Abstract
Background
Pseudomonas aeruginosa has gained an increasing amount of attention in the treatment of patients with pneumonia. However, the benefit of empirical combination therapy for pneumonia remains unclear. We evaluated the effects of adequate empirical combination therapy and multidrug-resistance in bacteremic Pseudomonas pneumonia on the mortality.
Methods
A retrospective cohort study was performed at the 2,700-bed tertiary care university hospital. We reviewed the medical records of patients with bacteremic pneumonia between January 1997 and February 2011. Patients who received either inappropriate or appropriate empirical therapy were compared by using marginal structural model. Furthermore, we investigated the direct impact of combination therapy on clinical outcomes in patients with monomicrobial bacteremic pneumonia.
Results
Among 100 consecutive patients with bacteremic Pseudomonas pneumonia, 65 patients were classified in the adequate empirical therapy group, 32 of whom received monotherapy and 33 combination therapy. In the marginal structural model, only inadequate therapy was significantly associated with 28-day mortality (p = 0.02), and multidrug-resistance was not a significant risk factor.
To examine further the direct impact of combination therapy, we performed a subgroup analysis of the 65 patients who received adequate therapy. Multivariate logistic regression analysis identified absence of septic shock at the time of bacteremia (OR, 0.07; 95% CI, 0.01-0.49; p = 0.008), and adequate combination therapy (OR, 0.05; 95% CI, 0.01-0.34; p = 0.002) as variables independently associated with decreased all-cause 28-day mortality.
Conclusions
Our study suggests that adequate empirical combination therapy can decrease mortality in patients with bacteremic Pseudomonas pneumonia.
Similar content being viewed by others
Background
Pseudomonas aeruginosa has emerged as a significant nosocomial pathogen with a substantial frequency of multidrug resistance (MDR) [1]. Moreover pneumonia caused by P. aeruginosa is known to be associated with greater mortality than infection of other sites [2–5]. Hence, treatment of P. aeruginosa pneumonia poses a great challenge to clinicians. Early studies, mainly of neutropenic patients with bacteremia, showed that mortality was decreased in patients receiving combination therapy [6]. However, the results of subsequent clinical studies on the effect of combination therapy on the treatment of severe P. aeruginosa infection have been conflicting [7–11]. These previous studies had significant limitations, including the enrollment of only small numbers of patients infected with different kinds of gram-negative bacilli and the lack of controls. Furthermore, the validity of diagnoses of P. aeruginosa pneumonia has itself been questioned because P. aeruginosa often colonizes the respiratory tract in hospital settings, and it is often difficult for clinicians to distinguish a colonizer from a true pathogen [2]. Thus, the isolation of P. aeruginosa from blood cultures, as well as respiratory specimens, constitutes strong evidence of true Pseudomonas pneumonia.
To help identify the best strategy for antibiotic therapy in Pseudomonas pneumonia, we evaluated the impact of empirical combination therapy on mortality in 100 consecutive patients with bacteremic P. aeruginosa pneumonia using a risk stratification model to adjust for potential differences.
Methods
Data collection
All patients ≥18 years with P. aeruginosa bacteremic pneumonia between January 1997 and February 2011 were included. Patients with blood cultures positive for P. aeruginosa were identified from the computerized database of the clinical microbiology unit. Infectious diseases doctors then reviewed the medical records of these patients and collected demographic, clinical, and microbiological data. Ultimately, only patients with Pseudomonas pneumonia (see below) were included in the analysis. Patients with polymicrobial infections were excluded. The study was approved by the Asan Medical Center Institutional Review Board (S2012-1034-0001), and the requirement for patient consent was waved due to the retrospective nature of the study.
Definitions
Bacteremia was defined as ≥ 1 positive blood culture for P. aeruginosa and the presence of the clinical features compatible with infection. If a patient had undergone recurrent episodes of P. aeruginosa bacteremia during the study period, only the first episode was considered. Pneumonia was defined as presence of: (1) new radiographic infiltration; (2) one or more of the following symptoms consistent with pneumonia (fever, cough, pleuritic chest pain, and dyspnea); and (3) isolation of P. aeruginosa from cultures of bronchoalveolar lavage (BAL) fluid or appropriate respiratory specimens [12, 13]. The categories of pneumonia have been previously defined [14, 15]. Empirical antibiotic therapy was considered adequate if therapy given intravenously within 48 h of the onset of pneumonia included antimicrobials to which the isolate was susceptible. Patients who received adequate treatment were stratified into 2 groups: a monotherapy group that received only 1 active antimicrobial, and a combination therapy group that simultaneously received 2 active antimicrobials [16]. Antimicrobial susceptibility testing was performed using the MicroScan system with the Neg Breakpoint Combo Panel 44 (Siemens Healthcare Diagnostics Inc., West Sacramento, CA) according to standard criteria of the Clinical and Laboratory Standards Institute [17]. MDR was defined as resistance to more than three classes of antibiotics such as anti-pseudomonal beta-lactams, carbapenems, fluoroquinolones, and aminoglycosides [18].
Statistical analysis
All statistical analyses were performed using SAS software, version 9.1 (SAS Institute Inc, Cary, NC). Marginal structural models were used to estimate the difference in mortality between the adequate therapy group and the inadequate therapy group. Careful adjustment was made using weighted Cox proportional-hazards regression models that were based on the inverse-probability-of-treatment weighted (IPTW) method in order to reduce the effect of potential confounding factors and selection bias in this observational study [19]. IPTW estimation relies on multivariable logistic regression analysis. All variables with a p value < 0.2 on univariable analysis were then introduced into the multivariable logistic regression model, and a backwards stepwise logistic regression was carried out. Sex, age, underlying diseases, multidrug resistance, McCabe score, APACHE II score, Pitt bacteremia score, clinical pulmonary infection score (CPIS), type of pneumonia, and use of previous antibiotics were classified as independent variables for the purposes of this study. P value ≤ 0.05 was considered statistically significant.
Results
During the study period 1,361 patients with P. aeruginosa bacteremia were identified from our hospital records. One hundred (7.3%) patients with concomitant pneumonia were eventually included in the analysis. The demographics, clinical features, microbiologic characteristics and clinical outcomes of these patients are shown in Table 1. Hematologic malignancy (34%) was the most common underlying disease, followed by solid cancer (23%). Of the 100 cases, 37 (37%) originated in the community (18 community-acquired and 19 healthcare-associated infections). Thirty-eight (38.0%) patients presented with septic shock. Sixty-five patients (65.0%) were assigned to the adequate empirical therapy group, 32 (49.2%) of whom received monotherapy and 33 (50.8%) combination therapy. The antimicrobials used in monotherapy were as follows: ceftazidime (n = 10), cefepime (n = 2), carbapenem (n = 8), piperacillin-tazobactam (n = 7), and ciprofloxacin (n = 5). The remainder of the patients received combination therapy: piperacillin-tazobactam plus ciprofloxacin (n = 11), cefoperazone-sulbactam plus aminoglycoside (n = 9), ceftazidime plus aminoglycoside (n = 8), ceftazidime plus ciprofloxacin (n = 3), and carbapenem plus ciprofloxacin (n = 2). MDR pathogens were commonly found in the inadequate therapy group (42.9% [15 of 35] vs. 12.3% [8 of 65], p < 0.001). Among the 65 patients in the adequate therapy group, there was no significant difference in terms of the emergence of antimicrobial resistance between the monotherapy and combination therapy group (21.9% [7/32] and 12.1% [4/33], respectively) (p = 0.29). However, the 2-week bacteria eradication rate (54.5% [18/33] vs.18.8% [6/32], p = 0.04) and the 4-week eradication rate (54.5% [18/33] vs. 28.1% [9/32], p = 0.04) were significantly higher in the combination therapy group than the monotherapy group. There were no subsequent episodes of Pseudomonas pneumonia after 1 month, but there were 6 subsequent episodes within the first 6 months (2 patients in the inadequate therapy group [5.7%], 1 patient in adequate monotherapy group [3.1%], and 3 patients in adequate combination therapy group [9.1%]). However, there were no deaths due to recurrent P. aeruginosa infection, and all patients with subsequent episodes demonstrated full recoveries.
We identified 14 patients who had coinfection at the time of Pseudomonas pneumonia (6 patients in the inadequate therapy group and 8 patients in the adequate therapy group), though the rates of coinfection were not significantly different between the monotherapy group (9.4% [3 of 32]) and the combination therapy group (15.2% [5 of 33], p = 0.71). Of these 14 patients, 8 patients died (4 patients in inadequate therapy, 2 patients in monotherapy, and 2 patients in the combination therapy group), but there were no deaths due to coinfection in either group.
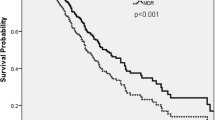
The overall all-cause 28-day mortality was 51.0% (51 of 100). The 28-day mortality was significantly higher in the inadequate therapy group than the adequate therapy group (68.6% [24/35] vs. 41.5% [27/65], p = 0.01). Variables such as sex, age, MDR, McCabe score, APACHE II score, Pitt bacteremia score, CPIS, and the use of previous antibiotics (which were determined to be significant by univariate analysis) were subjected to logistic regression modeling in order to identify the independent risk factors for all-cause mortality. Multivariate analysis indicated that the APACHE II score (adjusted odds ratio [AOR]: 1.08; 95% confidence interval [CI]: 1.02–1.15; p = 0.01) and inadequate therapy (AOR: 2.73; 95% CI: 1.11–6.71; p = 0.03) were independently associated with all-cause 28-day mortality (Additional file 1: Table S1). The marginal structural model was estimated using multiple logistic regression analysis. To reduce the effects of potential confounding factors and selection bias, additional analyses were performed with covariable adjustment using IPTW. These additional analyses showed that only inadequate therapy was significantly associated with 28-day mortality (AOR: 3.02; 95% CI: 1.15–7.93; p = 0.02) and that MDR was not a significant risk factor (data not shown).
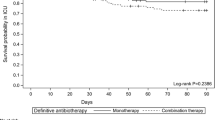
To further examine the direct impact of combination therapy, we performed a subgroup analysis of the 65 patients who received adequate therapy. In univariate analysis, variables that were significantly associated with 28-day mortality included underlying hematologic malignancy, Pitt bacteremia score, initial clinical manifestation of bacteremia, and monotherapy. Multivariate logistic regression analysis identified the absence of septic shock at the time of bacteremia (AOR, 0.07; 95% CI, 0.01-0.49; p = 0.008), and combination therapy (AOR, 0.05; 95% CI, 0.01-0.34; p = 0.002) as variables that were independently associated with decreased all-cause 28-day mortality (Table 2).
Discussion
In our present study, we evaluated the impact of empirical combination therapy on clinical outcomes in 100 consecutive patients with monomicrobial bacteremic Pseudomonas pneumonia. Adequate empirical combination therapy was associated with significantly lower 28-day mortality.
Despite the high mortality rates in patients with P. aeruginosa pneumonia, it is still not clear how best to treat Pseudomonas pneumonia. Paul et al., in their meta-analysis of 64 randomized trials, compared the clinical outcomes of beta lactam monotherapy and beta lactam-aminoglycoside combination therapy for the treatment of sepsis in immunocompetent patients [7]. In their study, beta lactam–aminoglycoside combination therapy was not associated with decreased mortality. On the other hand, Safdar and colleagues previously examined the impact of combination therapy on patients with gram-negative bacteremia and found a survival benefit associated with combination therapy in the subgroup of patients with P. aeruginosa bacteremia, demonstrating an approximately 50% reduction in mortality (OR: 0.50; 95% CI: 0.32-0.79) [8]. These differing results may have been due to the limitations of the earlier studies, including: (1) the combinations of different pathogens reported; (2) the greatly varying proportion of patients with pneumonia (range: 14%-100%); (3) the use of aminoglycoside as a monotherapy, which is not currently considered an appropriate therapy for P. aeruginosa infection; and (4) the possibility of P. aeruginosa colonization of the respiratory tract was not excluded. To overcome these limitations, we included a large number of consecutive patients with monomicrobial bacteremic Pseudomonas pneumonia in our study.
In our present analyses, adequate empirical therapy was associated with a significant reduction in mortality after 7 days. Analysis of the adequate empirical therapy group revealed that combination therapy was a variable independently associated with decreased 28-day mortality. One possible explanation for the decreased mortality could be a reduced frequency of emergence of antimicrobial resistance. However, there was no significant difference between the emergence of antimicrobial resistance in the monotherapy group (21.9% [7/32]) and the combination therapy group (12.1% [4/33], p = 0.29). Even in cases in where antimicrobial resistance emerged, only 3 patients (3 of 7) and 1 patient (1 of 4) died, respectively. Thus, the emergence of resistance may not affect the mortality rate. In contrast, the 2-week (18.8% vs. 54.5%, p = 0.04) and 4-week bacteria eradication rates (28.1% vs. 54.5%, p = 0.04) after bacteremia were significantly higher in the combination therapy group than in the monotherapy group. Because there was no significant difference in terms of the emergence of antimicrobial resistance between the monotherapy and combination therapy groups, these findings suggest that empirical combination therapy may contribute to the reduction in mortality by accelerating eradication. Hence, the manner in which combination therapy decreases mortality in patients with P. aeruginosa infection is an interesting question. Unfortunately, we did not perform a prospective study that could evaluate this and future analyses of this type will be required to do so.
The present study has some limitations. First, it was retrospective and performed at a single center, so there is the potential for bias that would limit the ability to draw a firm conclusion about the direct impact of antimicrobial therapy. However, it has been shown that elaborate statistical methods, such as the marginal structural model using IPTW, provide a better method of control for confounding influences by improving the adjustment of differences between treatment groups [20]. Furthermore, we tried to evaluate the possible factors that could affect the clinical outcomes of patients with pneumonia as much as possible. Second, our study included only patients with bacteremia, so our finding may not be directly applicable to Pseudomonas pneumonia without bacteremia.
Conclusions
In conclusion, our data strongly suggest that adequate empirical combination therapy can decrease mortality in patients with bacteremic Pseudomonas pneumonia. Additional prospective studies are therefore warranted.
References
Joo EJ, Kang CI, Ha YE, Park SY, Kang SJ, Wi YM, Lee NY, Chung DR, Peck KR, Song JH: Impact of inappropriate empiric antimicrobial therapy on outcome in Pseudomonas aeruginosa bacteraemia: a stratified analysis according to sites of infection. Infection. 2011, 39 (4): 309-318. 10.1007/s15010-011-0124-6.
Fujitani S, Sun HY, Yu VL, Weingarten JA: Pneumonia due to Pseudomonas aeruginosa: part I: epidemiology, clinical diagnosis, and source. Chest. 2011, 139 (4): 909-919. 10.1378/chest.10-0166.
National Nosocomial Infections Surveillance System: National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control. 2004, 32 (8): 470-485. 10.1016/j.ajic.2004.10.001.
Sun HY, Fujitani S, Quintiliani R, Yu VL: Pneumonia due to Pseudomonas aeruginosa: part II: antimicrobial resistance, pharmacodynamic concepts, and antibiotic therapy. Chest. 2011, 139 (5): 1172-1185. 10.1378/chest.10-0167.
El Solh AA, Alhajhusain A: Update on the treatment of Pseudomonas aeruginosa pneumonia. J Antimicrob Chemother. 2009, 64 (2): 229-238. 10.1093/jac/dkp201.
Anderson ET, Young LS, Hewitt WL: Antimicrobial synergism in the therapy of gram-negative rod bacteremia. Chemotherapy. 1978, 24 (1): 45-54. 10.1159/000237759.
Paul M, Benuri-Silbiger I, Soares-Weiser K, Leibovici L: Beta lactam monotherapy versus beta lactam-aminoglycoside combination therapy for sepsis in immunocompetent patients: systematic review and meta-analysis of randomized trials. BMJ. 2004, 328 (7441): 668-681. 10.1136/bmj.38028.520995.63.
Safdar N, Handelsman J, Maki DG: Does combination antimicrobial therapy reduce mortality in Gram-negative bacteraemia? A meta-analysis. Lancet Infect Dis. 2004, 4 (8): 519-527. 10.1016/S1473-3099(04)01108-9.
Traugott KA, Echevarria K, Maxwell P, Green K, Lewis JS: Monotherapy or combination therapy? The Pseudomonas aeruginosa conundrum. Pharmacotherapy. 2011, 31 (6): 598-608. 10.1592/phco.31.6.598.
Heyland DK, Dodek P, Muscedere J, Day A, Cook D, Canadian Critical Care Trials Group: Randomized trial of combination versus monotherapy for the empiric treatment of suspected ventilator-associated pneumonia. Crit Care Med. 2008, 36 (3): 737-744. 10.1097/01.CCM.0B013E31816203D6.
Chamot E, Boffi El Amari E, Rohner P, Van Delden C: Effectiveness of combination antimicrobial therapy for Pseudomonas aeruginosa bacteremia. Antimicrob Agents Chemother. 2003, 47 (9): 2756-2764. 10.1128/AAC.47.9.2756-2764.2003.
Carratalà J, Mykietiuk A, Fernández-Sabé N, Suárez C, Dorca J, Verdaguer R, Manresa F, Gudiol F: Health care-associated pneumonia requiring hospital admission: epidemiology, antibiotic therapy, and clinical outcomes. Arch Intern Med. 2007, 167 (13): 1393-1399. 10.1001/archinte.167.13.1393.
Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, Dowell SF, File TM, Musher DM, Niederman MS, Torres A, Whitney CG, Infectious Diseases Society of America; American Thoracic Society: Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007, 44: S27-S72. 10.1086/511159.
Kollef MH, Shorr A, Tabak YP, Gupta V, Liu LZ, Johannes RS: Epidemiology and outcomes of health-care-associated pneumonia: results from a large US database of culture-positive pneumonia. Chest. 2005, 128 (6): 3854-3862. 10.1378/chest.128.6.3854.
American Thoracic Society; Infectious Diseases Society of America: Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005, 171 (4): 388-416.
Garnacho-Montero J, Sa-Borges M, Sole-Violan J, Barcenilla F, Escoresca-Ortega A, Ochoa M, Cayuela A, Rello J: Optimal management therapy for Pseudomonas aeruginosa ventilator-associated pneumonia: an observational, multicenter study comparing monotherapy with combination antibiotic therapy. Crit Care Med. 2007, 35 (8): 1888-1895. 10.1097/01.CCM.0000275389.31974.22.
Clinical and Laboratory Standards Institute: Performance standards for antimicrobial testing: seventeenth informational supplement. CLSI document M100-S17. 2007, Clinical and Laboratory Standards Institute, Wayne, PA
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, Harbarth S, Hindler JF, Kahlmeter G, Olsson-Liljequist B, Paterson DL, Rice LB, Stelling J, Struelens MJ, Vatopoulos A, Weber JT, Monnet DL: Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012, 18 (3): 268-281. 10.1111/j.1469-0691.2011.03570.x.
Robins JM, Hernán MA, Brumback B: Marginal structural models and causal inference in epidemiology. Epidemiology. 2000, 11 (5): 550-560. 10.1097/00001648-200009000-00011.
Suarez D, Haro JM, Novick D, Ochoa S: Marginal structural models might overcome confounding when analyzing multiple treatment effects in observational studies. J Clin Epidemiol. 2008, 61 (6): 525-530. 10.1016/j.jclinepi.2007.11.007.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2334/12/308/prepub
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
Conceived and designed the study: SYP, SOL, SHC; Performed the study: SYP, HJP, SMM. Analyzed the data: SYP, KHP. YPC. Contributed reagents/materials/analysis tools: SYP, MNK, SHK, YSK, JHW. Wrote the paper: SYP, SHC. Critical review of the paper: All. All authors read and approved the final manuscript.
Electronic supplementary material
12879_2012_2078_MOESM1_ESM.doc
Additional file 1 : Table S1. Logistic regression analysis of the risk factors for 28-day mortality in all patients. (DOC 50 KB)
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Park, SY., Park, H.J., Moon, S.M. et al. Impact of adequate empirical combination therapy on mortality from bacteremic Pseudomonas aeruginosapneumonia. BMC Infect Dis 12, 308 (2012). https://doi.org/10.1186/1471-2334-12-308
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2334-12-308