Abstract
Purpose
Pseudomonas aeruginosa bacteraemia is associated with high mortality, and most monotherapies are beta-lactam-based. We aimed to investigate clinical outcomes of definitive fluoroquinolone monotherapy versus beta-lactam monotherapy for P. aeruginosa bacteraemia.
Methods
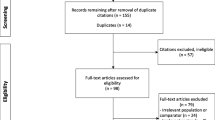
This retrospective study enrolled adult patients receiving definitive monotherapy with beta-lactam or fluoroquinolone between November 2013 and November 2014 at Taipei Veterans General Hospital. The independent risk factors for 28-day mortality were analyzed by logistic regression and propensity score-adjusted analysis.
Results
Among the 105 patients enrolled, 78 patients received beta-lactams and 27 received fluoroquinolones (20 with ciprofloxacin and 7 with levofloxacin). Primary bacteraemia (39.0%) and urinary tract infections (37.1%) were the most common sources of bacteraemia. The 28-day mortality rate was 11.1% for those receiving fluoroquinolones and 32.1% for those receiving beta-lactams (P = 0.062). The 28-day mortality rate between the two groups stratified by APACHE II and Pitt bacteraemia scores showed no significant differences in each category. Propensity score-adjusted multivariate analysis revealed that definitive therapy with a fluoroquinolone was not associated with 28-day mortality (OR 0.42; 95% CI 0.08–2.23; P = 0.305).
Conclusions
Fluoroquinolone might be an alternative to beta-lactam as a definitive monotherapy for P. aeruginosa bacteraemia provided they are active in vitro. Our results could be a basis for further studies and provide a possible target for antibiotic stewardship interventions in P. aeruginosa bacteraemia.
Similar content being viewed by others
References
Kang CI, Kim SH, Kim HB, Park SW, Choe YJ, Oh MD, et al. Pseudomonas aeruginosa bacteremia: risk factors for mortality and influence of delayed receipt of effective antimicrobial therapy on clinical outcome. Clin Infect Dis. 2003;37:745–51. https://doi.org/10.1086/377200.
Micek ST, Lloyd AE, Ritchie DJ, Reichley RM, Fraser VJ, Kollef MH. Pseudomonas aeruginosa bloodstream infection: importance of appropriate initial antimicrobial treatment. Antimicrob Agents Chemother. 2005;49:1306–11. https://doi.org/10.1128/AAC.49.4.1306-1311.2005.
Horino T, Chiba A, Kawano S, Kato T, Sato F, Maruyama Y, et al. Clinical characteristics and risk factors for mortality in patients with bacteremia caused by Pseudomonas aeruginosa. Intern Med. 2012;51:59–64.
Parkins MD, Gregson DB, Pitout JD, Ross T, Laupland KB. Population-based study of the epidemiology and the risk factors for Pseudomonas aeruginosa bloodstream infection. Infection. 2010;38:25–32. https://doi.org/10.1007/s15010-009-9145-9.
Siegman-Igra Y, Ravona R, Primerman H, Giladi M. Pseudomonas aeruginosa bacteremia: an analysis of 123 episodes, with particular emphasis on the effect of antibiotic therapy. Int J Infect Dis. 1998;2:211–5.
Chamot E, Boffi El Amari E, Rohner P, Van Delden C. Effectiveness of combination antimicrobial therapy for Pseudomonas aeruginosa bacteremia. Antimicrob Agents Chemother. 2003;47:2756–64.
Lodise TP Jr, Patel N, Kwa A, Graves J, Furuno JP, Graffunder E, et al. Predictors of 30-day mortality among patients with Pseudomonas aeruginosa bloodstream infections: impact of delayed appropriate antibiotic selection. Antimicrob Agents Chemother. 2007;51:3510–5. https://doi.org/10.1128/AAC.00338-07.
Bliziotis IA, Petrosillo N, Michalopoulos A, Samonis G, Falagas ME. Impact of definitive therapy with beta-lactam monotherapy or combination with an aminoglycoside or a quinolone for Pseudomonas aeruginosa bacteremia. PLoS One. 2011;6:e26470. https://doi.org/10.1371/journal.pone.0026470.
Schechner V, Gottesman T, Schwartz O, Korem M, Maor Y, Rahav G, et al. Pseudomonas aeruginosa bacteremia upon hospital admission: risk factors for mortality and influence of inadequate empirical antimicrobial therapy. Diagn Microbiol Infect Dis. 2011;71:38–45. https://doi.org/10.1016/j.diagmicrobio.2011.05.010.
Pena C, Suarez C, Ocampo-Sosa A, Murillas J, Almirante B, Pomar V, et al. Effect of adequate single-drug vs combination antimicrobial therapy on mortality in Pseudomonas aeruginosa bloodstream infections: a post Hoc analysis of a prospective cohort. Clin Infect Dis. 2013;57:208–16. https://doi.org/10.1093/cid/cit223.
Bowers DR, Liew YX, Lye DC, Kwa AL, Hsu LY, Tam VH. Outcomes of appropriate empiric combination versus monotherapy for Pseudomonas aeruginosa bacteremia. Antimicrob Agents Chemother. 2013;57:1270–4. https://doi.org/10.1128/AAC.02235-12.
Kim YJ, Jun YH, Kim YR, Park KG, Park YJ, Kang JY, et al. Risk factors for mortality in patients with Pseudomonas aeruginosa bacteremia; retrospective study of impact of combination antimicrobial therapy. BMC Infect Dis. 2014;14:161. https://doi.org/10.1186/1471-2334-14-161.
Morata L, Cobos-Trigueros N, Martinez JA, Soriano A, Almela M, Marco F, et al. Influence of multidrug resistance and appropriate empirical therapy on the 30-day mortality rate of Pseudomonas aeruginosa bacteremia. Antimicrob Agents Chemother. 2012;56:4833–7. https://doi.org/10.1128/AAC.00750-12.
Tam VH, Rogers CA, Chang KT, Weston JS, Caeiro JP, Garey KW. Impact of multidrug-resistant Pseudomonas aeruginosa bacteremia on patient outcomes. Antimicrob Agents Chemother. 2010;54:3717–22. https://doi.org/10.1128/AAC.00207-10.
Hilf M, Yu VL, Sharp J, Zuravleff JJ, Korvick JA, Muder RR. Antibiotic therapy for Pseudomonas aeruginosa bacteremia: outcome correlations in a prospective study of 200 patients. Am J Med. 1989;87:540–6.
Safdar N, Handelsman J, Maki DG. Does combination antimicrobial therapy reduce mortality in gram-negative bacteraemia? A meta-analysis. Lancet Infect Dis. 2004;4:519–27. https://doi.org/10.1016/S1473-3099(04)01108-9.
Bodey GP, Jadeja L, Elting L. Pseudomonas bacteremia. Retrospective analysis of 410 episodes. Arch Intern Med. 1985;145:1621–9.
Park SY, Park HJ, Moon SM, Park KH, Chong YP, Kim MN, et al. Impact of adequate empirical combination therapy on mortality from bacteremic Pseudomonas aeruginosa pneumonia. BMC Infect Dis. 2012;12:308. https://doi.org/10.1186/1471-2334-12-308.
Vardakas KZ, Tansarli GS, Bliziotis IA, Falagas ME. beta-Lactam plus aminoglycoside or fluoroquinolone combination versus beta-lactam monotherapy for Pseudomonas aeruginosa infections: a meta-analysis. Int J Antimicrob Agents. 2013;41:301–10. https://doi.org/10.1016/j.ijantimicag.2012.12.006.
Hu Y, Li L, Li W, Xu H, He P, Yan X, et al. Combination antibiotic therapy versus monotherapy for Pseudomonas aeruginosa bacteraemia: a meta-analysis of retrospective and prospective studies. Int J Antimicrob Agents. 2013;42:492–6. https://doi.org/10.1016/j.ijantimicag.2013.09.002.
Polk RE, Johnson CK, McClish D, Wenzel RP, Edmond MB. Predicting hospital rates of fluoroquinolone-resistant Pseudomonas aeruginosa from fluoroquinolone use in US hospitals and their surrounding communities. Clin Infect Dis. 2004;39:497–503. https://doi.org/10.1086/422647.
Shorr AF, Susla GB, Kollef MH. Quinolones for treatment of nosocomial pneumonia: a meta-analysis. Clin Infect Dis. 2005;40:S115–22. https://doi.org/10.1086/426191.
West M, Boulanger BR, Fogarty C, Tennenberg A, Wiesinger B, Oross M, et al. Levofloxacin compared with imipenem/cilastatin followed by ciprofloxacin in adult patients with nosocomial pneumonia: a multicenter, prospective, randomized, open-label study. Clin Ther. 2003;25:485–506.
Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, et al. Health care-associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med. 2002;137:791–7.
Chong YP, Moon SM, Bang KM, Park HJ, Park SY, Kim MN, et al. Treatment duration for uncomplicated Staphylococcus aureus bacteremia to prevent relapse: analysis of a prospective observational cohort study. Antimicrob Agents Chemother. 2013;57:1150–6. https://doi.org/10.1128/AAC.01021-12.
Lee NY, Huang YT, Hsueh PR, Ko WC. Clostridium difficile bacteremia, Taiwan. Emerg Infect Dis. 2010;16:1204–10. https://doi.org/10.3201/eid1608.100064.
Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing: twenty-second informational supplement M100–S22. Wayne: CLSI; 2012.
American Thoracic Society, Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416. https://doi.org/10.1164/rccm.200405-644ST.
Kalil AC, Metersky ML, Klompas M, Muscedere J, Sweeney DA, Palmer LB, et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;63:e61–111. https://doi.org/10.1093/cid/ciw353.
Vestergaard M, Paulander W, Marvig RL, Clasen J, Jochumsen N, Molin S, et al. Antibiotic combination therapy can select for broad-spectrum multidrug resistance in Pseudomonas aeruginosa. Int J Antimicrob Agents. 2016;47:48–55. https://doi.org/10.1016/j.ijantimicag.2015.09.014.
Acknowledgements
This work was supported by the Ministry of Science and Technology (MOST 103-2314-B-010-052-MY2) in Taiwan and the Taipei Veterans General Hospital (Grant V105B-001, V106B-001, and V107C-081). We thank the Medical Science and Technology Building of Taipei Veterans General Hospital for providing experimental space and facilities. Some result of this study was presented as an ePoster at the 26th European Congress of Clinical Microbiology and Infectious Diseases (ECCMID) in Amsterdam, Netherlands.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical statement
This study was approved by the Institution Review Board of Taipei Veterans General Hospital, and the written informed consent form was waived.
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wu, PF., Lin, YT., Wang, FD. et al. Is fluoroquinolone monotherapy a useful alternative treatment for Pseudomonas aeruginosa bacteraemia?. Infection 46, 365–373 (2018). https://doi.org/10.1007/s15010-018-1131-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-018-1131-7