Abstract
Background and Aims
Metabolic syndrome (MetS) comprises a set of risk factors that contribute to the development of chronic and cardiovascular diseases, increasing the mortality rate. Altered lipid metabolism is associated with the development of metabolic disorders such as insulin resistance, obesity, atherosclerosis, and metabolic syndrome; however, there is a lack of knowledge about lipids compounds and the lipidic pathways associated with this condition, particularly in the Latin-American population. Innovative approaches, such as lipidomic analysis, facilitate the identification of lipid species related to these risk factors. This study aimed to assess the plasma lipidome in subjects with MetS.
Methods
This correlation study included healthy adults and adults with MetS. Blood samples were analyzed. The lipidomic profile was determined using an Agilent Technologies 1260 liquid chromatography system coupled to a Q-TOF 6545 quadrupole mass analyzer with electrospray ionization. The main differences were determined between the groups.
Results
The analyses reveal a distinct lipidomic profile between healthy adults and those with MetS, including increased concentrations of most identified glycerolipids -both triglycerides and diglycerides- and decreased levels of ether lipids and sphingolipids, especially sphingomyelins, in MetS subjects. Association between high triglycerides, waist circumference, and most differentially expressed lipids were found.
Conclusion
Our results demonstrate dysregulation of lipid metabolism in subjects with Mets, supporting the potential utility of plasma lipidome analysis for a deeper understanding of MetS pathophysiology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metabolic syndrome (MetS) is a collection of risk factors associated with the development of chronic and cardiovascular diseases. Individuals with MetS face a fivefold higher risk of developing type 2 diabetes and a three times higher risk of a heart attack or stroke [1]. The diagnosis of MetS involves three to five risk components, including dysregulation of blood pressure, central obesity, dyslipidemia, and impaired glucose metabolism [2]. The presence of even one to two components of MetS has been correlated with an increase in mortality [3], and the prevalence of MetS is estimated to be greater than 20% for the North American and Latin American populations [4, 5].
MetS components have been linked, through metabolomic studies, to over 300 metabolites found in biological fluids, primarily associated with altered glucose levels and lipids [6]. Changes in the metabolism of fatty acids and triglycerides appear to involve mechanisms inducing insulin resistance and a pro-inflammatory state. This occurs through the excessive accumulation of free fatty acids in the liver and muscle, along with the secretion of cytokines that are overexpressed in obesity [7, 8]. Furthermore, imbalances in the lipid signaling pathways controlling various cellular processes have been implicated in the development of pathological conditions such as MetS through signaling lipids such as sphingolipids, fatty acids, and eicosanoids [9].
The analysis and identification of lipids through liquid chromatography coupled with mass spectrometry (LC–MS) have been instrumental in establishing associations between lipid species and cardiometabolic risk. Multiple lipids have been linked to conditions such as obesity, hypertension, insulin resistance, type 2 diabetes, and MetS [10,11,12]. Moreover, lipidomic analysis of blood has unveiled alterations in several lipid species associated with metabolic diseases and the discovery of new lipids distinguishing normal conditions from disease states [13].
Studies have documented distinct metabolomic and lipidomic profiles associated with MetS and its components. Using lipidomic approaches, these studies have revealed different patterns of lipid alterations in individuals with MetS compared to healthy controls [6]. This analysis provides valuable insights into the specific lipid alterations associated with MetS, highlighting potential biomarkers for early detection and therapeutic targets for intervention. However, there is a lack of information concerning the Latin-American population, particularly in individuals without another associated disease. Understanding these lipidomic signatures is important for developing region-specific diagnostic tools and personalized treatment strategies for MetS in Latin America. Consequently, we aimed to identify the variations in lipidomic profiles and metabolic pathways between individuals with and without MetS by a nondirected lipidomics analysis to provide valuable insights into the metabolic pathways of MetS in the Latin-American population.
Materials and methods
Characterization of the subjects studied and sample collection
The present study utilized samples from a previous investigation conducted by Suarez-Ortegon et al. [14] to explore iron levels and their association with insulin sensitivity and type 2 diabetes in adults. The original study, conducted between 2009 and 2010, involved 245 adult subjects of both sexes who did not have systemic diseases (except for type I obesity (body mass index (BMI) ≥ 30 and < 35)), chronic communicable diseases, or infectious or inflammatory processes at the time of enrollment. This study adhered to the guidelines outlined in the Declaration of Helsinki's guidelines, received approval from the ethics committee of the University of Valle, and obtained informed consent from all participants. Additionally, participants of the study granted authorization to use their data in subsequent research.
For the present study, we selected a subpopulation of 80 subjects with serum samples stored at -80 °C in the Nutrition group´s sample bank. These samples were divided into two groups: 1. Healthy (control) group (n = 40) (HeS) consisting of adults without systemic or inflammatory diseases and lacking risk factors or characteristics of MetS; 2. MetS group (n = 40) included adults who met 3–5 criteria for diagnosing MetS. The cases of MetS were identified based on the criteria of the Harmonized definition of MetS (2), which includes: a. Elevated waist circumference: men ≥ 90 cm and women ≥ 80 cm; b. High triglycerides: ≥ 150 mg/dL (1.7 mmol/L), c. Reduced high-density lipoprotein cholesterol (HDL-C): < 40 mg/dL (1.0 mmol/L) in men; < 50 mg/dL (1.3 mmol/L) in women; d. Elevated blood pressure: systolic ≥ 130 and/or diastolic ≥ 85 mmHg, e. Elevated fasting glucose: ≥ 100 mg/dL.
The participant database and relevant anthropometric and clinical data were extracted from the previous study. Subsequently, samples were obtained from the sample bank of the Nutrition group at the Universidad del Valle in Cali, Colombia. After selecting samples for the current study, they were appropriately labeled, refrigerated, and transported to the metabolomics laboratory of the University of the Andes, MetCore, in Bogotá, Colombia, for processing.
Anthropometric and clinical information
The patients underwent a 12-h fasting period for blood sampling, blood pressure measurement and anthropometric assessment. Personal and family data was gathered through a survey. At the same time, waist circumference (WC) was measured with a metric band, height with a stadiometer, weight on a digital scale, and body fat percentage using a portable impedance meter (OMRON®). BMI was calculated by the formula weight/(height2). Systolic and diastolic pressures were measured twice using a digital sphygmomanometer (OMRON®) in the supine position in the right arm with an interval of 10 min between the two measurements. Blood samples were collected via antecubital vein puncture, with 15 mL of blood extracted into three Vacutainer® tubes without additive. Samples were transported to the laboratory in refrigerators between 4–8 °C, and within an hour, they were centrifuged at 3000 rpm to obtain serum, which was then stored at -20 °C until processing. Biochemical markers were analyzed: high-sensitivity C-reactive Protein using turbidimetry; glucose, total cholesterol, triglycerides, and HDL-C using enzymatic colorimetric assays (BioSystems SA®) and insulin by chemiluminescence (Immulite®). The homeostatic model assessment of insulin resistance (HOMA-IR) index [15] was calculated with the following formula:
Lipidomic analysis
For lipid extraction, 50 μL of serum was mixed with a combination of 175 μL of MeOH at -20 °C and 175 μL of MTBE at room temperature, vortexed at 3200 rpm for 15 min, centrifuged at 16,000 g at 24 °C for 10 min. Finally, the supernatant (upper phase containing the lipids) was taken, and 80 μL was transferred to an LC–MS vial for subsequent analysis. The lipidomic profile was determined using an Agilent Technologies 1260 liquid chromatography system coupled to a Q-TOF 6545 quadrupole mass analyzer with electrospray ionization. Five microliters of the sample extract were injected into a C18 column (InfinityLab Poroshell 120 EC-C18 (150 × 3.0 mm, 2.7 μm)). Liquid chromatography separation was performed at 60 °C using a mobile phase consisting of 10 mM of formate and 0.1% formic acid in ACN-H2O (60:40) (Phase A) and 10 mM formate and 0.1% formic acid in IPA-ACN (90:10) (Phase B) with a flow constant of 0.5 mL/min. The elution gradient varied from 15 to 99% B in 11.5. The gradient was maintained for 0.5 min at 99% before the gradient returned to its initial conditions and was kept constant for 6 min to ensure re-equilibration of the column. The data were collected in positive and negative ESI ionization modes in separate runs, operated in full scan mode from 100 to 1700 m/z. Throughout the analysis, two masses of reference: m/z 121.0509 (C5H4N4) and m/z 922.0098 (C18H18O6N3P3F24) for the positive mode of ionization and m/z 112.9856 (C2O2F3(NH4)) and m/z 1033.9881 (C18H18O6N3P3F24) for the negative ionization mode. Five iterative-MS/MS runs were performed using a QC sample for both ion modes at the end of the analytical run. The iterative-MS/MS runs were set with a collision energy of 20 and 40 eV.
Quality control samples
The quality control (QC) samples were prepared by mixing equal volumes of each sample. First, the QC samples were analyzed following the procedures described above. Then, several QC runs were performed to determine the reproducibility of the sample preparation and the stability of the analytical platform used until the analytical system was equilibrated. After that, the QC samples were analyzed for every 10 randomized samples.
Data processing and analysis
The data are presented as the mean ± standard deviation for the subjects' characteristics. Statistical analyses were performed using IBM SPSS 25.0. The differences between the two groups were analyzed using the independent t-test (parametric distribution) for means with continuous data and the chi-squared test for categorical data. A value of p < 0.05 was defined as statistically significant.
For lipidomic analysis, the significant differences between the serum samples of both groups were evaluated by univariate (UVA) and multivariate statistical analysis (MVA). The UVA was performed using MATLAB (7.10.0 MathWorks, Inc., Natick), and the MVA was performed employing MatLab (7.10.0 Mathworks, Inc., Natick). First, data normality was verified by evaluating the Kolmogorov–Smirnov-Lillefors and Shapiro—Wilk tests and the variance ratio by Levene's test. Next, the p-value was determined by parametric (unpaired t-test) or non-parametric (Mann—Whitney U test) tests with a Benjamini—Hochberg False Discovery Rate posthoc correction (FDR). MVA was performed using SIMCA-P + 16.0 software (Umetrics, Umea, Sweden), in which an unsupervised principal component analysis (PCA) was performed to observe the unsupervised distribution of the analyzed samples. Then, a supervised orthogonal projection to latent structures discriminant analysis (OPLS-DA) model was performed to select the molecular characteristics responsible for separating the groups (HeS group and Mets group). For this comparison, the statistically significant molecular markers were chosen with the following requirements: 1) UVA: p < 0.05 and 2) MVA: variance important in projection (VIP) > 1 with jack-knife confidence interval (JK) not included 0.
To compare the effect of the components related to MetS to the explanation of the intersubject variability, one-way analysis of variance (ANOVA) and analysis of covariance were performed to determine the significant differences between the components of the MetS and the lipids identified adjusted for age and sex as covariates, a corrected p < 0.0004 was considered statistically significant for this analysis. The correlations of the latter with obesity, BMI, insulin, and HOMA-IR were also determined. A corrected p < 0.002 was considered statistically significant for this analysis. All p values obtained were corrected for multiple comparisons using the Bonferroni fit test [16, 17].
Lipid annotation
The lipids obtained in the LC–MS analysis were identified with three identification tools: molecular formula generator, available online databases using the CEU mass mediator tool, and MS/MS analysis. First, the statistically significant molecular features were tentatively identified based on the MS1 data using our online tool CEU Mass Mediator (http://ceumass.eps.uspceu.es/mediator/) through a search in METLIN databases (http://metlin.scripps.edu), KEGG (http://genome.jp/kegg), lipid MAPS (http://lipidMAPS.org), and HMDB (http://hmdb.ca). The tentative assignment was performed based on accurate mass with a maximum mass error tolerance of 10 ppm, the isotopic pattern distribution in the molecular formula generated in the experimental data, the possibility of cation and anion formation and adduct formation, and the retention time. Then, a manual MS/MS spectral interpretation was carried out comparing MS/MS fragmentation to the available spectra data in MS-DIAL, LIPID MAPS, and the Lipid Annotator software (Agilent Technologies Inc., Santa Clara, CA, USA). Finally, the identification level was assigned according to Blaženović, I. et al. [18].
Pathway analysis
The metabolic pathways were analyzed using the MetaboAnalyst 5.0 tool (http://www.metaboanalyst.ca/), which integrates two approaches: pathway enrichment analysis and pathway topology analysis. In addition, a list of compound names of the identified significant lipids was included and processed using the "Homo sapiens" library. [19]. The selected metabolic pathways had a higher impact on the analysis.
Results
Table 1 presents the characteristics of the study participants, comprising 40 individuals with MetS and 40 without MetS. No significant differences in age and sex were observed, although there was a higher proportion of women in healthy subjects’ group. Following diagnostic criteria, participants with MetS exhibited higher values in blood pressure, waist circumference, BMI, insulin, glucose, triglycerides (TG), HOMA-IR, high-sensitivity C-reactive protein, and lower HDL cholesterol than the control group. However, the two groups had no significant differences in low-density lipoprotein (LDL) or cholesterol.
The reproducibility of the analytical platforms was assessed by grouping the quality control (QC) samples through Principal Component Analysis (PCA), ensuring data quality and the preservation of the biological variation across the experimental data (Fig. 1). The PCA model exhibited a tendency to separate the samples from healthy subjects and those with MetS in the score plot.
PCA score plots for global lipidomics of both polarities. (MetS: blue points,HeS: green points), quality control samples: gray dots) A. LC-QTOF-MS ( +): R2 (cum):0.901, Q2 (cum): 0.703; B. LC-QTOF-MS (-): R2 (cum): 0.896, Q2 (cum): 0.6227. OPLS-DA MODELS. Lipidomics of the MetS (blue points) and HeS (green points) groups. C. OPLS-DA in ESI + , LC-QTOF-MS ( +): R2(cum):0.804, Q2 (cum): 0.681, cv-anova: 1.99e-12; D OPLS-DA in ESI-, LC-QTOF-MS(-): R2(cum): 0.707, Q.2 (cum): 0.609, cv-anova: 5.211e-9
Both unsupervised (PCA) and supervised statistical analyses (OPLS-DA) demonstrated a distinct separation between the groups of healthy subjects (depicted as green points) and the subjects with MetS (represented as blue points). Clear separations were achieved from the orthogonal predictive components of the OPLS-DA model between the two groups, with acceptable values of predictive variance (R2) (LC-QTOF-MS ( +): R2(cum):0.804, LC-QTOF-MS(-): R2(cum): 0.707), predictive ability (Q2) (LC-QTOF-MS ( +): Q2 (cum): 0.681; LC-QTOF-MS(-): Q2 (cum): 0.609) and p-value in the CV-ANOVA tests (LC-QTOF-MS ( +): cv-ANOVA: 1.99e-12; LC-QTOF-MS(-): cv-ANOVA: 5.211e-9) indicating that the OPLS-DA models are not overfitting (Fig. 1).
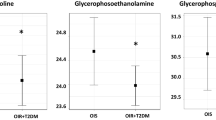
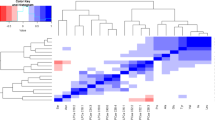
A total of 100 lipids exhibited statistical differences between MetS and HeS through the MS-based platforms: 12 lipids by LC–MS (-) (Table S1) and 88 lipids by LC–MS ( +) (Table S2). The significant lipids belonged to various classes, including glycerolipids (di-acylglycerols (DG) and triglyceride (TG)); glycerophospholipids (lysophosphatidylcholines (LPC), phosphatidylcholine (PC) and ether phospholipids); and sphingolipids (sphingomyelins (SM). Glycerolipids showed increased levels in the MetS group, whereas glycerophospholipids and sphingolipids exhibited decreased in the MetS group compared to HeS group. After adjusting for sex and age, nineteen lipids showed distinct expression patterns between MetS and the HeS group (Table 2).
Furthermore, we sought to assess if any of the 100 identified lipids exhibited individual correlations with components of Metabolic Syndrome. Our analysis revealed that thirty-nine lipids were identified as correlated with one or more MetS components (Table S3). Additionally, to investigate if variations in lipid expression related to MetS components persisted after accounting for age and sex differences between groups, we conducted an adjustment. The results showed that 18 lipids continued to exhibit differential expression between groups, even after adjusting for age and sex.
Table 3 presents the list of lipids associated with each MetS component. Among the 18 lipids linked to individual components of MetS, eleven glycerolipids notably contributed to the differentiation between the groups (VIP > 1). Notably, this analysis revealed that ninety-five percent of the lipids associated with MetS components were linked to the triglyceride (TG) component, and all identified TGs had higher expression in subjects with MetS. The waist circumference component showed associations with ten identified lipids, nine exhibiting higher expression in subjects with MetS than HeS. In comparison, one lipid (PC O-44:5 // PC P-44:4) showed lower expression in the MetS group. The HDL and systolic blood pressure components were associated with three and two lipids, all of which had higher expression in subjects with MetS compared to healthy controls.
Given the well-established role of obesity and insulin resistance in Metabolic Syndrome development, we calculated correlations between the 18 lipids exhibiting differential expression and key MetS components: BMI, insulin, and HOMA-IR. This analysis revealed nine lipids positively correlated with BMI (Table 4), 13 with insulin, and 14 with HOMA-IR. Notably, PC O-44:5 // PC P-44:4 demonstrated a negative correlation with insulin and HOMA-IR (Table 5). All lipids associated with BMI, insulin, and HOMA-IR displayed increased levels in the MetS group, except for PC O-44:5 // PC P-44:4, which exhibited a decrease.
Several lipid species, including DG (34:2), DG (38:5), and phosphatidic acid (PA) (P-32:2), demonstrated associations with at least three MetS components, including BMI, insulin, and HOMA-IR. However, DG (42:6), while associated with three MetS components, did not show correlations with BMI, insulin, or HOMA-IR.
Pathway analysis revealed that the metabolic pathways of glycerophospholipids and lipid ether metabolism were the most significantly affected, showing the highest significance and the high number of identified lipids related to these pathways. Additionally, alterations in the linoleic acid, alpha-linoleic acid, arachidonic acid, and sphingolipid pathways were observed, with fewer lipids identified (Fig. 2).
Discussion
This study revealed a distinct differentiation in the lipidomic profile between healthy adults and those with MetS. The observed differential expression of the identified lipids aligns with findings from prior research [6, 20]. Specifically, an increase in the expression of most glycerolipids, including triglycerides (TG) and diacylglycerols (DG), was consistent, while the behavior of glycerophospholipids exhibited variability [11, 21, 22].
Notably, most studies indicate a positive association between sphingolipid levels, such as ceramides and sphingomyelins and cardiovascular and metabolic diseases [23, 24]. However, in contrast to these findings, our study observed a decreased expression of sphingomyelins (SMs) in subjects with MetS.
Variability of sphingolipids levels concerning cardiometabolic diseases has been previously documented [25]. Elevated levels of SMs have been identified in obese young individuals and strongly correlated with parameters such as obesity, insulin resistance, liver function, and lipid metabolism [26]. However, reduced serum concentrations of glycerophospholipids and sphingomyelins have also been observed in patients with altered fasting glucose levels or type 2 diabetes compared to healthy controls, even after adjusting for age, sex, and BMI [27]. The variations in SM levels associated with MetS could be related to the fact that SMs can exert based on the composition of their acyl chain. For instance, studies in a murine model of obesity have shown an increase in SM C14 and a decrease in SMs C22, C22:1, and C24 in ob/ob mice compared to lean mice [28]. Other studies have correlated increased in insulin secretion with higher SMs C14:0, C22:3, and C24:4 [29], while C18:0, C20:0, C22:0, and C24:0 have been associated with greater BMI and lower insulin sensitivity [26]. In this study, the SMs contained a C24:1 fatty acid chain, exhibiting more pronounced differential expression in subjects with MetS. Notably, only SM 41:1 played a significant role in distinguishing between the groups and showed a correlation with waist circumference. However, it's important to acknowledge that the expression of these SMs might be influenced by significant variables such as sex and age. Their correlation ceased to be significant after adjusting for these covariates.
Most of the lipid species significantly associated with components of MetS in this study demonstrated strong correlations with triglycerides (TG) and waist circumference, which are robustly linked to obesity [30]. The metabolic profile in obesity and diabetes often exhibits a positive association with elevated concentrations of TG and diacylglycerols (DG) in plasma [11, 31]. High levels of DG have been implicated in the pathophysiological mechanisms underlying insulin resistance in obesity, particularly through activating the protein kinase C pathway [32]. Our study observed upregulation of all TG and DG in subjects with MetS. Specifically, DG (32:1), DG (34:1), DG (34:2), and DG (38:5), which positively correlated with BMI, have been reported in previous studies to correlate with obesity and insulin resistance [31]. Notably, DG (38:5) and DG (34:2) maintained their differential expression with three MetS components after adjustment for age and sex, and they showed positive correlations with insulin levels and the HOMA-IR index. These two DG species have been associated with different indices of insulin sensitivity in prior studies [33, 34]. DG (42:6) exhibited the highest percentage change in concentration between MetS and control groups and remained associated with three MetS components after adjusting for covariates. However, none of these components were insulin, HOMA-IR, or BMI. Notably, DG (42:6) has not been previously reported as a relevant lipid in the metabolic disorder population.
Despite Latin American men and women having the smallest waist circumference cut-off compared to their counterparts in the United States (white, black, and Hispanic populations), they exhibit a higher overall risk [35]. The prevalence of Metabolic Syndrome in Latin American countries indicates that the most frequent components of MetS are low HDL cholesterol levels (62.9%) and abdominal obesity (45.8%) [36]. The INTERHEART study observed that abdominal obesity is the most significant risk factor for cardiovascular diseases in Latin America compared to the rest of the world [37]. Colombia, in particular, stands out with a higher prevalence of elevated cholesterol [38] and high triglycerides [38] compared to other Latin American countries. This observation may explain why most lipid species found in this study are associated with waist circumference and triglycerides.
Pathway analysis (Fig. 2) revealed alterations in the metabolic pathways of ether-bound lipids and glycerophospholipids. We observed a subgroup of phospholipids linked to ether bonds that predominantly exhibited lower concentrations in subjects with Metabolic Syndrome than healthy controls. This disparity contributed to the differentiation between the two groups and was correlated with triglycerides, waist circumference, and systolic blood pressure. Notably, PA (P-32:2), PA (P-34:3), and PA (P-34:2-) showed higher concentrations in the MetS group and corresponded to ether-bound forms of phosphatidic acid. Ether lipids, classified as glycerophospholipids derived from peroxisomes, feature a hydrocarbon chain in the sn-1 position of the glycerol skeleton linked by an ether bond, unlike the more common diacylphospholipids that have an ester bond. They are further categorized into plasmanylphospholipids or plasmenylphospholipids (plasmalogens) [39]. Deficiency in ether lipids has been linked to various diseases. The ether-bound form of PA serves as the precursor for more complex forms of ether phospholipids, where the molecule attached to the phosphate group is generally choline or ethanolamine [39].
The presence of phosphatidic acid linked to ether bonds, particularly in the context of Metabolic Syndrome, has not been reported in previous studies. Among the lipids we identified, three showed concentrations positively correlated with triglyceride levels. Notably, PA (P-32:2) was the sole lipid that exhibited correlations with TG concentration and insulin and Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) levels. Phosphatidic acids play crucial roles as signaling molecules and have been implicated as modulators of insulin signaling. Elevated levels of PAs, especially those containing C16:0 acids, as observed in this study, have been associated with alterations in insulin function and contribute to insulin resistance [40].
In the context of metabolic diseases, the levels of lipids bound to ether bonds can exhibit variations. For instance, Graessler et al. identified a pattern of decreased levels of ether-bound phosphatidylcholines (PCs) that correlated with BMI and hypertension. A comparison between obese and nonobese twins revealed a more significant reduction in ether-bound lipids among obese twins compared to their nonobese counterparts [41]. This finding aligns with the observations in our study, where we noted reduced levels of all ether-bound lipids derived from phosphocholines and phosphoethanolamines. Notably, compounds like PC (O-34:3) were negatively correlated with hypertension, BMI, and insulin resistance, consistent with the results reported by Graessler et al. in 2009. [42].
Lipids bound by ether bonds are ubiquitous in most cell membranes, contributing to various essential functions such as mediating membrane dynamics and structure, acting as storage molecules for polyunsaturated fatty acids and lipid mediators, and serving as endogenous antioxidants [43]. Subjects with elevated triglycerides often exhibit low levels of plasmalogens [44]. Plasmalogens are particularly susceptible to oxidation due to the vinyl ether substituent at the sn-1 position of the glycerol main chain, making them preferential targets for oxidative damage [45]. Research indicates a decrease in plasmalogen concentration under conditions of oxidative stress, as observed in the oxidation of low-density lipoprotein (LDL) in atherosclerosis [46] and non-alcoholic steatohepatitis [47]. This decrease in plasmalogen levels found in our study might be related to oxidative stress, which also plays a significant role in the development of MetS [48].
Alterations in the metabolism of glycerophospholipids in various tissues have been documented in metabolic disorders such as obesity, insulin resistance, and atherosclerosis [49]. Variability in phosphatidylcholines (PCs), coupled with a reduction in lysophosphatidylcholines, has been linked to obesity [50], insulin resistance, and the development of type 2 diabetes [32]. In our study, we noted fluctuations in the levels of certain PCs. PC (33:2) and PC (33:1) exhibited higher concentrations in subjects with Metabolic Syndrome, showing associations with triglycerides and waist circumference and positive correlations with insulin and HOMA-IR. PC (33:1) also positively correlated with BMI, while PC (33:0), a discriminative factor between patient groups, displayed lower concentration.
Consistent with our findings, increased PC synthesis has been correlated with elevated diacylglycerol (DG) levels [51, 52]. Additionally, PC plays a vital role in the formation and secretion of very low-density lipoproteins and chylomicrons. The observed increase in PC levels in subjects with MetS might be associated with heightened synthesis of very low-density lipoprotein particles; this aligns with the proposed notion that increased hepatic synthesis of PC stimulates the production of very low-density lipoprotein particles [49]. Furthermore, the elevated plasma concentration of PCs has been linked to an unfavorable metabolic risk profile involving increased cholesterol and TG levels, given that around 65% of hepatic TG content appears to originate from hepatic PC [53]. However, some studies have correlated lower PC levels with cardiovascular risk factors, potentially linked to the fatty acid composition of PCs [54, 55].
LPCs are derived from the hydrolysis of PC by phospholipase A2 and can exert their biological functions by inducing cell division, releasing inflammatory factors, and promoting oxidative stress [56]. Alterations in plasma LPC levels have been reported in conditions like obesity and type 2 diabetes, with reduced LPC levels observed in healthy obese individuals and those with type 2 diabetes compared to their healthy counterparts [57]. In this study, we observed lower levels of LPC (20:4), LPC (18:1), and LPC (18:2) in the Metabolic Syndrome (MetS) group. However, when considering covariates such as sex and age, these differences lost statistical significance, suggesting that age and sex may play important roles in determining circulating LPC levels. Other studies have also identified differential LPC levels associated with age and sex [58].
Elevated phosphatidylinositols (PI) levels were also noted in our study, showing a correlation with triglyceride concentration. The relationship between PI levels and metabolic diseases has yielded varied findings in the existing literature. Animal models in experimental studies have suggested that inositol deficiency is linked to increased hepatic triglyceride accumulation [59] while supplementation with PI has been associated with improved insulin sensitivity, reduced TG concentration, and elevated high-density lipoprotein cholesterol (HDL-C) levels [60,61,62]. A study involving intraperitoneal streptozotocin found increased serum inositol and decreased hepatic inositol in rats with acute diabetes [63]. Meikle et al. reported a positive association between PI and phosphatidylserine levels in individuals with diabetes and prediabetes [64], and increases in myo-inositol levels have been documented in patients with severe heart failure [63, 65]. We observed a positive correlation of PI (32:1) with insulin and HOMA-IR, and PI (40:6) showed a positive correlation with insulin.
MetS is a complex disorder with a cluster of different factors that are not identical across individuals; however, our study has pinpointed pathways that significantly contribute to the elevation of triacylglycerol levels and increased waist circumference, particularly prevalent in our population (Fig. 3). A noteworthy discovery in our investigation is the identification of DG (34:2) and DG (38:5), two metabolites not only positively associated with MetS but also correlated with three key MetS components, higher insulin levels, HOMA-IR index, and BMI. These metabolites show potential as key molecules in understanding the pathways underlying MetS. Additionally, DG (42:6), positively associated with MetS and three of its components, represents a novel finding not previously reported as a significant lipid in individuals with MetS. This suggests that DG (42:6) could be a metabolite specifically relevant to the Latin-American population.
Lipid metabolic pathways associated with metabolic syndrome—MetS. Abdominal obesity and insulin resistance are the main mechanisms related to the alteration in lipid metabolism in the body. Plasma glucose and fatty acid levels are directly associated with dietary intake and stimulate lipogenesis pathways through various mechanisms. The subjects with MetS in this study presented an increase in the synthesis and degradation pathways of TG and DG. The increases in the TG and DG synthesis intermediates contribute to an alteration in the glycerophospholipids and sphingolipids pathways, generating a decrease in the synthesis and/or intermediates of these compounds. Abbreviations: FFA: Free Fatty acids; TG: triglycerides; PI: phosphatidylinositol; PC: phosphatidylcholine; PE: phosphatidylethanolamine; G3P: glycerol 3-phosphate; LPA: lysophosphatidic acid; PA: phosphatidic acid; DG: diacylglycerol; VLDL: very low-density lipoprotein; SM: sphingomyelin; FA: fatty acid
Limitations and perspectives
The findings from this study highlight molecules such as TG, DG, and SM as potential markers for progression in individuals with MetS. Follow-up studies are essential to investigate whether this lipidomic profile is associated with the development of complications. A potential limitation of this study is the storage time of the samples. Although these samples were appropriately preserved, and other studies have demonstrated the stability of lipids in long-term storage. However, some less stable molecules may have degraded, limiting the presentation of a complete lipidomic profile. Longitudinal studies tracking patients and their lipidomic profiles, along with the development of complications, would provide valuable insights into the utility of these biomarkers for managing adults at risk.
Conclusions
The lipidomic profile distinguishes adults with MetS from those without. Our results indicate that TG, DG, PC, and SM are crucial lipid classes reflective of the mechanisms underlying insulin resistance development through alterations in the synthesis and degradation pathways of glycerolipids and glycerophospholipids. Most of the lipids exhibiting differential levels in this study were correlated with serum insulin and HOMA-IR. These findings enhance our understanding of the metabolic pathways contributing to insulin resistance development and its physiopathology within the context of MetS. Furthermore, they suggest that an altered lipidomic profile, characterized by elevated levels of these molecules, may be associated with an inadequate progression of the disorder and an increased risk of developing complications.
Data availability
Derived data supporting the findings of this study are available from the corresponding author MM on request.
References
Stern MP, Williams K, González-Villalpando C, Hunt KJ, Haffner SM. Does the metabolic syndrome improve identification of individuals at risk of type 2 diabetes and/or cardiovascular disease?, (in eng). Diabetes Care. 2004;27(11):2676–81. https://doi.org/10.2337/diacare.27.11.2676.
Alberti KGMM et al., Harmonizing the Metabolic Syndrome. Circulation. 2009;120(16):1640–1645, 2009/10/20. doi: https://doi.org/10.1161/CIRCULATIONAHA.109.192644.
Eberly LE, et al. Metabolic syndrome: risk factor distribution and 18-year mortality in the multiple risk factor intervention trial, (in eng). Diabetes Care. 2006;29(1):123–30. https://doi.org/10.2337/diacare.29.1.123.
Escobedo J et al., Prevalence of the metabolic syndrome in Latin America and its association with sub-clinical carotid atherosclerosis: the CARMELA cross sectional study, (in eng), Cardiovasc Diabetol. 2009;8:52. doi: https://doi.org/10.1186/1475-2840-8-52.
Kolovou GD, Anagnostopoulou KK, Salpea KD, Mikhailidis DP. “The prevalence of metabolic syndrome in various populations,” (in eng). Am J Med Sci. Jun2007;333(6):362–71. https://doi.org/10.1097/MAJ.0b013e318065c3a1.
Monnerie S, Comte B, Ziegler D, Morais JA, Pujos-Guillot E, Gaudreau P. Metabolomic and Lipidomic Signatures of Metabolic Syndrome and its Physiological Components in Adults: A Systematic Review. Scientific Reports. 2020;10(1):669, 2020/01/20. doi: https://doi.org/10.1038/s41598-019-56909-7.
Miranda PJ, DeFronzo RA, Califf RM, Guyton JR. Metabolic syndrome: definition, pathophysiology, and mechanisms, (in eng). Am Heart J, 2005;149(1):33–45, 2005/01//, https://doi.org/10.1016/j.ahj.2004.07.013.
Emanuela F, Grazia M, Marco de R, Maria Paola L, Giorgio F, Marco B. Inflammation as a Link between Obesity and Metabolic Syndrome, (in eng), J Nutr Metab, 2012;2012:476380. doi: https://doi.org/10.1155/2012/476380.
Wymann MP, Schneiter R. Lipid signalling in disease. Nature Rev Mol Cell Biol. 2008;9(2):162–176, 2008/02/01. doi: https://doi.org/10.1038/nrm2335.
Yin X, et al. “Lipidomic profiling identifies signatures of metabolic risk,” (in eng). EBioMedicine. Jan2020;51:102520. https://doi.org/10.1016/j.ebiom.2019.10.046.
Ho JE, et al. “Metabolomic Profiles of Body Mass Index in the Framingham Heart Study Reveal Distinct Cardiometabolic Phenotypes,” (in eng). PLoS ONE. 2016;11(2):e0148361. https://doi.org/10.1371/journal.pone.0148361.
Kulkarni H, Mamtani M, Blangero J, Curran JE. “Lipidomics in the Study of Hypertension in Metabolic Syndrome,” (in eng). Curr Hypertens Rep. Jan2017;19(1):7. https://doi.org/10.1007/s11906-017-0705-6.
Lydic TA, Goo Y-H. “Lipidomics unveils the complexity of the lipidome in metabolic diseases,” (in eng). Clin Transl Med. 2018;7(1):4–4. https://doi.org/10.1186/s40169-018-0182-9.
Suárez-Ortegón MF, Arbeláez A, Mosquera M, Moreno-Navarrete JM, Aguilar-Plata C, Fernández-Real JM. Circulating Hepcidin Is Independently Associated with Systolic Blood Pressure in Apparently Healthy Individuals. Arch Med Res. 2015;46(6):507–513, 2015/08/01/. https://doi.org/10.1016/j.arcmed.2015.07.007.
Yero J, Iglesias Á, González D. Utilidad del índice HOMA-IR con una sola determinación de insulinemia para diagnosticar resistencia insulínica. Revista Cubana de Endocrinología, 2011;22:69–77, 08/01.
Armstrong RA. When to use the Bonferroni correction. Ophthal Physiol Optics. 2014;34(5):502–508, 2014/09/01. doi: https://doi.org/10.1111/opo.12131.
Aickin M, Gensler H. Adjusting for multiple testing when reporting research results: the Bonferroni vs Holm methods, (in eng). Am J Public Health. 1996;86(5):726–8. https://doi.org/10.2105/ajph.86.5.726.
Blaženović I, Kind T, Ji J, Fiehn O. Software Tools and Approaches for Compound Identification of LC-MS/MS Data in Metabolomics, (in eng), Metabolites. 2018;8(2), doi: https://doi.org/10.3390/metabo8020031.
Xia J, Wishart DS. Web-based inference of biological patterns, functions and pathways from metabolomic data using MetaboAnalyst, (in eng). Nat Protoc. 2011;6(6):743–60. https://doi.org/10.1038/nprot.2011.319.
Kulkarni H et al. Plasma lipidome is independently associated with variability in metabolic syndrome in Mexican American families. J Lipid Res, 2014;55(5):939–946, 2014/05/01/. https://doi.org/10.1194/jlr.M044065.
Ramakrishanan N, Denna T, Devaraj S, Adams-Huet B, Jialal I. Exploratory lipidomics in patients with nascent Metabolic Syndrome, (in eng). J Diabetes Complications. 2018;32(8):791–4. https://doi.org/10.1016/j.jdiacomp.2018.05.014.
Gong LL et al. Discovery of metabolite profiles of metabolic syndrome using untargeted and targeted LC-MS based lipidomics approach, (in eng), J Pharm Biomed Anal. 2020;177:112848, doi: https://doi.org/10.1016/j.jpba.2019.112848.
Pan W, et al. Elevation of ceramide and activation of secretory acid sphingomyelinase in patients with acute coronary syndromes, (in eng). Coron Artery Dis. 2014;25(3):230–5. https://doi.org/10.1097/mca.0000000000000079.
Majumdar I, Mastrandrea LD. Serum sphingolipids and inflammatory mediators in adolescents at risk for metabolic syndrome. Endocrine, 2012;41(3):442–449, 2012/06/01. doi: https://doi.org/10.1007/s12020-011-9589-4.
Cowart LA. Sphingolipids: players in the pathology of metabolic disease, (in eng). Trends Endocrinol Metab. 2009;20(1):34–42. https://doi.org/10.1016/j.tem.2008.09.004.
Hanamatsu H et al. Altered levels of serum sphingomyelin and ceramide containing distinct acyl chains in young obese adults. Nutrition & Diabetes. 2014;4(10):e141-e141, 2014/10/01. doi: https://doi.org/10.1038/nutd.2014.38.
Xu F, Tavintharan S, Sum CF, Woon K, Lim SC, Ong CN. “Metabolic signature shift in type 2 diabetes mellitus revealed by mass spectrometry-based metabolomics,” (in eng). J Clin Endocrinol Metab. 2013;98(6):E1060–5. https://doi.org/10.1210/jc.2012-4132.
Samad F, Hester KD, Yang G, Hannun YA, Bielawski J. Altered Adipose and Plasma Sphingolipid Metabolism in Obesity. Diabetes. 2006;55(9):2579. https://doi.org/10.2337/db06-0330.
Bergman BC, et al. “Serum sphingolipids: relationships to insulin sensitivity and changes with exercise in humans,” (in eng), American journal of physiology. Endocrinol Metab. 2015;309(4):E398–408. https://doi.org/10.1152/ajpendo.00134.2015.
Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr. 2004;79(3):379–84. https://doi.org/10.1093/ajcn/79.3.379.
Tonks KT et al. Skeletal muscle and plasma lipidomic signatures of insulin resistance and overweight/obesity in humans. Obesity. 2016;24(4):908–916, 2016/04/01. https://doi.org/10.1002/oby.21448.
Petersen MC, Shulman GI. Roles of Diacylglycerols and Ceramides in Hepatic Insulin Resistance, (in eng). Trends Pharmacol Sci. 2017;38(7):649–65. https://doi.org/10.1016/j.tips.2017.04.004.
Kopprasch S, et al. Detection of Independent Associations of Plasma Lipidomic Parameters with Insulin Sensitivity Indices Using Data Mining Methodology, (in eng). PLoS ONE. 2016;11(10):e0164173. https://doi.org/10.1371/journal.pone.0164173.
Bagheri M et al. A lipidome-wide association study of the lipoprotein insulin resistance index, (in eng), Lipids Health Dis. 2020;19(1):153. doi: https://doi.org/10.1186/s12944-020-01321-8.
Herrera VM, et al. “Interethnic differences in the accuracy of anthropometric indicators of obesity in screening for high risk of coronary heart disease,” (in eng). Int J Obes (Lond). 2009;33(5):568–76. https://doi.org/10.1038/ijo.2009.35.
Márquez-Sandoval F, Macedo-Ojeda G, Viramontes-Hörner D, Fernández Ballart JD, Salas Salvadó J, Vizmanos B. The prevalence of metabolic syndrome in Latin America: a systematic review, (in eng), Public Health Nutr, 2011;14(10):1702–13. doi: https://doi.org/10.1017/s1368980010003320.
Lanas F et al. Risk Factors for Acute Myocardial Infarction in Latin America. Circulation. 2007;115(9):1067–1074, 2007/03/06, doi: https://doi.org/10.1161/CIRCULATIONAHA.106.633552.
Miranda JJ et al. Major cardiovascular risk factors in Latin America: a comparison with the United States. The Latin American Consortium of Studies in Obesity (LASO), (in eng), PLoS One. 2013;8(1):e54056. doi: https://doi.org/10.1371/journal.pone.0054056.
Dean JM, Lodhi IJ. Structural and functional roles of ether lipids, (in eng). Protein Cell. 2018;9(2):196–206. https://doi.org/10.1007/s13238-017-0423-5.
Zhang C, et al. Inhibited Insulin Signaling in Mouse Hepatocytes Is Associated with Increased Phosphatidic Acid but Not Diacylglycerol *. J Biol Chem. 2015;290(6):3519–28. https://doi.org/10.1074/jbc.M114.602789.
Pietiläinen KH et al. Acquired obesity is associated with changes in the serum lipidomic profile independent of genetic effects--a monozygotic twin study, (in eng), PLoS One. 2007;2(2):e218. doi: https://doi.org/10.1371/journal.pone.0000218.
Graessler J, Schwudke D, Schwarz PE, Herzog R, Shevchenko A, Bornstein SR. Top-down lipidomics reveals ether lipid deficiency in blood plasma of hypertensive patients, (in eng), PLoS One. 2009;4(7):e6261. doi: https://doi.org/10.1371/journal.pone.0006261.
da Silva TF, Sousa VF, Malheiro AR, Brites P. The importance of ether-phospholipids: A view from the perspective of mouse models. Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease. 2012;1822(9):1501–1508, 2012/09/01/. https://doi.org/10.1016/j.bbadis.2012.05.014.
Brosche T, Platt D. The biological significance of plasmalogens in defense against oxidative damage, (in eng). Exp Gerontol. 1998;33(5):363–9. https://doi.org/10.1016/s0531-5565(98)00014-x.
Brosche T. Plasmalogen levels in serum from patients with impaired carbohydrate or lipid metabolism and in elderly subjects with normal metabolic values, (in eng). Arch Gerontol Geriatr. 2001;32(3):283–94. https://doi.org/10.1016/s0167-4943(01)00105-4.
Rasmiena AA, et al. Plasmalogen modulation attenuates atherosclerosis in ApoE- and ApoE/GPx1-deficient mice, (in eng). Atherosclerosis. 2015;243(2):598–608. https://doi.org/10.1016/j.atherosclerosis.2015.10.096.
Ikuta A, et al. Composition of plasmalogens in serum lipoproteins from patients with non-alcoholic steatohepatitis and their susceptibility to oxidation, (in eng). Clin Chim Acta. 2019;493:1–7. https://doi.org/10.1016/j.cca.2019.02.020.
Mahjoub S, Masrour-Roudsari J. Role of oxidative stress in pathogenesis of metabolic syndrome, (in eng), Caspian J Internal Med. 2012;3(1):386–396, Winter.
van der Veen JN, Kennelly JP, Wan S, Vance JE, Vance DE, Jacobs RL. The critical role of phosphatidylcholine and phosphatidylethanolamine metabolism in health and disease, (in eng), Biochim Biophys Acta Biomembr. 2017;1859(9 Pt B):1558–1572. doi: https://doi.org/10.1016/j.bbamem.2017.04.006.
Rauschert S, et al. Lipidomics Reveals Associations of Phospholipids With Obesity and Insulin Resistance in Young Adults, (in eng). J Clin Endocrinol Metab. 2016;101(3):871–9. https://doi.org/10.1210/jc.2015-3525.
Araki W, Wurtman RJ. Control of membrane phosphatidylcholine biosynthesis by diacylglycerol levels in neuronal cells undergoing neurite outgrowth, (in eng). Proc Natl Acad Sci U S A. 1997;94(22):11946–50. https://doi.org/10.1073/pnas.94.22.11946.
Lim P, Cornell R, Vance DE. The supply of both CDP-choline and diacylglycerol can regulate the rate of phosphatidylcholine synthesis in HeLa cells, (in eng). Biochem Cell Biol. 1986;64(7):692–8. https://doi.org/10.1139/o86-095.
van der Veen JN, Lingrell S, Vance DE. The membrane lipid phosphatidylcholine is an unexpected source of triacylglycerol in the liver, (in eng). J Biol Chem. 2012;287(28):23418–26. https://doi.org/10.1074/jbc.M112.381723.
Kulkarni H, et al. Variability in associations of phosphatidylcholine molecular species with metabolic syndrome in Mexican-American families, (in eng). Lipids. 2013;48(5):497–503. https://doi.org/10.1007/s11745-013-3781-7.
Syme C, et al. Glycerophosphocholine Metabolites and Cardiovascular Disease Risk Factors in Adolescents: A Cohort Study, (in eng). Circulation. 2016;134(21):1629–36. https://doi.org/10.1161/circulationaha.116.022993.
Liu P et al. The mechanisms of lysophosphatidylcholine in the development of diseases, (in eng), Life Sci. 2020;247:117443. doi: https://doi.org/10.1016/j.lfs.2020.117443.
Barber MN, et al. Plasma lysophosphatidylcholine levels are reduced in obesity and type 2 diabetes, (in eng). PLoS ONE. 2012;7(7):e41456. https://doi.org/10.1371/journal.pone.0041456.
Beyene HB, et al. High-coverage plasma lipidomics reveals novel sex-specific lipidomic fingerprints of age and BMI: Evidence from two large population cohort studies, (in eng). PLoS Biol. 2020;18(9):e3000870–e3000870. https://doi.org/10.1371/journal.pbio.3000870.
Pani A et al., Inositol and Non-Alcoholic Fatty Liver Disease: A Systematic Review on Deficiencies and Supplementation. Nutrients. 2020;12(11). doi: https://doi.org/10.3390/nu12113379.
Shirouchi B, et al. Dietary phosphatidylinositol prevents the development of nonalcoholic fatty liver disease in Zucker (fa/fa) rats, (in eng). J Agric Food Chem. 2008;56(7):2375–9. https://doi.org/10.1021/jf703578d.
Shimizu K, Ida T, Tsutsui H, Asai T, Otsubo K, Oku N. Anti-obesity effect of phosphatidylinositol on diet-induced obesity in mice, (in eng). J Agric Food Chem. 2010;58(21):11218–25. https://doi.org/10.1021/jf102075j.
Stamler CJ, Breznan D, Neville TA, Viau FJ, Camlioglu E, Sparks DL. Phosphatidylinositol promotes cholesterol transport in vivo, (in eng). J Lipid Res. 2000;41(8):1214–21.
Palmano KP, Whiting PH, Hawthorne JN. Free and lipid myo-inositol in tissues from rats with acute and less severe streptozotocin-induced diabetes. Biochem J. 1977;167(1):229–35. https://doi.org/10.1042/bj1670229.
Meikle PJ, et al. Plasma lipid profiling shows similar associations with prediabetes and type 2 diabetes, (in eng). PLoS ONE. 2013;8(9):e74341. https://doi.org/10.1371/journal.pone.0074341.
Deidda M et al. Metabolomic approach to profile functional and metabolic changes in heart failure. J Trans Med. 2015;13(1):297, 2015/09/12. doi: https://doi.org/10.1186/s12967-015-0661-3.
Acknowledgements
A special thanks to the original study participants for their contribution to this research. To Universidad del Valle for the financial support for the research, and the Universidad de los Andes for the contribution to the sample processing.
Funding
Open Access funding provided by Colombia Consortium. This work was financially supported by Universidad del Valle de Colombia. (Grand number 1881–2019).
Author information
Authors and Affiliations
Contributions
M.F. Serna was responsible for project development, designed the experimental approaches, performed experimental manipulations, interpreted the data, and drafted the manuscript. M.F. Suárez-Ortegón and E. Jiménez-Charris: designed the experimental approaches, interpreted the data, and critical review the manuscript. M.P. Cala: performed experimental manipulations, interpreted the data, and critical review the manuscript. I. Echeverri and M. Mosquera: were responsible for designing the conceptualization, experimental approaches, resources, methodology, interpreted the data, and critical review of the manuscript. All authors have reviewed and approved the final submitted manuscript.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights.
• Lipidomic profiles showed molecules related to MetS and its components.
• Glycerophospholipids metabolism was the most affected metabolic pathway in MetS.
• Sphingolipids showed a decrease in subjects with MetS.
• The first study showed lipidomic modification in the Colombian population with MetS.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Serna, M.F., Suarez-Ortegón, M.F., Jiménez-Charris, E. et al. Lipidomic signatures in Colombian adults with metabolic syndrome. J Diabetes Metab Disord (2024). https://doi.org/10.1007/s40200-024-01423-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40200-024-01423-5