Abstract
Purpose
Blood culture contamination is still a frequently observed event and may lead to unnecessary antibiotic prescriptions and additional hazards and costs. However, in patients hospitalized in tertiary care, true bacteremias for pathogens that are classically considered as contaminants can be observed. We assessed the diagnostic accuracy of procalcitonin for differentiating blood culture contamination from bacteremia in patients with positive blood cultures for potential contaminants.
Methods
We carried out a retrospective, cross-sectional, observational study on consecutive patients hospitalized between January 2016 and May 2019 at the University Hospital of Nancy and who had a positive peripheral blood culture for a pathogen classically considered as a potential contaminant.
Results
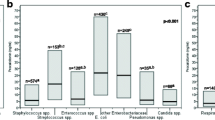
During the study period, 156 patients were screened, and 154 were retained in the analysis. Among the variables that were significantly associated with a diagnosis of blood culture contamination in univariate analyses, four were maintained in multivariate logistic regression analysis: a number of positive blood culture bottles ≤ 2 (OR 23.76; 95% CI 1.94–291.12; P = 0.01), procalcitonin < 0.1 ng/mL (OR 14.88; 95% CI 1.62–136.47; P = 0.02), non-infection-related admission (OR 13.00; 95% CI 2.17–77.73; P = 0.005), and a percentage of positive blood culture bottles ≤ 25% (OR 12.15; 95% CI 2.02–73.15; P = 0.006).
Conclusions
These data provide new evidence on the usefulness of plasma procalcitonin as a reliable diagnostic biomarker in the diagnostic algorithm of peripheral blood culture contamination among patients hospitalized in tertiary care.
Clinical trial
ClinicalTrials.gov #NCT04573894.

Similar content being viewed by others
Data availability
Anonymized patient data are available for use in collaborative studies to researchers upon reasonable request (a.lozniewski@chru-nancy.fr and abderrahim.oussalah@univ-lorraine.fr). Data will be provided following the review and approval of a research proposal (including a statistical analysis plan) and the completion of a data-sharing agreement. Responses to the request for the raw data will be judged by the IRB of the University Hospital of Nancy.
References
Doern GV, Carroll KC, Diekema DJ, Garey KW, Rupp ME, Weinstein MP, et al. Practical guidance for clinical microbiology laboratories: a comprehensive update on the problem of blood culture contamination and a discussion of methods for addressing the problem. Clin Microbiol Rev. 2019;33:e00009-19.
Bassetti M, Russo A, Righi E, Dolso E, Merelli M, D’Aurizio F, et al. Role of procalcitonin in bacteremic patients and its potential use in predicting infection etiology. Expert Rev Anti Infect Ther. 2019;17:99–105.
Oussalah A, Ferrand J, Filhine-Tresarrieu P, Aissa N, Aimone-Gastin I, Namour F, et al. Diagnostic accuracy of procalcitonin for predicting blood culture results in patients with suspected bloodstream infection: an observational study of 35,343 consecutive patients (a STROBE-compliant article). Medicine (Baltimore). 2015;94:e1774.
Schuetz P, Albrich W, Mueller B. Procalcitonin for diagnosis of infection and guide to antibiotic decisions: past, present and future. BMC Med. 2011;9:107.
Jeong S, Park Y, Cho Y, Kim HS. Diagnostic utilities of procalcitonin and C-reactive protein for the prediction of bacteremia determined by blood culture. Clin Chim Acta. 2012;413:1731–6.
Schuetz P, Mueller B, Trampuz A. Serum procalcitonin for discrimination of blood contamination from bloodstream infection due to coagulase-negative staphylococci. Infection. 2007;35:352–5.
Shomali W, Hachem R, Chaftari AM, Bahu R, Helou GE, Jiang Y, et al. Can procalcitonin differentiate Staphylococcus aureus from coagulase-negative staphylococci in clustered gram-positive bacteremia? Diagn Microbiol Infect Dis. 2013;76:158–61.
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988;16:128–40.
Leal J, Gregson DB, Ross T, Flemons WW, Church DL, Laupland KB. Development of a novel electronic surveillance system for monitoring of bloodstream infections. Infect Control Hosp Epidemiol. 2010;31:740–7.
Timsit JF, Ruppe E, Barbier F, Tabah A, Bassetti M. Bloodstream infections in critically ill patients: an expert statement. Intensive Care Med. 2020;46:266–84.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–45.
Efron B, Tibshirani RJ. An introduction to the bootstrap. Taylor & Francis; 1994.
Nagelkerke NJ. A note on a general definition of the coefficient of determination. Biometrika. 1991;78:691–2.
Dargere S, Cormier H, Verdon R. Contaminants in blood cultures: importance, implications, interpretation and prevention. Clin Microbiol Infect. 2018;24:964–9.
Rahkonen M, Luttinen S, Koskela M, Hautala T. True bacteremias caused by coagulase negative Staphylococcus are difficult to distinguish from blood culture contaminants. Eur J Clin Microbiol Infect Dis. 2012;31:2639–44.
Dargere S, Parienti JJ, Roupie E, Gancel PE, Wiel E, Smaiti N, et al. Unique blood culture for diagnosis of bloodstream infections in emergency departments: a prospective multicentre study. Clin Microbiol Infect. 2014;20:O920–7.
Lamy B, Dargere S, Arendrup MC, Parienti JJ, Tattevin P. How to optimize the use of blood cultures for the diagnosis of bloodstream infections? A state-of-the art. Front Microbiol. 2016;7:697.
Lamy B, Sundqvist M, Idelevich EA, ESCMID Study Group for Bloodstream Infections, Endocarditis and Sepsis (ESGBIES). Bloodstream infections—standard and progress in pathogen diagnostics. Clin Microbiol Infect. 2020;26:142–50.
Lamy B, Roy P, Carret G, Flandrois JP, Delignette-Muller ML. What is the relevance of obtaining multiple blood samples for culture? A comprehensive model to optimize the strategy for diagnosing bacteremia. Clin Infect Dis. 2002;35:842–50.
Yu D, Larsson A, Parke A, Unge C, Henning C, Sunden-Cullberg J, et al. Single-sampling strategy vs. multi-sampling strategy for blood cultures in sepsis: a prospective non-inferiority study. Front Microbiol. 2020;11:1639.
Acknowledgements
We wish to thank all the patients and staff from all the units that participated in the study.
Funding
University Hospital of Nancy, Department of Methodology, Promotion, and Investigation.
Author information
Authors and Affiliations
Contributions
Study concept and design: AL and AO; study supervision, guarantors of the article: AL and AO; data collection: CB; statistical analysis: AO; acquisition of data: CB; drafting, review, and approval of the report: CB, NA, AEM, JLG, AO, and AL; critical revision of the manuscript for important intellectual content: CB, NA, AEM, JLG, AO, and AL; approved the final draft submitted: CB, NA, AEM, JLG, AO, and AL.
Corresponding authors
Ethics declarations
Conflict of interest
The authors who have taken part in this study declare that they do not have anything to disclose regarding conflicts of interest concerning this manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Berthezène, C., Aissa, N., Manteaux, A.E. et al. Accuracy of procalcitonin for diagnosing peripheral blood culture contamination among patients with positive blood culture for potential contaminants. Infection 49, 1249–1255 (2021). https://doi.org/10.1007/s15010-021-01697-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-021-01697-4