Abstract
Introduction
Traumatic subaxial fractures account for more than half of all cervical spine injuries. The optimal surgical approach is a matter of debate and may include anterior, posterior or a combined anteroposterior (360º) approach. Analyzing a cohort of patients initially treated with anterior cervical discectomy and fusion (ACDF) for traumatic subaxial injuries, the study aimed to identify predictors for treatment failure and the subsequent need for supplementary posterior fusion (PF).
Methods
A retrospective, single center, consecutive cohort study of all adult patients undergoing primary ACDF for traumatic subaxial cervical spine fractures between 2006 and 2018 was undertaken and 341 patients were included. Baseline clinical and radiological data for all included patients were analyzed and 11 cases of supplementary posterior fixation were identified.
Results
Patients were operated at a median of 2.0 days from the trauma, undergoing 1-level (78%), 2-levels (16%) and ≥ 3-levels (6.2%) ACDF. A delayed supplementary PF was performed in 11 cases, due to ACDF failure. On univariable regression analysis, older age (p = 0.017), shorter stature (p = 0.031), posterior longitudinal ligament (PLL) injury (p = 0.004), injury to ligamentum flavum (p = 0.005), bilateral facet joint dislocation (p < 0.001) and traumatic cervical spondylolisthesis (p = 0.003) predicted ACDF failure. On the multivariable regression model, older age (p = 0.015), PLL injury (p = 0.048), and bilateral facet joint dislocation (p = 0.010) remained as independent predictors of ACDF failure.
Conclusions
ACDF is safe and effective for the treatment of subaxial cervical spine fractures. High age, bilateral facet joint dislocation and traumatic PLL disruption are independent predictors of failure. We suggest increased vigilance regarding these cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Traumatic subaxial cervical spine fractures constitute the majority of cervical spine injuries. Cases with low-grade instability may be treated nonsurgically with external cervical stabilization; while, cases with high-grade instability require fixation surgery. The surgical options include anterior, posterior, or combined anteroposterior (360°) fixations. However, the optimal surgical approach is still a matter of debate [1,2,3,4]. Anterior cervical instrumentation, including anterior cervical discectomy and fusion (ACDF) and corpectomy and fusion (ACCF) are common approaches for the treatment of subaxial cervical spine fractures. In a systematic review on 300 000 patients, early graft or instrumentation failure was reported in about 2% of all procedures [5]. The exact mechanisms behind construct failure are poorly described, but suboptimal implant placement [6] and poor bone quality [7] are important factors. Cases with unsatisfactory anterior fixations can be successfully managed with supplementary posterior fixations (PF) [6, 7]. However, in selected cases, repeat surgery can be avoided if anteroposterior (360) surgery is performed at index surgery. Recent studies show that patients with subaxial spine injuries were equally satisfied and reported similar health-related quality of life (HRQoL) measures, regardless of the surgical approach [8, 9]. Nonetheless, anteroposterior surgery is more extensive and carries greater surgical risks due to increased duration of surgery and two incision sites [8], necessitating well defined guidelines to support clinical decision making when identifying these cases [10]. The study sought to define predictors of ACDF failure and the need of PF in patients primarily treated with ACDF, aiming to identify patients that would benefit from an anteroposterior fixation at index surgery. Improved decision making at index surgery may reduce the likelihood for postoperative neurological deterioration, renewed surgery, longer hospital stay, and delayed rehabilitation.
Material and methods
Patient selection
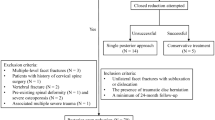
This retrospective, single-center study was performed in accordance with the STROBE guidelines and was approved by the Regional Ethical Review Board (Dnr: 2016/1708–31/4) that waived the need for informed consent. The study hospital is a publicly funded tertiary care center serving a region of approximately two million inhabitants. It is the region’s only level 1 trauma center and handles the majority of the spinal trauma cases in the region. Patients were identified through the surgical management software Orbit (Evry Healthcare Systems, Solna, Sweden). Medical records and imaging data from digital hospital charts were retrospectively reviewed using the health record software TakeCare (Compu Group Medical Sweden AB, Farsta, Sweden). A total of 415 adult patients treated with ACDF during the period of 2006 to 2018 were screened and 341 cases with traumatic injuries and complete records were included in the study. The inclusion criteria were traumatic subaxial cervical spine injury, treated with single- or multilevel ACDF at index surgery. The exclusion criteria were ankylosing spondylitis, non-traumatic cases, traumatic cases primarily treated with posterior or anteroposterior surgery, traumatic cases treated with ACCF and cases with incomplete records. Preoperative diagnostic imaging included, in the vast majority, an initial trauma CT scan followed by an MRI.
Surgical techniques
All surgeries were performed by one or more senior neurosurgeons. For ACDF, a standard right-sided Smith–Robinson approach was performed. Discectomy and osteophyte removal was performed with microsurgical technique to ensure spinal cord decompression, but the posterior longitudinal ligament was typically not opened unless disrupted due to the trauma. PEEK (polyetheretherketone) cages were used in all cases. Adequate alignment and correct position of the cage was confirmed by fluoroscopy. An anterior plate was then positioned, bridging the vertebrae above and below the cage(s) and stabilized with bicortical screws under fluoroscopic guidance.
Construct failure was defined as instrumentation failure, implant subsidence, loss of alignment, screw loosening or combinations of theses resulting in radiological instability.
Supplementary PF was performed with the patient in the prone position and the head fixed in a Mayfield clamp. A midline incision was used to expose the posterior aspects of the spine. Lateral mass screws were placed, typically 2 levels above and below the fracture. When needed, fixations were extended to the upper thoracic levels, where pedicle screws were placed. Cross-links were used when fixations extended 4 levels or more.
Postoperative follow-up
Patients were mobilized without collars after surgery. Postoperative neurological examination was performed within the first 24 h. Complications were categorized based on their severity grade according to the Ibanez classification scheme. [11] In adherence with routine protocols, all patients underwent a postoperative low-dose CT scan within 24 h from surgery and follow-up low-dose CT scans at approximately 4 weeks and 3 months after the initial surgery. All patients were clinically evaluated by their surgeon after 3 months. Additional imaging was performed if clinically indicated. When supplementary PF was performed, the above-mentioned follow-up imaging protocol was repeated.
Statistics
Categorical data are presented as numbers (proportions). The normality of continuous variables was evaluated using the Shapiro–Wilk test. Since all continuous variables deviated significantly from a normal distribution pattern, medians, and interquartile ranges (IQR) were used. To identify predictors of ACDF failure and the need for delayed PF, a univariable logistic regression was used with delayed PF as the outcome and possible predictors as explanatory variables. Factors that showed a trend toward significance in the univariate analysis (p < 0.1) were then entered into a step-down multivariable logistic regression to determine independent risk factors. In the stepwise model, the least significant variable was sequentially eliminated until only significant variables remained. Listwise deletion was used to handle missing data. Statistical significance was set to p < 0.05. All analyses were conducted using the statistical software program R (version 4.1.2).
Results
Baseline data
In total 415 patients with traumatic cervical spine injuries were screened and 74 were excluded due to ACCF (n = 19), prior cervical surgery (n = 15), ankylosing spondylitis (n = 13), or incomplete records (n = 27).
For the remaining 341 patients, the most common trauma mechanisms were motor vehicle accidents (32%), falls from a height (29%), and same level falls (27%). The most common injuries were anterior longitudinal ligament (ALL) disruptions (87%) followed by traumatic disc ruptures (63%). ALL disruptions in combination with other radiological signs of instability constituted unstable injuries. The preoperative ASIA-IS (AIS) grades were D (28%), C (16%), B (5.3%) and A (5.3%); while, 45% of the patients were neurologically intact (Table 1).
ACDF failure and delayed PF
Patients were operated at a median of 2.0 days from the trauma, undergoing 1-level (78%), 2-levels (16%) and ≥ 3-levels (6.2%) ACDF. Surgical site infections requiring antibiotic therapy occurred in 8 (2.3%) and requiring surgical revision in 3 (0.9%). One case of postoperative hematoma (0.3%) and one case of vertebral artery injury (0.3%) were reported (Table 2).
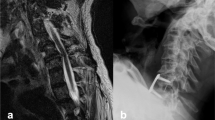
A delayed supplementary PF was performed in 11 cases (3.2%) within a median of 20 days from the index surgery (Table 3). In all cases PF was performed due to construct failure with radiological signs of instability. The patients in the PF group were older (medians 74 vs 59 years) and more frequently smokers (45% vs 32%). A posterior longitudinal ligament injury was seen in 9 (82%) and 7 (64%) had bilateral facet joint dislocation. A combined injury to the PLL, ligamentum flavum, and a bilateral facet dislocation was seen in 27 patients, 6 of whom had failure (22%). A combined PLL, flavum injury, and either uni- or bilateral facet dislocation was seen in 49: of whom 7 had failure (14%). A combined PLL injury and bilateral facet dislocation was seen in 37: of whom 6 had failure (16%). In total, among these patients, 10 (91%) underwent 1-level and 1 (9%) a 3-level ACDF at index surgery (Tables 1 and 2). A median of 5-levels [range: 4–7] were treated with PF. One patient worsened neurologically after ACDF and before PF.
Predictors of ACDF failure and the need for delayed PF
In a univariable regression model designed to identify index surgery predictors of delayed PF, significant association was seen for age (OR = 1.06, p = 0.017), height (OR = 0.92, p = 0.031), PLL injury (OR = 9.78, p = 0.004), ligamentum flavum injury (OR = 7.00, p = 0.005), bilateral facet joint dislocation (OR = 12.0, p < 0.001), and traumatic spondylolisthesis (OR = 10.3, p = 0.003) (Table 4).
Of the above, step-down multivariable logistic regression identified age (OR = 1.07, p = 0.015), PLL injury (OR = 5.61, p = 0.048), and bilateral facet joint dislocation (OR = 6.54, p = 0.010) as independent predictors of ACDF failure and the need for delayed PF (Table 4).
On conditional density (CD) plot of the probability density of delayed PF (y-axis) as a function of age (x-axis), we observed an initial tentative increase in the probability density of delayed PF at 40 years, followed by a steep increase after 60 years (Fig. 1).
Discussion
In this single-center retrospective study of 341 consecutive cases of subaxial cervical spine fractures treated with ACDF and followed for 4.7 years, 3% exhibited ACDF failure that required supplementary PF within three weeks. Age over 60 years, PLL injury and bilateral facet joint dislocation were identified as independent predictors of ACDF failure and the need for supplementary PF. ACDF surgery is a common surgical approach for cervical injuries, but the choice of approach can vary depending on the nature of the injury as well as patient specific factors [7]. Predictors for reoperation, or complications that may lead to reoperation are poorly studied in traumatic ACDF compared to ACDF for degenerative disorders [12,13,14,15]. An anterior approach is suitable for most subaxial cervical injuries where the main goals are spinal cord decompression, restoration of alignment, and fusion of the injured segments [7, 16]. Factors such as a fracture’s involvement of the vertebral body or the presence of a traumatic disc rupture are considered before the decision of surgical approach [7]. Other criteria that determine the management strategy are individual patient aspects such as age, general health, comorbidities, and bone quality. Brodke et al. compared the outcomes of 52 patients with reduced unstable cervical fractures and spinal cord injuries, randomized to either anterior or posterior stabilization. They reported that there were no significant differences in fusion rates, neurological recovery or long-term complaints of pain with regards to the chosen approach [17]. In general, the anterior approach offers easier access to the vertebra and the disc while also utilizing a safer supine patient position [18]. The anterior approach has, however, some limitations. Johnson et al. reported a 13% failure rate for traumatic superior endplate compression fractures, which required a supplementary PF [19].
Historically, several models to assess cervical spine stability have been proposed. Holdsworth described a two-column model where the posterior column including the posterior bony structures and the posterior ligaments was the key to maintaining stability [20]. In the three-column concept of spinal stability proposed by Denis, the middle column consisting of the posterior longitudinal ligament (PLL), the posterior one-third of the vertebral body and the intervertebral disc was the key to stability [21]. A stage 2 distractive-extension injury according to the Spine Trauma Study Group classification, is considered extremely unstable due to injury to the PLL with retrolisthesis of the cephalad vertebra which may result in spinal cord compression [22]. Our findings are well in line with these classification models where a PLL injury is an independent predictor of greater instability. Similarly, bilateral facet joint injury, a posterior column injury is indicative of greater instability and was also identified as an independent predictor of ACDF failure.
Cadaveric, biomechanical studies on bilateral facet joint injuries have reported superior stabilization when PF was performed compared to ACDF [23, 24]. Failure rates of 5–54%, after ACDF for facet joint injuries have been reported [19, 25, 26]. This variability could be due to differences in the relative contribution of uni- and bilateral facet joint injuries, small sample sizes and differences in surgical techniques and instrumentations. However, several clinical studies report successful treatment results with ACDF, with high fusion and low infection rates [19, 25, 27, 28]. Suggested solutions to lower failure rates include plates with screw locking mechanism, use of longer (bicortical) screws, accentuating the lordosis and avoiding large interbody grafts to prevent facet distraction [29]. Anissipour et al. described a series with 16 unilateral and 20 bilateral facet dislocations treated with ACDF [29]. The failure rate was 8% and the main predictor was endplate fracture at the inferior level. Johnson et al. described 65 bilateral and 22 unilateral single segment facet injuries in a cohort with the mean age of 37 years [19]. In their study, the authors could not identify a correlation between facet injury and failure; while, they found that injuries at C6-C7 were at higher risk of failure. The strongest correlation with radiographic failure was with endplate fractures. We had a similar failure rate due to facet joint dislocation and found it to be an independent predictor of failure. Other dissimilarities include the considerably higher age in our cohort (60 vs 37 years). Age at surgery was identified as an independent and significant predictor of ACDF failure and subsequent PF, in our study. The need for supplementary PF in our material rises steeply after the age of 60 years (Fig. 1). Age has previously been identified as a risk factor for medical complications. However, reports on surgical complications after ACDF due to age are scarce [30,31,32,33].
Our findings indicate that ACDF is a safe and effective method for surgical stabilization in subaxial cervical spine injuries with 97% success rate and mostly minor complications. A subgroup of 11 patients (3%) exhibited ACDF failure and required a supplementary PF in the early postoperative period (Table 3). These cases were mainly older patients with factors contributing to a higher degree of instability (i.e., three-column injury). We argue that a staged PF in immediate proximity to the index surgery could have been considered in these cases.
Strengths and limitations
The strengths of this study reside in its large sample size, availability of radiological imaging at injury and follow-up, and the long follow-up period. The limitations are inherent to the retrospective and single-center design of the study. Also, no patient-reported outcome measures reflecting the health-related quality of life in this patient group were available.
Conclusion
Conclusions: ACDF is a safe and effective approach for the treatment of subaxial cervical spine fractures, with a relatively low failure rate of 3%. Our findings indicate that high age, bilateral facet joint dislocation, and traumatic PLL disruption are independent predictors of failure. Increased vigilance is hence warranted in these cases and alternative approaches including a combined anteroposterior one may be considered at index surgery. This study provides pivotal insights for the informed decision-making when treating patients with traumatic subaxial spine injuries.
References
Frojd Revesz D, Norell A, Charalampidis A, Endler P, Gerdhem P (2021) Subaxial spine fractures: a comparison of patient-reported outcomes and complications between anterior and posterior surgery. Spine (Phila Pa 1976) 46(17):E926-E931
Samuel S, Lin JL, Smith MM et al (2015) Subaxial injury classification scoring system treatment recommendations: external agreement study based on retrospective review of 185 patients. Spine (Phila Pa 1976) 40(3):137–142
Sharif S, Ali MYJ, Sih IMY, Parthiban J, Alves OL (2020) Subaxial cervical spine injuries: WFNS Spine Committee Recommendations. Neurospine 17(4):737–758
Rezaee H, Keykhosravi E, Mashhadinejad M, Pishjoo M (2021) Comparison of anterior, posterior, and combined surgical approaches on the outcomes of patients suffering from subaxial cervical spine injuries. Bull Emerg Trauma 9(3):133–137
Yee TJ, Swong K, Park P (2020) Complications of anterior cervical spine surgery: a systematic review of the literature. J Spine Surg 6(1):302–322
Belirgen M, Dlouhy BJ, Grossbach AJ, Torner JC, Hitchon PW (2013) Surgical options in the treatment of subaxial cervical fractures: a retrospective cohort study. Clin Neurol Neurosurg 115(8):1420–1428
Dvorak MF, Fisher CG, Fehlings MG et al (2007) The surgical approach to subaxial cervical spine injuries: an evidence-based algorithm based on the SLIC classification system. Spine (Phila Pa 1976) 32(23):2620–2629
Singh A, Blixt S, Edstrom E, Elmi-Terander A, Gerdhem P (2023) Outcome and health related quality of life after combined anteroposterior surgery vs anterior surgery alone in subaxial cervical spine fractures: analysis of a national multicenter dataset. Spine (Phila Pa 1976)
El-Hajj VG, Singh A, Blixt S, Edstrom E, Elmi-Terander A, Gerdhem P (2023) Evolution of patient-reported outcome measures, 1, 2, and 5 years after surgery for subaxial cervical spine fractures, a nation-wide registry study. Spine J
Tatter C, Persson O, Burstrom G, Edstrom E, Elmi-Terander A (2020) Anterior cervical corpectomy and fusion for degenerative and traumatic spine disorders, single-center experience of a case series of 119 patients. Oper Neurosurg (Hagerstown) 20(1):8–17
Landriel Ibanez FA, Hem S, Ajler P et al (2011) A new classification of complications in neurosurgery. World Neurosurg 75(5–6):709–715; discussion 604–711
Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH (1999) Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 81(4):519–528
Lee JC, Lee SH, Peters C, Riew KD (2014) Risk-factor analysis of adjacent-segment pathology requiring surgery following anterior, posterior, fusion, and nonfusion cervical spine operations: survivorship analysis of 1358 patients. J Bone Joint Surg Am 96(21):1761–1767
Kelly MP, Eliasberg CD, Riley MS, Ajiboye RM, SooHoo NF (2018) Reoperation and complications after anterior cervical discectomy and fusion and cervical disc arthroplasty: a study of 52,395 cases. Eur Spine J 27(6):1432–1439
Chambers JS, Kropp RG, Gardocki RJ (2023) Reoperation rates and patient-reported outcomes of single and two-level anterior cervical discectomy and fusion. Arch Orthop Trauma Surg 143(1):265–268
Schleicher P, Kobbe P, Kandziora F et al (2018) Treatment of injuries to the subaxial cervical spine: recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Global Spine J 8(2 Suppl):25S-33S
Brodke DS, Anderson PA, Newell DW, Grady MS, Chapman JR (2003) Comparison of anterior and posterior approaches in cervical spinal cord injuries. J Spinal Disord Tech 16(3):229–235
Tabarestani TQ, Lewis NE, Kelly-Hedrick M et al (2022) Surgical considerations to improve recovery in acute spinal cord injury. Neurospine 19(3):689–702
Johnson MG, Fisher CG, Boyd M, Pitzen T, Oxland TR, Dvorak MF (2004) The radiographic failure of single segment anterior cervical plate fixation in traumatic cervical flexion distraction injuries. Spine (Phila Pa 1976) 29(24):2815–2820
Holdsworth F (1970) Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg Am 52(8):1534–1551
Denis F (1983) The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 8(8):817–831
Zaveri G, Das G (2017) Management of sub-axial cervical spine injuries. Indian J Orthop 51(6):633–652
Do Koh Y, Lim TH, Won You J, Eck J, An HS (2001) A biomechanical comparison of modern anterior and posterior plate fixation of the cervical spine. Spine (Phila Pa 1976) 26(1):15–21
Coe JD, Warden KE, Sutterlin CE, 3rd, McAfee PC (1989) Biomechanical evaluation of cervical spinal stabilization methods in a human cadaveric model. Spine (Phila Pa 1976) 14(10):1122–1131
Razack N, Green BA, Levi AD (2000) The management of traumatic cervical bilateral facet fracture-dislocations with unicortical anterior plates. J Spinal Disord 13(5):374–381
Henriques T, Olerud C, Bergman A, Jonsson H Jr (2004) Distractive flexion injuries of the subaxial cervical spine treated with anterior plate alone. J Spinal Disord Tech 17(1):1–7
Song KJ, Lee KB (2008) Anterior versus combined anterior and posterior fixation/fusion in the treatment of distraction-flexion injury in the lower cervical spine. J Clin Neurosci 15(1):36–42
Kwon BK, Fisher CG, Boyd MC et al (2007) A prospective randomized controlled trial of anterior compared with posterior stabilization for unilateral facet injuries of the cervical spine. J Neurosurg Spine 7(1):1–12
Anissipour AK, Agel J, Baron M, Magnusson E, Bellabarba C, Bransford RJ (2017) Traumatic cervical unilateral and bilateral facet dislocations treated with anterior cervical discectomy and fusion has a low failure rate. Global Spine J 7(2):110–115
Di Capua J, Somani S, Kim JS et al (2017) Elderly age as a risk factor for 30-day postoperative outcomes following elective anterior cervical discectomy and fusion. Global Spine J 7(5):425–431
Narain AS, Hijji FY, Haws BE et al (2020) Risk factors for medical and surgical complications after 1-2-level anterior cervical discectomy and fusion procedures. Int J Spine Surg 14(3):286–293
Buerba RA, Giles E, Webb ML, Fu MC, Gvozdyev B, Grauer JN (2014) Increased risk of complications after anterior cervical discectomy and fusion in the elderly: an analysis of 6253 patients in the American College of Surgeons National Surgical Quality Improvement Program database. Spine (Phila Pa 1976) 39(25):2062–2069
Lawless MH, Tong D, Claus CF et al (2022) Age as a risk factor for complications following anterior cervical discectomy and fusion: analysis from the Michigan Spine Surgery Improvement Collaborative (MSSIC). Spine (Phila Pa 1976) 47(4):343–351
Funding
Open access funding provided by Karolinska Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors report any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Singh, A., El-Hajj, V.G., Fletcher-Sandersjöö, A. et al. Predictors of failure after primary anterior cervical discectomy and fusion for subaxial traumatic spine injuries. Eur Spine J 33, 2332–2339 (2024). https://doi.org/10.1007/s00586-024-08264-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-024-08264-z