Abstract
Background
Serplulimab is a potential valuable therapy, while patients, physicians, and decision-makers are uncertain about the cost-effectiveness of this novel drug and its corresponding reasonable price. This study aimed to simulate the price at which serplulimab was cost-effective as first-line therapy for United States (US) and Chinese extensive-stage small-cell lung cancer (ES-SCLC) patients.
Methods
In this economic evaluation, a partitioned survival model was constructed from the perspective of US and Chinese payers. Baseline characteristics of patients and critical clinical data were obtained from ASTRUM-005. Costs and utilities were collected from open-access databases and published literature. Cumulative costs (in US dollars), life years, quality-adjusted life years (QALYs), and incremental cost-effectiveness ratios (ICERs) were measured and compared. Price simulation was conducted to inform the pricing strategy at the given willingness-to-pay (WTP) threshold. The robustness of the model was assessed via sensitivity analyses and scenario analyses; subgroup analyses were also included.
Results
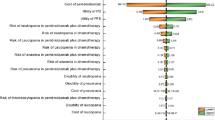
Base-case analysis indicated that serplulimab ($818.16/100 mg) would be cost-effective in the US at the WTP threshold of $150,000, with improved effectiveness of 0.61 QALYs and an additional cost of $64,918 (ICER $106,757). Serplulimab ($818.16/100 mg, patient assistance program considered) was cost-effective in China, with improved effectiveness of 0.58 QALYs and an increased overall cost of $19,369 (ICER $33,392). The price simulation results indicated that serplulimab was favored in the US when the price was less than $762.11/100 mg and $1261.57/100 mg at the WTP threshold of $100,000 and $150,000, respectively; it was cost-effective at the WTP threshold of $38,184 when the price was less than $373.37/100 mg in China. Sensitivity analyses revealed that the above results were stable. Subgroup analysis results indicated an overall trend for subgroups with better survival advantages to have a higher probability of cost-effectiveness, despite serplulimab not being cost-effective in some subgroups.
Conclusions
Serplulimab might be a valuable and cost-effective therapy in both the US and China. The evidence-based pricing strategy provided by this study could benefit decision-makers in making optimal decisions and clinicians in general clinical practice. More evidence about the budget impact and affordability for patients is needed.



Similar content being viewed by others
References
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660.
Rudin CM, Ismaila N, Hann CL, et al. Treatment of small-cell lung cancer: American Society of clinical oncology endorsement of the American College of chest physicians guideline. J Clin Oncol. 2015;33(34):4106–11. https://doi.org/10.1200/JCO.2015.63.7918.
Byers LA, Rudin CM. Small cell lung cancer: where do we go from here? Cancer. 2015;121(5):664–72. https://doi.org/10.1002/cncr.29098.
Farago AF, Keane FK. Current standards for clinical management of small cell lung cancer. Transl Lung Cancer Res. 2018;7(1):69–79. https://doi.org/10.21037/tlcr.2018.01.16.
Socinski MA, Smit EF, Lorigan P, et al. Phase III study of pemetrexed plus carboplatin compared with etoposide plus carboplatin in chemotherapy-naive patients with extensive-stage small-cell lung cancer. J Clin Oncol. 2009;27(28):4787–92. https://doi.org/10.1200/JCO.2009.23.1548.
Wang J, Zhou C, Yao W, et al. Adebrelimab or placebo plus carboplatin and etoposide as first-line treatment for extensive-stage small-cell lung cancer (CAPSTONE-1): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2022;23(6):739–47. https://doi.org/10.1016/S1470-2045(22)00224-8.
Horn L, Mansfield AS, Szczesna A, et al. First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N Engl J Med. 2018;379(23):2220–9. https://doi.org/10.1056/NEJMoa1809064.
Liu SV, Reck M, Mansfield AS, et al. Updated overall survival and PD-L1 subgroup analysis of patients with extensive-stage small-cell lung cancer treated with atezolizumab, carboplatin, and etoposide (IMpower133). J Clin Oncol. 2021;39(6):619–30. https://doi.org/10.1200/JCO.20.01055.
Goldman JW, Dvorkin M, Chen Y, et al. Durvalumab, with or without tremelimumab, plus platinum-etoposide versus platinum-etoposide alone in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): updated results from a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2021;22(1):51–65. https://doi.org/10.1016/S1470-2045(20)30539-8.
Paz-Ares L, Chen Y, Reinmuth N, et al. Durvalumab, with or without tremelimumab, plus platinum-etoposide in first-line treatment of extensive-stage small-cell lung cancer: 3-year overall survival update from CASPIAN. ESMO Open. 2022;7(2): 100408. https://doi.org/10.1016/j.esmoop.2022.100408.
Rudin CM, Awad MM, Navarro A, et al. Pembrolizumab or placebo plus etoposide and platinum as first-line therapy for extensive-stage small-cell lung cancer: randomized, double-blind, phase III KEYNOTE-604 study. J Clin Oncol. 2020;38(21):2369–79. https://doi.org/10.1200/JCO.20.00793.
Lee A. Serplulimab: first approval. Drugs. 2022;82(10):1137–41. https://doi.org/10.1007/s40265-022-01740-0.
Qin S, Li J, Zhong H, et al. Efficacy and safety of HLX10, a novel anti-PD-1 antibody, in patients with previously treated unresectable or metastatic microsatellite instability-high or mismatch repair-deficient solid tumors: a single-arm, multicenter, phase 2 study. J Clin Oncol. 2021;39(15):2566–2566. https://doi.org/10.1200/JCO.2021.39.15_suppl.2566.
Cheng Y, Han L, Wu L, et al. Serplulimab, a novel anti-PD-1 antibody, plus chemotherapy versus chemotherapy alone as first-line treatment for extensive-stage small-cell lung cancer: an international randomized phase 3 study. J Clin Oncol. 2022;40(16):8505–8505. https://doi.org/10.1200/JCO.2022.40.16_suppl.8505.
Cheng Y, Han L, Wu L, et al. Effect of first-line serplulimab vs placebo added to chemotherapy on survival in patients with extensive-stage small cell lung cancer: the ASTRUM-005 randomized clinical trial. JAMA. 2022;328(12):1223–32. https://doi.org/10.1001/jama.2022.16464.
National Comprehensive Cancer Network. NCCN Guidelines for Small Cell Lung Cancer. https://www.nccn.org/profile?ReturnURL=https://www.nccn.org/professionals/physician_gls/pdf/sclc.pdf. Accessed 28 August, 2022
Zhou K, Zhou J, Huang J, et al. Cost-effectiveness analysis of atezolizumab plus chemotherapy in the first-line treatment of extensive-stage small-cell lung cancer. Lung Cancer. 2019;130:1–4. https://doi.org/10.1016/j.lungcan.2019.01.019.
Ding D, Hu H, Li S, et al. Cost-effectiveness analysis of durvalumab plus chemotherapy in the first-line treatment of extensive-stage small cell lung cancer. J Natl Compr Canc Netw. 2021. https://doi.org/10.6004/jnccn.2020.7796.
Tong YH, Ding HY, Xin WX, et al. Cost-effectiveness analysis of durvalumab plus etoposide: platinum in the first-line therapy of extensive stage small-cell lung cancer from the Chinese payers’ perspective. Tumori. 2022;108(1):33–9. https://doi.org/10.1177/0300891620985309.
Liu G, Kang S. Cost-effectiveness of adding durvalumab to first-line chemotherapy for extensive-stage small-cell lung cancer in China. Expert Rev Pharmacoecon Outcomes Res. 2022;22(1):85–91. https://doi.org/10.1080/14737167.2021.1888717.
Li L, Wang H, Chen X, Li W, Cui J. First-line atezolizumab plus chemotherapy in treatment of extensive small cell lung cancer: a cost-effectiveness analysis from China. Chin Med J (Engl). 2019;132(23):2790–4. https://doi.org/10.1097/CM9.0000000000000536.
Redsenol. The price and the PAP of Serplulimab. https://redsenol.com/28821.html. Accessed 29 August, 2022
Husereau D, Drummond M, Augustovski F, et al. Consolidated health economic evaluation reporting standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. Value Health. 2022;25(1):3–9. https://doi.org/10.1016/j.jval.2021.11.1351.
Goulart B, Ramsey S. A trial-based assessment of the cost-utility of bevacizumab and chemotherapy versus chemotherapy alone for advanced non-small cell lung cancer. Value Health. 2011;14(6):836–45. https://doi.org/10.1016/j.jval.2011.04.004.
Wu B, Chen H, Shen J, Ye M. Cost-effectiveness of adding rh-endostatin to first-line chemotherapy in patients with advanced non-small-cell lung cancer in China. Clin Ther. 2011;33(10):1446–55. https://doi.org/10.1016/j.clinthera.2011.09.016.
Williams C, Lewsey JD, Mackay DF, Briggs AH. Estimation of survival probabilities for use in cost-effectiveness analyses: a comparison of a multi-state modeling survival analysis approach with partitioned survival and markov decision-analytic modeling. Med Decis Making. 2017;37(4):427–39. https://doi.org/10.1177/0272989X16670617.
Ishak KJ, Kreif N, Benedict A, Muszbek N. Overview of parametric survival analysis for health-economic applications. Pharmacoeconomics. 2013;31(8):663–75. https://doi.org/10.1007/s40273-013-0064-3.
Su D, Wu B, Shi L. Cost-effectiveness of atezolizumab plus bevacizumab vs sorafenib as first-line treatment of unresectable hepatocellular carcinoma. JAMA Netw Open. 2021;4(2): e210037. https://doi.org/10.1001/jamanetworkopen.2021.0037.
Dieleman JL, Cao J, Chapin A, et al. US health care spending by payer and health condition, 1996–2016. JAMA. 2020;323(9):863–84. https://doi.org/10.1001/jama.2020.0734.
Guoen L. Chinese guidelines for pharmacoeconomics evaluation 2020. China Market Press; 2020
National Bureau of Statistics. 2021 Statistical Bulletin of National Economic and Social Development. http://www.stats.gov.cn/xxgk/jd/sjjd2020/202202/t20220228_1827972.html. Accessed 25 March, 2022
National Institute for Clinical Excellence. Developing NICE guidelines: the manual. www.nice.org.uk/process/pmg20. Accessed 29 August, 2022
Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness–the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371(9):796–7. https://doi.org/10.1056/NEJMp1405158.
Guyot P, Ades AE, Ouwens MJ, Welton NJ. Enhanced secondary analysis of survival data: reconstructing the data from published Kaplan-Meier survival curves. BMC Med Res Methodol. 2012;12:9. https://doi.org/10.1186/1471-2288-12-9.
Kearns B, Stevenson MD, Triantafyllopoulos K, Manca A. Generalized linear models for flexible parametric modeling of the hazard function. Med Decis Making. 2019;39(7):867–78. https://doi.org/10.1177/0272989X19873661.
The National Institute for Health and Care Excellence. NICE DSU technical support document 21: Flexible Methods for Survival Analysis. https://www.sheffield.ac.uk/sites/default/files/2022-02/TSD21-Flex-Surv-TSD-21_Final_alt_text.pdf. Accessed 3 April, 2022
Federico PV, Kurt M, Zhang L, et al. Heterogeneity in survival with immune checkpoint inhibitors and its implications for survival extrapolations: a case study in advanced melanoma. MDM Policy Pract. 2022;7(1):23814683221089660. https://doi.org/10.1177/23814683221089659.
MENET. MENET.com.cn. https://www.menet.com.cn/. Accessed 25 March, 2022
Yaoch. YAOZH.com. https://www.yaozh.com/. Accessed 25 March, 2022
Centers for Medicare & Medicaid Services. 2022 ASP Drug Pricing Files. https://www.cms.gov/medicare/medicare-part-b-drug-average-sales-price/2022-asp-drug-pricing-files. Accessed 28 August, 2022
Centers for Medicare & Medicaid Services. 2022 Physician Fee Schedule. https://www.cms.gov/medicare/physician-fee-schedule/search. Accessed 28 August, 2022
Amiri-Kordestani L, Wilkerson J, Balasubramaniam S, Bates SE, Fojo AT. Difference between duration of treatment (DOT) and progression-free survival (PFS) as a marker of unbalanced censoring. J Clin Oncol. 2012;30(15):2548–2548. https://doi.org/10.1200/jco.2012.30.15_suppl.2548.
Shao T, Ren Y, Zhao M, Tang W. Cost-effectiveness analysis of camrelizumab plus chemotherapy as first-line treatment for advanced squamous NSCLC in China. Front Public Health. 2022. https://doi.org/10.3389/fpubh.2022.912921.
Rui M, Fei Z, Wang Y, et al. Cost-effectiveness analysis of sintilimab + chemotherapy versus camrelizumab + chemotherapy for the treatment of first-line locally advanced or metastatic nonsquamous NSCLC in China. J Med Econ. 2022;25(1):618–29. https://doi.org/10.1080/13696998.2022.2071066.
Bullement A, Nathan P, Willis A, et al. Cost effectiveness of avelumab for metastatic merkel cell carcinoma. Pharmacoecon Open. 2019;3(3):377–90. https://doi.org/10.1007/s41669-018-0115-y.
Kuznik A, Smare C, Chen CI, et al. Cost-effectiveness of cemiplimab versus standard of care in the united states for first-line treatment of advanced non-small cell lung cancer with programmed death-ligand 1 expression >/=50. Value Health. 2022;25(2):203–14. https://doi.org/10.1016/j.jval.2021.08.009.
National Institute for Health and Clinical Excellence. Atezolizumab with carboplatin and etoposide for untreated extensive-stage small-cell lung cancer. https://www.nice.org.uk/guidance/ta638/evidence. Accessed 28 August, 2022
Vedadi A, Shakik S, Brown MC, et al. The impact of symptoms and comorbidity on health utility scores and health-related quality of life in small cell lung cancer using real world data. Qual Life Res. 2021;30(2):445–54. https://doi.org/10.1007/s11136-020-02615-1.
Nafees B, Lloyd AJ, Dewilde S, Rajan N, Lorenzo M. Health state utilities in non-small cell lung cancer: an international study. Asia Pac J Clin Oncol. 2017;13(5):e195–203. https://doi.org/10.1111/ajco.12477.
Li Y, Chen X, Shen Z, et al. Electrolyte and acid-base disorders in cancer patients and its impact on clinical outcomes: evidence from a real-world study in China. Ren Fail. 2020;42(1):234–43. https://doi.org/10.1080/0886022X.2020.1735417.
Tolley K, Goad C, Yi Y, et al. Utility elicitation study in the UK general public for late-stage chronic lymphocytic leukaemia. Eur J Health Econ. 2013;14(5):749–59. https://doi.org/10.1007/s10198-012-0419-2.
Hatswell AJ, Bullement A, Schlichting M, Bharmal M. What is the impact of the analysis method used for health state utility values on QALYs in oncology? A simulation study comparing progression-based and time-to-death approaches. Appl Health Econ Health Policy. 2021;19(3):389–401. https://doi.org/10.1007/s40258-020-00620-6.
Enstone A, Greaney M, Povsic M, et al. The economic burden of small cell lung cancer: a systematic review of the literature. Pharmacoecon Open. 2018;2(2):125–39. https://doi.org/10.1007/s41669-017-0045-0.
Mor V, Wagner TH, Levy C, et al. Association of expanded VA hospice care with aggressive care and cost for veterans with advanced lung cancer. JAMA Oncol. 2019;5(6):810–6. https://doi.org/10.1001/jamaoncol.2019.0081.
Wu B, Li T, Cai J, Xu Y, Zhao G. Cost-effectiveness analysis of adjuvant chemotherapies in patients presenting with gastric cancer after D2 gastrectomy. BMC Cancer. 2014;14:984. https://doi.org/10.1186/1471-2407-14-984.
Zhu Y, Hu H, Ding D, et al. First-line pembrolizumab plus chemotherapy for extensive-stage small-cell lung cancer: a United States-based cost-effectiveness analysis. Cost Eff Resour Alloc. 2021;19:1. https://doi.org/10.1186/s12962-021-00329-w.
Zhang L, Hang Y, Liu M, Li N, Cai H. First-line durvalumab plus platinum-etoposide versus platinum-etoposide for extensive-stage small-cell lung cancer: a cost-effectiveness analysis. Front Oncol. 2020. https://doi.org/10.3389/fonc.2020.602185.
Liu Q, Luo X, Yi L, Zeng X, Tan C. First-line chemo-immunotherapy for extensive-stage small-cell lung cancer: a united states-based cost-effectiveness analysis. Front Oncol. 2021. https://doi.org/10.3389/fonc.2021.699781.
Kang S, Wang X, Zhang Y, et al. First-line treatments for extensive-stage small-cell lung cancer with immune checkpoint inhibitors plus chemotherapy: a network meta-analysis and cost-effectiveness analysis. Front Oncol. 2021;11:740091–740091. https://doi.org/10.3389/fonc.2021.740091.
Wang Y, Rui M, Yang L, et al. Economic evaluation of first-line atezolizumab for extensive-stage small-cell lung cancer in the US. Front Public Health. 2021. https://doi.org/10.3389/fpubh.2021.650392.
Lin S, Luo S, Gu D, et al. First-line durvalumab in addition to etoposide and platinum for extensive-stage small cell lung cancer: a US-basedcost-effectiveness analysis. Oncologist. 2021;26(11):e2013–20. https://doi.org/10.1002/onco.13954.
Liu Q, Tan C, Yi L, et al. Cost-effectiveness analysis of pembrolizumab plus chemotherapy as first-line therapy for extensive-stage small-cell lung cancer. PLoS ONE. 2021;16(11): e0258605. https://doi.org/10.1371/journal.pone.0258605.
Ionova Y, Vuong W, Sandoval O, et al. Cost-effectiveness analysis of atezolizumab versus durvalumab as first-line treatment of extensive-stage small-cell lung cancer in the USA. Clin Drug Investig. 2022;42(6):491–500. https://doi.org/10.1007/s40261-022-01157-3.
Karve SJ, Price GL, Davis KL, et al. Comparison of demographics, treatment patterns, health care utilization, and costs among elderly patients with extensive-stage small cell and metastatic non-small cell lung cancers. BMC Health Serv Res. 2014;14:555. https://doi.org/10.1186/s12913-014-0555-8.
Choudhury NJ, Riely GJ. Serplulimab with chemotherapy in extensive-stage SCLC. JAMA. 2022;328(12):1205–7. https://doi.org/10.1001/jama.2022.16442.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Taihang Shao, Mingye Zhao, Leyi Liang, and Wenxi Tang declare that they have no conflicts of interest that might be relevant to the contents of this article.
Author contributions
TS is the corresponding author. TS had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: All the authors. Acquisition, analysis, or interpretation of data: TS, MZ, LL. Drafting of the manuscript: TS. Critical revision of the manuscript for important intellectual content: MZ, LL, WT. Statistical analysis: TS, MZ. Obtained funding: WT. Administrative, technical, or material support: WT. Supervision: WT.
Funding
This work was sponsored by the General Program of National Natural Science Foundation of China (No. 72174207).
Role of the funder/sponsor
The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data availability statement
All data generated or analyzed during this study are included in this article and its supplementary materials.
Code availability
The models and codes for reproducing this study can be found on GitHub (https://github.com/TaihangShao/Serplulimab_drug_pricing).
Ethics approval, Consent for participation and publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shao, T., Zhao, M., Liang, L. et al. Serplulimab Plus Chemotherapy vs Chemotherapy for Treatment of US and Chinese Patients with Extensive-Stage Small-Cell Lung Cancer: A Cost-Effectiveness Analysis to Inform Drug Pricing. BioDrugs 37, 421–432 (2023). https://doi.org/10.1007/s40259-023-00586-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40259-023-00586-6