Abstract
Background and Objective
Breast cancer patients treated with adriamycin-cyclophosphamide plus paclitaxel (AC-T) are often challenged with serious adverse effects for which no effective therapies are available. Here, we investigated whether metformin, an antidiabetic drug with additional pleiotropic effects could favourably offset AC-T induced toxicities.
Patients and Methods
Seventy non-diabetic breast cancer patients were randomised to receive either AC-T (adriamycin 60 mg/m2 + cyclophosphamide 600 mg/m2 × 4 cycles Q21 days, followed by weekly paclitaxel 80 mg/m2 × 12 cycles) alone or AC-T plus metformin (1700 mg/day). Patients were assessed regularly after each cycle to record the incidence and severity of adverse events based on the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI-CTCAE), version 5.0. Moreover, baseline echocardiography and ultrasonography were done and repeated after the end of neoadjuvant therapy.
Results
Addition of metformin to AC-T resulted in significantly less incidence and severity of peripheral neuropathy, oral mucositis, and fatigue (p < 0.05) compared to control arm. Moreover, the left ventricular ejection fraction (LVEF%) in the control arm dropped from a mean of 66.69 ± 4.57 to 62.2 ± 5.22% (p = 0.0004) versus a preserved cardiac function in the metformin arm (64.87 ± 4.84 to 65.94 ± 3.44%, p = 0.2667). Furthermore, fatty liver incidence was significantly lower in metformin compared with control arm (8.33% vs 51.85%, p = 0.001). By contrast, haematological disturbances caused by AC-T were preserved after concurrent metformin administration (p > 0.05).
Conclusion
Metformin offers a therapeutic opportunity for controlling toxicities caused by neoadjuvant chemotherapy in non-diabetic breast cancer patients.
Trial Registration
This randomised controlled trial was registered on November 20, 2019 in ClinicalTrials.gov under registration number: NCT04170465.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Metformin reduces the incidence and severity of AC-T-evoked peripheral neuropathy, oral mucositis, fatigue, and cardiac and hepatic complications. |
Haematological and gastrointestinal complications of AC-T therapy are preserved following metformin administration. |
1 Introduction
Breast cancer (BC) is the most common type of cancer encountered in females in Egypt and worldwide. In 2020, the International Agency for Research on Cancer GLOBOCAN 2020 reported that the prevalence of BC in Egypt was 121 per 100,000 Egyptian females [1]. Although chemotherapy is fundamental in the management of BC, the erupting adverse events (AEs) sometimes necessitate the interruption of therapy and mandate the use of less effective regimens [2,3,4]. Adriamycin (doxorubicin) combined with cyclophosphamide, followed by weekly paclitaxel (i.e., AC-T) regimen is commonly used in Egypt in the neoadjuvant and adjuvant treatment of BC [5, 6]. A frequently reported AE encountered in paclitaxel-treated patients is peripheral neuropathy [7]. Paclitaxel-induced peripheral neuropathy (PIPN) affects the quality of life of patients, and is also a dose-limiting adverse effect that can impede cancer therapy and affect cancer prognosis [8, 9]. Oral mucositis is another common toxicity of AC-T regimen that appears in 77% of patients [3, 10]. The combination of doxorubicin and cyclophosphamide causes a 3-fold increase in the risk of oral mucositis compared to individual drugs [11]. Oral mucositis reduces food intake and body immunity, making patients more liable to life-threatening systemic infections [12]. The AC-T regimen causes distressful fatigue in almost all BC patients, which is not relieved by rest [3, 13]. Cardiotoxicity is a major life-threatening AE of doxorubicin, which can progress to irreversible congestive heart failure [4]. Additionally, chemotherapy induces hepatic steatosis as a result of the oxidative stress generated in hepatocytes, which if left untreated, can progress to steatohepatitis and hepatocytes degeneration [14]. Among chemotherapeutic regimens used in BC treatment, the AC-T regimen accounts for more than 50% of fatty liver cases [2, 14].
To date, no effective pharmacologic therapies have been identified to prevent or treat the above-mentioned devastating chemotherapy-induced toxicities. Management of PIPN is limited to symptomatic treatment with pain killers [8]. Numerous medications have been proposed for chemotherapy-induced oral mucositis, but not one has proven completely beneficial [15]. Additionally, no current therapies have proven effective in alleviating cancer-related fatigue [16, 17]. On the other hand, dexrazoxane has been the only FDA-approved cardioprotective agent against doxorubicin-induced cardiotoxicity. However, its use has been limited because of increased incidence of secondary malignancies and reduced anti-tumour efficacy of doxorubicin [18, 19]. Lifestyle interventions such as exercise and a healthy low-fat diet can lower the incidence of non-alcoholic fatty liver disease (NAFLD) [20].
The antidiabetic drug metformin has been shown to favourably reprogramme molecular and cellular pathways that arbitrate the clinical presentation of several diseases including cancer [21,22,23]. Such advantageous actions of metformin are largely attributed to the upregulation of adenosine monophosphate-activated protein kinase (AMPK) and consequent interruption of downstream inflammatory and antioxidative cascades [21, 22]. Oncology research has established antitumor benefits for metformin including its ability to reduce metastasis risk, facilitate chemotherapy efficacy, and improve patient survivability, and clinical and pathologic outcomes [24,25,26,27,28,29]. However, little or no information is available to date regarding whether metformin could protect or at least minimise the troublesome sequels of AC-T chemotherapy. In the current randomised clinical trial, we tested the hypothesis that the simultaneous administration of metformin rectifies the AEs caused by the neoadjuvant AC-T regimen in chemotherapy-naïve non-diabetic BC patients.
2 Materials and Methods
2.1 Study Design and Participants
This is a multicentre randomised controlled trial conducted at the Medical Research Institute and Alexandria Main University Hospital, Alexandria University, Egypt. Institutional ethical approvals by Alexandria University (IRB no. 00012098), and Damanhour University (IRB no. 919PP18) were obtained before commencement of the study. The study was conducted in compliance with the Declaration of Helsinki. All study participants provided a written informed consent. This study is a part of the METNEO study registered in ClinicalTrials.gov under registration number: NCT04170465 (https://clinicaltrials.gov/ct2/show/NCT04170465).
Patients were eligible if they were aged 18–65 years, candidates for neoadjuvant chemotherapy, received no prior chemotherapy, and had baseline left ventricular ejection fraction (LVEF) greater than 50%, normal liver functions, and Eastern Cooperative Oncology Group Performance Status (ECOG-PS) from zero to two. Patients with diabetes, history of anti-diabetic medication use, pregnancy, breastfeeding, metastatic or recurrent breast cancer, or increased risk of metformin-induced lactic acidosis, such as those with heart failure or estimated glomerular filtration rate (eGFR) ≤ 45 mL/min/1.73 m2 were excluded from the study. Fasting blood glucose level test was done for patients with no history of diabetes to make sure they were not underdiagnosed and were eligible for participation in the study. Also, baseline LVEF%, renal and liver function, and complete blood count with differentials were determined.
Eligible patients were randomised in a 1:1 ratio to either metformin or control arms using blocked randomisation with random block sizes of two, four, and six. The randomisation scheme was generated by using the website “http://www.randomization.com”. Allocation to either arm was concealed using sealed numbered envelopes by an independent third-party individual. The control arm received AC-T chemotherapy 16 cycles protocol (i.e., doxorubicin 60 mg/m2 slow intravenous [IV] push over 10–15 min and cyclophosphamide 600 mg/m2 IV infusion over 1 h every 21 days for a total of four cycles followed by paclitaxel 80 mg/m2 IV infusion over 1 h every week for a total of 12 cycles). The metformin arm received the same chemotherapy protocol in addition to oral metformin 850 mg once daily for 1 week followed by 850 mg twice a day during the entire neoadjuvant treatment period and stopped metformin only 3–7 days before surgery. Metformin was slowly titrated and was prescribed with meals to reduce the incidence of associated gastrointestinal (GI) side effects. Moreover, vitamin B12 was supplemented to study participants when peripheral neuropathy symptoms develop in both metformin and control arms.
Patients were interviewed in person and data about birthdate, weight, height, ECOG-PS, menopausal status, history of gestation, pregnancy and abortion, breastfeeding, method of contraception, other comorbidities, and family history were collected.
2.2 Monitoring for Adverse Events
Complete blood picture with differentials was obtained, and patients were monitored for the incidence of haematological side effects (i.e., anaemia, thrombocytopenia, neutropenia, and febrile neutropenia) before each of the 16 cycles. Also, non-haematological side effects (i.e., fatigue, nausea, vomiting, diarrhoea, constipation, oral mucositis, and peripheral sensory neuropathy) were monitored after each chemotherapy session during the whole treatment period. At baseline, echocardiography and ultrasonography for abdomen and pelvis were done. Moreover, renal and liver function tests were assessed before each cycle.
Before the commencement of neoadjuvant therapy, patients were interviewed in person and patient education about the proper measures for preventing and self-management of oral mucositis was provided equally in both arms. After each chemotherapy session, each participant was assessed within the first week and again after 18–21 days from the session by an independent physician and the study investigator by telephone or face to face. Patients were assessed for the occurrence of any AE based on the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI-CTCAE) version 5.0 [30], using an assessment form extracted from the NCI-CTCAE v.5 that contains the CTCAE terms for the studied AEs and their severity grades from 1 to 5 with a checkbox underneath each grade, and a key providing the definitions for the AEs and the corresponding severity grades (Electronic supplementary file 1). Moreover, echocardiography and ultrasonography were repeated after completing treatment, to assess the state of the patient before surgery. The haematological toxicities, cardiotoxicity, and hepatotoxicity were assessed by a blind investigator.
2.3 Statistical Analysis
All statistical analyses were performed using Stata version 14.2. For interval variables, Shapiro–Wilk test was used to inspect data normality, Levene’s test was used to check equality of variances between arms, followed by the two-sided two-sample independent t test with equal or unequal variances, which was used as appropriate to test for differences between treatment arms. Pearson’s Chi-square, or Fisher’s exact tests were used as appropriate for categorical variables. To detect the difference in the severity grades of different AEs (i.e., peripheral neuropathy, oral mucositis, fatigue, gastrointestinal, and haematological adverse effects) between the two arms at each time point, the Mann–Whitney U test was used, and data were expressed as frequencies and percentages of occurrence of different severity grades. Then ordered logistic regression was performed to detect the effect size of treatment per cycle, and the odds ratio (OR) with its 95% confidence intervals (CI) was reported. On the other hand, the paired t test was used to compare pre-treatment to post-treatment values of LVEF% in each arm, and data were expressed as means ± SD, then the multiple linear regression was performed to detect the effect size of metformin and baseline LVEF% on post-treatment LVEF% values, and the β-coefficient with its 95% CIs was reported. Binary logistic regression was used to estimate the effect size of metformin treatment and other parameters on fatty liver development, and the OR with its 95% CIs was reported. Two-sided p values of < 0.05 were considered significant. The sample size was estimated based on a previous study [31], in which 60 patients (i.e., 30 per arm) were needed to detect a change in the incidence of peripheral neuropathy using Chi-square test with an alpha error of 5%, a beta error of 10%, and a 20% drop-out rate. As indicated above, peripheral neuropathy is one of the most common toxicities encountered in BC patients treated with AC-T chemotherapy [32, 33].
3 Results
3.1 Patients’ Demographics and Tumour Characteristics
Between November 2019 and February 2021, 663 patients with biopsy-proven BC were screened for eligibility to participate in the study. Of these, 586 patients did not meet the inclusion criteria and 7 patients refused to participate. Seventy patients met the eligibility criteria and were randomised to either metformin or control arms in a 1:1 ratio. All patients were assessed for study outcomes. The CONSORT diagram summarises the study flow (Fig. 1).
Patient and tumour characteristics are summarised in Table 1. Patients in both metformin and control arms showed similar baseline characteristics. Most females were aged < 40 years and were premenopausal (68.57% and 71.43%, respectively). Most patients were obese, representing 67.14% of participants. Most patients (67.14%) had no family history of BC. Moreover, the luminal molecular subtype (65.71%) and clinical prognostic stage of IIIB (44.29%) were more prevalent among patients.
3.2 Adverse Events
The frequency and proportion of AEs during the whole treatment period were summarised in Table 2. No AE-related deaths (i.e., grade 5) were observed during the entire study. The most frequently occurring AEs observed were anaemia, fatigue, neutropenia, peripheral sensory neuropathy, oral mucositis, nausea, and diarrhoea (Table 2). Most AEs were of grades 1 and 2. The metformin arm showed a lower incidence and severity of fatigue, oral mucositis, and peripheral neuropathy (Electronic supplementary file 2, Fig. 1). On the other hand, no significant differences were observed between the two arms in diarrhoea, constipation, nausea, vomiting, anaemia, thrombocytopenia, neutropenia, and febrile neutropenia.
3.2.1 Effect of Metformin on Peripheral Neuropathy
Peripheral neuropathy is a common AE encountered with paclitaxel therapy. As shown in Fig. 2, the incidence of peripheral neuropathy was minimal and approximately similar in the 2 arms during the 4 AC cycles. Discrepancies started to appear after the first paclitaxel cycle. An intriguing finding of this study was that metformin significantly reduced the odds of peripheral neuropathy during paclitaxel cycles 4 to 12, respectively, as illustrated in Table 3 (see Electronic supplementary file 3 for additional information).
Incidence of different Common Terminology Criteria for Adverse Events (CTCAE) grades of peripheral neuropathy by cycle between metformin and control arms experienced during neoadjuvant therapy. Data are expressed as percentages of frequencies of incident events of 35 observations in each arm. AC adriamycin-cyclophosphamide cycle, CI confidence interval, G grade of severity, OR odds ratio, Tw paclitaxel weekly cycle. *p value < 0.05 versus control values
3.2.2 Effect of Metformin on Oral Mucositis
The incidence and severity of oral mucositis was lower in the metformin arm compared to the control arm throughout the whole treatment period as shown in Fig. 3. During the doxorubicin-cyclophosphamide cycles, metformin significantly reduced the odds of oral mucositis (Table 3). Moreover, patients in the control arm experienced oral mucositis with higher frequencies and grades of severity compared to those in the metformin arm during the following 12 paclitaxel cycles, where the likelihood of oral mucositis in the metformin arm was significantly reduced (Table 3) (see Electronic supplementary file 3 for additional information).
Incidence of different Common Terminology Criteria for Adverse Events (CTCAE) grades of oral mucositis by cycle between metformin and control arms experienced during neoadjuvant therapy. Data are expressed as percentages of frequencies of incident events of 35 observations in each arm. AC adriamycin-cyclophosphamide cycle, CI confidence interval, G grade of severity, OR odds ratio, Tw paclitaxel weekly cycle. *p value < 0.05 versus control values
3.2.3 Effect of Metformin on Fatigue
The incidence of fatigue in all study participants was higher during the first 4 AC cycles, than with paclitaxel cycles. Nevertheless, patients in the metformin arm experienced less fatigue during the whole treatment period (Fig. 4). The difference in fatigue severity grades between arms during the 4 AC cycles did not reach statistical significance. However, during the following paclitaxel cycles there was a significant reduction in the odds of fatigue observed in metformin arm in cycles 1–5, and 8–10 (Table 3) (see Electronic supplementary file 3 for additional information).
Incidence of different Common Terminology Criteria for Adverse Events (CTCAE) grades of fatigue by cycle between metformin and control arms experienced during neoadjuvant therapy. Data are expressed as percentages of frequencies of incident events of 35 observations in each arm. AC adriamycin-cyclophosphamide cycle, CI confidence interval, G grade of severity, OR odds ratio, Tw paclitaxel weekly cycle. *p value < 0.05 versus control values
3.2.4 Effect of Metformin on AC-T-Induced Cardiotoxicity
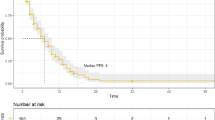
Echocardiography test was done for all patients before the initiation of therapy, and again after the last chemotherapy cycle, right before surgery. At baseline, there was no significant difference in the LVEF% between either arm (mean ± SD [95% CI]: 66.69 ± 4.57% [65.12– 68.25] vs 64.87 ± 4.84% [63.21–66.53] in the control and metformin arms, respectively [p = 0.1115]). However, post-treatment LVEF% differed significantly between arms (62.2 ± 5.22% [60.41– 63.99] vs 65.94 ± 3.44% [64.76–67.12] in control and metformin arms, respectively [p = 0.0007]).
The LVEF% of control arm, as expected with chemotherapy, tended to decrease and this reduction was found to be significant when a paired t test was performed (p = 0.0004). On the other hand, the mean LVEF% did not significantly change in metformin arm (p = 0.2667) (Electronic supplementary file 2, Fig. 2). Interestingly, metformin could preserve the cardiac function and protect against AC-T-induced cardiotoxicity, with a predicted increase of 3.88 units in LVEF% (β = 3.878 ± 1.082 [1.719– 6.037], p = 0.001) with metformin ingestion compared to control patients. Moreover, baseline LVEF% value had no impact on post-treatment values (β = 0.074 ± 0.114 [− 0.154 to 0.303], p = 0.518).
3.2.5 Effect of Metformin on Hepatotoxicity
All patients were evaluated by ultrasonography for fatty liver at baseline and after chemotherapy. The frequency of fatty liver in the control arm at baseline was 22.86% (n = 8), compared to 31.43% (n = 11) in the metformin arm. No significant difference was found at baseline (p = 0.420). After completion of therapy, ultrasonography showed a significant reduction (p < 0.0001) in the frequency of fatty liver in the metformin arm (n = 6, 17.14%) compared to the control arm (n = 21, 60.00%), which was approximately tripled (Electronic supplementary file 4, Fig. 3a and Table 2). In univariate analysis, only metformin ingestion, patients’ age, pre-existing fatty liver disease, and obesity (BMI > 30 kg/m2), had significant influence (p < 0.05) on development of chemotherapy-induced fatty liver. However, when multivariate analysis was performed, patients with history of fatty liver had approximately 6 times the likelihood for developing AC-T-induced fatty liver (OR: 5.67 [1.19–26.98], p = 0.029), and those taking metformin had 92% protection from fatty liver development (adjusted OR: 0.08 [0.02–0.33], p < 0.0001) (Electronic supplementary file 4, Table 3).
Moreover, when limiting the analysis on patients with no pre-existing fatty liver in control (n = 27) and metformin (n = 24) arms, 14 patients (51.85%) in the control arm developed fatty liver after neoadjuvant treatment, compared to only 2 patients (8.33%) in the metformin arm (p = 0.001) (Electronic supplementary file 4, Fig. 3b and Table 2). In univariate analysis, the effect of metformin on the development of fatty liver was the only significant factor (OR: 0.08 [0.02–0.43], p = 0.003).
3.2.6 Effect of Metformin on Other Gastrointestinal AEs
No significant differences were observed in the incidence or severity of diarrhoea, constipation, nausea, and vomiting between either arm. Diarrhoea tended to increase in the metformin arm; however, this increase was not significant. Also, vomiting tends to non-significantly increase in the metformin arm during AC cycles II, III, and IV (Electronic supplementary file 5).
3.2.7 Effect of Metformin on Haematological AEs
In our study population, haematological AEs such as anaemia, neutropenia, febrile neutropenia, and thrombocytopenia were similarly demonstrated in both arms (Electronic supplementary file 6). No thrombocytopenia was observed in participants. Grade I and II anaemia was the most common haematological toxicity, followed by grades I and II neutropenia. While febrile neutropenia was a rare event (Table 2).
4 Discussion
Chemotherapy-induced toxicities remain a major problem in the management of BC. In the present study, we investigated whether metformin would protect against these toxicities in non-diabetic BC patients receiving neoadjuvant AC-T chemotherapy. This is the first randomised controlled trial to endorse a protective effect of metformin on PIPN, oral mucositis, fatigue, cardiotoxicity, and hepatotoxicity induced by AC-T chemotherapy regimen.
An intriguing finding of our study is the ability of metformin to protect against peripheral neuropathy induced by the AC-T regimen. The paclitaxel component of the AC-T regimen is often blamed for the evoked neuropathy response, possibly due to the disruption of the assembly of neuron microtubules, and subsequent impairment in axonal transport and neuronal functions [34]. Considering the debilitating effects of peripheral neuropathy on sensory and motor functions [35], the improvement of PIPN by metformin is expected to warrant a better post-treatment quality of life for BC patients. Remarkably, the anti-neuropathic action of metformin is unlikely to be linked to its antidiabetic effect and is mostly reported in preclinical studies [36,37,38,39,40]. Metformin displays an anti-neuroinflammatory effect in spinal cord-injured rats comparable to that of minocycline, the tetracycline antibiotic with potent neuroprotective properties [41]. In another in vivo study, metformin reverses the structural brain plasticity that accompany neuropathic pain [42]. In one clinical study undertaken in patients with stage III colorectal cancer, metformin was found to reduce peripheral neuropathy induced by oxaliplatin [43]. The present study is therefore the first randomised controlled study to report on the protective effect of metformin against peripheral neuropathy caused by AC-T in non-diabetic BC patients.
Another fascinating finding of our study is that the metformin arm had significantly lower incidence of and less severe oral mucositis during the entire neoadjuvant treatment period. Oral mucositis is a well-known AE of chemotherapy, in which the generation of reactive oxygen species (ROS) produces DNA damage and subsequent basal epithelial cell death in the oral mucosa [44]. The protective effect of metformin against oral mucositis caused by AC-T chemotherapy regimen, has not been investigated in preclinical or clinical settings. That said, a promising therapeutic potential for metformin in mucosal protection and regeneration has been demonstrated only in preclinical studies such as: (i) metformin administration before indomethacin inhibits the development of gastric ulcer in rats [45], (ii) metformin heals indomethacin-induced gastric ulcer in rats in a way comparable to the proton pump inhibitor omeprazole [46], (iii) topical hydrogel preparation of metformin hydrochloride effectively promotes wound healing and re-epithelisation [47], (iv) metformin off-sets radiotherapy-induced mucositis [48], and metformin protects against 5-fluorouracil-induced oral mucositis in mice via reducing endoplasmic reticulum stress [49]. The current clinical study, therefore, is the first to authenticate the protective effect of metformin against AC-T-induced oral mucositis in BC patients.
Adriamycin treatment induces skeletal muscle loss and consequent fatigue and decreased quality of life [50, 51]. Several studies demonstrated no additional benefit for adding metformin to adriamycin therapy in terms of skeletal muscle protection [52,53,54]. This observation was in line with our findings, where we found no privileged effect for metformin on fatigue during the four adriamycin-cyclophosphamide (AC) chemotherapy cycles. By contrast, during paclitaxel chemotherapy sessions we found that the simultaneous treatment with metformin clearly diminished in the incidence and severity of fatigue. While no data are available in the literature regarding the effect of metformin on AC-T regimen-related fatigue, a recent clinical study conducted on patients with stage IV non-small cell lung cancer receiving immune-checkpoint inhibitors revealed significantly less fatigue upon co-administration of metformin [55]. As fatigue has traditionally been associated with paclitaxel therapy [56, 57], the current data are the first to highlight that metformin conceivably reduces the heightened risk of fatigue incited by paclitaxel in non-diabetic BC patients.
Despite the high efficacy of adriamycin and related anthracyclines as anticancer agents in solid tumours, their cumulative and dose-dependent cardiotoxicity remains one of the most devastating consequences when used alone [58], or combined with cyclophosphamide plus paclitaxel [59]. The cardiotoxic influences of adriamycin such as myocardial morphological damage, cardiomyopathy, and congestive heart failure could necessitate cardiac transplantation or have fatal consequences [58]. The overproduction of ROS has been largely blamed for the cardiotoxicity of adriamycin, but other proposed mechanisms include mitochondrial dysfunction, disruption of Ca2+ homeostasis, and upregulated apoptosis [60]. Previous preclinical studies have revealed a cardioprotective action for metformin against adriamycin cardiotoxicity [61, 62]. Such an advantageous effect of metformin was mimicked in a single clinical study against radiation-induced cardiotoxicity in diabetic BC patients [63]. Importantly, the current clinical study is the first to establish an effective cardioprotective action for metformin in non-diabetic BC women receiving AC-T neoadjuvant chemotherapy. This view is validated by the observation that the significant drop in the LVEF% caused by AC-T regimen in the control arm was nullified after concurrent administration of metformin.
Non-alcoholic fatty liver disease has always been linked to obesity, insulin resistance, and type 2 diabetes mellitus [64]. Clinical studies have indicated a beneficial action for metformin on NAFLD in diabetic and nondiabetic patients and the effect of metformin surpassed the improvement produced by lifestyle interventions, the only available interventional option for NAFLD [20, 65, 66]. The risk of developing fatty liver during chemotherapy in BC patients has not been properly studied and knowledge on the exact molecular mechanisms for AC-T protocol-induced fatty liver is scarce [2, 67]. Izadpanahi et al, showed that AC-T chemotherapy leads to the development of fatty liver in more than half of BC patients [2], through a mechanism that mainly involves mitochondrial dysfunction [68]. In the present study, 31% of all participants who had no fatty liver at baseline, developed fatty liver after AC-T administration. More importantly, the decreased proportion of fatty liver in the metformin arm points to a protective effect for metformin against chemotherapy-induced hepatotoxicity. It is worth noting that the recruitment of nondiabetic patients and the equal distribution of obese individuals in the two arms of the study (p = 0.799) made comparisons between both arms reliable.
The present study data revealed that signs of GI toxicity induced by AC-T regimen, such as diarrhoea and constipation, were still manifest in the metformin arm. This is consistent with earlier reports in which metformin failed to relieve episodes of diarrhoea caused by chemotherapeutic drugs such as 5-fluorouracil and irinotecan [69, 70]. Notwithstanding, a protective effect of metformin against diarrhoea provoked by abdominal radiotherapy has been recently reported [71]. Such discrepancy in metformin effects might relate to the specific anticancer therapy employed, chemotherapy versus radiotherapy. In fact, differences in the magnitude/nature of intestinal lesions induced by the two therapies and predisposing cellular mechanisms have been described [72, 73]. Additionally, a protective effect for metformin against 5-fluorouracil-induced diarrhoea has been reported [74], but this study was conducted in mice and employed a shorter period of therapy with metformin and 5-fluorouracil. It should be remembered that in addition to the specific anticancer intervention utilised, other factors may contribute to gastrointestinal upsets in cancer patients such as dietary habits, exercise, infection, anxiety and psychological distress [75]. In the present investigation, we attempted to limit the impact of these distractors and reduce the incidence of gastrointestinal anomalies by gradual escalation of the metformin dose and randomly assigning patients to the two arms of the study.
4.1 Limitations
This study was an open-label randomised controlled study. However, the implementation of allocation concealment and the blind outcome assessment for haematological toxicity, cardiotoxicity and hepatotoxicity may have reduced bias in the estimated effect of treatment. Also, results may have been reinforced by measuring specific confirmatory biomarkers for AC-T-induced toxicities.
5 Conclusion
The data suggest a multitude of beneficial effects for metformin when co-administered with AC-T chemotherapy in BC patients. Metformin reduces the incidence and severity of serious toxicities typically associated with AC-T use, namely PIPN, oral mucositis, fatigue, cardiotoxicity, and hepatotoxicity. This contrasts with haematological and gastrointestinal toxicities of the AC-T regimen that are preserved following metformin administration. Undertaking the study in a population of non-diabetic patients argues against the dependence of the metformin effects on the diabetic state. Moreover, the random assignment of patients to the control and metformin regimens eliminates the influence of confounders that could have affected the outcome of the study. Notably, further large-scale double-blind randomised controlled studies are needed to reinforce the protective effect of metformin against the harmful actions caused by AC-T chemotherapy or likely other chemotherapeutic protocols.
References
Ferlay J , E.M., Lam F, Colombet M, Mery L, Piñeros M, Znaor A, Soerjomataram I, Bray F. Global cancer observatory: cancer today. 2020 [cited 2021 August 29]. https://gco.iarc.fr/today. Accessed 29 Aug 2021.
Izadpanahi P, et al. Effect of chemotherapy on fatty liver occurrence in breast and gastrointestinal cancer patients: a case-controlled study. Hepatitis Mon. 2020;20(3): e97986.
Gadisa DA, et al. Toxicity profile of doxorubicin-cyclophosphamide and doxorubicin-cyclophosphamide followed by paclitaxel regimen and its associated factors among women with breast cancer in Ethiopia: a prospective cohort study. J Oncol Pharm Pract. 2020;26(8):1912–20.
Smith LA, et al. Cardiotoxicity of anthracycline agents for the treatment of cancer: systematic review and meta-analysis of randomised controlled trials. BMC Cancer. 2010;10(1):1–14.
El-Haggar SM, et al. Metformin may protect nondiabetic breast cancer women from metastasis. Clin Exp Metas. 2016;33(4):339–57.
El-khayat SM, et al. The effect of metformin when combined with neoadjuvant chemotherapy in breast cancer patients. Med Oncol. 2021;39(1):1.
Klein I, Lehmann HC. Pathomechanisms of paclitaxel-induced peripheral neuropathy. Toxics. 2021;9(10):229.
Leen AJ, et al. A systematic review and meta-analysis of the effectiveness of neuroprotectants for paclitaxel-induced peripheral neuropathy. Front Oncol. 2021;11: 763229.
Mols F, et al. Chemotherapy-induced peripheral neuropathy and its association with quality of life: a systematic review. Support Care Cancer. 2014;22(8):2261–9.
Menezes BC, et al. Laser therapy as a preventive approach for oral mucositis in cancer patients undergoing chemotherapy: the potential role of superoxide dismutase. Asian Pac J Cancer Prev. 2021;22(10):3211–7.
Raber-Durlacher JE, et al. Oral mucositis in patients treated with chemotherapy for solid tumors: a retrospective analysis of 150 cases. Support Care Cancer. 2000;8(5):366–71.
Raber-Durlacher JE. Current practices for management of oral mucositis in cancer patients. Support Care Cancer. 1999;7(2):71–4.
Glaus A, Crow R, Hammond S. A qualitative study to explore the concept of fatigue/tiredness in cancer patients and in healthy individuals. Support Care Cancer. 1996;4(2):82–96.
Sharma A, et al. Chemotherapy induced liver abnormalities: an imaging perspective. Clin Mol Hepatol. 2014;20(3):317–26.
ArbabiSarjou A, et al. The effect of self-care training on the severity of oral mucositis in breast cancer patients undergoing chemotherapy. Med Surg Nurs J. 2021;10(4): e123386.
Thong MSY, et al. Cancer-related fatigue: causes and current treatment options. Curr Treat Options Oncol. 2020;21(2):17.
Soones T, Ombres R, Escalante C. An update on cancer-related fatigue in older adults: a narrative review. Journal of Geriatric Oncology. 2022;13(2):125–31.
Pai VB, Nahata MC. Cardiotoxicity of chemotherapeutic agents. Drug Saf. 2000;22(4):263–302.
van Dalen EC, et al. Cardioprotective interventions for cancer patients receiving anthracyclines. Cochrane Database Syst Rev. 2011;2011(6):Cd003917.
Chalasani N, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328–57.
Zhou G, et al. Role of AMP-activated protein kinase in mechanism of metformin action. J Clin Investig. 2001;108(8):1167–74.
Ala M, Ala M. Metformin for cardiovascular protection, inflammatory bowel disease, osteoporosis, periodontitis, polycystic ovarian syndrome, neurodegeneration, cancer, inflammation and senescence: what is next? ACS Pharmacol Transl Sci. 2021;4(6):1747–70.
Lv Z, Guo Y. Metformin and its benefits for various diseases. Front Endocrinol. 2020;11:191.
Jiralerspong S, et al. Metformin and pathologic complete responses to neoadjuvant chemotherapy in diabetic patients with breast cancer. J Clin Oncol. 2009;27(20):3297–302.
Kim HJ, et al. Metformin increases survival in hormone receptor-positive, HER2-positive breast cancer patients with diabetes. Breast Cancer Res. 2015;17(1):64.
Jacob L, et al. Impact of metformin on metastases in patients with breast cancer and type 2 diabetes. J Diabetes Complications. 2016;30(6):1056–9.
Shafiei-Irannejad V, et al. Metformin enhances doxorubicin sensitivity via inhibition of doxorubicin efflux in P-gp-overexpressing MCF-7 cells. Chem Biol Drug Des. 2018;91(1):269–76.
El-Ashmawy NE, et al. Metformin augments doxorubicin cytotoxicity in mammary carcinoma through activation of adenosine monophosphate protein kinase pathway. Tumor Biol. 2017;39(5):1010428317692235.
Yam C, et al. Efficacy and safety of the combination of metformin, everolimus and exemestane in overweight and obese postmenopausal patients with metastatic, hormone receptor-positive, HER2-negative breast cancer: a phase II study. Investig New Drugs. 2019;37(2):345–51.
Common Terminology Criteria for Adverse Events (CTCAE) v5.0. 2017 [cited 2019 October 14]. https://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/CTCAE_v5_Quick_Reference_8.5x11.pdf. Accessed 14 Oct 2019.
Argyriou AA, et al. Preventing paclitaxel-induced peripheral neuropathy: a phase II trial of vitamin E supplementation. J Pain Symptom Manag. 2006;32(3):237–44.
Yardley DA, et al. TITAN: phase III study of doxorubicin/cyclophosphamide followed by ixabepilone or paclitaxel in early-stage triple-negative breast cancer. Breast Cancer Res Treat. 2017;164(3):649–58.
Sparano JA, et al. Weekly paclitaxel in the adjuvant treatment of breast cancer. N Engl J Med. 2008;358(16):1663–71.
Scripture CD, Figg WD, Sparreboom A. Peripheral neuropathy induced by paclitaxel: recent insights and future perspectives. Curr Neuropharmacol. 2006;4(2):165–72.
Pachman D, et al. Chemotherapy-induced peripheral neuropathy: prevention and treatment. Clin Pharmacol Ther. 2011;90(3):377–87.
Koo BK. Metformin preserves peripheral nerve damage with comparable effects to alpha lipoic acid in streptozotocin/high-fat diet induced diabetic rats (Diabetes Metab J 2020;44:842–53). Diabetes Metab J. 2021;45(1):125–6.
Hacimuftuoglu A, et al. The analgesic effect of metformin on paclitaxel-induced neuropathic pain model in rats: by considering pathological results. J Cancer Res Ther. 2020;16(1):34–9.
Mao-Ying Q-L, et al. The anti-diabetic drug metformin protects against chemotherapy-induced peripheral neuropathy in a mouse model. PLoS ONE. 2014;9(6): e100701.
Inyang KE, et al. Alleviation of paclitaxel-induced mechanical hypersensitivity and hyperalgesic priming with AMPK activators in male and female mice. Neurobiol Pain. 2019;6: 100037.
Ludman T, Melemedjian OK. Bortezomib and metformin opposingly regulate the expression of hypoxia-inducible factor alpha and the consequent development of chemotherapy-induced painful peripheral neuropathy. Mol Pain. 2019;15:1744806919850043.
Afshari K, et al. Anti-inflammatory effects of Metformin improve the neuropathic pain and locomotor activity in spinal cord injured rats: introduction of an alternative therapy. Spinal Cord. 2018;56(11):1032–41.
Shiers S, et al. Neuropathic pain creates an enduring prefrontal cortex dysfunction corrected by the type II diabetic drug metformin but not by gabapentin. J Neurosci. 2018;38(33):7337–50.
El-fatatry BM, et al. Role of metformin in oxaliplatin-induced peripheral neuropathy in patients with stage III colorectal cancer: randomized, controlled study. Int J Colorectal Dis. 2018;33(12):1675–83.
Pulito C, et al. Oral mucositis: the hidden side of cancer therapy. J Exp Clin Cancer Res. 2020;39(1):1–15.
İpek BE, Yüksel M, Cumbul A, Ercan F, Cabadak H, Aydın B, Alican İ. The Effect of Metformin on Ethanol-and IndomethacinInduced Gastric Ulcers in Rats. The Turkish journal of gastroenterology: the official journal of Turkish Society of Gastroenterology. 2022;33(9):767–76.
AbdelAziz EY, Tadros MG, Menze ET. The effect of metformin on indomethacin-induced gastric ulcer: involvement of nitric oxide/Rho kinase pathway. Eur J Pharmacol. 2021;892: 173812.
Tawfeek HM, et al. Pharmaceutical, clinical, and immunohistochemical studies of metformin hydrochloride topical hydrogel for wound healing application. Arch Dermatol Res. 2020;312(2):113–21.
Bagheri H, Rezapoor S, Najafi M, Safar H, Shabeeb D , et al. Metformin Protects the Rat Small Intestine Against Radiation Enteritis. Jundishapur J Nat Pharm Prod. 2019;14(4):e67352.
Sun H, et al. Metformin protects 5-Fu-induced chemotherapy oral mucositis by reducing endoplasmic reticulum stress in mice. Eur J Pharm Sci. 2022;173: 106182.
Van Norren K, et al. Direct effects of doxorubicin on skeletal muscle contribute to fatigue. Br J Cancer. 2009;100(2):311–4.
Gilliam LA, St. Clair DK. Chemotherapy-induced weakness and fatigue in skeletal muscle: the role of oxidative stress. Antioxid Redox Signal. 2011;15(9):2543–63.
Murphy TS, et al. Metformin limits loss of mitochondrial respiration seen with doxorubicin treatment without affecting muscle function. FASEB J. 2016;30:1245.9.
de Lima EA, et al. Aerobic exercise, but not metformin, prevents reduction of muscular performance by AMPk activation in mice on doxorubicin chemotherapy. J Cell Physiol. 2018;233(12):9652–62.
Mackay AD, et al. Exercise, but not metformin prevents loss of muscle function due to doxorubicin in mice using an in situ method. Int J Mol Sci. 2021;22(17):9163.
Afzal MZ, et al. Clinical outcomes in non-small-cell lung cancer patients receiving concurrent metformin and immune checkpoint inhibitors. Lung Cancer Manag. 2019;8(2):LMT11.
ten Tije AJ, et al. Weekly paclitaxel as first-line chemotherapy for elderly patients with metastatic breast cancer. A multicentre phase II trial. Eur J Cancer. 2004;40(3):352–7.
Pusztai L, et al. Changes in plasma levels of inflammatory cytokines in response to paclitaxel chemotherapy. Cytokine. 2004;25(3):94–102.
Zhao L, Zhang B. Doxorubicin induces cardiotoxicity through upregulation of death receptors mediated apoptosis in cardiomyocytes. Sci Rep. 2017;7(1):1–11.
Hu W, Song M, Li L. Grading Evaluation of Cardiotoxicity in Patients with Breast Cancer Treated with Adjuvant Paclitaxel Anthracycline/Cyclophosphamide Chemotherapy: A Meta-Analysis. Computational and Mathematical Methods in Medicine. 2022;2022:7963146-.
Raj S, Franco VI, Lipshultz SE. Anthracycline-induced cardiotoxicity: a review of pathophysiology, diagnosis, and treatment. Curr Treat Options Cardiovasc Med. 2014;16(6):1–14.
Ajzashokouhi A, et al. A review on the cardioprotective mechanisms of metformin against doxorubicin. Hum Exp Toxicol. 2020;39(3):237–48.
Sheibani M, Azizi Y, Shayan M, Nezamoleslami S, Eslami F, Farjoo MH, Dehpour AR. Doxorubicin-induced cardiotoxicity: an overview on pre-clinical therapeutic approaches. Cardiovascular Toxicology. 2022;22(4):292–310.
Yu J-M, et al. Metformin reduces radiation-induced cardiac toxicity risk in patients having breast cancer. Am J Cancer Res. 2019;9(5):1017.
Machado MV, Cortez-Pinto H. Non-alcoholic fatty liver disease: what the clinician needs to know. World J Gastroenterol. 2014;20(36):12956–80.
Mazza A, Fruci B, Garinis GA, Giuliano S, Malaguarnera R, Belfiore A. The role of metformin in the management of NAFLD. Experimental Diabetes Research. 2011;2012:716404-.
Duseja A, et al. Metformin is effective in achieving biochemical response in patients with nonalcoholic fatty liver disease (NAFLD) not responding to lifestyle interventions. Ann Hepatol. 2007;6(4):222–6.
Ahn JH, et al. Alternative therapy and abnormal liver function during adjuvant chemotherapy in breast cancer patients. J Korean Med Sci. 2004;19(3):397–400.
Schumacher JD, Guo GL. Mechanistic review of drug-induced steatohepatitis. Toxicol Appl Pharmacol. 2015;289(1):40–7.
Miranda VC, et al. Phase 2 trial of metformin combined with 5-fluorouracil in patients with refractory metastatic colorectal cancer. Clin Colorectal Cancer. 2016;15(4):321-328.e1.
Bragagnoli AC, et al. Metformin plus lrinotecan in patients with refractory colorectal cancer: a phase 2 clinical trial. Br J Cancer. 2021;124(6):1072–8.
Yang JY, Liu MJ, Lv L, Guo JR, He KY, Zhang H, Wang KK, Cui CY, Yan BZ, Du DD, Wang JH. Metformin alleviates irradiation-induced intestinal injury by activation of FXR in intestinal epithelia. Frontiers in Microbiology. 2022;13:932294-.
Melichar B, Zezulová M. The significance of altered gastrointestinal permeability in cancer patients. Curr Opin Support Palliat Care. 2011;5(1):47–54.
Peterson DE, Cariello A. Mucosal damage: a major risk factor for severe complications after cytotoxic therapy. InSeminars in oncology 2004;31(3 Suppl 8):35–44.
Xia J, et al. Metformin ameliorates 5-fluorouracil-induced intestinalinjury by inhibiting cellular senescence, inflammation, and oxidative stress. Int Immunopharmacol. 2022;113(Pt A): 109342.
Ma C, et al. Behavioural factors associated with diarrhea among adults over 18 years of age in Beijing, China. BMC Public Health. 2014;14(1):451.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Conflicts of interest
Manar A. Serageldin, Amira B. Kassem, Yasser El-Kerm, Maged W. Helmy, Mahmoud M. El-Mas, and Noha A. El-Bassiouny declare no conflict of interest.
Availability of data and material
All data generated or analysed during this study are included in this published article and its supplementary information files.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki and its later amendments. Institutional ethical approvals were obtained from Alexandria University (IRB no. 00012098), and Damanhour University (IRB no. 919PP18) before the commencement of the study.
Consent to participate
Written informed consent was obtained from all participants before participation in this study.
Consent to publish
Not applicable.
Code availability
Not applicable.
Authors’ contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Manar A. Serageldin. The first draft of the manuscript was written by Manar A. Serageldin and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Serageldin, M.A., Kassem, A.B., El-Kerm, Y. et al. The Effect of Metformin on Chemotherapy-Induced Toxicities in Non-diabetic Breast Cancer Patients: A Randomised Controlled Study. Drug Saf 46, 587–599 (2023). https://doi.org/10.1007/s40264-023-01305-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-023-01305-4