Abstract
Background
To date, a large proportion of people still suffer from diarrhea diseases. In addition to the burden of diarrhea, there are substantial social and economic costs caused by the high incidence of diarrheal diseases. Therefore, the purpose of this study was to explore the self-reported prevalence of diarrhea and associated risk factors of diarrhea among adults in Beijing, China.
Methods
A multistage, stratified study based on cross-sectional data was performed using randomized and systematic sampling, recruiting 12,936 adults over 18 years of age in Beijing. All adults were requested to complete a questionnaire, including information such as demographic characteristics, incidence of diarrhea, and behaviors related to the diarrhea.
Results
The self-reported prevalence of diarrhea was 17.5% during the last year prior to the survey. Six behavioral factors were significantly associated with diarrhea in our study including: (1) washing hands before meals and after defecation (Adjusted Odds Ratio (AOR) 0.707, 95% CI 0.597 ~ 0.837), (2) washing hands with soap and running water (AOR 0.872, 95% CI 0.786 ~ 0.967), (3) consuming raw seafood (AOR 1.285, 95% CI 1.138 ~ 1.450), (4) using the same chopping block and knife when processing raw and cooked food (AOR 1.375, 95% CI 1.225 ~ 1.542), (5) using the same chopsticks to handle raw and cooked food (AOR1.149, 95% CI 1.041 ~ 1.268), and (6) regularly participating in physical exercise (AOR 0.719, 95% CI 0.651 ~ 0.793).
Conclusion
Good health habits, good eating habits, and regular exercise can prevent the episodes of diarrhea, and thus decrease the potential for disease occurrence.
Similar content being viewed by others
Background
Diarrheal diseases are common world-wide and can induce a broad spectrum of symptoms ranging from mild discomfort to dehydration or death if treatment is not administered. In the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10), different forms of diarrhea are listed including infective neonatal diarrhea, unspecified diarrhea, functional diarrhea, non-infective neonatal diarrhea, and irritable bowel syndrome with diarrhea. Diarrhea can be caused by bacterial infection, viral infection, parasites, drugs, psychological factors, allergies, etc. A systematic analysis for the Global Burden of Disease (GBD) indicated that there are ten aetiologies for diarrhea in the cause list for 2010 [1].
Episodes of diarrhea illness can cause serious complications, such as dehydration, acidosis, and viral myocarditis, particularly in more vulnerable groups including children, elderly, or those with chronic disease [2]. GBD data from World Health Organization (WHO) showed that diarrheal disease is the fifth most common cause of death, which accounted for 3.7% (2.2 million) of all deaths in 2004 [3]. In 2010, 1.4 million people, across all ages, died from diarrheal diseases, and the age-standardized death rate was 20.9 per 100,000, which has fallen 49% between the years of 1990 and 2010 [1]. Although death rates from diarrheal diseases have been dramatically declining over the past twenty years, a large proportion of people still suffer from such diseases. In addition to the burden of disease, a large proportion of people still suffer from such diseases. In addition to the burden of disease, there are also substantial social and economic costs caused by the high incidence of diarrheal diseases [4–6]. Furthermore, people with diarrhea generally have a lower health-related quality of life, increased absenteeism from work or school, and reduced social interaction.
To date, there are no effective vaccinations against the various causes of diarrhea disease. Therefore, decreasing the morbidity is the most fundamental and effective approach to minimize the impact of diarrhea. A variety of risk factors have been identified in previous studies, including food contaminate, distance between the septic tank and well water, drink contaminate, household behaviors, restaurant sanitation, and environmental hygiene [7–12]. Medical examination and treatment including gastrointestinal endoscopy and early use of a pacifier have been found to lead to diarrhea [13, 14]. In addition, total monthly household income is an influence factor for diarrhea [12]. The contribution of individual factors influencing the onset of diarrhea varies in different areas or regions due to cultural differences, eating habits and behaviors, economic status, among others. In order to design effective prevention strategies and interventions against episodes of diarrhea among the adults in Beijing, identifying factors, especially risk behaviors, which contributed most to diarrhea is very important. Few large-scale population surveys have been conducted to identify the prevalence of diarrhea and characterize the risk factors associated with diarrhea in adults of Beijing. Therefore, the aim of the present study was to investigate the prevalence of diarrhea relating to influential factors of behaviors among adults in Beijing, China.
Methods
Subjects
The target population was adults over 18 years of age in Beijing, China. The respondents were classified into 20 subgroups according to living area (urban or suburban), gender (male or female) and age group (18 to 29, 30 to 39, 40 to 49, 50 to 59, and 60 and above). The following formula was used to estimate the sample size in each subgroup: n = (t2pq/d2)*deff, where t = 1.96 (Type I error), P = 50% (we could not get the reporting rate of diarrhea among subjects, thus P is equal to 50 to attain maximum sample size), q = 1 – p, d = 0.1p (permissive error) and a hypothesis of design effect (deff) of 1.5. Assuming that no-answer rate is 15%, then, a sample size of 13,248 questionnaires was calculated to obtain.
Beijing is the capital of China, has a population greater than 20 million people, and is divided into 16 districts, including 6 urban and 10 suburban districts. The survey was undertaken in six randomly selected districts, including three urban districts and three suburban districts. Participants were recruited using a multi-stage stratified sampling method in each district. Firstly, five towns/streets per district were randomly selected. Secondly, five villages/communities in each of the towns/streets were randomly selected. Thirdly, 29–44 households per village/community were randomly selected for interviews. The investigators visited the households individually, and interviewed each adult within the households until 87–89 residents were investigated in each community/village.
Data collection
A pre-test was conducted in different education levels and age groups to assess suitability with regard to study comprehension, language appropriateness, and duration. All investigators were trained in research and interviewing skills, content of questionnaire, and data quality. Before implementing the study, a letter which explained the objectives of the research was provided to all eligible participants. Then, questionnaires were carried out among those who gave verbal consent of participation. Respondents completed the questionnaire under the supervision of the trained investigators. Data in each of the questionnaires were checked carefully for incorrect or omitted items, and logistical errors by investigators.
Variable specification
The questionnaire consisted of three parts, demographic information (gender, age, education level, occupation, and living area), diarrhea, and behaviors. Diarrhea was defined according to criteria used by the WHO: 3 or more loose or liquid stools per day, or more frequently than is normal for the individual [15]. People were queried as to whether they have had diarrhea during the last year prior to the survey. They also answered questions regarding whether they washed hands before meals and after defecation for the day prior to diarrhea (every time, most of time, sometimes, almost not, or never), and the type of hand washing (soap with running water or others). Other questions included if subjects eat raw seafood or freshwater products (yes or no), use the same chopping block and knife when processing raw food and cooked food (yes or no), and use the same chopsticks to pick up raw food and cooked food when eating instant-boiled mutton slices (yes or no). Additionally, questions were asked if choice of restaurant was based on sanitary conditions; if subjects participate in regular physical exercise (more than three times every week, more than 30 minutes every time and medium to high intensity of exercise; yes or no).
Ethics Statement
This study was approved by the Institutional Review Board and Human Research Ethics Committee of Beijing Center for Disease Prevention and Control. At the beginning of each interview, the agreement and verbal consent of the interviewee was obtained. Anonymity of the participants was guaranteed.
Statistical analysis
Descriptive statistics (frequencies and proportions) were calculated for all items in the questionnaire. Weighted analysis was conducted to calculate the total incidence of diarrhea,the data were weighted for age and gender. As described previously [16, 17], the univariate logistic regression analysis was conducted to assess the factors that contributed to diarrhea. Multivariate logistic regressions adjusted for age groups, education level, and living area, were used to test the individual factors that led to diarrhea. A probability of P ≤ 0.05 was considered statistically significant. All statistical tests were two-sided. The data were processed, and statistical analysis was performed with SPSS 16.0 software (SPSS Inc., Chicago, IL, USA).
Results
The socio-demographic characteristics of the participants are illustrated in Table 1. Of the 12,936 respondents, the average age was 44.81 years (95% CI 44.81 ± 0.25), approximately 48% were male and 52% were female. The number of respondents at different age groups ranged from 2,514 to 2,683. More than 86% of respondents’ education level was junior high school or above. Of all respondents, 2,265 (17.5%) suffered from diarrhea during the last year. The self-reported rate of diarrhea was significantly different among age groups, education levels, and living areas (P < 0.05). In this study, the communities and villages were not selected with probability proportional according to population size, and the sample might not be representative of the underlying population. Therefore, weighted analysis was conducted to calculate the total incidence of diarrhea, which was17.9% after weighted for age and gender.
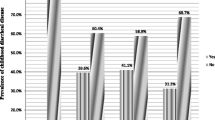
The self-reported prevalence of diarrhea among people who wash their hands before meals and after defecation (16.9%) is significantly lower than people who do not wash their hands in the same circumstances (24.1%) (P < 0.05) (Table 2). Approximately, 16% of people who wash their hands with soap and running water reported suffering from diarrhea, and the self-reported rates were significantly higher for people with inappropriate manners of hand-washing (19.4%) (P < 0.05). Moreover, there was a significant difference for those who self-reported the prevalence of diarrhea between the group of eating raw seafood (21.3%) and the group of never eating those foods (16.8%) (P < 0.05). Those who use the same chopping block and knife when processing raw and cooked foods self-reported a greater prevalence compared to those who use different chopping blocks and knives (P < 0.05). Additionally, those who use the same chopsticks to pick up raw food and cooked food when eating instant-boiled mutton slices self-reported a greater prevalence rate of diarrhea than those using separated (P < 0.05). However, there was no statistical significance found in self-reported diarrhea prevalence rates between people choosing to eat at restaurants based on their sanitary conditions (17.0%) and those who do not take sanitary conditions into account (18.3%) (P > 0.05). Meanwhile, self-reported prevalence rates of diarrhea among people being used to regular physical exercise (15.3%) was significantly lower than those with a more sedentary lifestyle (21.0%) (P < 0.05).
Six factors were significantly associated with diarrhea after adjustment for age, education level, and living area (P < 0.05; Table 3). They were: (1) hand-washing before meals and after defecation (AOR 0.707, 95% CI 0.597 ~ 0.837), (2) hand-washing with soap and running water (AOR 0.872, 95% CI 0.786 ~ 0.967), (3) eating raw seafood or freshwater products (AOR 1.285, 95% CI 1.138 ~ 1.450), (4) using the same chopping block and knife when processing raw and cooked food (AOR 1.375, 95% CI 1.225 ~ 1.542), (5) using the same chopsticks to pick up raw and cooked food when eating instant-boiled mutton slices (AOR1.149, 95% CI 1.041 ~ 1.268), and (6) regularly participating in physical exercise (AOR 0.719, 95% CI 0.651 ~ 0.793).
Discussion
In this study, the self-reported prevalence of diarrhea during the last year prior to the survey was 17.5% among adults in Beijing. A previous study, published in 2005, showed that the prevalence of reporting diarrhea in four weeks prior to interview were 6.5% in Australia, 7.9% in Canada, 3.6% in Ireland, and 7.8% in United States, with diarrhea being defined as more than 3 loose stools or bowel movements in any 24 h period in the study [2]. Similarly, Wheeler J G et al. found that the retrospective estimate of reported rate of diarrhea in the last month was 6.5% in England which was published in 1999 [18], and Feldman R A et al. reported it was 7.9% in Great Britain [19]. If the reporting rates of diarrhea in the past days in above studies are converted to one year, it might be higher than the results of the study presented here. The difference may partially be due to the change of behaviors and sanitary condition over time, and the diarrhea definition. However, we cannot rule out the possibility that the differences are caused by recall bias. Moreover, our result is different compared to Elaine et al. showing the prevalence of diarrhea was consistently higher in females, while it was lowest in person more than 65 years of age among Australia, Canada, Ireland, and United States and it was published in 2005 [2]. These differences might be associated with the variations in the cause of diarrhea as well as the behavior model of people between developed countries and developing countries.
Many types of pathogens, such as Vibrio cholera, Shigella spp, Salmonella spp, and rotavirus, multiply in the human gut, exit in excreta, and transition through the environment, which can ultimately cause diarrhea in new hosts [20, 21]. Because pathogens of diarrheal diseases occur in feces, the prevention of fecal matter from polluting the environment is likely to be of great significance to public health [22]. Safe stool disposal and adequate hand washing, especially after defecation, are the key principal barriers to the transmission of enteric pathogens [21]. Hands can serve as a medium, which transmit pathogens to food and drink and ultimately to the mouths of susceptible individuals. This is supported by a systematic showing hand washing reduced diarrhea incidence with a median of 35% in five studies [23]. Similarly, another review demonstrated that washing hands with soap can reduce the risk of diarrheal diseases by 42% [20]. In the present study, the risk of suffering diarrhea among the subjects washing their hand before meals and after defecation reduce diarrhea incidence by 29%, which further confirmes previous findings in different countries.
A wide range of bacteria, viruses, and parasites have been involved in seafood-related outbreaks, which are reported globally [24]. The risk factor most commonly associated with infection is consumption of raw or undercooked seafood [24]. At least ten genera of bacterial pathogens have been involved in seafood-borne diseases [25]. Previous research shows that consumption of raw or undercooked seafood contaminated with Vibrio parahaemolyticus may result in development of acute gastroenteritis characterized by diarrhea, and this pathogen is a common cause of food-borne illness in Asia, including China, Japan, and Taiwan [26]. Kain K C et al. found that among P. shigelloides-infected patients, 29% acquired the infections locally in association with the consumption of seafood or untreated water or both [27]. This gives evidence that there is a significantly greater frequency of occurrence of diarrhea in people who eat raw seafood over people who do not, thus education should be implemented with regard to safe food preparation habits and dietary health habit.
It has been well established that improper practices of food preparation in consumer homes contribute to a substantial proportion of food-borne diseases [28, 29]. For instance, bacteria, including Salmonella spp can be readily transferred to cutting boards and utensils during food preparation, which can cross-contaminate other foods if the boards and utensils are not cleaned [30]. It has been estimated that cross-contamination in the household kitchen resulting in food poisoning can be attributed to contamination from Escherichia coli O157:H7 (40%), Campylobacter (30%), and Salmonella (20%) [11]. Our results are similar to previous findings showing that factors associated with a lower risk of self-reported diarrhea used separate chopping boards when processing raw meats and cooked meats (OR 0.803, 95% CI 0.648 ~ 0.994) or other raw and cooked foods (OR 0.741, 95% CI 0.599 ~ 0.919) [11].
There are some limitations in our study. The first and main limitation is recall bias. The study contents involved cases of diarrhea throughout a year prior to filling out the questionnaire. The information was collected retrospectively, and the interviewees may be likely to have forgotten about their high-risk behaviours. Secondly, some respondents suffered from diarrhea more than once, thus the prevalence rates may have been underestimated in our study. Thirdly, most of the risk factors in our regression model are associated with infective diarrhea, however, non-infective diarrhea caused by drugs, psychological factors, allergies, etc. also contributed to diarrhea of the respondents in last year. Hence, additional risk factors related to non-infective diarrhea should be taken into account in future studies. The results of this study provide evidence that more attention should be given to the issues regarding domestic kitchen hygiene, especially food handling, preparation, and storage practices, in order to effectively and efficiently reduce the prevalence of diarrhea in the developing world.
Conclusions
This is a large-scale population surveys to identify the prevalence of diarrhea and explore the risk factors associated with diarrhea in adults in Beijing. The self-reported prevalence of diarrhea was lower than some other countries. The results suggest that good health habits, good eating habits, and regular exercise can prevent the episodes of diarrhea, and thus decrease the potential for disease occurrence.
References
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Barker-Collo S, Bartels DH, Bell ML, Benjamin EJ, Bennett D, Bhalla K, Bikbov B, Bin Abdulhak A, Birbeck G, Blyth F, Bolliger I, Boufous S, Bucello C, Burch M, et al: Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012, 380 (9859): 2095-2128. 10.1016/S0140-6736(12)61728-0.
Scallan E, Majowicz SE, Hall G, Banerjee A, Bowman CL, Daly L, Jones T, Kirk MD, Fitzgerald M, Angulo FJ: Prevalence of diarrhoea in the community in Australia, Canada, Ireland, and the United States. Int J Epidemiol. 2005, 34 (2): 454-460. 10.1093/ije/dyh413.
World Health Organization: The global burden of disease: 2004 updata. [http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf?ua=1]
Buzby JC, Roberts T: Economic costs and trade impacts of microbial foodborne illness. World Health Stat Q. 1997, 50 (1–2): 57-66.
Roberts JA, Cumberland P, Sockett PN, Wheeler J, Rodrigues LC, Sethi D, Roderick PJ, Infectious Intestinal Disease Study E: The study of infectious intestinal disease in England: socio-economic impact. Epidemiol Infect. 2003, 130 (1): 1-11. 10.1017/S0950268802007690.
Hellard ME, Sinclair MI, Harris AH, Kirk M, Fairley CK: Cost of community gastroenteritis. J Gastroenterol Hepatol. 2003, 18 (3): 322-328. 10.1046/j.1440-1746.2003.02959.x.
de Wit MA, Koopmans MP, van Duynhoven YT: Risk factors for norovirus, Sapporo-like virus, and group A rotavirus gastroenteritis. Emerg Infect Dis. 2003, 9 (12): 1563-1570. 10.3201/eid0912.020076.
Fewtrell L, Kaufmann RB, Kay D, Enanoria W, Haller L, Colford JM: Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and meta-analysis. Lancet Infect Dis. 2005, 5 (1): 42-52. 10.1016/S1473-3099(04)01253-8.
Bentley ME: Household Behaviors in the Management of Diarrhea and Their Relevance for Persistent Diarrhea. Acta Paediatr. 1992, 81: 49-54. 10.1111/j.1651-2227.1992.tb12372.x.
Sumner S, Brown LG, Frick R, Stone C, Carpenter LR, Bushnell L, Nicholas D, Mack J, Blade H, Tobin-D'Angelo M, Everstine K, Environmental Health Specialists Network Working Group: Factors Associated with Food Workers Working while Experiencing Vomiting or Diarrhea. J Food Prot. 2011, 74 (2): 215-220. 10.4315/0362-028X.JFP-10-108.
Stenberg A, Macdonald C, Hunter PR: How effective is good domestic kitchen hygiene at reducing diarrhoeal disease in developed countries? A systematic review and reanalysis of the UK IID study. BMC Public Health. 2008, 8: 71-10.1186/1471-2458-8-71.
Ozkan S, Tuzun H, Gorer N, Ceyhan M, Aycan S, Albayrak S, Bumin MA: Water usage habits and the incidence of diarrhea in rural Ankara, Turkey. Trans R Soc Trop Med Hyg. 2007, 101 (11): 1131-1135. 10.1016/j.trstmh.2007.05.011.
Festini F, Giusti F, Paoletti E, Biancalani L, Poggi GM: Is early use of pacifier a risk factor for diarrhea?. Minerva Pediatr. 2012, 64 (3): 303-305.
Selinger CP, Greer S, Sutton CJ: Is gastrointestinal endoscopy a risk factor for Clostridium difficile associated diarrhea?. Am J Infect Control. 2010, 38 (7): 581-582. 10.1016/j.ajic.2010.01.010.
World Health Organization: Health topics, Diarrhoea. [http://www.who.int/topics/diarrhoea/en/]
Zhang Y, Seale H, Yang P, MacIntyre CR, Blackwell B, Tang S, Wang Q: Factors associated with the transmission of pandemic (H1N1) 2009 among hospital healthcare workers in Beijing, China. Influenza Other Respi Viruses. 2013, 7 (3): 466-471. 10.1111/irv.12025.
Zhang D, Liu W, Yang P, Zhang Y, Li X, Germ KE, Tang S, Sun W, Wang Q: Factors associated with household transmission of pandemic (H1N1) 2009 among self-quarantined patients in Beijing, China. PloS one. 2013, 8 (10): e77873-10.1371/journal.pone.0077873.
Wheeler JG, Sethi D, Cowden JM, Wall PG, Rodrigues LC, Tompkins DS, Hudson MJ, Roderick PJ: Study of infectious intestinal disease in England: rates in the community, presenting to general practice, and reported to national surveillance, The Infectious Intestinal Disease Study Executive. BMJ. 1999, 318 (7190): 1046-1050. 10.1136/bmj.318.7190.1046.
Feldman RA, Banatvala N: The frequency of culturing stools from adults with diarrhoea in Great Britain. Epidemiol Infect. 1994, 113 (1): 41-44. 10.1017/S095026880005144X.
Curtis V, Cairncross S: Effect of washing hands with soap on diarrhoea risk in the community: a systematic review. Lancet Infect Dis. 2003, 3 (5): 275-281. 10.1016/S1473-3099(03)00606-6.
Wang D, Xu X, Deng X, Chen C, Li B, Tan H, Wang H, Tang S, Qiu H, Chen J, Ke B, Ke C, Kan B: Detection of Vibrio cholerae O1 and O139 in environmental water samples by an immunofluorescent-aggregation assay. Appl Environ Microbiol. 2010, 76 (16): 5520-5525. 10.1128/AEM.02559-09.
Curtis V, Cairncross S, Yonli R: Domestic hygiene and diarrhoea - pinpointing the problem. Trop Med Int Health. 2000, 5 (1): 22-32. 10.1046/j.1365-3156.2000.00512.x.
Huttly SR, Morris SS, Pisani V: Prevention of diarrhoea in young children in developing countries. Bull World Health Organ. 1997, 75 (2): 163-174.
Butt AA, Aldridge KE, Sanders CV: Infections related to the ingestion of seafood Part I: Viral and bacterial infections. Lancet Infect Dis. 2004, 4 (4): 201-212. 10.1016/S1473-3099(04)00969-7.
Feldhusen F: The role of seafood in bacterial foodborne diseases. Microbes Infect. 2000, 2 (13): 1651-1660. 10.1016/S1286-4579(00)01321-6.
Su YC, Liu C: Vibrio parahaemolyticus: a concern of seafood safety. Food Microbiol. 2007, 24 (6): 549-558. 10.1016/j.fm.2007.01.005.
Kain KC, Kelly MT: Clinical features, epidemiology, and treatment of Plesiomonas shigelloides diarrhea. J Clin Microbiol. 1989, 27 (5): 998-1001.
Redmond EC, Griffith CJ: Consumer food handling in the home: a review of food safety studies. J Food Prot. 2003, 66 (1): 130-161.
Duff SB, Scott EA, Mafilios MS, Todd EC, Krilov LR, Geddes AM, Ackerman SJ: Cost-effectiveness of a targeted disinfection program in household kitchens to prevent foodborne illnesses in the United States, Canada, and the United Kingdom. J Food Prot. 2003, 66 (11): 2103-2115.
Zhao P, Zhao T, Doyle MP, Rubino JR, Meng J: Development of a model for evaluation of microbial cross-contamination in the kitchen. J Food Prot. 1998, 61 (8): 960-963.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2458/14/451/prepub
Acknowledgements
This work was financially supported by Beijing Nova Program of Beijing Science and Technology Commission (2011047), National Key Program for Infectious Disease of China (2012ZX10004215-003-001), and China Special Grant for the Prevention and Control of Infectious Diseases (2013ZX10004218). The funding agencies did not influence or participate in the design and conduct of the study, in the collection, management, analysis, or interpretation of the data, in the writing of the manuscript, or in the decision to submit the article for publication. The researchers were independent of the funding agencies.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
MC, WS, TS and WQ designed the study. MC, WS, YP and LH performed the data collection. MC analyzed the data and wrote the manuscript. All authors have read and approved the final version of the manuscript.
Chunna Ma, Shuangsheng Wu contributed equally to this work.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Ma, C., Wu, S., Yang, P. et al. Behavioural factors associated with diarrhea among adults over 18 years of age in Beijing, China. BMC Public Health 14, 451 (2014). https://doi.org/10.1186/1471-2458-14-451
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2458-14-451