid activation of different signaling pathways, including the mitogen-activated protein kinase (MAPK) or phosphatidylinositol-3 kinase (PI3K) pathways, and the subsequent production or modulation of second messengers such as AMPc, calcium mobilization or NO synthesis, which in turn directly influence various cell functions. The non-genomic effects usually occur within seconds or minutes after estrogenic treatment. Another membrane receptor termed G protein-coupled estrogen receptor 1 (GPER, also referred to as GPR30) has been more recently described to contribute to the physiological and pathological effects promoted by estrogens [90].
While the genomic and non-genomic pathways induced by estrogens play specific roles in the regulation of transcription and in rapid signaling, respectively, and modulate biological processes independently, they also interact in a still poorly described way. The activation of kinase signaling cascades can ultimately induce the phosphorylation and activation of transcription factors, including ERs themselves and coregulators, and therefore indirectly regulate gene expression. This interplay between both signaling pathways can thus result in enhanced transcriptional activity and cellular responses. Conversely, the genomic pathway can modulate the transcription of genes involved in the non-genomic signaling. Cellular responses and biological processes induced by estrogens are usually thought to be a convergence of both genomic and non-genomic pathways [91]. A schematic representation of genomic and non-genomic signaling pathways is presented in Fig. 3.
Schematic representation of genomic and non-genomic signaling pathways induced by estrogens. Classical estrogen signaling occurs via ERs belonging to the nuclear receptors protein family and mainly functioning as ligand-dependent transcription factors to modulate the transcription of target genes. Alternatively, estrogens may activate non-genomic signaling via ERs located at the plasma membrane. Non-genomic signaling events include the activation of kinase cascades in the cytoplasm and the production of second messengers that ultimately induce cellular responses. Genomic and non-genomic signaling pathways also interact and influence each other. ER estrogen receptor
4.2 Interaction of E4 with ERα and ERβ
E4 selectively binds to both ERα and ERβ, with a 4 to 5-fold higher binding affinity for ERα. The binding affinity of E4 for ERα is at least 25-fold lower compared with E2 [33].
When the crystal structures of the ERα LBD complexed with E4 or E2 were compared, both were found to be very similar in their overall conformation. In addition, the ligands were perfectly superimposable and interacted equally with residues within the ligand-binding pocket. In addition, similar to the E2-ERα complex, the E4-ERα complex binds to the key coactivator protein SRC3 [44]. A further functional characterization of E4-ERα has been performed through a coregulator recruitment assay, comparing the binding pattern of ERα to 154 coregulator motifs induced by E2 and E4. The pattern of coregulator recruitment induced by E4 was very similar to that elicited by E2, but E4 was less potent than E2 to induce this recruitment pattern [92].
4.3 E4 Genomic Signaling Pathways
E4 induces transcriptional activity via both ERα and ERβ. The impact of E4 on the activation and binding of ERα to the ERE was investigated with a luciferase reporter gene assay based on T47D-KBluc cells (breast cancer cell line) in the presence of increasing concentrations of E2 or E4. Like E2, E4 stimulated the ERE transactivation in these cells, although with a 100- to 1000-fold lower potency compared with E2. E4 failed to antagonize the effects of E2 on the induction of ERE transactivation [72]. These data are consistent with the lower ERα binding affinity of E4 compared with E2. The contribution of AF-1 and AF-2 in the classical genomic actions induced by E4 was evaluated in HepG2 and HeLa cell systems. As previously described for E2, both AF-1 and -2 are involved in this action in a cell type-dependent manner [44].
The capacity of E4 to promote non-classical genomic effects was also confirmed by measuring the expression of genes that do not harbor an ERE in their promoter region: BRCA1 and CCDN1. These genes are thought to be regulated by the recruitment of ERα to AP-1 or Sp1 sites in their promoter region. E4 was able to upregulate the expression of these genes [72], demonstrating the capacity of E4 to induce classical and non-classical genomic effects.
Several estrogen-induced biological responses have been described to be dependent on the nuclear activation of ERα, including uterine epithelial proliferation [93], vaginal epithelial proliferation and lubrication [45], prevention of bone demineralization [94], the cardioprotective effect observed in response to estrogens [44, 63], and the actions of estrogens on energy balance and glucose homeostasis [95]. As described in the different sections above, E4 is able to induce these responses to the same extent as other estrogens, confirming its capacity to activate the ERα nuclear pathway.
4.4 E4 Non-genomic Signaling Pathways
E4 has been shown to induce rapid extranuclear effects on the ERK1/2 and PI3K/AKT pathways in MCF-7 cells in vitro or in MCF-7 tumors collected from mice after 5 weeks of treatment. E4 increased the phosphorylation of ERK1/2 in a fast and transient manner, with maximal activation seen after 5 min [72]. However, in this study, the receptor responsible for the extranuclear effects induced by estrogens was not identified and the signal of the immunohistochemistry staining in tumors was not quantified.
The interaction between ERα and the tyrosine kinase Src leading to the extranuclear complex ERα:Src is a well-described aspect of ERα activation at the membrane [96,97,98]. While E2 was found to promote this interaction, E4 was much less efficient in inducing the ERα:Src interaction. In addition, when administrated together, the combination of E2 + E4 totally abrogated the interaction between ERα and Src [44].
The treatment of breast cancer cells with estrogens is associated with ERα membrane translocation and the rapid formation of specialized cell membrane structures through activation of the actin-binding protein moesin. This process is responsible for rapid changes in cell membrane morphology, leading to cell migration and invasion [99]. The treatment of T47-D cells with E4 stimulated migration and invasion to a much lower extent than E2. When E4 was added to E2, an inhibition of the actin remodeling induced by E2 was seen. E4 decreased the extent of movement and invasion induced by E2 [74].
E4 was tested on the activation of eNOS in mice aortae by measuring eNOS phosphorylation and NO production, which are thought to be exclusively dependent on membrane ERα signaling after estrogen treatment [44]. While E2 rapidly induced eNOS phosphorylation and NO production, E4 failed to produce these effects. Furthermore, when coadministered, E4 inhibited the stimulatory action of E2 on these endothelial actions.
Altogether, the data indicate that in specific cell types such as breast cancer cells and endothelial cells, E4 presents a specific profile of ERα activation by inducing only ERα nuclear actions and preventing ERα membrane actions.
Furthermore, a possible contribution of the membrane receptor GPER in E4-induced breast cancer cell growth has been suggested since G15, a GPER antagonist, partially decreased E4-induced MCF-7 cell growth [72]. The effect of E4 on endothelial cells migration has also been reported to be driven by GPER-dependent mechanisms [67].
5 A Unique Molecular Mode of Action and a Different Metabolism: The Reasons Behind the Selective Pharmacological Profile of E4?
Available clinical data indicate that E4 has a more selective pharmacological profile compared with other estrogens, reflected by a low estrogenic impact on the liver, including on SHBG production, hemostasis parameters and lipid profile. Preclinical data also suggest that E4 may have a differential effect on breast epithelial cells and breast cancer cells compared with other estrogens.
The biological effects induced by E4 were shown to be primarily driven via ERα. E4 is able to activate the nuclear ERα signaling pathway to the same extent as other estrogens to induce biological responses. However, in different cell types, E4 displays a specific profile of ERα activation uncoupling nuclear and membrane activation.
In breast cancer cells, E4 poorly induces the extranuclear interaction between ERα and Src and poorly induces the ERα-dependent activation of moesin. Both genomic and non-genomic actions of ERα play pivotal roles and work in concert to induce breast cancer cell proliferation and survival [91, 100]. The interaction between the MAPK pathway and ERα has, for example, been described to promote a proneoplastic transcriptional network in the mammary gland [101]. Furthermore, the extranuclear signaling between ERα and Src is reported to play an important role in ER+ breast cancer [97] and to constitute a potential new therapeutic target in breast cancer [96]. The molecular mode of action of E4 may therefore support the lower impact of E4 on breast cell proliferation and breast cancer growth observed in preclinical studies.
Next to the ER-mediated effects on breast cell proliferation, the production of highly reactive estrogen metabolites also contributes to the risk of breast carcinogenesis [10, 11]. CYP enzymes do not play a major role in the metabolism of E4, suggesting that E4 metabolism does not generate reactive metabolites and that E4 might be devoid of this carcinogenesis pathway, contrary to other estrogens. This hypothesis needs to be verified in dedicated studies.
While the precise mechanisms behind the modulation of hemostasis parameters by estrogens are not fully understood, several studies suggest that estrogen metabolism might be linked to the higher risk of VTE seen among estrogen users. Women using oral but not transdermal MHT have an increased risk of VTE, suggesting that the hepatic first-pass effect of oral estrogens might be involved. Oral MHT results in a substantial increase in plasma E1 concentration, and studies showed that E1 levels correlated with peak thrombin generation in women using oral MHT. The effect of E1, the main metabolite of oral E2, on thrombin generation may therefore provide an explanation for the higher thrombotic risk seen in women using oral MHT [102]. Another study indicated that the thrombotic risk may be modulated by the expression of CYP enzymes involved in the hepatic metabolism of estrogens. Carriers of the CYP3A5*1 allele exhibit a high expression of CYP3A5 and present a higher thrombotic risk with oral estrogen compared with non-carriers [103]. This suggests that the formation of hydroxylated estrogen derivatives could be involved in the exacerbated hormone response in the liver. Since CYP enzymes are not of importance in the metabolism of E4 and since E4 is not converted back into E1, the metabolic particularities of E4 may support its lower impact on the hemostasis balance compared with other estrogens.
The selective pharmacological profile of E4 is also characterized by a low impact on lipid profile. Using transgenic mice expressing the ligand-binding domain of ERα exclusively at the plasma membrane, a study showed that exposure to propyl-pyrazole-triol, a selective ERα agonist, influenced the expression of many genes involved in lipid synthesis and lipid content in the liver (cholesterol, triglycerides and fatty acids). These data indicate that membrane-localized ERα is able to regulate some metabolic responses, at least in the liver, through a mechanism independent of the nuclear ERα pathway [104]. The differential effect of E4 on the membrane ERα may therefore also play a role in the hepatic aspects and, more specifically, on the lipid profile.
Collectively, pieces of evidence suggest that the molecular mode of action of E4 and the different metabolism of E4 may provide explanations for its selective pharmacological profile.
6 Conclusions
E4 is the estrogenic component of a recently marketed COC in combination with the progestin DRSP. E4 is also under development for use as an MHT.
The pharmacological characterization conducted in the framework of these developments indicates that E4, alone or in combination with a progestin, offers therapeutic efficacy for the prevention of pregnancy and alleviation of menopausal symptoms.
E4 elicits an adequate estrogenic activity in uterovaginal tissues and has the potential to prevent bone loss, as shown by preliminary clinical data. In addition, preclinical studies highlighted that E4 exerts beneficial actions on different cardiovascular functions.
While the use of oral estrogens can cause unwanted effects due to their impact on non-target tissues, E4 seems to display a more selective pharmacological profile. This includes a low estrogenic impact on the liver and the hemostasis balance, suggestive of a lower thrombotic risk. Although sex steroids can promote the growth of certain hormone-dependent tissues and tumors due to their hormonal action, preclinical evidence suggests that E4 may be associated with a lower risk of breast carcinogenesis compared with other estrogens. Epidemiological studies will be essential to verify these hypotheses and to confirm the improved safety profile of E4.
The main pharmacological properties of E4 described in this review are summarized in Fig. 4.
While further elucidation of the possible mechanisms will provide a deeper understanding, current data suggest that the molecular mode of action and the different metabolism of E4 may support its selective pharmacological profile and therefore its favorable benefit–risk ratio.
Data availability statement
No datasets were generated for the current review.
References
Brisken C, O’Malley B. Hormone action in the mammary gland. Cold Spring Harb Perspect Biol. 2010;2(12): 003178.
Anderson E, Clarke RB, Howell A. Estrogen responsiveness and control of normal human breast proliferation. J Mammary Gland Biol Neoplasia. 1998;3(1):23–35.
Olsson H, et al. Proliferation of the breast epithelium in relation to menstrual cycle phase, hormonal use, and reproductive factors. Breast Cancer Res Treat. 1996;40(2):187–96.
Isaksson E, et al. Effects of oral contraceptives on breast epithelial proliferation. Breast Cancer Res Treat. 2001;65(2):163–9.
Garcia y Narvaiza D, et al. Effect of combined oral contraceptives on breast epithelial proliferation in young women. Breast J. 2008;14(5):450–5.
Sung H, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49.
Morch LS, et al. Contemporary hormonal contraception and the risk of breast cancer. N Engl J Med. 2017;377(23):2228–39.
Beral V, Million Women Study C. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2003;362(9382):419–27.
Lyytinen H, Pukkala E, Ylikorkala O. Breast cancer risk in postmenopausal women using estradiol-progestogen therapy. Obstet Gynecol. 2009;113(1):65–73.
Cavalieri E, et al. Catechol estrogen quinones as initiators of breast and other human cancers: implications for biomarkers of susceptibility and cancer prevention. Biochim Biophys Acta. 2006;1766(1):63–78.
Cavalieri EL, Rogan EG. Depurinating estrogen-DNA adducts in the etiology and prevention of breast and other human cancers. Future Oncol. 2010;6(1):75–91.
Wang Z, et al. Development of a liquid chromatography electrospray ionization tandem mass spectrometry method for analysis of stable 4-hydroxyequilenin-DNA adducts in human breast cancer cells. Chem Res Toxicol. 2009;22(6):1129–36.
Embrechts J, et al. Detection of estrogen DNA-adducts in human breast tumor tissue and healthy tissue by combined nano LC-nano ES tandem mass spectrometry. J Am Soc Mass Spectrom. 2003;14(5):482–91.
Pruthi S, et al. Evaluation of serum estrogen-DNA adducts as potential biomarkers for breast cancer risk. J Steroid Biochem Mol Biol. 2012;132(1–2):73–9.
Gaikwad NW, et al. Urine biomarkers of risk in the molecular etiology of breast cancer. Breast Cancer (Auckl). 2009;3:1–8.
Cavalieri E, Rogan E. The 3,4-quinones of estrone and estradiol are the initiators of cancer whereas resveratrol and N-acetylcysteine are the preventers. Int J Mol Sci. 2021;22(15):8238.
Kopec AK, Luyendyk JP. Coagulation in liver toxicity and disease: role of hepatocyte tissue factor. Thromb Res. 2014;133(Suppl 1):S57–9.
Lidegaard O, et al. Hormonal contraception and venous thromboembolism. Acta Obstet Gynecol Scand. 2012;91(7):769–78.
Tchaikovski SN, Rosing J. Mechanisms of estrogen-induced venous thromboembolism. Thromb Res. 2010;126(1):5–11.
Lidegaard O. Hormonal contraception, thrombosis and age. Expert Opin Drug Saf. 2014;13(10):1353–60.
Morimont L, et al. Combined oral contraceptives and venous thromboembolism: review and perspective to mitigate the risk. Front Endocrinol (Lausanne). 2021;12: 769187.
Goldstajn M S et al. Effects of transdermal versus oral hormone replacement therapy in postmenopause: a systematic review. Arch Gynecol Obstet. 2022.
Hagen AA, Barr M, Diczfalusy E. Metabolism of 17-beta-oestradiol-4-14-C in early infancy. Acta Endocrinol (Copenh). 1965;49:207–20.
Tulchinsky D, et al. Plasma estetrol as an index of fetal well-being. J Clin Endocrinol Metab. 1975;40(4):560–7.
Coelingh Bennink F, et al. Maternal and fetal estetrol levels during pregnancy. Climacteric. 2008;11(Suppl 1):69–72.
Tseng L, Gurpide E. Competition of estetrol and ethynylestradiol with estradiol for nuclear binding in human endometrium. J Steroid Biochem. 1976;7(10):817–22.
Martucci C, Fishman J. Uterine estrogen receptor binding of catecholestrogens and of estetrol (1,3,5(10)-estratriene-3,15alpha,16alpha,17beta-tetrol). Steroids. 1976;27(3):325–33.
Holinka CF, Gurpide E. In vivo effects of estetrol on the immature rat uterus. Biol Reprod. 1979;20(2):242–6.
Holinka CF, et al. Comparison of effects of estertrol and tamoxifen with those of estriol and estradiol on the immature rat uterus. Biol Reprod. 1980;22(4):913–26.
Heikkila J, Luukkainen T. Urinary excretion of estriol and 15 alpha-hydroxyestriol in complicated pregnancies. Am J Obstet Gynecol. 1971;110(4):509–21.
Notation AD, Tagatz GE. Unconjugated estriol and 15alpha-hydroxyestriol in complicated pregnancies. Am J Obstet Gynecol. 1977;128(7):747–56.
Visser M, Holinka CF, Coelingh Bennink HJ. First human exposure to exogenous single-dose oral estetrol in early postmenopausal women. Climacteric. 2008;11(Suppl 1):31–40.
Visser M, Foidart JM, Coelingh Bennink HJ. In vitro effects of estetrol on receptor binding, drug targets and human liver cell metabolism. Climacteric. 2008;11(Suppl 1):64–8.
Gérard C, et al. RF34 | PMON202 the human metabolic profile of estetrol. J Endocrine Soc. 2022;6(Suppl 1):A714–5.
Coelingh Bennink HJ, et al. Ovulation inhibition by estetrol in an in vivo model. Contraception. 2008;77(3):186–90.
Duijkers IJ, et al. Inhibition of ovulation by administration of estetrol in combination with drospirenone or levonorgestrel: results of a phase II dose-finding pilot study. Eur J Contracept Reprod Health Care. 2015;20(6):476–89.
Duijkers I, et al. Effects of an oral contraceptive containing estetrol and drospirenone on ovarian function. Contraception. 2021;103(6):386–93.
Creinin MD, et al. Estetrol-drospirenone combination oral contraceptive: North American phase 3 efficacy and safety results. Contraception. 2021;104(3):222–8.
Gemzell-Danielsson K, et al. Estetrol-Drospirenone combination oral contraceptive: a clinical study of contraceptive efficacy, bleeding pattern and safety in Europe and Russia. BJOG. 2022;129(1):63–71.
Jensen JT, et al. Pooled efficacy results of estetrol/drospirenone combined oral contraception phase 3 trials. Contraception. 2022;116:37–43.
Holinka CF, Brincat M, Coelingh Bennink HJ. Preventive effect of oral estetrol in a menopausal hot flush model. Climacteric. 2008;11(Suppl 1):15–21.
Gaspard U, et al. A multicenter, randomized study to select the minimum effective dose of estetrol (E4) in postmenopausal women (E4Relief): part 1. Vasomotor symptoms and overall safety. Menopause. 2020;27(8):848–57.
Heegaard AM, et al. Estrogenic uterovaginal effects of oral estetrol in the modified Allen-Doisy test. Climacteric. 2008;11(Suppl 1):22–8.
Abot A, et al. The uterine and vascular actions of estetrol delineate a distinctive profile of estrogen receptor alpha modulation, uncoupling nuclear and membrane activation. EMBO Mol Med. 2014;6(10):1328–46.
Benoit T, et al. Estetrol, a fetal selective estrogen receptor modulator, acts on the vagina of mice through nuclear estrogen receptor alpha activation. Am J Pathol. 2017;187(11):2499–507.
Archer DF, Mansour D, Foidart JM. Bleeding patterns of oral contraceptives with a cyclic dosing regimen: an overview. J Clin Med. 2022;11(15).
Gallo MF, et al. 20 microg versus >20 microg estrogen combined oral contraceptives for contraception. Cochrane Database Syst Rev. 2013;8: CD003989.
Kaunitz AM et al. Pooled analysis of two phase 3 trials evaluating the effects of a novel combined oral contraceptive containing estetrol/drospirenone on bleeding patterns in healthy women. Contraception. 2022.
Apter D, et al. Bleeding pattern and cycle control with estetrol-containing combined oral contraceptives: results from a phase II, randomised, dose-finding study (FIESTA). Contraception. 2016;94(4):366–73.
Gaspard U et al. A multicenter, randomized, placebo-controlled study to select the minimum effective dose of estetrol in postmenopausal participants (E4Relief): part 2-vaginal cytology, genitourinary syndrome of menopause, and health-related quality of life. Menopause. 2023.
Seeger H, Hadji P, Mueck AO. Endogenous estradiol metabolites stimulate the in vitro proliferation of human osteoblastic cells. Int J Clin Pharmacol Ther. 2003;41(4):148–52.
Coelingh Bennink HJ, et al. Oral bioavailability and bone-sparing effects of estetrol in an osteoporosis model. Climacteric. 2008;11(Suppl 1):2–14.
Mawet M, et al. Unique effects on hepatic function, lipid metabolism, bone and growth endocrine parameters of estetrol in combined oral contraceptives. Eur J Contracept Reprod Health Care. 2015;20(6):463–75.
Coelingh Bennink HJT, et al. Pharmacodynamic effects of the fetal estrogen estetrol in postmenopausal women: results from a multiple-rising-dose study. Menopause. 2017;24(6):677–85.
Douxfils J, et al. Impact of estetrol (E4) on hemostasis, metabolism and bone turnover in postmenopausal women. Climacteric. 2022;26:1–9.
Coelingh Bennink HJT, et al. Estetrol cotreatment of androgen deprivation therapy in infiltrating or metastatic, castration-sensitive prostate cancer: a randomized, double-blind, phase II trial (PCombi). Eur Urol Open Sci. 2021;28:52–61.
Arnal JF, Bayard F. Vasculoprotective effects of oestrogens. Clin Exp Pharmacol Physiol. 2001;28(12):1032–4.
Wu Q, et al. Non-nuclear estrogen receptor signaling in the endothelium. J Biol Chem. 2011;286(17):14737–43.
Montt-Guevara MM, et al. Estetrol modulates endothelial nitric oxide synthesis in human endothelial cells. Front Endocrinol (Lausanne). 2015;6:111.
Yamazaki Y, Kondo Y, Kamiyama Y. Estimation of shear-stress-induced endothelial nitric oxide production from flow-mediated dilation. Annu Int Conf IEEE Eng Med Biol Soc. 2013;2013:4521–4.
Vanhoutte PM. Nitric Oxide: from good to bad. Ann Vasc Dis. 2018;11(1):41–51.
Vanhoutte PM, et al. Thirty years of saying NO: sources, fate, actions, and misfortunes of the endothelium-derived vasodilator mediator. Circ Res. 2016;119(2):375–96.
Guivarc'h E et al. Predominant role of nuclear versus membrane estrogen receptor alpha in arterial protection: implications for estrogen receptor alpha modulation in cardiovascular prevention/safety. J Am Heart Assoc. 2018:7(13).
Levine MG, Miodovnik M, Clark KE. Uterine vascular effects of estetrol in nonpregnant ewes. Am J Obstet Gynecol. 1984;148(6):735–8.
Hilgers RH, et al. Vasorelaxing effects of estetrol in rat arteries. J Endocrinol. 2012;215(1):97–106.
Davezac M, et al. The different natural estrogens promote endothelial healing through distinct cell targets. JCI Insight. 2023;8(5): e161284.
Dama A, et al. Regulation of human endothelial cell migration by oral contraceptive estrogen receptor ligands. Eur J Pharmacol. 2023;945: 175591.
Buscato M, et al. Estetrol prevents Western diet-induced obesity and atheroma independently of hepatic estrogen receptor alpha. Am J Physiol Endocrinol Metab. 2021;320(1):E19–29.
Smirnova NF, et al. The activation function-1 of estrogen receptor alpha prevents arterial neointima development through a direct effect on smooth muscle cells. Circ Res. 2015;117(9):770–8.
Gerard C, et al. Estetrol is a weak estrogen antagonizing estradiol-dependent mammary gland proliferation. J Endocrinol. 2015;224(1):85–95.
Liu S, et al. Oestetrol stimulates proliferation and oestrogen receptor expression in breast cancer cell lines: comparison of four oestrogens. Eur J Contracept Reprod Health Care. 2015;20(1):29–35.
Gerard C, et al. Combined estrogenic and anti-estrogenic properties of estetrol on breast cancer may provide a safe therapeutic window for the treatment of menopausal symptoms. Oncotarget. 2015;6(19):17621–36.
Gallez A, et al. Estetrol combined to progestogen for menopause or contraception indication is neutral on breast cancer. Cancers (Basel). 2021;13(10):2486.
Giretti MS, et al. Effects of estetrol on migration and invasion in T47-D breast cancer cells through the actin cytoskeleton. Front Endocrinol (Lausanne). 2014;5:80.
Singer CF, et al. Antiestrogenic effects of the fetal estrogen estetrol in women with estrogen-receptor positive early breast cancer. Carcinogenesis. 2014;35(11):2447–51.
Schmidt M, et al. Tumor suppression, dose-limiting toxicity and wellbeing with the fetal estrogen estetrol in patients with advanced breast cancer. J Cancer Res Clin Oncol. 2021;147(6):1833–42.
Klipping C, et al. Endocrine and metabolic effects of an oral contraceptive containing estetrol and drospirenone. Contraception. 2021;103(4):213–21.
Apter D, et al. Estetrol combined with drospirenone: an oral contraceptive with high acceptability, user satisfaction, well-being and favourable body weight control. Eur J Contracept Reprod Health Care. 2017;22(4):260–7.
Gemzell-Danielsson K, et al. A novel estetrol-containing combined oral contraceptive: European expert panel review. Eur J Contracept Reprod Health Care. 2022;27(5):373–83.
Odlind V, et al. Can changes in sex hormone binding globulin predict the risk of venous thromboembolism with combined oral contraceptive pills? Acta Obstet Gynecol Scand. 2002;81(6):482–90.
van Rooijen M, et al. Sex hormone-binding globulin–a surrogate marker for the prothrombic effects of combined oral contraceptives. Am J Obstet Gynecol. 2006;194(5):1499.
Hammond GL, et al. Estetrol does not bind sex hormone binding globulin or increase its production by human HepG2 cells. Climacteric. 2008;11(Suppl 1):41–6.
Douxfils J, et al. Evaluation of the effect of a new oral contraceptive containing estetrol and drospirenone on hemostasis parameters. Contraception. 2020;102(6):396–402.
Valera MC, et al. Effect of estetrol, a selective nuclear estrogen receptor modulator, in mouse models of arterial and venous thrombosis. Mol Cell Endocrinol. 2018;477:132–9.
Rosing J, et al. Oral contraceptives and venous thrombosis: different sensitivities to activated protein C in women using second- and third-generation oral contraceptives. Br J Haematol. 1997;97(1):233–8.
Douxfils J, et al. Validation and standardization of the ETP-based activated protein C resistance test for the clinical investigation of steroid contraceptives in women: an unmet clinical and regulatory need. Clin Chem Lab Med. 2020;58(2):294–305.
Hemker HC, et al. Calibrated automated thrombin generation measurement in clotting plasma. Pathophysiol Haemost Thromb. 2003;33(1):4–15.
Morimont L et al. Low thrombin generation in users of a contraceptive containing estetrol and drospirenone. J Clin Endocrinol Metab. 2022.
Chen MJ, et al. Tolerability and safety of the estetrol/drospirenone combined oral contraceptive: Pooled analysis of two multicenter, open-label phase 3 trials. Contraception. 2022;116:44–50.
Prossnitz ER, Barton M. Estrogen biology: new insights into GPER function and clinical opportunities. Mol Cell Endocrinol. 2014;389(1–2):71–83.
Wilkenfeld SR, Lin C, Frigo DE. Communication between genomic and non-genomic signaling events coordinate steroid hormone actions. Steroids. 2018;133:2–7.
Gerard C, et al. Profile of estetrol, a promising native estrogen for oral contraception and the relief of climacteric symptoms of menopause. Expert Rev Clin Pharmacol. 2022;15(2):121–37.
Abot A, et al. The AF-1 activation function of estrogen receptor alpha is necessary and sufficient for uterine epithelial cell proliferation in vivo. Endocrinology. 2013;154(6):2222–33.
Borjesson AE, et al. Roles of transactivating functions 1 and 2 of estrogen receptor-alpha in bone. Proc Natl Acad Sci USA. 2011;108(15):6288–93.
Handgraaf S, et al. Prevention of obesity and insulin resistance by estrogens requires ERalpha activation function-2 (ERalphaAF-2), whereas ERalphaAF-1 is dispensable. Diabetes. 2013;62(12):4098–108.
Jacquemetton J, et al. Analysis of genomic and non-genomic signaling of estrogen receptor in PDX models of breast cancer treated with a combination of the PI3K inhibitor alpelisib (BYL719) and fulvestrant. Breast Cancer Res. 2021;23(1):57.
Chiu JH, et al. Role of estrogen receptors and Src signaling in mechanisms of bone metastasis by estrogen receptor positive breast cancers. J Transl Med. 2017;15(1):97.
Yu L, et al. Src couples estrogen receptor to the anticipatory unfolded protein response and regulates cancer cell fate under stress. Biochim Biophys Acta Mol Cell Res. 2020;1867(10): 118765.
Song RX, et al. Linkage of rapid estrogen action to MAPK activation by ERalpha-Shc association and Shc pathway activation. Mol Endocrinol. 2002;16(1):116–27.
Faltas CL, LeBron KA, Holz MK. Unconventional estrogen signaling in health and disease. Endocrinology. 2020;161(4).
Ludwik KA, et al. ERalpha-mediated nuclear sequestration of RSK2 is required for ER(+) breast cancer tumorigenesis. Cancer Res. 2018;78(8):2014–25.
Bagot CN, et al. The effect of estrone on thrombin generation may explain the different thrombotic risk between oral and transdermal hormone replacement therapy. J Thromb Haemost. 2010;8(8):1736–44.
Canonico M, et al. Synergism between oral estrogen therapy and cytochrome P450 3A5*1 allele on the risk of venous thromboembolism among postmenopausal women. J Clin Endocrinol Metab. 2008;93(8):3082–7.
Pedram A, et al. Estrogen reduces lipid content in the liver exclusively from membrane receptor signaling. Sci Signal. 2013;6(276):ra36.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Funding provided by Estetra SRL (an affiliate company of Mithra Pharmaceuticals).
Conflicts of interest/Competing interests
CG is an employee of Estetra SRL (an affiliate company of Mithra Pharmaceuticals) and JMF is a member of the board at Mithra Pharmaceuticals.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Author’s contributions
CG and JMF equally contributed to the writing of the review.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Gérard, C., Foidart, JM. Estetrol: From Preclinical to Clinical Pharmacology and Advances in the Understanding of the Molecular Mechanism of Action. Drugs R D 23, 77–92 (2023). https://doi.org/10.1007/s40268-023-00419-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40268-023-00419-5