Abstract
Background
Numerous biologic drugs, including etanercept and adalimumab, are administered subcutaneously. This study reviewed the evidence on the usability and preference of self-injection devices of SB4 and SB5 compared with the reference product injectors.
Methods
A systematic search was conducted in PubMed using the search string “(Imraldi OR Hadlima OR SB5 OR Benepali OR Brenzys OR SB4) AND (preference) AND (device)” covering the period from 28 January 2016 (first introduction of SB4) to 31 May 2022. Only articles and abstracts on usability or preference-rating of SB4 and SB5 autoinjectors (AI) written in English were selected. Additional papers identified via manual search supplemented the retrieved papers.
Results
A total of nine articles and one conference poster were selected (seven surveys, one observational study, and two phase II studies). Overall, participants of the studies included nurses and rheumatologists, as well as patients who were from three medical specialties where these medicines are most commonly used (rheumatology, gastroenterology, and dermatology). The majority of patients and healthcare professionals rated ease of use and ease of grip as the most important device attributes. SB4/Pen and SB5/Pen were mostly preferred over their prefilled syringes (PFS), Enbrel/Pen, and Humira/Pen.
Conclusion
The analyzed data on usability and device preference indicate that SB4/Pen and SB5/Pen were preferred over the other reference product autoinjectors, thanks to their button-free design, auditory and visual injection feedback, and overall ease of use. Therefore, they were preferred over the other reference product autoinjectors. Because user-friendly devices can improve treatment adherence, pharmaceutical companies should consider patient convenience when developing medical devices.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Device features of self-injecting biosimilars may be one of the factors that can differentiate biosimilars that are expected to have similar efficacy and safety profiles. |
By providing device features that are preferred by patients, biosimilars may improve patient experience, on top of the biosimilars’ expected benefit of lower cost and increased accessibility. |
1 Introduction
Biological therapies that inhibit tumor necrosis factor (TNF) (e.g., etanercept and adalimumab) have improved the management of various inflammatory and immune-mediated diseases such as rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis [1, 2].
SB4 (Benepali™ or Brenzys®, Samsung Bioepis) was the first etanercept biosimilar to demonstrate equivalent efficacy and pharmacokinetics and comparable safety to its reference product (Enbrel, Pfizer; Enbrel is a trademark of Wyeth LLC) in clinical trials [3, 4]. It received marketing authorization in the European Union (EU) in 2016 and the USA in 2019 [3]. SB5 (Imraldi™ or Hadlima™, Samsung Bioepis) is an adalimumab biosimilar, which demonstrated equivalent efficacy and pharmacokinetics and comparable safety to its reference product (Humira, AbbVie; Humira is a trademark of Abbvie Biotechnology Ltd) in clinical trials and was approved in the EU in 2017 and the USA in 2019 [5,6,7]. Both SB4 and SB5 received an extrapolated approval for all major indications of the respective reference product based on the totality of evidence [8].
The first biologic drug in this area was given by intravenous infusion, with many subsequent drugs formulated to be administered by subcutaneous injection [9]. This allows patients to self-inject their medication and permits home administration, which many patients find more convenient, and it also reduces the burden on the healthcare system. Automated self-injection devices, often referred to as autoinjectors (AIs) or pens, have been developed to simplify the handling and reduce the burden to patients when performing self-injection [10]. Notably, biosimilars may present with different delivery devices than the reference product or other biosimilars of the same reference product, assuming equivalence of efficacy and pharmacokinetics and comparability of safety are not affected [11]. In phase I studies of SB4 and SB5, bioequivalence between prefilled syringes (PFS) and AIs was demonstrated in healthy subjects [12, 13]. Open-label phase II studies of SB4 and SB5 showed a greater preference for AI rather than PFS in patients with rheumatoid arthritis (RA) [14, 15].
Overall, preference studies assess device attributes for patients’ benefit by comparing new injection devices with already existing and approved ones [9]. This can be important for patients with RA in whom treatment compliance is suboptimal, possibly due to struggles with self-administration resulting from limitations in hand-function and manual dexterity [16, 17]. The objective of this literature review is to assess available evidence for patients’ preference and usability with an emphasis on the medical device properties of SB4, SB5, and their reference products.
2 Methods
2.1 Search Strategy and Selection Criteria
PubMed was searched for journal articles and abstracts with the search string “(Imraldi OR Hadlima OR SB5 OR Benepali OR Brenzys OR SB4) AND (preference) AND (device)” covering the period from 28 January 2016 (first introduction of SB4) to 31 May 2022. Relevant articles were supplemented with hand-selected references and data available to the authors. The search hits were screened using titles and abstracts, followed by full-text screening and appraisal. Subsequently, abstracts and manuscripts that reported on preference studies, surveys, and usability data related to SB4 and SB5 medical devices, based on patient and/or healthcare professional (HCP) input, were selected for this review. Non-English articles and articles without data on the usability of or preference for SB4 and/or SB5 medical devices were excluded.
2.2 Data Extraction
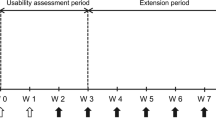
The following data were examined and collated in summary tables—study objectives, design and population, number of enrolled participants, importance of medical device attributes, evaluated medical devices, experience with the medical devices, ratings of the evaluated devices in terms of medical device attributes, participants’ overall medical device preference, and key reasons for preference. For the purpose of this review, both the drug and device name are combined, even if the text about experience/preference primarily refers to the device part (AI or PFS) of the product, i.e., SB4/Pen (AI), SB5/Pen (AI), Enbrel/Pen (AI), and Humira/Pen (AI) (Fig. 1). For SB4 and SB5, data on the PFS device were also identified and presented.
2.3 Outcome Measurement
Results about the importance of device attributes, perceived performance of the devices in those attributes, and the overall device preference were stratified according to the study group and compared between the medical devices. Since different studies and surveys used slightly different terms for certain attributes, results for terms referring to the same attribute can be summarized under one term. If applicable, the attributes were summarized in the categories “easy to use,” “button-free device,” “weight,” “easy to grip,” “needle concealment,” “audible feedback,” “visual feedback,” “convenient shape,” “quick administration,” “feedback of injection,” “checking solution clarity,” “size,” “intuitive,” “easy to remove the cap,” and “less painful injection”.
3 Results
3.1 Search Results
Overall, there were eight search results from PubMed [14, 15, 18,19,20,21,22,23]. A manual search of in-house databases yielded one additional relevant article [24] and one conference poster [25]. After the title/abstract and full-text screening, all ten references were considered eligible for this review (Fig. 2) and the relevant key information was extracted and collated in Table 1.
Six studies, which include five surveys [18,19,20,21, 24] and one phase II study [14], reported usability results for SB4/Pen and of these, five compared the usability of SB4 administration via PFS and AI, respectively. Participants included patients with inflammatory rheumatic diseases in five studies [14, 18, 20, 21, 24], nurses in three studies [19,20,21], and rheumatologists in one study [21]. SB4/Pen was compared with Enbrel/Pen in four studies [18,19,20,21], with Humira/Pen in one study [20], and with SB4/PFS in one study [14]. One study assessed the satisfaction for SB4/Pen without a comparator group [24].
Four references comprising two surveys [22, 23], one observational study [25], and one phase II study [15] reported outcomes on usability of SB5/Pen and the usability of SB5/Pen versus SB5/PFS. The included populations comprised patients with RA [15], patients with inflammatory joint or bowel diseases [22], patients with inflammatory arthritis, psoriasis, and inflammatory bowel disease [23], patients with Crohn’s disease [25], and nurses [22]. The SB5/Pen was evaluated in comparison with Enbrel/Pen in one study [22], Humira/Pen in two studies [22, 23], and SB5/PFS in one study [15]. One study reported the usability of SB5/Pen and SB5/PFS without comparing it with another injector [25].
A total of 1830 patients and 440 HCPs (409 nurses, 31 rheumatologists) participated in the usability assessments of SB4 and SB5. The assessment methods comprised face-to-face interviews in four studies [18,19,20, 22], a telephone interview in one study [23], and paper questionnaires in two studies [21, 24]. Three studies specified only that they used a questionnaire but not how it was completed [14, 15, 25]. Reported outcomes were the importance of medical device attributes in four studies [18,19,20, 22], the preference ratings of medical devices in ten studies [14, 15, 18,19,20,21,22,23,24,25], and the preferred device for treatment continuation in eight studies [14, 15, 18,19,20,21,22,23].
Four studies used a training device without the needle and active ingredient [18,19,20, 22]. One study asked participants to test the AIs by injecting into a skin-mimicking pad [21]. Five studies evaluated the usability in patients using the device of their current treatments, comprising two phase II studies [14, 15], one cross-sectional study [24], and two studies on the switch from Humira/Pen to SB5/Pen [23, 25].
The majority of studies included participants who had prior experience with an AI [18,19,20,21,22, 24, 25]. One study included patients with and without AI experience [21] and three studies [14, 15, 23] did not report whether participants had prior experience with an AI.
3.2 Importance of Device Attributes
Four of the publications included in this review assessed the importance of device features in patients and nurses [18,19,20, 22]. The importance of the device features was mostly related to ease of administration, device characteristics, safety, and feedback mechanism (Table 1) [18,19,20, 22]. Thakur et al., reported that both patients and nurses considered the same attributes as most important, namely “easy to operate self-administration”, “easy to grip the AI,” and “intuitive usage” [18, 19]. Also the following three attributes in the ranking, namely “concealment of the needle,” as well as “visual confirmation” and “audible confirmation” of the dose administration, were the same with just slightly different order among patients and nurses [18, 19].
Similarly, patients and nurses in another study, ranked “easy to use” as the most and “easy to grip” as the second-most important device characteristics, and “audible feedback” as the third and fourth most important attribute, respectively [20]. In Fenwick et al., nurses stated that the design of the AI was important and patients should feel comfortable when self-administering [22].
3.3 Preference in Various Device Attributes
3.3.1 Ease of Administration
Ease of self-injection was assessed for SB4 and SB5 in six [14, 18,19,20,21, 24] and four [15, 22, 23, 25] studies, respectively.
The majority of the patients and HCPs found that SB4/Pen was easier to self-administer and more intuitive to use when compared with Enbrel/Pen, Humira AI, and SB4/PFS [14, 18,19,20,21]. Overall, satisfaction ratings for ease of use ranged from 73 to 89% for SB4/Pen [18,19,20,21, 24], compared with 7–69% for Enbrel/Pen [18,19,20,21] and 61–64% for the Humira/Pen [20]. When compared with SB4/PFS, 84.9% of the patients stated that SB4/Pen was easier to use, and 86.8% mentioned that it was more convenient [14]. In addition, SB4/Pen was found to be less painful by 60.4% of patients who had used SB4/PFS before. Patients and nurses rated the intuitive use 63–70% for SB4/Pen, 18–63% for Enbrel/Pen, and 56–57% for Humira/Pen [18,19,20].
One study compared current users of either SB4/Pen, Enbrel/Pen, or Humira/Pen and each patient assessed satisfaction with their currently used AI [20]. Ratings on satisfaction with the ease of self-injection by these clinically experienced patients were 83% for SB4/Pen, 69% for Enbrel/Pen, and 64% for Humira/Pen (both p < 0.01 versus SB4/Pen) [20]. Nurses that were experienced with SB4/Pen, Enbrel/Pen, and Humira/Pen also reported a greater satisfaction with ease of use of SB4/Pen (73%), compared with 64% for Enbrel/Pen and 61% for Humira/Pen (p < 0.05 versus SB4/Pen) [20]. Among patients who used the SB4/Pen at least for 3 months, and those who were naïve or had experience with other application systems (i.e., another pen, syringe, or intravenous infusion), the overall satisfaction for the ease of use of SB4/Pen was 89% [24].
The preference for SB4/Pen over Enbrel/Pen was confirmed in three other studies by 74% of patients and 80–86% of HCPs in the overall preference tests. Main reasons for the preference were easier self-administration and a buttonless injector [18, 19, 21].
In two studies of SB5/Pen, patients and nurses reported a greater preference in relation to ease of self-injection for SB5/Pen (71.7–89%) compared with Humira/Pen (11–13%), Enbrel/Pen (6–11%), and SB5/PFS (21.7%) [15, 22]. In comparison with SB5/PFS, 76.1% and 65.2% of patients found the injection with SB5/Pen more convenient and less time consuming, respectively [15]. Combining the findings of SB5/Pen and SB5/PFS after 48 weeks, one study reported that 69.5% and 63.5% of patients with Crohn’s disease were satisfied with the ease of use and the duration of injection [25].
In phone interviews of patients in Iceland who underwent a nationwide switching program from Humira/Pen to SB5/Pen, 12.5% found the administration of SB5/Pen easier than Humira/Pen, and 37.6% stated no difference. About 90.5% of patients stated that they received individualized instruction on using the Humira/Pen, compared with 18.2% who accepted instruction in the case of the SB5/Pen [23]. In overall preference tests, the majority of the patients with various inflammatory diseases and nurses with adequate experience (≥ 1 year of experience and dedication of 75% of overall time for patient care) living in the UK and Germany chose SB5/Pen over Enbrel/Pen and Humira/Pen based on its ease of use, ease of grip, and button-free injector [22].
3.3.2 Feedback Mechanism
The audible and visual feedback of SB4/Pen and SB5/Pen were assessed in five studies [18,19,20,21, 24] and two studies [22, 25], respectively. Of these, three studies reported a greater patient-rated satisfaction with the auditory confirmation of SB4/Pen (43–91%) compared with Enbrel/Pen (5–54%) and Humira/Pen (33%) [18, 20, 24]. Nurses who had experience with patients with RA preferred the audible confirmation of SB4/Pen (58–70%) over Enbrel/Pen (7–63%) and Humira/Pen (59%) [19, 20].
Ratings on satisfaction with the visual feedback by patients with RA was higher for SB4/Pen (49–76%) than Enbrel/Pen (4–47%) and Humira/Pen (50%) [18, 20]. Without specifying auditory or visual, patients and HCPs preferred the dose delivery confirmation of the SB4/Pen (63.3% and 77%, respectively) compared with Enbrel/Pen [21]. In one study of patients using SB4/Pen for at least 3 months, patients’ satisfaction for indication of injection completion was 87% [24].
Nurses and patients reported a greater preference for the audible confirmation of dose delivery of the SB5/Pen (58–88% and 65–83%, respectively) compared with the Enbrel/Pen (11% and 9%, respectively) and Humira/Pen (9% and 10%, respectively) [22]. The preference tests confirmed the overall favorable results for SB5/Pen (nurses 85–86%, patients 78–79%) compared with Enbrel/Pen and Humira/Pen, with the key rationales including large and visual feedback that is suitable for hearing-impaired patients and double click that is suitable for visually impaired patients [22]. Patients and nurses stated that the SB5/Pen (62–85% and 56–84%, respectively) was better in regard to the indication of dose administration compared with Enbrel/Pen (5% and 9%, respectively) and Humira/Pen (7% and 6%, respectively) [22]. Among patients using the SB5/Pen or SB5/PFS for 48 weeks after having used the reference product for at least 16 weeks, patients’ satisfaction with the indication of completed injection ranged from 79.9 to 86.7% [25].
3.3.3 Device Characteristics
Device characteristics were investigated for SB4 and SB5 in six [14, 18,19,20,21, 24], and two studies [15, 22], respectively.
For patients with RA, SB4/Pen was found to be easier to grip (50–87%) than Enbrel/Pen (14–67%) and Humira/Pen (61%) [18, 20]. Nurses reported a higher satisfaction with the ease of grip for SB4/Pen (44–55%) compared with Enbrel/Pen (19–62%) and Humira/Pen (72%) [19, 20]. After use of SB4/pen for at least 3 months, patients with inflammatory joint diseases rated the satisfaction with ease of grip 89% [24].
The patient-rated satisfaction with the convenient shape were 74% for SB4/Pen, 56% for Enbrel/Pen, and 46% for the Humira/Pen [20]. Nurse-reported satisfaction with convenient shape was 54% for the SB4/Pen, 51% for the Enbrel/Pen, and 53% for the Humira/Pen [20].
Patients preferred the weight of the SB4/Pen (63–87%) compared with the weight of Enbrel/Pen (4–67%) and Humira/Pen (59%) [18, 20, 24]. Ratings of the nurses’ preference with the device weight ranged from 60 to 61% for the SB4/Pen, compared with 8 to 59% for the Enbrel/Pen and 57% for the Humira/Pen [19, 20].
Only one study assessed the easiness of cap removal [21]. Patients and HCPs stated that it was easier to remove the cap of SB4/Pen (60% and 55.2%, respectively) than that of Enbrel/Pen [21].
The ratings for the needle concealment differed across studies for SB4/Pen [18,19,20]. Patient satisfaction with the concealment of the needle was higher for SB4/Pen (94%), compared to those for Enbrel/Pen (79%, p < 0.01 versus SB4/Pen) and Humira/Pen (76%, p < 0.01 versus SB4 AI) [20]. In two studies, 72% of the patients [18] and 69% of the nurses [19] stated a preference for both SB4/Pen and Enbrel/Pen with respect to needle concealment, respectively. Lastly, patients and nurses found the design of SB4/Pen (37% and 42%, respectively) more attractive than that of Enbrel/Pen (27% and 32%, respectively) [18, 19].
Patients and nurses reported a higher preference in relation to the ease of grip for the SB5/Pen (74–81% and 85–90%, respectively) compared with Enbrel/Pen (14% and 6%, respectively) and Humira/Pen (17% and 7%, respectively) [22]. Notably, 62% of the patients in the national switch study in Iceland reported that the grip for both SB5/Pen and Humira/Pen was the same [23].
For patients with RA, the safety of SB5/Pen (67.4%) was found to be better compared with SB5/PFS (13%) [15]. Patients and nurses reported a higher preference in relation to the ease of checking solution clarity for the SB5/Pen (60–87% and 52–78%, respectively) compared with Enbrel/Pen (8% and 6%, respectively) and Humira/Pen (7% and 10%, respectively) [22]. In the overall preference tests, the non-slip surface of the SB5/Pen has been cited as one of the top reasons why patients and nurses prefer it to Enbrel/Pen and Humira/Pen [22].
4 Discussion
This review assessed the usability and preference of SB4 and SB5 AIs compared with available reference products. Patients and nurses considered ease of self-injection and ease of grip as the most important device attributes [18,19,20, 22]. The majority of patients and HCPs preferred the AIs of SB4 and SB5 over other reference products’ injectors [14, 15, 18, 19, 21, 22]. These conclusions are in line with six of the included studies [14, 15, 18, 19, 21, 22], and supported by the higher preference for the AIs of SB4 and SB5 compared with Enbrel/Pen, Humira/Pen, SB4/PFS, and SB5/PFS. Even though not compared with another injector directly, two studies reported high satisfaction of patients with SB4/Pen and SB5/Pen or SB5/PFS [24, 25]. In contrast, a study in Iceland reported higher preference for Humira/Pen than for SB5/Pen. The majority of patients in that study lacked personal instruction for SB5/Pen. Only 18.2% accepted instruction on SB5/Pen, compared with Humira/Pen (90.5%). This study’s results highlight the importance of thorough patient education prior to switching to biosimilars [23].
Patients with RA can develop hand deformities that cause difficulty in self-administration of the drug [26]. Both SB4/Pen and SB5/Pen have a buttonless two-step administration that requires only removal of the cap and a firm push towards the injection site [27, 28]. In comparison, Enbrel/Pen and Humira/Pen require pushing a button to initiate injection and patients need to remove a second cap from Humira/Pen to reveal this injection button [29, 30].
Patients’ needs and prior experience with other AIs may influence their perceptions of device attributes [20]. Considering those with visual or auditory impairment, both SB4/Pen and SB5/Pen have visual as well as auditory confirmations of dose delivery [27, 28]. These consist of a double click sound indicating the initiation and termination of the injection and a large window turning yellow with the dose administration [27, 28]. The double click confirmation also exists in Enbrel/Pen, but not in Humira/Pen, which only clicks once at the beginning of the injection [29, 30]. Furthermore, compared with SB4/Pen and SB5/Pen, Enbrel/Pen and Humira/Pen have smaller windows that turn purple and yellow, respectively [29, 30]. Apart from these factors, SB4/Pen and SB5/Pen have similar needle gauge compared to their alternatives [27,28,29,30]. The needle shields of all devices were latex-free, except for Enbrel/Pen, which might cause discomfort in patients with latex allergy [27,28,29,30]. The SB4/Pen is lighter and more compact than its reference product [20]. Notably, SB4/Pen, Enbrel/Pen, and Humira/Pen have a round-shaped pen [20], whereas SB5/Pen has an angular shape with non-slip surface [22], which can prevent the rolling or falling off of the pen compared with round-shaped pens. Altogether, these features can influence the handling of the device.
Limitations of this review include the absence of a standardized questionnaire and assessment method, together with selection and interviewer bias across studies. Furthermore, most of the studies assessed the usability and preference with training devices or injection pads, rather than clinical experience. The order of introduced medical devices and different experience levels of participants with each of the evaluated AIs may also have biased the overall assessment. Nevertheless, these studies provide useful patient and provider insights that can shape the development of self-injection devices. Considering the positive association between patient preference and treatment adherence [31], further studies should investigate the device usability in a broader population with a focus on ease of self-administration for better clinical outcomes.
5 Conclusion
Medical devices that are easy to use, increase patients’ satisfaction, and hence improve the treatment adherence, could potentially lead to better patient outcomes. Evidence from surveys, and usability and preference studies indicate that SB4/Pen and SB5/Pen are perceived to be easier to use by most, and hence preferred over other reference product autoinjectors; feedback from postapproval preference surveys on devices may not provide insight during the development phase, yet the feedback should be considered for future development of medical device of another product and potential changes in current device if deemed necessary. These findings suggest that pharmaceutical companies should consider ease of use when developing self-injection devices and offer patients a variety of alternatives based on their preference.
References
Smolen JS, Aletaha D, Koeller M, Weisman MH, Emery P. New therapies for treatment of rheumatoid arthritis. Lancet. 2007;370(9602):1861–74.
Mehta P, Manson JJ. What is the clinical relevance of TNF inhibitor immunogenicity in the management of patients with rheumatoid arthritis? Front Immunol. 2020;11:589.
Pelechas E, Drosos AA. Etanercept biosimilar SB-4. Expert Opin Biol Ther. 2019;19(3):173–9.
Emery P, Vencovský J, Sylwestrzak A, et al. 52-week results of the phase 3 randomized study comparing SB4 with reference etanercept in patients with active rheumatoid arthritis. Rheumatology. 2017;56(12):2093–101.
Gisbert JP, Gaffney K, Young D, Ebbers HC, Girolomoni G. Current evidence on the use of the adalimumab biosimilar SB5 (Imraldi): a multidisciplinary perspective. Expert Opin Biol Ther. 2022 (just-accepted).
Weinblatt ME, Baranauskaite A, Niebrzydowski J, et al. Phase III randomized study of SB 5, an adalimumab biosimilar, versus reference adalimumab in patients with moderate-to-severe rheumatoid arthritis. Arthritis Rheumatol. 2018;70(1):40–8.
Dignass A, Gisbert J, Freudensprung U, Addison J. P434 The PROPER study: interim analysis of a pan-European real-world study of SB5 adalimumab biosimilar after transition from reference adalimumab in patients with Crohn’s disease. J Crohns Colitis. 2022;15(Suppl 1):S459–60.
Tesser JR, Furst DE, Jacobs I. Biosimilars and the extrapolation of indications for inflammatory conditions. Biol Targets Ther. 2017;11:5.
van den Bemt BJ, Gettings L, Domańska B, Bruggraber R, Mountian I, Kristensen LE. A portfolio of biologic self-injection devices in rheumatology: how patient involvement in device design can improve treatment experience. Drug Deliv. 2019;26(1):384–92.
Rekaya N, Vicik SM, Hulesch BT, McDonald LL. Enhancement of an auto-injector device for self-administration of etanercept in patients with rheumatoid arthritis confers emotional and functional benefits. Rheumatol Ther. 2020;7(3):537–52.
EMA. Guideline on similar biological medicinal products. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-similar-biological-medicinal-products-rev1_en.pdf. Date accessed: 22 Jun 2022.
Shin D, Kim Y, Go A, Velinova M. Comparison of the pharmacokinetics, safety, and tolerability of the autoinjector (AI) and pre-filled syringe (PFS) of SB4 in healthy subjects. Drug Des Dev Ther. 2020;14:43.
Shin D, Lee Y, Jeong D, Ellis-Pegler R. Comparative pharmacokinetics of an adalimumab biosimilar SB5 administered via autoinjector or prefilled syringe in healthy subjects. Drug Des Dev Ther. 2018;12:3799.
Rho YH, Rychlewska-Hańczewska A, Śliwowska B, Kim TH. Usability of prefilled syringe and autoinjector for SB4 (an etanercept biosimilar) in patients with rheumatoid arthritis. Adv Ther. 2019;36(9):2287–95.
Ghil J, Zielińska A, Lee Y. Usability and safety of SB5 (an adalimumab biosimilar) prefilled syringe and autoinjector in patients with rheumatoid arthritis. Curr Med Res Opin. 2019;35(3):497–502.
Kilic MC, Calik BB, Cobankara V, Balkarli A. The relationship between hand function and activity performance in patients with rheumatoid arthritis. Age. 2018;32(65): 50.7-9.9.
Schwarzenbach F, Trong MD, Grange L, et al. Results of a human factors experiment of the usability and patient acceptance of a new autoinjector in patients with rheumatoid arthritis. Patient Prefer Adherence. 2014;8:199.
Thakur K, Biberger A, Handrich A, Rezk MF. Patient perceptions and preferences of two etanercept autoinjectors for rheumatoid arthritis: findings from a patient survey in Europe. Rheumatol Ther. 2016;3(2):245–56.
Thakur K, Biberger A, Handrich A, Rezk MF. Perceptions and preferences of two etanercept autoinjectors for rheumatoid arthritis: a new European Union-approved etanercept biosimilar (Benepali®) versus etanercept (Enbrel®)-findings from a nurse survey in Europe. Rheumatol Ther. 2016;3(1):77–89.
Tischer B, Mehl A. Patients’ and nurses’ preferences for autoinjectors for rheumatoid arthritis: results of a European survey. Patient Prefer Adherence. 2018;12:1413.
Egeth M, Soosaar J, Nash P, et al. Patient and healthcare professionals preference for Brenzys vs. Enbrel autoinjector for rheumatoid arthritis: a randomized crossover simulated-use study. Adv Ther. 2017;34(5):1157–72.
Fenwick S, Thakur K, Munro D. Nurse and patient perceptions and preferences for subcutaneous autoinjectors for inflammatory joint or bowel disease: findings from a European survey. Rheumatol Ther. 2019;6(2):195–206.
Karlsdottir K, Gunnarsdottir AI, Grondal G, et al. A patients’ perspective towards the injection devices for Humira® and Imraldi® in a nationwide switching program; 2022.
Maucksch C, Aries PM, Zinke S, Müller-Ladner U. Patient satisfaction with the etanercept biosimilar SB4 device, among rheumatoid arthritis and spondyloarthropathy patients—a German observational study. Open Rheumatol J. 2020;14(1).
Dignass A, Gisbert J, Bossa F, et al. P434 The PROPER study: interim analysis of a Pan-European real-world study of SB5 adalimumab biosimilar after transition from reference adalimumab in patients with Crohn’s disease. J Crohns Colitis. 2021;16(Suppl 1):418. https://doi.org/10.1093/ecco-jcc/jjab232.561.
Kivitz A, Cohen S, Dowd JE, et al. Clinical assessment of pain, tolerability, and preference of an autoinjection pen versus a prefilled syringe for patient self-administration of the fully human, monoclonal antibody adalimumab: the TOUCH trial. Clin Ther. 2006;28(10):1619–29.
EMA. Benepali summary of product characteristics. https://www.ema.europa.eu/en/documents/product-information/benepali-epar-product-information_en.pdf. Date accessed: 14 Jun 2022.
EMA. Imraldi summary of product characteristics. Accessed Jun-14, 2022. https://www.ema.europa.eu/en/documents/product-information/imraldi-epar-product-information_en.pdf. Date accessed: 14 Jun 2022.
EMA. Humira summary of product characteristics. https://www.ema.europa.eu/en/documents/product-information/humira-epar-product-information_en.pdf. Date accessed: 15 Jun 2022
EMA. Enbrel summary of product characteristics. https://www.ema.europa.eu/en/documents/product-information/enbrel-epar-product-information_en.pdf. Date accessed: 15 Jun 2022.
Losi S, Berra CCF, Fornengo R, Pitocco D, Biricolti G, Federici MO. The role of patient preferences in adherence to treatment in chronic disease: a narrative review. Drug Target Insights. 2021;15:13–20. https://doi.org/10.33393/dti.2021.2342.
Acknowledgements
Medical writing support was provided by SFL Regulatory Affairs and Scientific Communications, and funded by Samsung Bioepis Co., Ltd.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Funding for medical writing was sponsored by Samsung Bioepis Co., Ltd.
Conflict of Interest
H.C. received consultancy/advisory boards fees, lecturing/research support/education support from MSD, Lilly, AbbVie, Pfizzer, Gebro, BMS, Roche, Sanofi, Novartis, UCB, Celgene, Amgen, Biogen, Khern, Galapagos, Fresenius, and Chiesi. D.Y. declares no conflict of interest to disclose. F.C. received consultancy/lecturing/research support/education support from AbbVie, Amgen, AstraZeneca, Biogen, Celltrion, Galapagos, Gilead, GlaxoSmithKline, Janssen, MSD, Nestle Health Sciences, Norgine, Pfizer, Pharmacosmos, Samsung Bioepis, Shield Therapeutics, Takeda, and Vifor. Y.B. has received consulting/advisory board fees from AbbVie, Amgen, Biogaran, Biogen, Boehringer Ingelheim, Celltrion, Ferring, Fresenius Kabi, Gilead, Hospira, Iterative Scopes, Janssen, Lilly, Mayoli Spindler, Merck, MSD, Norgine, Pfizer, Roche, Sandoz, Sanofi, Shire, Takeda, Tillotts, and UCB. A.A. has received consulting/advisory board fees from AbbVie, Allergan, Amgen, Arena, Biogen, Bristol-Myers Squibb, Celgene, Celltrion, Eli-Lilly, Ferring, Galapagos, Gilead, Janssen, MSD, Mylan, Pfizer, Protagonist Therapeutics, Roche, Samsung Bioepis, Sandoz, and Takeda; speaker’s fees from AbbVie, Amgen, Arena, Biogen, Bristol-Myers Squibb, Eli-Lilly, Ferring, Galapagos, Gilead, Janssen, MSD, Novartis, Pfizer, Roche, Samsung Bioepis, Sandoz, Takeda, and Tigenix; research support from MSD, Takeda, Pfizer, and Biogen. J.K. is an employee of Samsung Bioepis.
Ethics Approval
This review is based on previously conducted studies and does not contain any studies with human participants or animals performed by the author.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Data Availability
Not applicable.
Code Availability
Not applicable.
Author Contributions
HC, DY, JRFC, UB, AA, DT and JK contributed to the conception, drafts, and final version of this article, and gave approval of the version to be published.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Corominas, H., Young, D., Cummings, J.R.F. et al. Healthcare Professional (HCP) and Patient Usability Evaluation and Preferences of Two Auto-injector Devices for Self-Injection of Biosimilars, SB4 and SB5: A Literature Review. Clin Drug Investig 43, 579–593 (2023). https://doi.org/10.1007/s40261-023-01284-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-023-01284-5