Abstract
Introduction
Combined lateral mass screw-rod (LMSR) fixation and anterior cervical discectomy and fusion (ACDF) surgery is currently the most widely described and accepted procedure for subaxial cervical facet fracture with traumatic disc herniation. Recent biomechanical studies have demonstrated that the use of transfacet screw (TFS) can be considered as a simple alternative method to LMSR. However, to date, little is known about the feasibility and effectiveness of TFS in the combined approach. The aim of this study was to compare the clinical and radiographic results of TFS + ACDF surgery and LMSR + ACDF surgery, and to provide a less invasive alternative technique for spine surgeons.
Method
We retrospectively reviewed patients with unilateral cervical facet fracture with traumatic disc herniation who had undergone TFS + ACDF (N = 36) or LMSR + ACDF (N = 34) with a minimum 2-year follow-up. Clinical assessments, which included American Spinal Injury Association impairment scale (AIS), visual analog scale for neck pain (VASSNP) score and patient satisfaction, were made before surgery and at follow-up. For the radiographic outcomes, the instability parameters of segmental kyphosis and sagittal translation were measured.
Results
The demographic characteristics of the two groups of patients were similar. In terms of clinical outcomes, both two groups were associated with significant improvements at the final follow-up. There were no significant between-group differences in VASSNP score or patient satisfaction (both P > 0.05). The LMSR + ACDF group suffered more blood loss and had longer operative time (mean 206.0 ml; mean 274.4 min, respectively) than in the TFS + ACDF group (mean 110.0 ml; mean 142.8 min, respectively) (P < 0.001 for both comparisons). For the radiographic results, the segmental kyphosis and sagittal translation were significantly corrected after surgery in both groups (P < 0.001 for both groups), and no significant differences were found between groups at the last follow-up (P > 0.05).
Conclusion
In the absence of any self-evident clinical and radiographic benefits of one technique over the other (TFS + ACDF vs. LMSR + ACDF), we recommend combined TFS + ACDF surgery as a safe and less invasive alternative treatment for unilateral cervical facet fractures with traumatic disc herniation, as it was associated with a shorter duration of surgery and lower estimated blood loss than LMSR + ACDF surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Patients with unilateral cervical facet fracture accompanied by traumatic disc herniation always have acute neck pain and high risk of spinal cord compression. |
Combined lateral mass screw-rod (LMSR) fixation and anterior cervical discectomy and fusion (ACDF) surgery is currently one of the most common procedures for this complex three-column injury, although it is associated with several drawbacks, including longer operative time, increased blood loss, a relatively high risk of neurovascular injury and surgical site infection. |
Transfacet screw (TFS) is a simple alternative method with comparable biomechanical properties to LMSR. However, limited data are available in the clinical literature on the feasibility and effectiveness of combined TFS and ACDF surgery. |
The aim of this study was to compare clinical and radiographic outcomes of TFS + ACDF and LMSR + ACDF, and to provide a relatively less invasive therapeutic option for spine surgeons. |
What was learned from the study? |
Compared with LMSR + ACDF surgery, TFS + ACDF surgery is a safe and less invasive alternative method for unilateral cervical facet fractures with traumatic disc herniation. |
Introduction
Fractures involving facets of the cervical spine are a subset of cervical spine injuries that often result in rotational subluxation or dislocation of the spine at the affected level. Specific to a unilateral facet fracture, which accounts for approximately 85% of cervical facet fractures [1], the posterior ligamentous complex is likely to be the site of the initial injury, with the injury then spreading to the anterior disco-ligamentous complex, leading to additional further rotation or translation injury mechanism [2,3,4]. Previous studies have reported that the incidence of disc disruption may be as high as 40% in cases of unilateral cervical facet fracture–dislocation [5]. Traumatic cervical disc herniation is likely to cause further compression of the spinal cord and increase the risk of neurological deterioration during closed reduction procedure.
To manage cervical facet fracture accompanied by anterior disc pathology, an increasing number of surgeons are trending towards utilization of anterior cervical discectomy and fusion (ACDF) and open reduction [6], possibly due to a concern for neurological deterioration in patients with an associated disc herniation [7,8,9]. However, for some unilateral cervical locked facets, the failure rate of open ventral reduction using previously reported anterior techniques is reported to be approximately 25–40%, necessitating additional posterior open reduction [10,11,12,13]. Furthermore, data from biomechanical studies have suggested that anterior fixation provides less stability than posterior fixation [14, 15]. Thus, combined approaches (i.e. anterior-approach, posterior-anterior, anterior–posterior-anterior) are now recommended to obtain satisfactory reduction, decompression and rigid fixation in cases of facet fractures–dislocation accompanied by a suspected disc herniation. Currently, combined ACDF and lateral mass screw-rod (LMSR) constructs are the most widely described and accepted constructs for the cervical spine [16, 17]. Unfortunately, this strategy had several drawbacks, including longer operative time, increased blood loss, a relatively high risk of neurovascular injury and surgical site infection [15, 18].
The transfacet screw (TFS) for instrumented fixation in the cervical spine is not a new concept and has been used as an alternative method of LMSR to achieve posterior cervical spine fixation strength. Klekamp et al. [19] were the first to note that cervical TFS fixation without rods has a greater pullout strength than LMSR fixation. DalCanto et al. [20] and Newton et al. [21] conducted a biomechanical comparison of cervical TFS placement and LMSR for two-level and multilevel posterior cervical spine stabilization, respectively, and demonstrated that TFS without rods had similar biomechanical stability as typical LMSR constructs. In addition, based on the results of their comparison study, Alanay et al. [22] proposed that TFS placement might provide an alternative for rigid fixation in patients with altered cervical spine morphology and was potentially associated with a lower incidence of nerve root or vascular injury than the LMSR construct. In a more recent finite element study carried out by our research team [23], we found that there were no statistically significant differences biomechanically at a single-level C4/5 fixation between TFS (unilateral) + ACDF and LMSR (bilateral) + ACDF in terms of the treatment of unilateral subaxial cervical facet fracture with failure of the anterior disc.
For all of these above-mentioned reasons, TFS may be regarded as a less invasive and less risky technique to provide instant stability compared with LMSR. However, to date, little is known about the feasibility and utility of TFS in the combined approach. Therefore, the aim of this study was to perform TFS + ACDF surgery for the treatment of unilateral subaxial cervical facet fracture with traumatic disc herniation, and to compare the clinical and radiographic results of the TFS + ACDF and LMSR + ACDF strategies.
Methods
Study Design and Consent
This was a retrospective cohort study. The study was approved by the Institutional Review Board of Tongji Hospital of Tongji University (reference number: K-2021-009), which waived the informed consent requirement due to the retrospective nature of study, and was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Patient Population
Between December 2011 and August 2019, a total of 99 consecutive patients aged ≥ 18 years with subaxial cervical facet fractures were treated. Initially, all patients underwent examinations by cervical plain radiography and computed tomography with three-dimensional reconstruction for a clear diagnosis of unilateral or bilateral facet fractures with subluxations or dislocations. Pre-reduction cervical magnetic resonance imaging (MRI) was performed to evaluate for traumatic disc herniation, epidural hematoma, spinal cord compression and ligamentous injury. In fully awake patients with absence of traumatic disc herniation, we attempted closed reduction with external Gardner–Wells tongs (normally with 5 kg + 2.5 kg/level of injury below the C1 vertebra) under intensive lateral view radiographic control [12]. Five patients were realigned, and then treated nonoperatively with halo immobilization or hard collar. A single posterior approach surgery was conducted on 14 patients who suffered from unsuccessful reduction. For cases of traumatic disc herniation (N = 80), a decision was made to perform an immediate posterior open reduction and stabilization, and subsequent ACDF surgery.
Inclusion criteria were: (1) unilateral cervical facet fractures with subluxation or dislocation; (2) the preoperative MRI detected an extruded disc, which deformed the dural sac beyond the line between the postero-inferior corner of cranial vertebrae and the postero-superior corner of caudal vertebrae; and (3) a minimum of 24-month follow-up. To avoid aggravating neurological deterioration, traction with maximum weight (50% estimated body weight) under general anesthesia was not attempted. We excluded patients from our study who met at least one of the following criteria: (1) multiple-level facet fractures; (2) history of cervical spine surgery; (3) vertebral fracture; (4) cervical diseases affecting the fixed segment or clinical evaluation (e.g. pre-existing spinal deformity and severe osteoporosis); and (5) associated multiple severe trauma (Fig. 1). A total of 70 patients were treated using posterior open reduction and fixation (LMSR or TFS) and subsequent ACDF. The decision for the posterior fixation method was made according to the surgeon’s preference.
Clinical Outcomes
Patients were followed in an outpatient clinic postoperatively. The severity of neurological injury was evaluated using the American Spinal Injury Association (ASIA) impairment scale (AIS) grades, which range from grade A (sensory and motor complete spinal cord injury) to grade E (normal sensory and motor function) [24]. A visual analog scale score for neck pain (VASSNP) (range 1–10) was assessed before and at follow-up [25]. In addition, patient satisfaction (score range 1–10) at the time of final follow-up was compared between the TFS + ACDF group and the LMSR + ACDF group [26].
Radiographic Outcomes
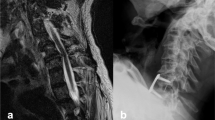
The instability parameters of segmental kyphosis and sagittal translation were measured on a neutral lateral X-ray (Fig. 2). The kyphosis was recorded as the angle between the superior endplate of the injured vertebrae and the inferior endplate of the subjacent intact vertebrae. An extension angle was by convention negative and a flexion angle was positive. The translation was classified as the horizontal displacement of the cephalic vertebra in relation to the caudal vertebral body of the injured segment. Initial instability was defined according to White as: > 3.5 mm displacement, and > 11° kyphosis of injury segment on static X-ray films. The spinal alignment and fusion status were evaluated using static and dynamic X-ray films during the follow-up. A successful outcome in this series necessitated an anatomic restoration of the spinal column, solid fusion of the segment, no adjacent instability and no late kyphosis or translation (> 11° and 3.5 mm) during the follow-up. These measurements were evaluated on all patients before surgery and at last follow-up by two senior orthopedic physicians in the picture archiving and communication system software workstation.
The segmental kyphosis was classified as the angle between the superior endplate of the injured vertebrae and the inferior endplate of the subjacent intact vertebrae on the lateral view. An extension angle is by convention negative and a flexion angle is positive. The sagittal translation was classified as the horizontal displacement of the cephalic vertebra relation to the caudal vertebral body of the injured segment
Surgical Technique
TFS + ACDF Technique
Patients were placed in the prone position on a gypsum bed under general anesthesia. Prior to the operation, axial traction was gently applied to the injured cervical spine using the Mayfield head holder. A conventional midline exposure of the posterior aspect of the cervical spine was performed, making sure that the boundaries of the lateral masses were adequately exposed. The detached bone fragments of the joint capsules of the affected side were then removed. To facilitate reduction, the tip of the superior articular process was resected using a high-speed burr. An intraoperative radiograph was then obtained to confirm that the deformity had been adequately reduced. The use of TFS fixation was contraindicated in the affected side due to split or comminuted articular process. The TFS was inserted under fluoroscopy guidance at the contralateral facets, with the entrance point 1 mm medial and 1–2 mm above to the midpoint of the lateral mass and with lateral angulation of 25–30° laterally and sagittal inclination of 30°–40° caudally. The trajectory pointed to the lower lateral of the lateral mass, which provided longer purchase to the vertebrae and avoided injury to the vertebral artery and cervical nerve root [27]. The feel of the passage of the drill through the four cortical surfaces could be felt. Once the drill passed through the cortical surfaces, the length of the screw had to be measured. The drilled hole was then tapped, followed by the placement of a 3.5-mm screw of appropriate length (mainly 16–20 mm) [28]. Restoration of lordosis was guaranteed by appropriate positioning of the cervical spine under fluoroscopy guidance prior to screw hole preparation. During the surgery, the upper and lower spinous processes could be gently lifted after insertion of the screw to check whether the fixation was reliable; this also provided immediate internal stability for the sequent anterior approach. Chips of allograft bone were grafted in the bone defect. The incision was washed clean and closed with a drainage tube left inside. The patients were then placed carefully in a supine position. A standard Smith–Robinson ACDF surgical procedure was subsequently performed [29] to remove the herniated disc and to stabilize and realign the spinal column (Fig. 3).
Imaging of a 55-year-old man, who had C4/5 unilateral facet fracture-subluxation and traumatic disc herniation after a motor vehicle accident, managed with posterior TFS + ACDF. a Preoperative lateral plain radiograph demonstrating facet subluxation of C4/5 vertebrae. b, c Preoperative computed tomography (CT) sagittal view of the mid and left cervical spine demonstrated the inferior articular process fracture with perching of the superior articular process to the fractured facet rostral (white rectangle). d MRI obtained at the time of injury, sagittal view, T2-weighted sequence, demonstrated anterior longitudinal ligament injury and hematoma in the prevertebral space (white arrow), a large dorsally extruded disc herniation with rostral migration and cord compression with T2-hyperintensity of the spinal cord, and severe posterior ligament complex injury (white circle). e An initial posterior approach was performed, followed by reduction of the facets and transfacet screw placement. f A subsequent anterior approach was performed, followed by removal of ruptured disc and fusion. g Upright cervical lateral radiograph at 1 year after surgery shows retention of normal cervical alignment and complete incorporation of the allograft with the C4 and C5 vertebral bodies
LMSR + ACDF Technique
A posterior midline subperiosteal exposure was performed as described above for the TFS + ACDF technique. Posterior reduction and fixation was performed at the affected level only. If the injury involved primarily the inferior articular process, placement of LMSR in some patients might prove difficult, necessitating extension of the construct to adjacent levels. After reduction was achieved, four lateral mass screws were inserted at the affected level bilaterally following the Magerl technique. The entry point for screw insertion was located slightly medial and rostral to the midpoint of the lateral mass. The direction of the screw was 25° laterally in the axial plane and parallel to the facet joint in the sagittal place. Gentle compression was applied between the screws to approximate the facets to posterior support and promotion of facet fusion. The fusion was completed by grafting chips of allograft bone after rod application, followed by a standard ACDF surgery (Fig. 4).
Imaging of a 48-year-old man, who had C6/7 unilateral facet fracture–dislocation and traumatic disc herniation after a motor vehicle accident, managed with posterior LMSR + ACDF. a Midline sagittal CT demonstrated mild anterior subluxations of C6 on C7. b, c Left side facet interlocking with ipsilateral inferior articular process fracture (yellow arrows) at C6/7 motion segment was discovered on CT three-dimensional reconstruction. d Preoperative sagittal T2-weighted MRI demonstrated that the patient had an anterior extruded intervertebral disc and severe posterior ligament complex injury. e, f CT performed immediately after posterior fixation and anterior discectomy and bone grafting demonstrated good realignment at the affected C6/7 segment. g Upright cervical lateral radiograph at at 1 year after surgery shows retention of normal cervical alignment and complete incorporation of the allograft with the C6 and C7 vertebral bodies
After each operation, the drainage tube was usually removed within 1 to 3 days, depending on the amount of drainage fluid. A Philadelphia collar was adopted for additional protection for 8–12 weeks as soon as the patient was allowed to walk.
Statistical Analysis
All statistical analysis was performed using SPSS software version 19.0 (SPSS IBM Corp., Armonk, NY, USA). Continuous variables with normal distribution were presented as the mean ± standard deviation (SD), and non-normal variables were reported as the median with interquartile range. Differences between parameters in each group were tested using paired-samples Student's t test for continuous variables. The means of two continuous normally distributed variables were compared by independent samples Student's t test. Nonnormally distributed variables were compared using the Wilcoxon signed rand test or Wilcoxon rank sum test. Differences in gender, mechanism of injury and injury site between the two groups of patients were evaluated using Chi-square test or Fisher exact test, respectively. P values of ≤ 0.05 were considered to be statistically significant.
Results
Patient Demographics
The patients’ demographic and baseline characteristics are summarized in Table 1. No significant between-group differences were observed in patients’ general data, such as age, sex, mechanism of injury and injury site (P > 0.05). The TFS + ACDF group was associated with shorter mean operative time than the LMSR + ACDF group (142.8 vs. 274.4 min, respectively; P < 0.001). The average estimated blood loss in the LMSR + ACDF group was greater than that in the TFS + ACDF group (206.0 vs. 110.0 ml, respectively; P < 0.001). The mean duration of the follow-up evaluation did not differ significantly between the two groups (30.1 [TFS +ACDF] and 30.7 [LMSR + ACDF] months; P = 0.622).
Neurological Status
On admission, neurological examination revealed various deficits. Based on the AIS of sensory or motor function loss, of the 36 patients in the TFS + ACDF group, six (16.7%) patients were assessed at grade A, seven (19.4%) at grade B, seven (19.4%) at grade C, ten (27.8%) at grade D and six (16.7%) at grade E. Of the 34 patients in the LMSR + ACDF group, based on the AIS, four (11.8%) were assessed at grade A, eight (23.5%) at grade B, nine (26.5%) at grade C, six (17.6%) at grade D and seven (20.6%) at grade E. The neurological results at the end of the follow-up period are presented in Table 2. At the final follow-up, there were no increases in neurological deficit in both groups. In the TFS + ACDF group, four AIS grade A patients remained at AIS grade A; however, all of them showed descent of the level of paralysis by one or two spinal cord segments; two AIS grade C patients and eight AIS grade D patients returned to normal neurological status (AIS grade E). With respect to the LMSR + ACDF group, two AIS grade A patients improved to AIS grade B; two AIS grade B patients improved to AIS grade D; dour AIS grade C patients and five AIS grade D patients returned to AIS grade E.
Clinical Outcomes
In terms of clinical outcomes, both two groups were associated with significant improvements at the final follow-up (Table 3). The average VASSNP was low in both groups, and no significant difference was found between groups (P = 0.070). There were no significant differences between groups in terms of patient satisfaction (P = 0.775).
Radiographic Outcomes
In the TFS + ACDF group, the mean (± SD) segmental kyphosis and sagittal translation on admission were 8.6° ± 6.9° and 4.3 ± 1.8 mm, respectively. In the LMSR + ACDF group, the mean segmental kyphosis and translation on admission were 9.8° ± 6.8° and 4.8 ± 1.8 mm, respectively. Before surgery, there was no significant difference between groups in kyphosis (P = 0.478) and translation (P = 0.302) (Table 4). At last follow-up, the segmental kyphosis and sagittal translation were significantly corrected to 3.3° ± 5.1° and 1.2 ± 0.9 mm in the TFS + ACDF group (P < 0.001), and 3.7° ± 4.2° and 1.2 ± 0.8 mm in LMSR + ACDF group (P < 0.001). With regard to the change of kyphosis and translation, no significant differences were observed between the two groups, although the change was larger in LMSR + ACDF group (Table 5).
At the final follow-up, satisfactory and solid bony unions were achieved in both groups, as evidenced by bridging bony trabeculae between adjacent vertebrae with absence of motion in flexion–extension views. Only one patient in the LMSR + ACDF group, however, experienced delayed bone fusion that was achieved at 9 months postoperatively.
Complications
In the LMSR + ACDF group, there was one patient with a wound infection with dehiscence that was debrided and subsequently healed uneventfully. Additionally, two patients suffered from lateral mass fracture during lateral mass screw insertion, necessitating extension of the LMSR construct to adjacent levels. In the TFS + ACDF group, wound dehiscence with no evidence of infection occurred in one patient 2 weeks after surgery, and the wound healed after extensive debridement. No screw loosening or breakage nor neurovascular complications related to screw malposition were observed in either group intraoperatively or during the follow-up period.
Discussion
In this study, we investigated the clinical and radiographic outcomes of 36 patients who underwent TFS + ACDF and 34 patients who underwent LMSR + ACDF during the treatment of unilateral subaxial cervical facet fractures with traumatic disc herniation. Our results demonstrated that both combination surgeries yielded similar clinical improvement and local kyphosis correction, as evaluated by AIS, VASSNP, patient satisfaction, segmental kyphosis and sagittal translation. The TFS + ACDF surgery was associated with a shorter operative time and lower estimated blood loss than the LMSR + ACDF surgery.
The treatment of cervical facet fractures with traumatic disc herniation is a controversial surgical subject. A posterior-anterior combined approach was suggested in our study because cases enrolled in this series were facet fractures with subluxations or dislocations that could not be treated by closed reduction. Compared to a standard anterior–posterior-anterior approach (anterior discectomy, posterior reduction and fixation, then anterior grafting and instrumentation), the current combined posterior fixation (i.e., TFS or LMSR) and subsequent ACDF surgery did not show neurologic deterioration, even though the posterior procedure was conducted first; this result is consistent with the results of two previous studies reported by Liu et al. [30] and Tofuku et al. [16]. In general, when an MRI scan showed a prolapsed disc, anterior discectomy was recommended before reduction to avoid the cord being compressed during the reduction maneuver. However, some authors have demonstrated that traumatic disc herniation does not increase the probability of neurological deterioration [4, 31, 32]. The neurological status results of this study are consistent with those reported in previous publications, possibly because a prompt anterior decompression was added to the procedure, although a prolapsed disc could have compressed the spinal cord further during the posterior reduction maneuver.
To our knowledge, the TFS + ACDF technique described herein was first applied in the treatment of unilateral subaxial cervical facet fracture. LMSR has become the standard method of posterior cervical spine fixation and stabilization for a variety of surgical indications over the past two decades. While a more minimally invasive approach using screws placed across the facet joints (i.e. TFS) is not as widely used as LMSR, it can be quite a useful procedure for isolated facet joint fusion and has been advocated as an alternative to LMSR in the cervical spine [22, 33, 34]. Klekamp et al. [19] were the first to note that TFS placement provided comparable, if not greater, pullout resistance than LMSR placement in the cervical spine, with the possible explanation that TFS penetrated upper and lower articular processes with four layers of cortical bone altogether, while LMS penetrated mostly through cancellous bone. Moreover, a recent biomechanical study by Yi et al. [35] revealed that TFS without rods had similar biomechanical stability as typical LMSR constructs in single-level insertions. Furthermore, in a more recent publication by our research team [23], we first constructed a finite element model of unilateral facet fracture with failure of anterior disc at C4/5 level and then assessed the construct stability (i.e. range of rotation, axial compression displacement and anterior shear displacement) at the operative level following TRS + ACDF and LMSR + ACDF. The results suggested that there was no obvious difference in terms of stabilization biomechanically between TFS and LMSR in the presence of anterior fixation. Impressively, the findings of the current study were supported by those reported by us recently in which a total of 36 TFSs were placed without loosening and acquired reliable fixation intraoperatively or during the period of follow-up, and the articular surfaces were all fused at final follow-up [23]. Collectively, these results suggest that TFS could provide satisfactory supplementary immediate fixation prior to anterior approach as well as solid bony fusion postoperatively.
Regarding clinical efficacy, the results of the present study revealed that VASSNP scores were improved within groups postoperatively whereas no significant differences were found between groups. A previous retrospective study reported a series of 21 patients with subaxial cervical facet injury accompanied by traumatic disc herniation treated with anterior decompression and bone grafting and posterior LMSR fixation [12]. The VASSNP decreased from 7.8 ± 1.2 before surgery to < 1.6 ± 0.5 (P < 0.05) 6 months postoperatively. This result is consistent with our successful clinical outcomes following a minimum 2-year follow-up. However, this previous study did not report general data on duration of the operation, operative bleeding volume and postoperative drainage volume. These latter variables are of significant concern in the the decision-making process of surgeons because they may be associated with anesthetic and surgical risks [15]. In the current study, the authors observed that TFS + ACDF surgery was associated with a shorter operative time and lower estimated blood loss than LMSR + ACDF surgery, with one possible explanation being the difference in number of screws: four screws were inserted using the LMSR technique and only one screw was needed when performing the TFS technique. Placement of fewer screws clearly contributed to reducing the duration of surgery and the number of intraoperative fluoroscopy. Additionally, TFS with lower implant profile might be related to lower blood loss, and a drainage tube was even not needed in some cases.
There have been few published reports to date that have compared the change in segmental radiographic parameters in the treatment of cervical facet fractures. Our findings suggest that segmental kyphosis and translation were effectively corrected and maintained during the follow-up within groups. Despite the mean corrected kyphosis and translation in the LMSR + ACDF group being greater than those in the TFS + ASCF group, no significant difference was observed between groups. In agreement with the present results, Feng et al. [12] evaluated segmental vertebral kyphosis in patients treated by LMSR + ACDF surgery. They found that preoperative local sagittal alignment at the injured segment averaged 17.7° ± 6.3° kyphosis. During follow-up, the kyphosis was significantly corrected to 6.5° ± 4.1° and remained 5.9° ± 4.2° 1 year later. Feng et al. demonstrated a larger local kyphosis correction, which the current study did not, possibly because the patients enrolled by Feng et al. included those with both unilateral and bilateral facet injury and, in addition, the number of surgical segments was not strictly controlled. In contrast, in the present study, enrollment was limited to a single-level unilateral facet fracture. Moreover, in a 2-year follow-up retrospective study related to single-level subaxial cervical facet injury, Lifeso and Colucci [36] proposed that single posterior LMSR stabilization and fusion procedure was inclined to lead to late-developing kyphosis (> 10°) as the result of anterior disc space collapse, even though the solid posterior fusion was achieved. Taken together, these radiographic findings indicate that posterior fixation is necessary for the reduction of malalignment in the treatment of subaxial cervical facet fractures with traumatic disc herniation, and that posterior TFS fixation plays a vital role similar to that of LMSR fixation in the stabilization of the unstable motion segment.
Several potential limitations of this work have been identified. Similar to most retrospective studies, the number of patients available (and eligible) for enrollment in current study was small (i.e., N = 70). We can not speculate whether the results obtained would have changed with a larger number of patients. Additionally, success rates may be overestimated due to lack of sufficient follow-up to detect late complications of fusion procedures. Furthermore, this study has a risk of bias due to the methodological design (nonrandomized study). In other words, the patient allocation was not randomized; rather, it was based on surgeon preference due to the lack of high-quality trials, which might result in a selection bias. Despite this, this is the first study to investigate the clinical and radiographic outcomes of two comparable procedures (i.e. TFS + ACDF vs. LMSR + ACDF), and early data from our study are promising. Further prospective randomized studies are necessary to address these limitations and validate the results of this study.
Conclusions
In conclusion, we found that clinical improvement and local kyphosis correction was similar for TFS + ACDF and LMSR + ACDF surgeries for single-level unilateral cervical facet fracture with traumatic disc herniation. In addition, TFS + ACDF surgery was associated with a shorter operative time and lower estimated blood loss than LMSR + ACDF surgery. Therefore, we recommend the TFS + ACDF surgery as a safe and effective therapeutic alternative for the treatment of single-level unilateral cervical facet fracture with traumatic disc herniation.
References
Kepler CK, Vaccaro AR, Chen E, et al. Treatment of isolated cervical facet fractures: a systematic review. J Neurosurg Spine. 2016;24(2):347–54.
Allen BL Jr, Ferguson RL, Lehmann TR, O’Brien RP. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine (Phila Pa 1976). 1982;7(1):1–27.
Crawford NR, Duggal N, Chamberlain RH, Park SC, Sonntag VK, Dickman CA. Unilateral cervical facet dislocation: injury mechanism and biomechanical consequences. Spine (Phila Pa 1976). 2002;27(17):1858–64 (Discussion 1864).
Bauze RJ, Ardran GM. Experimental production of forward dislocation in the human cervical spine. J Bone Jt Surg Br. 1978;60-B(2):239–45.
Rizzolo SJ, Piazza MR, Cotler JM, Balderston RA, Schaefer D, Flanders A. Intervertebral disc injury complicating cervical spine trauma. Spine (Phila Pa 1976). 1991;16(Suppl 6):S187–9.
Nassr A, Lee JY, Dvorak MF, et al. Variations in surgical treatment of cervical facet dislocations. Spine (Phila Pa 1976). 2008;33(7):e188–93.
Eismont FJ, Arena MJ, Green BA. Extrusion of an intervertebral disc associated with traumatic subluxation or dislocation of cervical facets. Case report. J Bone Jt Surg Am. 1991;73(10):1555–60.
Doran SE, Papadopoulos SM, Ducker TB, Lillehei KO. Magnetic resonance imaging documentation of coexistent traumatic locked facets of the cervical spine and disc herniation. J Neurosurg. 1993;79(3):341–5.
Harrington JF, Likavec MJ, Smith AS. Disc herniation in cervical fracture subluxation. Neurosurgery. 1991;29(3):374–9.
Ordonez BJ, Benzel EC, Naderi S, Weller SJ. Cervical facet dislocation: techniques for ventral reduction and stabilization. J Neurosurg. 2000;92(Suppl 1):S18-23.
Zhang Z, Liu C, Mu Z, et al. Anterior facetectomy for reduction of cervical facet dislocation. Spine (Phila Pa 1976). 2016;41(7):e403–9.
Feng G, Hong Y, Li L, et al. Anterior decompression and nonstructural bone grafting and posterior fixation for cervical facet dislocation with traumatic disc herniation. Spine (Phila Pa 1976). 2012;37(25):2082–8.
Reindl R, Ouellet J, Harvey EJ, Berry G, Arlet V. Anterior reduction for cervical spine dislocation. Spine (Phila Pa 1976). 2006;31(6):648–52.
Bozkus H, Ames CP, Chamberlain RH, et al. Biomechanical analysis of rigid stabilization techniques for three-column injury in the lower cervical spine. Spine (Phila Pa 1976). 2005;30(8):915–22.
Do Koh Y, Lim TH, Won You J, Eck J, An HS. A biomechanical comparison of modern anterior and posterior plate fixation of the cervical spine. Spine (Phila Pa 1976). 2001;26(1):15–21.
Tofuku K, Koga H, Yone K, Komiya S. Distractive flexion injuries of the subaxial cervical spine treated with a posterior procedure using cervical pedicle screws or a combined anterior and posterior procedure. J Clin Neurosci. 2013;20(5):697–701.
Wang B, Zhu Y, Jiao Y, et al. A new anterior-posterior surgical approach for the treatment of cervical facet dislocations. J Spinal Disord Tech. 2014;27(3):e104–9.
Rabb CH, Lopez J, Beauchamp K, Witt P, Bolles G, Dwyer A. Unilateral cervical facet fractures with subluxation: injury patterns and treatment. J Spinal Disord Tech. 2007;20(6):416–22.
Klekamp JW, Ugbo JL, Heller JG, Hutton WC. Cervical transfacet versus lateral mass screws: a biomechanical comparison. J Spinal Disord. 2000;13(6):515–8.
DalCanto RA, Lieberman I, Inceoglu S, Kayanja M, Ferrara L. Biomechanical comparison of transarticular facet screws to lateral mass plates in two-level instrumentations of the cervical spine. Spine (Phila Pa 1976). 2005;30(8):897–902.
Miyanji F, Mahar A, Oka R, Newton P. Biomechanical differences between transfacet and lateral mass screw-rod constructs for multilevel posterior cervical spine stabilization. Spine (Phila Pa 1976). 2008;33(23):e865–9.
Aydogan M, Enercan M, Hamzaoglu A, Alanay A. Reconstruction of the subaxial cervical spine using lateral mass and facet screw instrumentation. Spine (Phila Pa 1976). 2012;37(5):e335–41.
Jin C, Wang Z, Liu P, Liu YY, Wang ZW, Xie N. A biomechanical analysis of anterior cervical discectomy and fusion alone or combined cervical fixations in treating compression-extension injury with unilateral facet joint fracture: a finite element study. BMC Musculoskelet Disord. 2021;22(1):938.
Kirshblum SC, Burns SP, Biering-Sorensen F, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34(6):535–46.
Huskisson EC. Measurement of pain. Lancet. 1974;2(7889):1127–31.
Molinari RW, Khera OA, Gruhn WL, McAssey RW. Rigid cervical collar treatment for geriatric type II odontoid fractures. Eur Spine J. 2012;21(5):855–62.
Abumi K, Shono Y, Ito M, Taneichi H, Kotani Y, Kaneda K. Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine (Phila Pa 1976). 2000;25(8):962–9.
Liu G, Xu R, Ma W, Sun S, Feng J. Anatomical considerations for the placement of cervical transarticular screws. J Neurosurg Spine. 2011;14(1):114–21.
Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Jt Surg Am. 1958;40-A(3):607–24.
Liu P, Zhao J, Liu F, Liu M, Fan W. A novel operative approach for the treatment of old distractive flexion injuries of subaxial cervical spine. Spine (Phila Pa 1976). 2008;33(13):1459–64.
Vaccaro AR, Falatyn SP, Flanders AE, Balderston RA, Northrup BE, Cotler JM. Magnetic resonance evaluation of the intervertebral disc, spinal ligaments, and spinal cord before and after closed traction reduction of cervical spine dislocations. Spine (Phila Pa 1976). 1999;24(12):1210–7.
Grant GA, Mirza SK, Chapman JR, et al. Risk of early closed reduction in cervical spine subluxation injuries. J Neurosurg. 1999;90(Suppl 1):S13–8.
Zhao L, Xu R, Liu J, et al. The study on comparison of 3 techniques for transarticular screw placement in the lower cervical spine. Spine (Phila Pa 1976). 2012;37(8):e468–72.
Horn EM, Theodore N, Crawford NR, Bambakidis NC, Sonntag VK. Transfacet screw placement for posterior fixation of C-7. J Neurosurg Spine. 2008;9(2):200–6.
Yi S, Rim DC, Nam KS, et al. Biomechanical comparison of cervical fixation via transarticular facet screws without rods versus lateral mass screws with rods. World Neurosurg. 2015;83(4):548–52.
Lifeso RM, Colucci MA. Anterior fusion for rotationally unstable cervical spine fractures. Spine (Phila Pa 1976). 2000;25(16):2028–34.
Acknowledgements
Funding
This study and the journal’s Rapid Service Fee were funded by the National Natural Science Foundation of China (Grant No. 81974190) and the Science and Technology Commission of Shanghai Municipality (Grant No. 19411962900).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole and have given their approval for this version to be published.
Author Contributions
Conceptualization: Ning Xie; methodology: Chen Jin and Ning Xie; formal analysis and investigation: Chen Jin, Jianjie Wang and Yilong Ren; writing—original draft preparation: Chen Jin and Ning Xie; writing—review and editing: Chen Jin, Ning Xie, Jianjie Wang, Yilong Ren and Qunfeng Guo and Lianshun Jia; funding acquisition: Ning Xie; resources: Ning Xie and Liming Cheng; supervision: Ning Xie and Liming Cheng.
Compliance with Ethics Guidelines
The study was conducted according to the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of Tongji Hospital of Tongji University (reference number: K-2021-009), which waived the informed consent due to the retrospective nature of study.
Disclosures
Chen Jin, Ning Xie, Jianjie Wang, Yilong Ren, Qunfeng Guo, Lianshun Jia and Liming Cheng have nothing to disclose.
Data Availability
The datasets generated and/or analyzed during the current study are not publicly available due to the data is confidential patient data but are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Jin, C., Xie, N., Wang, J. et al. Clinical and Radiographic Outcomes of Combined Posterior Transfacet Screw Fixation and Anterior Cervical Discectomy and Fusion Surgery for Unilateral Cervical Facet Fracture with Traumatic Disc Herniation: A Retrospective Cohort Study. Pain Ther 11, 225–240 (2022). https://doi.org/10.1007/s40122-021-00349-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-021-00349-7