Abstract
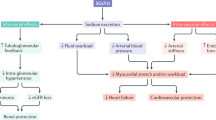
Diabetes mellitus (DM) is an increasingly prevalent condition that has a significant impact on health systems worldwide, particularly in older people. It is estimated that 30% of people aged > 65 years fulfil the diagnostic criteria for DM, with 90% having type 2 DM (T2DM). Generally, specific guidelines for the treatment of T2DM in older people address in a very limited manner the use of more recent therapies, such as sodium–glucose co-transporter-2 inhibitors (SGLT2i), which have important benefits for older people, such as a low risk of hypoglycemia, reduction of cardiovascular and renal risk, and an insulin-independent mechanism, allowing its use in disease of any duration. The SGLT2i class is well-tolerated, though some caution is also suggested, including adjustment of concomitant therapies, such as insulin and antihypertensives, especially loop diuretics. This review discusses the pathophysiological characteristics of the older patient with T2DM and evaluates the main benefits of and cautions for the use of SGLT2i in this population.
Similar content being viewed by others
References
Defronzo RA. Banting lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes. 2009;58(4):773–95.
International Diabetes Federation. IDF Diabetes Atlas, 9th edn. Brussels: 2019. http://www.diabetesatlas.org. Accessed 5 Sept 2019.
Chang AM, Halter JB. Aging and insulin secretion. Am J Physiol Endocrinol Metab. 2003;284(1):E7–12.
Sinclair AJ, Rodriguez-Mañas L. Diabetes and frailty: two converging conditions? Can J Diabetes. 2016;40:77–83.
Gæde P, Lund-Andersen H, Parving H-H, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med. 2008;358:580–91.
UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood–glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998;352(9131):854–65.
https://www.accessdata.fda.gov/scripts/cder/daf. Accessed 5 Sept 2019.
https://www.ema.europa.eu/en/medicines. Accessed 20 Aug 2019.
DeFronzo RA, Norton L, Abdul-Ghani M. Renal, metabolic and cardiovascular considerations of SGLT2 inhibition. Nat Rev Nephrol. 2016;13:11–26.
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–28.
Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–57.
Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347–57.
Fioretto P, Mansfield TA, Ptaszynska A, Yavin Y, Johnsson E, Parikh S. Long-term safety of dapagliflozin in older patients with type 2 diabetes mellitus: a pooled analysis of phase IIb/III studies. Drugs Aging. 2016;33(7):511–22.
Sinclair AJ, Bode B, Harris S, Vijapurkar U, Shaw W, Desai M, et al. Efficacy and safety of canagliflozin in individuals aged 75 and older with type 2 diabetes mellitus: a pooled analysis. J Am Geriatr Soc. 2016;64(3):543–52.
Cahn A, Wiviott S, Mosenzon O, Yanuv I, Rozenberg A, Murphy S, et al. Safety and efficacy of dapagliflozin in the elderly: analysis from the DECLARE TIMI 58 study. European Association for the Study of Diabetes Annual Scientific Session (EASD 2019), Barcelona, Spain, September 19, 2019.
Monteiro P, Bergenstal RM, Toural E, Inzucchi SE, Zinman B, Hantel S, et al. Efficacy and safety of empagliflozin in older patients in the EMPA-REG OUTCOME trial. Age Ageing. 2019;48(6):859–66.
Scheen AJ. Diabetes mellitus in the elderly: insulin resistance and/or impaired insulin secretion? Diabetes Metab. 2005; 31 Spec No 2:5S27-5S34. Review.
Kelley D, Mokan M, Veneman T. Impaired postprandial glucose utilization in non inulin-dependent diabetes mellitus. Metabolism. 1994;43(12):1549–57.
Mordarska K, Godziejewska-Zawada M. Diabetes in the elderly. Prz Menopauzalny. 2017;16(2):38–43.
Emerging Risk Factors Collaboration, Di Angelantonio E, Kaptoge S, Wormser D, Willeit P, Butterworth AS, et al. Association of cardiometabolic multimorbidity with mortality. JAMA. 2015;314:52.
Kasznicki J, Drzewoski J. Heart failure in the diabetic population—pathophysiology, diagnosis and management. Arch Med Sci. 2014;10(3):546.
Isfort M, Stevens SC, Schaffer S, Jong CJ, Wold LE. Metabolic dysfunction in diabetic cardiomyopathy. Heart Fail Rev. 2014;19(1):35–48.
Gerstein HC. The Hemoglobin A1c Level as a progressive risk factor for cardiovascular death, hospitalization for heart failure, or death in patients with chronic heart failure: an analysis of the Candesartan in Heart Failure: Assessment of Reduction in Mortality and Morbidity (CHARM) Program. Arch Intern Med. 2008;168:1699.
Heart Outcomes Prevention Evaluation (HOPE) Study Investigators. Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. Lancet. 2000;355:253–9.
Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345:861–9.
Silva-Palacios A, Königsberg M, Zazueta C. Nrf2 signaling and redox homeostasis in the aging heart: a potential target to prevent cardiovascular diseases? Ageing Res Rev. 2016;26:81–95.
Bolignano D, Mattace-Raso F, Sijbrands EJG, Zoccali C. The aging kidney revisited: a systematic review. Ageing Res Rev. 2014;14:65–80.
Sesti G, Antonelli Incalzi R, Bonora E, Consoli A, Giaccari A, Maggi S, et al. Management of diabetes in older adults. Nutr Metab Cardiovasc Dis. 2018;28:206–18.
Tahrani AA, Barnett AH, Bailey CJ. SGLT inhibitors in management of diabetes. Lancet Diabetes Endocrinol. 2013;1(2):140–51.
Miller EM. Elements for success in managing type 2 diabetes with SGLT-2 inhibitors: individualizing treatment with SGLT-2 inhibitor therapy in type 2 diabetes mellitus. J Fam Pract. 2017;66(2 Suppl):S13–6.
Cintra R, Moura FA, Carvalho LSF, Barreto J, Tambascia M, Pecoits-Filho R, et al. Inhibition of the sodium–glucose co-transporter 2 in the elderly: clinical and mechanistic insights into safety and efficacy. Rev Assoc Med Bras. 2019;65(1):70–86.
Bolinder J, Ljunggren Ö, Kullberg J, Johansson L, Wilding J, Langkilde AM, et al. Effects of dapagliflozin on body weight, total fat mass, and regional adipose tissue distribution in patients with type 2 diabetes mellitus with inadequate glycemic control on metformin. J Clin Endocrinol Metab. 2012;97(3):1020–31.
Bolinder J, Ljunggren Ö, Johansson L, Wilding J, Langkilde AM, Sjöström CD, et al. Dapagliflozin maintains glycaemic control while reducing weight and body fat mass over 2 years in patients with type 2 diabetes mellitus inadequately controlled on metformin. Diabetes Obes Metab. 2014;16(2):159–69.
Custodio JS Jr, Duraes AR, Abreu M, Albuquerque Rocha N, Roever L. SGLT2 inhibition and heart failure—current concepts. Heart Fail Rev. 2018;23:409–18.
Hirshberg B, Raz I. Impact of the US food and drug administration cardiovascular assessment requirements on the development of novel antidiabetes drugs. Diabetes Care. 2011;34:S101–6.
White WB, Cannon CP, Heller SR, Nissen SE, Bergenstal RM, Bakris GL, et al. Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N Engl J Med. 2013;369:1327–35.
Scirica BM, Bhatt DL, Braunwald E, Steg PG, Davidson J, Hirshberg B, et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med. 2013;369:1317–26.
Green JB, Bethel MA, Armstrong PW, Buse JB, Engel SS, Garg J, et al. Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015;373:232–42.
Wanner C, Inzucchi SE, Zinman B. Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med. 2016;375:1801–2.
McMurray JJV, DeMets DL, Inzucchi SE, Køber L, Kosiborod MN, Langkildeet AM, et al. The dapagliflozin and prevention of adverse-outcomes in heart failure (DAPA-HF) trial: baseline characteristics. Eur J Heart Fail. 2019;21(11):1402–11.
Verma S. Potential mechanisms of sodium–glucose co-transporter 2 inhibitor-related cardiovascular benefits. Am J Cardiol. 2019;124(Suppl 1):S36–44.
Muskiet MHA, Wheeler DC, Heerspink HJL. New pharmacological strategies for protecting kidney function in type 2 diabetes. Lancet Diabetes Endocrinol. 2019;7(5):397–412.
Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Bonaca MP, et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet. 2019;393:31–9.
Verma S, Jüni P, Mazer CD. Pump, pipes, and filter: do SGLT2 inhibitors cover it all? Lancet. 2019;393(10166):3–5.
Garber AJ, Abrahamson MJ, Barzilay JI, Blonde L, Bloomgarden ZT, Bush MA, et al. Consensus statement by the american association of clinical endocrinologists and american college of endocrinology on the comprehensive type 2 diabetes management algorithm—2019 EXECUTIVE SUMMARY. Endocr Pract. 2019;25(1):69–100.
Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41(2):255–323.
Davies MJ, D’Alessio DA, Fradkin J, Kernan W, Mathieu C, Mingrone G, et al. Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41(12):2669–701.
https://www.fda.gov/Drugs/DrugSafety/ucm617360.htm. Accessed Dec 2019.
Strotmeyer ES, Cauley JA, Schwartz AV, Nevitt MC, Resnick HE, Bauer DC, et al. Nontraumatic fracture risk with diabetes mellitus and impaired fasting glucose in older white and black adults: the health, aging, and body composition study. Arch Intern Med. 2005;165(14):1612–7.
Ljunggren Ö, Bolinder J, Johansson L, Wilding J, Langkilde AM, Sjöström CD, et al. Dapagliflozin has no effect on markers of bone formation and resorption or bone mineral density in patients with inadequately controlled type 2 diabetes mellitus on metformin. Diabetes Obes Metab. 2012;14(11):990–9.
Bilezikian JP, Watts NB, Usiskin K, Polidori D, Fung A, Sullivan D, et al. Evaluation of bone mineral density and bone biomarkers in patients with type 2 diabetes treated with canagliflozin. J Clin Endocrinol Metab. 2016;101(1):44–51.
Alba M, Xie J, Fung A, Desai M. The effects of canagliflozin, a sodium glucose co-transporter 2 inhibitor, on mineral metabolism and bone in patients with type 2 diabetes mellitus. Curr Med Res Opin. 2016;32(8):1375–85.
Watts NB, Bilezikian JP, Usiskin K, Edwards R, Desai M, Law G, et al. Effects of canagliflozin on fracture risk in patients with type 2 diabetes mellitus. J Clin Endocrinol Metab. 2016;101(1):157–66.
Bonaca M, Wiviott S, Zelniker T, Mosenzon O, Furtado RHM, Goodrich E, et al. Dapagliflozin and outcomes in patients with peripheral artery disease: insights from DECLARE—TIMI. American College of Cardiology Annual Scientific Session (ACC 2019), New Orleans, LA, March 18, 2019.
Rosenstock J, Ferrannini E. Euglycemic diabetic ketoacidosis: a predictable, detectable, and preventable safety concern with SGLT2 inhibitors. Diabetes Care. 2015;38(9):1638–42.
Handelsman Y, Henry RR, Bloomgarden ZT, Dagogo-Jack S, DeFronzo RA, Einhorn D, et al. American association of clinical endocrinologists and american college of endocrinology position statement on the association of SGLT-2 inhibitors and diabetic ketoacidosis. Endocr Pract. 2016;22(6):753–62.
Abdel-Kader K, Palevsky PM. Acute kidney injury in the elderly. Clin Geriatr Med. 2009;25(3):331–58.
Johnsson K, Johnsson E, Mansfield TA, Yavin Y, Ptaszynska A, Parikh SJ. Osmotic diuresis with SGLT2 inhibition: analysis of events related to volume reduction in dapagliflozin clinical trials. Postgrad Med. 2016;128(4):346–55.
Weber MA, Mansfield TA, Alessi F, Iqbal N, Parikh S, Ptaszynska A. Effects of dapagliflozin on blood pressure in hypertensive diabetic patients on renin-angiotensin system blockade. Blood Press. 2016;25(2):93–103.
Filippatos TD, Tsimihodimos V, Liamis G, Elisaf MS. SGLT2 inhibitors-induced electrolyte abnormalities: an analysis of the associated mechanisms. Diabetes Metab Syndr. 2018;12(1):59–63.
Mosenzon O, Wiviott SD, Cahn A, Rozenberg A, Yanuv I, Goodrich EL, et al. Effects of dapagliflozin on development and progression of kidney disease in patients with type 2 diabetes: an analysis from the DECLARE-TIMI 58 randomised trial. Lancet Diabetes Endocrinol. 2019;7(8):606–17.
Cherney DZ, Perkins BA, Soleymanlou N, Maione M, Lai V, Lee A, et al. Renal hemodynamic effect of sodium–glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation. 2014;129(5):587–97.
https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-strengthens-kidney-warnings-diabetes-medicines-canagliflozin Accessed Dec 2019.
LeRoith D, Biessels GJ, Braithwaite SS, Casanueva FF, Draznin B, Halter JB, et al. Treatment of diabetes in older adults: an Endocrine Society* Clinical Practice Guideline. J Clin Endocrinol Metab. 2019;104:1520–74.
American Diabetes Association. 12. older adults: standards of medical care in diabetes—2019. Diabetes Care. 2019;42(Suppl 1):S139–47.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–56.
Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 2012;16(7):601–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Funding for the preparation of this manuscript was received from AstraZeneca.
Conflict of interest
Joaquim Custódio has served as a speaker for AstraZeneca, Boehringer Ingelheim, and Eli Lilly. João Eduardo Nunes Salles has served as a speaker and has received consulting fees from Abbot, AstraZeneca, Boehringer Ingelheim, Eli Lilly, MSD, and Novo Nordisk. Jarbas Roriz has served as a speaker for AstraZeneca. Catarina Cavalcanti is an employee of AstraZeneca. Amanda Martins was a previous employee of AstraZeneca.
Rights and permissions
About this article
Cite this article
Custódio, J.S., Roriz-Filho, J., Cavalcanti, C.A.J. et al. Use of SGLT2 Inhibitors in Older Adults: Scientific Evidence and Practical Aspects. Drugs Aging 37, 399–409 (2020). https://doi.org/10.1007/s40266-020-00757-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-020-00757-y