Abstract
Chronic migraine (CM) diagnosis is nowadays based on the threshold of 15 headache days/month for three consecutive months, of which at least eight have migraine headache features. In recent years, proposals for reducing the threshold to 8 days/month have been proposed. The sole frequency parameter, however, is partial considering the variability in frequency, pain severity, associated symptoms, such as nausea, osmophobia, and photophobia, and presence of aura, but also the variable response to treatment and the association with several comorbidities. Therefore, in our opinion, a multiparameter perspective has to be taken into account that considers the underlying pathophysiology, in particular the presence of tension-type-like pain, cutaneous allodynia, and reduced pain threshold. A paradigm change in the definition of chronic migraine moves far beyond the mere 8 vs. 15 days/month, but has ethical and practical implications for treatment: should patients be treated with the most effective prophylactic drugs, i.e., monoclonal antibodies (MABs), if they enter into a new definition of CM? How should clinicians deal with treatment escalation towards MABs? What is the role of associated conditions, response to treatments, lifestyle issues, and psychological factors? And, finally, which endpoint should we use to define effectiveness? Is improvement in headache frequency enough, or should we move towards disability, quality of life, or workplace productivity?
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The definition of chronic migraine (CM) is based upon frequency of headache over a 3-month period and a proposal to move from 15 to 8 days has been made. |
Migraine is subject to variations related to frequency and clinical features which might predispose to a chronification pattern. |
The mechanism of chronification is better captured by changes in clinical features rather than headache frequency, the most evident being the presence of tension-type headache (TTH)-like pain, cutaneous allodynia, and reduced pain threshold. |
Therefore, if a revision of CM criteria is to be made, then a multiparameter approach is warranted. |
Introduction
The third version of the International Classification of Headache Disorders (ICHD-3) sets the threshold of 15 headache days/month for three consecutive months for the definition of chronic migraine (CM), provided that at least eight of these days have migraine headache features [1]. CM is a burdensome condition, associated with high level of disability, low levels of quality of life (QoL), relevant comorbidities, and increased costs [2,3,4,5,6,7]. Compared to the episodic counterpart, i.e., migraine with up to 14 days of headache per month, it has been postulated to be a much burdensome condition, associated with higher levels of disability and reduced quality of life, reduced productivity and higher unemployment status, as well as higher healthcare resource use [8,9,10,11,12,13,14,15,16,17,18,19,20,21].
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Defining the Temporal Evolution of Migraine
Different definitions of migraine severity based on frequency exist. CM is clearly defined upon the presence of 15 days of headache or more, and is recognized so by the ICHD-3, but among the so-called episodic forms, two different subgroups are sometimes defined: high-frequency episodic migraine (HFEM) and low-frequency episodic migraine (LFEM), the former being used for patients with 8–14 days/month and the latter for patients with fewer than seven. These two conditions, although not formally recognized by the ICHD-3, are of clinical interest, as the variability of migraine headache frequency constitutes an “alarm bell” for the risk of chronification. In fact, patients with 8–14 migraine headache days per month are particularly susceptible to the risk of overusing medication, a major cause of headache chronification, and cephalalgiaphobia, a peculiar feature of patients with migraine associated with anxiety, depression, and increase medication intake, which is in turn associated with the frequency of migraine episodes [22, 23]. It has, however, to be noted that such an 8-day threshold is not formal. It has been in use since middle of the decade beginning in 2010 (e.g., in 2015 in the phase 2b trial of TEV-48125 [24]), but in previous years the threshold has been set at 10 days, e.g., in the American Migraine Prevalence and Prevention Study [25].
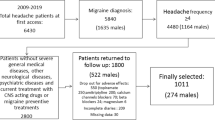
Recently, two different manuscripts suggested the inadequacy of the 15-day threshold for the definition of CM [26, 27] and suggested that 8 days/month would be a new and more adequate threshold for the definition of CM. Much of the argument behind this proposal is based on the lack of difference, regarding migraine impact, observed between patients with 8–14 and 15–23 days/month. Ishii and colleagues [27] performed a comparative analysis on a subset of records included in the American Registry for Migraine Research, a longitudinal patient registry established by the American Migraine Foundation. The authors extracted records referred to the subset of patients with migraine who were included in the registry between February 2016 and March 2020 and who completed the migraine disability assessment (MIDAS) (836 out of 1780), and divided the selected sample on the basis of migraine headache frequency: up to 7, 8–14, 15–23, and more than 24 days/month. Their results show a lack of difference between patients with 8–14 and 15–23 days for absenteeism, presenteeism, overall work productivity impairment, total activity impairment (i.e., general disability), and pain interference. No difference was shown for the MIDAS [28], which is not surprising considering that it is basically collinear to headache frequency, whereas the post hoc tests for anxiety and disability were not carried out. On the basis of these results, the authors suggest that—since no difference in the impact of migraine was observed between patients with 8–14 and 15–23 days/month—diagnosis of CM should use 8 days/month as a threshold, with the clear implication of extending the treatments that are nowadays dedicated to patients with a diagnosis of CM based upon the ICHD-3 to those patients with migraine with eight or more headaches per month.
Inadequacy of Moving the Sole Frequency Bar
Some issues related to the sole frequency parameter, however, deserve a comment. First, the sample was extracted ad hoc and no a priori statistical sample size calculation was performed; this implies that risk of an inadequate sample on which to draw conclusions is relevant. Second, migraine is known to be variable over time in terms of frequency and pain intensity, as well as in terms of frequency of migraine-like episodes which, compared to those with the features of tension-type headache (TTH), are more disabling, as well as in terms of response to acute treatment. What is not clearly stated is the amount of headache days with migraine-like and TTH-like features: the possibility that patients with migraine and 8–14 days/month of frequency might have the same (if not higher) number of migraine-like episodes compared to those with 15–23 cannot be excluded. Similarly, patients with CM might show lower disability and impact compare to those with HFEM if they have a better response to acute treatment. Third, hemiplegic migraine (ICHD-3 code 1.2.3) is a subtype of migraine with aura: the rationale for excluding these cases (i.e., they are too disabling irrespective of headaches frequency), although rare, is not in line with the overall aim to address differences in migraine-related impact as a driver to propose an update of diagnostic criteria. Fourth, the frequency of headaches is reported as “on a monthly basis”. What is not clearly reported in the manuscript is how it was determined, i.e., on the basis of the last month before inclusion or as an average of the last trimester. And, if based on the last trimester, was it determined on the basis of MIDAS item referred to headache frequency or on the basis of structured headache diaries? This is not irrelevant, not only because of the aforementioned variability in frequency but also because of recall bias: this is a concern for frequent headaches, and the MIDAS adequacy in patients with CM has already been questioned [29] because of the likelihood of recall bias and the tendency of reporting answers using multiples by five, i.e., “rounding up” to 5, 10, 15 and so on in their responses. The reasons for these differences in reporting might be due, as also postulated by Stewart at the time of MIDAS development [28], to the way in which pain experience is recalled in relation to its frequency and intensity. They hypothesized that a pattern that is constant over time can be recalled as a general impression, rather than as a series of single events: in the former case, headache frequency is encoded as a semantic memory; in the latter case, headache frequency is encoded as an episodic memory. Clearly, the occurrence of specific events—such as the presence of few days with very intense pain out of a large amount of moderate ones—might alter such a constant pattern.
The diagnosis of CM, as contrasted to that of HFEM or LFEM, should be based upon clinical features of the disease. In a condition such as migraine—which is characterized by variability in frequency, pain severity, associated symptoms of nausea, osmophobia, and photophobia, presence of aura, variable response to treatment, and finally several comorbidities [30]—the frequency of headaches alone may predict disease outcome in a partial way: therefore, the underlying pathophysiology should be taken into adequate consideration. As shown in a narrative review, the number of domains in which migraine exerts its effects is wide and the burden or impact of disease is dependent on the “activity profile” and on demographic issues of each patient (i.e., a working female mother of two sons will likely experience higher burden than a non-working women of the same age or a woman with no sons), and that there is a tendency towards worse outcomes consistently with higher headache frequency [31]: for most studies this means higher scores on MIDAS [28] or the six-item headache impact test (HIT-6) [32], which are used in the vast majority of migraine research [33].
Setting a Multiparametric Definition of Chronicity
If a revision of the way in which migraine is categorized must be carried out, then extensive collaborative research is warranted which includes different perspectives, and not only a mere issue of migraine headache days. In fact, fluctuations of headache frequency are common in patients with migraine which makes it complex to define borders [34] and, at the same time, the role of medication overuse and use of prophylaxis cannot be ignored. Progression to CM is often associated with medication overuse and, at the same time, most patients with CM remit towards an episodic pattern following medical prophylaxis [35] at least in the short term. This is, however, not valid for everyone as relapses into CM or withdrawal failure might be quite common [36], which further on shows how relevant fluctuations are among patients with migraine. Such an aspect contains a relevant risk: incorrect identification of patients for whom the clinical status deserves attention.
In our opinion, the mechanism of chronification is better captured by changes in clinical features rather than headache frequency, the most evident being the presence of TTH-like pain, cutaneous allodynia, and reduced pain threshold. CM shares with TTH the activation of the trigeminal nucleus caudalis [37]. The activation of the trigeminal nucleus, driven by the peripheral sensitization of the dural, pial, and meningeal arteries, is deemed to be an important mechanism of migraine pathogenesis [38], and it is produced in a way that is like TTH myofascial trigger points. It has moreover been hypothesized that TTH-like episodes in patients with CM might be mild migraine headaches without accompanying symptoms of nausea, phonophobia, and photophobia: their response to triptans and the overuse of medications may explain the emergence of TTH-like headaches and their increase in frequency [37]. The process of chronification is finally associated with pain sensitization which, in turn, determines decreased pain threshold. The derangement of top-down pain induces increased susceptibility to external noxious stimuli, and aggravates the trigeminal sensitization, thus generating a vicious cycle [39]. The effect of such pathophysiological changes is usually a fluctuating increase in headache frequency: so, the “trend” has to be observed. In this sense, the proposals recently made by Chalmer and colleagues and by Ishii and colleagues [26, 27] are partial as they are based on a cross-sectional evaluation: the patients that they identified as potentially new cases of CM (i.e., those commonly addressed as HFEM) might be more or less stable in that pattern, or might be in a phase of increase in frequency or in a decreasing one. Tracking the point is essential because diagnosis and trend leads to treatment considerations.
Changing Way of Looking at Things
The last implication is related to the availability of prophylaxis. Recent years have seen new specific treatments based on calcitonin gene-related peptide monoclonal antibodies (CGRP(r)-MAb) enter the market. Such treatments showed great efficacy in clinical trials and effectiveness in real life, too [40, 41]. They have therefore the potential to positively impact on a significant portion of patients with migraine. However, the high cost of such therapies (which exceed US $8000 per year [42]) might limit their widespread applicability to patients [43], and an indirect comparison between CGRP(r)-MAb and “traditional” therapies does not seem to support the possibility for a complete paradigm shift in treatment, as shown in a recent review by Vandervorst and colleagues [44]. The authors conclude that the efficacy of CGRP(r)-MAb is comparable to that of traditional preventive drugs—namely candesartan, topiramate, valproate, beta-blockers, amitriptyline, and onabotulinumtoxinA—but with a more favorable safety profile. Such a result is based on available clinical trials, whereas the impact of such treatments in terms of clinical response in real life is in its infancy. To the best of our knowledge, one phase IV trial compared erenumab and topiramate in a 1:1 double-blind randomized controlled trial: patients with four or more migraine headaches per month were randomized to subcutaneous administration of erenumab (70 or 140 mg/month) plus oral administration of topiramate placebo, or to oral administration of topiramate (50–100 mg/day) plus subcutaneous administration of erenumab placebo. The results showed a better outcome among those receiving erenumbab as active compound: they reported lower discontinuation rates (10.6% vs. 38.9%) and higher rates of at least 50% reduction in monthly migraines compared to baseline (55.4% vs. 31.2%) [45]. Large studies comparing different compounds in patients with different types of migraine are therefore needed.
Any change in the current definition may favor treatment escalation to the new drugs. However, a mere consideration of the frequency may be reductive and other issues such as previous failure of previous preventatives, which therefore impacts on the burden of migraine, are of importance to select the population of patients who is more in need of access to the more expensive drugs. Recently, the European Headache Federation together with the European Migraine and Headache Alliance proposed to use the label “resistant migraine” for those patients with at least eight debilitating migraine days and inadequate response, or contraindication, to at least three classes of migraine preventatives [46]. As further shown by the Burden and Attitude to Resistant and Refractory migraine study, resistant migraine is a common problem met by those who are involved in headache care, irrespective of the setting [47]. Contrasted with these difficult to treat patients, which might fall into the episodic or chronic patterns, there are also some patients with CM or HFEM who show a favorable profile. They are usually seen in clinical practice as those who progressed into CM or HFEM from a lower episodic pattern but were never prescribed prophylaxis and respond well to traditional, oral preventatives. Those patients should be offered advice on treatment and lifestyle—e.g., stress, bad posture, physical inactivity, sleep hygiene, poor diet, and excess use of digital technology [48]—but clearly should not be considered in need of advanced treatments.
Concluding Remarks
A paradigm shift in the definition of chronic migraine moves far beyond the mere 8 vs. 15 days/month, but it has profound implications for treatment. Such implications are open to ethical and practical issues: should patients be treated with the most effective prophylactic drugs, i.e., CGRP(r)-MAb, if they enter into a new definition of CM, or based upon cost-effectiveness and effectiveness–safety profiles? How should clinicians deal with treatment escalation from traditional oral prophylaxis towards MABs? What kind of role do associated conditions, response to acute and prophylactic treatments, as well as lifestyle issues and psychological factors have? And, finally, which endpoint should we use to define effectiveness: improvement in headache frequency, in functioning, disability, quality of life, or workplace productivity? These are the questions we have to face in the near future [48].
References
Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38(1):1–211. https://doi.org/10.1177/0333102417738202.
Lantéri-Minet M, Duru G, Mudge M, Cottrell S. Quality of life impairment, disability and economic burden associated with chronic daily headache, focusing on chronic migraine with or without medication overuse: a systematic review. Cephalalgia. 2011;31(7):837–50. https://doi.org/10.1177/0333102411398400.
Mercante JP, Bernik MA, Zukerman-Guendler V, Zukerman E, Kuczynski E, Peres MF. Psychiatric comorbidities decrease quality of life in chronic migraine patients. Arq Neuropsiquiatr. 2007;65(3B):880–4. https://doi.org/10.1590/s0004-282x2007000500031.
Seng EK, Buse DC, Klepper JE, et al. Psychological factors associated with chronic migraine and severe migraine-related disability: an observational study in a tertiary headache center. Headache. 2017;57(4):593–604. https://doi.org/10.1111/head.13021.
Raggi A, Schiavolin S, Leonardi M, et al. Chronic migraine with medication overuse: association between disability and quality of life measures, and impact of disease on patients’ lives. J Neurol Sci. 2015;348(1–2):60–6. https://doi.org/10.1016/j.jns.2014.11.004.
D’Amico D, Sansone E, Grazzi L, et al. Multimorbidity in patients with chronic migraine and medication overuse headache. Acta Neurol Scand. 2018;138(6):515–22. https://doi.org/10.1111/ane.13014.
Raggi A, Leonardi M, Sansone E, Curone M, Grazzi L, D’Amico D. The cost and the value of treatment of medication overuse headache in Italy: a longitudinal study based on patient-derived data. Eur J Neurol. 2020;27(1):62-e1. https://doi.org/10.1111/ene.14034.
Lipton RB, Seng EK, Chu MK, et al. The effect of psychiatric comorbidities on headache-related disability in migraine: results from the Chronic Migraine Epidemiology and Outcomes (CaMEO) Study. Headache. 2020;60(8):1683–96. https://doi.org/10.1111/head.13914.
Bagley CL, Rendas-Baum R, Maglinte GA, et al. Validating Migraine-Specific Quality of Life Questionnaire v2.1 in episodic and chronic migraine. Headache. 2012;52(3):409–21. https://doi.org/10.1111/j.1526-4610.2011.01997.x.
Carvalho GF, Chaves TC, Gonçalves MC, et al. Comparison between neck pain disability and cervical range of motion in patients with episodic and chronic migraine: a cross-sectional study. J Manip Physiol Ther. 2014;37(9):641–6. https://doi.org/10.1016/j.jmpt.2014.09.002.
Lipton RB, Manack Adams A, Buse DC, Fanning KM, Reed ML. A Comparison of the Chronic Migraine Epidemiology and Outcomes (CaMEO) Study and American Migraine Prevalence and Prevention (AMPP) Study: demographics and headache-related disability. Headache. 2016;56(8):1280–9. https://doi.org/10.1111/head.12878.
Canuet L, Ishii R, Fernandez-Concepcion O, Iwase M, Takeda M. Severity of depressive symptoms as predictor of impairment of quality of life in chronic migraine: comparison with episodic migraine. Psychiatry Clin Neurosci. 2008;62(6):738–40. https://doi.org/10.1111/j.1440-1819.2008.01867.x.
Ferracini GN, Florencio LL, Dach F, et al. Myofascial trigger points and migraine-related disability in women with episodic and chronic migraine. Clin J Pain. 2017;33(2):109–15. https://doi.org/10.1097/AJP.0000000000000387.
D’Amico D, Grazzi L, Usai S, Rigamonti A, Curone M, Bussone G. Disability pattern in chronic migraine with medication overuse: a comparison with migraine without aura. Headache. 2005;45(5):553–60. https://doi.org/10.1111/j.1526-4610.2005.05109.x.
D’Amico D, Grazzi L, Curone M, et al. Difficulties in work activities and the pervasive effect over disability in patients with episodic and chronic migraine. Neurol Sci. 2015;36(Suppl 1):9–11. https://doi.org/10.1007/s10072-015-2130-4.
Raggi A, Giovannetti AM, Leonardi M, et al. Disability and mood state in patients with episodic and chronic migraine associated to medication overuse. Neurol Sci. 2012;33(Suppl 1):S169-71. https://doi.org/10.1007/s10072-012-1076-z.
Bigal ME, Rapoport AM, Lipton RB, Tepper SJ, Sheftell FD. Assessment of migraine disability using the migraine disability assessment (MIDAS) questionnaire: a comparison of chronic migraine with episodic migraine. Headache. 2003;43(4):336–42. https://doi.org/10.1046/j.1526-4610.2003.03068.x.
Linde M, Gustavsson A, Stovner LJ, et al. The cost of headache disorders in Europe: the Eurolight project. Eur J Neurol. 2012;19(5):703–11. https://doi.org/10.1111/j.1468-1331.2011.03612.x.
Lublóy Á. Economic burden of migraine in Latvia and Lithuania: direct and indirect costs. BMC Public Health. 2019;19(1):1242. https://doi.org/10.1186/s12889-019-7461-2.
Stewart WF, Wood GC, Manack A, Varon SF, Buse DC, Lipton RB. Employment and work impact of chronic migraine and episodic migraine. J Occup Environ Med. 2010;52(1):8–14. https://doi.org/10.1097/JOM.0b013e3181c1dc56.
Raggi A, Covelli V, Guastafierro E, et al. Validation of a self-reported instrument to assess work-related difficulties in patients with migraine: the HEADWORK questionnaire. J Headache Pain. 2018;19(1):85. https://doi.org/10.1186/s10194-018-0914-7.
Lipton RB. Tracing transformation: chronic migraine classification, progression, and epidemiology. Neurology. 2009;72(5 suppl):S3–7. https://doi.org/10.1212/WNL.0b013e3181974b19.
Giannini G, Zanigni S, Grimaldi D, et al. Cephalalgiophobia as a feature of high-frequency migraine: a pilot study. J Headache Pain. 2018;14(1):49. https://doi.org/10.1186/1129-2377-14-49.
Bigal ME, Dodick DW, Rapoport AM, et al. Safety, tolerability, and efficacy of TEV-48125 for preventive treatment of high-frequency episodic migraine: a multicentre, randomised, double-blind, placebo-controlled, phase 2b study. Lancet Neurol. 2015;14(11):1081–90. https://doi.org/10.1016/S1474-4422(15)00249-5.
Buse DC, Serrano D, Reed ML, et al. Adding additional acute medications to a triptan regimen for migraine and observed changes in headache-related disability: results from the American Migraine Prevalence and Prevention (AMPP) Study. Headache. 2015;55(6):825–39. https://doi.org/10.1111/head.12556.
Chalmer MA, Hansen TF, Lebedeva ER, Dodick DW, Lipton RB, Olesen J. Proposed new diagnostic criteria for chronic migraine. Cephalalgia. 2020;40(4):399–406. https://doi.org/10.1177/0333102419877171.
Ishii R, Schwedt TJ, Dumkrieger G, et al. Chronic versus episodic migraine: the 15-day threshold does not adequately reflect substantial differences in disability across the full spectrum of headache frequency. Headache. 2021;61:992–1003. https://doi.org/10.1111/head.14154.
Stewart WF, Lipton RB, Kolodner KB, Sawyer J, Lee C, Liberman JN. Validity of the Migraine Disability Assessment (MIDAS) score in comparison to a diary-based measure in a population sample of migraine sufferers. Pain. 2000;88(1):41–52. https://doi.org/10.1016/S0304-3959(00)00305-5.
Raggi A, Grazzi L, Grignani E, et al. The use of MIDAS in patients with chronic migraine and medication-overuse headache: should we trust it? Neurol Sci. 2018;39(Suppl 1):125–7. https://doi.org/10.1007/s10072-018-3373-7.
Caponnetto V, Deodato M, Robotti M, et al. Comorbidities of primary headache disorders: a literature review with meta-analysis. J Headache Pain. 2021;22(1):71. https://doi.org/10.1186/s10194-021-01281-z.
Leonardi M, Raggi A. A narrative review on the burden of migraine: when the burden is the impact on people’s life. J Headache Pain. 2019;20(1):41. https://doi.org/10.1186/s10194-019-0993-0.
Kosinski M, Bayliss MS, Bjorner JB, et al. A six-item short-form survey for measuring headache impact: the HIT-6. Qual Life Res. 2003;12:963–74. https://doi.org/10.1023/a:1026119331193.
D’Amico D, Tepper SJ, Guastafierro E, et al. Mapping assessments instruments for headache disorders against the ICF biopsychosocial model of health and disability. Int J Environ Res Public Health. 2020;18(1):246. https://doi.org/10.3390/ijerph18010246.
Serrano D, Lipton RB, Scher AI, et al. Fluctuations in episodic and chronic migraine status over the course of 1 year: implications for diagnosis, treatment and clinical trial design. J Headache Pain. 2017;18:101. https://doi.org/10.1186/s10194-017-0787-1.
Vandenbussche N, Laterza D, Lisicki M, et al. Medication-overuse headache: a widely recognized entity amidst ongoing debate. J Headache Pain. 2018;19:50. https://doi.org/10.1186/s10194-018-0875-x.
Katsarava Z, Limmroth V, Finke M, Diener HC, Fritsche G. Rates and predictors for relapse in medication overuse headache: a 1-year prospective study. Neurology. 2003;60:1682–3. https://doi.org/10.1212/01.wnl.0000063322.14078.90.
Blumenfeld A, Schim J, Brower J. Pure tension-type headache versus tension-type headache in the migraineur. Curr Pain Headache Rep. 2010;14:465–9. https://doi.org/10.1007/s11916-010-0147-1.
Olesen J, Burstein R, Ashina M, Tfelt-Hansen P. Origin of pain in migraine: evidence for peripheral sensitisation. Lancet Neurol. 2009;8:679–90. https://doi.org/10.1016/S1474-4422(09)70090-0.
May A, Schulte LH. Chronic migraine: risk factors, mechanisms and treatment. Nat Rev Neurol. 2016;12:455–64. https://doi.org/10.1038/nrneurol.2016.93.
Sacco S, Bendtsen L, Ashina M, et al. European headache federation guideline on the use of monoclonal antibodies acting on the calcitonin gene related peptide or its receptor for migraine prevention. J Headache Pain. 2019;20(1):6. https://doi.org/10.1186/s10194-018-0955-y.
Caronna E, Gallardo VJ, Alpuente A, Torres-Ferrus M, Pozo-Rosich P. Anti-CGRP monoclonal antibodies in chronic migraine with medication overuse: real-life effectiveness and predictors of response at 6 months. J Headache Pain. 2021;22(1):120. https://doi.org/10.1186/s10194-021-01328-1.
Arca K, Reynolds J, Sands KA, Shiue HJ. Calcitonin gene-related peptide antagonists for the prevention of migraine: highlights from pivotal studies and the clinical relevance of this new drug class. Ann Pharmacother. 2020;54(8):795–803. https://doi.org/10.1177/1060028020903417.
Chen YY, Ye XQ, Tang TC, She TW, Chen M, Zheng H. Calcitonin gene-related peptide monoclonal antibodies versus botulinum neurotoxin a in the preventive treatment of chronic migraine: an adjusted indirect treatment comparison meta-analysis. Front Pharmacol. 2021;12: 671845. https://doi.org/10.3389/fphar.2021.671845.
Vandervorst F, Van Deun L, Van Dycke A, et al. CGRP monoclonal antibodies in migraine: an efficacy and tolerability comparison with standard prophylactic drugs. J Headache Pain. 2021;22(1):128. https://doi.org/10.1186/s10194-021-01335-2.
Reuter U, Ehrlich M, Gendolla A, et al. Erenumab versus topiramate for the prevention of migraine—a randomised, double-blind, active-controlled phase 4 trial. Cephalalgia. 2022;42(2):108–18. https://doi.org/10.1177/03331024211053571.
Sacco S, Braschinsky M, Ducros A, et al. European headache federation consensus on the definition of resistant and refractory migraine: developed with the endorsement of the European Migraine and Headache Alliance (EMHA). J Headache Pain. 2020;21(1):76. https://doi.org/10.1186/s10194-020-01130-5.
Sacco S, Lampl C, Maassen-van-den-Brink A, et al. Burden and attitude to resistant and refractory migraine: a survey from the European Headache Federation with the endorsement of the European Migraine and Headache Alliance. J Headache Pain. 2021;22(1):39. https://doi.org/10.1186/s10194-021-01252-4.
Goadsby PJ, Lantéri-Minet M, Michel MC, et al. 21st century headache: mapping new territory. J Headache Pain. 2021;22(1):19. https://doi.org/10.1186/s10194-021-01233-7.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Conceptualization: Paolo Martelletti; Writing - original draft preparation: Alberto Raggi; Writing – review and editing: Matilde Leonardi and Simona Sacco; Supervision: Paolo Martelletti.
Disclosures
Alberto Raggi, Matilde Leonardi, Simona Sacco, and Paolo Martelletti have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Raggi, A., Leonardi, M., Sacco, S. et al. Migraine Outcome Should Not Be Used to Determine Diagnosis, Severity, and Therapy: Moving Towards a Multiparametric Definition of Chronicity. Pain Ther 11, 331–339 (2022). https://doi.org/10.1007/s40122-022-00375-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-022-00375-z