Abstract
Purpose of Review
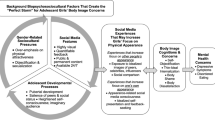
Obesity rates continue to rise among children and have shown persistent racial disparities. Racism plays a potentially essential and actionable role in these disparities. This report reviews some mechanisms through which racism may shape childhood obesity.
Recent Findings
From the youngest ages, disparities in childhood obesity prevalence are already present. Racism may shape intergenerational and prenatal factors that affect obesity and various stressors and environments where children grow up. The relationships between clinicians and patients may also be shaped by everyday racism and legacies of past racism, which may affect obesity prevalence and treatment efficacy.
Summary
Comprehensive data on the extent to which racism shapes childhood obesity is limited. However, compelling evidence suggests many ways through which racism ultimately does affect childhood obesity. Interventions to address racism at multiple points where it shapes childhood obesity, including intergenerational and prenatal mechanisms, may help to close disparities.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in us youth and adults by sex and age, 2007–2008 to 2015–2016. JAMA. 2018;319(16):1723–5. https://doi.org/10.1001/jama.2018.3060.
Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–14. https://doi.org/10.1001/jama.2014.732.
Ogden CL, Flegal KM. Obesity and socioeconomic status in adults: United States. 2010;2005–2008:50.
Claire Wang Y, Gortmaker SL, Taveras EM. Trends and racial/ethnic disparities in severe obesity among US children and adolescents, 1976–2006. Int J Pediatr Obes. 2011;6(1):12–20. https://doi.org/10.3109/17477161003587774.
Rossen LM, Schoendorf KC. Measuring health disparities: trends in racial−ethnic and socioeconomic disparities in obesity among 2- to 18-year old youth in the United States, 2001–2010. Ann Epidemiol. 2012;22(10):698–704. https://doi.org/10.1016/j.annepidem.2012.07.005.
Cunningham SA, Hardy ST, Jones R, Ng C, Kramer MR, Narayan KMV. Changes in the incidence of childhood obesity. Pediatrics. 2022;150(2):e2021053708. https://doi.org/10.1542/peds.2021-053708.
Anderson PM, Butcher KF, Schanzenbach DW. Understanding recent trends in childhood obesity in the United States. Econ Hum Biol. 2019;34:16–25. https://doi.org/10.1016/j.ehb.2019.02.002.
Isong IA, Rao SR, Bind MA, Avendaño M, Kawachi I, Richmond TK. Racial and ethnic disparities in early childhood obesity. Pediatrics. 2018;141(1):e20170865. https://doi.org/10.1542/peds.2017-0865.
Friedlander SL, Larkin EK, Rosen CL, Palermo TM, Redline S. Decreased quality of life associated with obesity in school-aged children. Arch Pediatr Adolesc Med. 2003;157(12):1206–11. https://doi.org/10.1001/archpedi.157.12.1206.
Rankin J, Matthews L, Cobley S, et al. Psychological consequences of childhood obesity: psychiatric comorbidity and prevention. Adolesc Health Med Ther. 2016;7:125–46. https://doi.org/10.2147/AHMT.S101631.
King JE, Jebeile H, Garnett SP, Baur LA, Paxton SJ, Gow ML. Physical activity based pediatric obesity treatment, depression, self-esteem and body image: a systematic review with meta-analysis. Ment Health Phys Act. 2020;19:100342. https://doi.org/10.1016/j.mhpa.2020.100342.
Sahoo K, Sahoo B, Choudhury AK, Sofi NY, Kumar R, Bhadoria AS. Childhood obesity: causes and consequences. J Family Med Prim Care. 2015;4(2):187–92. https://doi.org/10.4103/2249-4863.154628.
Cawley J. The economics of obesity. NBER. https://www.nber.org/reporter/2013number4/economics-obesity. Published December 2013. Accessed 27 Mar 2023.
Mocan NH, Tekin E. Obesity, self-esteem and wages. 2009. https://doi.org/10.3386/w15101.
Schwimmer JB, Burwinkle TM, Varni JW. Health-related quality of life of severely obese children and adolescents. JAMA. 2003;289(14):1813–9. https://doi.org/10.1001/jama.289.14.1813.
Maffeis C, Tatò L. Long-term effects of childhood obesity on morbidity and mortality. Horm Res. 2004;55(Suppl. 1):42–5. https://doi.org/10.1159/000063462.
Biro FM, Wien M. Childhood obesity and adult morbidities. Am J Clin Nutr. 2010;91(5):1499S–1505S. https://doi.org/10.3945/ajcn.2010.28701B.
Braveman PA, Arkin E, Proctor D, Kauh T, Holm N. Systemic and structural racism: definitions, examples, health damages, and approaches to dismantling. Health Aff. 2022;41(2):171–8. https://doi.org/10.1377/hlthaff.2021.01394.
Crimmins EM, Seeman TE. Integrating biology into the study of health disparities. Popul Dev Rev. 2004;30:89–107.
Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among Blacks and Whites in the United States. Am J Public Health. 2006;96(5):826–33. https://doi.org/10.2105/AJPH.2004.060749.
Forde AT, Crookes DM, Suglia SF, Demmer RT. The weathering hypothesis as an explanation for racial disparities in health: a systematic review. Ann Epidemiol. 2019;33:1-18.e3. https://doi.org/10.1016/j.annepidem.2019.02.011.
Alvidrez J, Castille D, Laude-Sharp M, Rosario A, Tabor D. The National Institute on Minority Health and Health Disparities Research Framework. Am J Public Health. 2019;109(S1):S16–20. https://doi.org/10.2105/AJPH.2018.304883.
McEWEN BS. Stress, adaptation, and disease: allostasis and allostatic load. Ann N Y Acad Sci. 1998;840(1):33–44. https://doi.org/10.1111/j.1749-6632.1998.tb09546.x.
McEWEN BS, Seeman T. Protective and Damaging effects of mediators of stress: elaborating and testing the concepts of allostasis and allostatic load. Ann NY Acad Sci. 1999;896(1):30–47. https://doi.org/10.1111/j.1749-6632.1999.tb08103.x.
Thomas MD, Michaels EK, Reeves AN, et al. Differential associations between everyday versus institution-specific racial discrimination, self-reported health, and allostatic load among black women: implications for clinical assessment and epidemiologic studies. Ann Epidemiol. 2019;35:20–28.e3. https://doi.org/10.1016/j.annepidem.2019.05.002.
Walsemann KM, Pearson J, Abbruzzi E. Education in the Jim Crow South and Black-White inequities in allostatic load among older adults. SSM Popul Health. 2022;19:101224. https://doi.org/10.1016/j.ssmph.2022.101224.
Miller HN, LaFave S, Marineau L, Stephens J, Thorpe RJ. The impact of discrimination on allostatic load in adults: an integrative review of literature. J Psychosom Res. 2021;146:110434. https://doi.org/10.1016/j.jpsychores.2021.110434.
Seeman TE, McEwen BS, Rowe JW, Singer BH. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc Natl Acad Sci. 2001;98(8):4770–5. https://doi.org/10.1073/pnas.081072698.
McEwen BS. Allostasis and allostatic load: implications for neuropsychopharmacology. Neuropsychopharmacology. 2000;22(2):108–24. https://doi.org/10.1016/S0893-133X(99)00129-3.
Geronimus AT, Hicken MT, Pearson JA, Seashols SJ, Brown KL, Cruz TD. Do US Black women experience stress-related accelerated biological aging? Hum Nat. 2010;21(1):19–38. https://doi.org/10.1007/s12110-010-9078-0.
Geronimus AT. Black/white differences in the relationship of maternal age to birthweight: a population-based test of the weathering hypothesis. Soc Sci Med. 1996;42(4):589–97. https://doi.org/10.1016/0277-9536(95)00159-X.
Doamekpor LA, Dinwiddie GY. Allostatic load in foreign-born and US-born Blacks: evidence from the 2001–2010 National Health and Nutrition Examination Survey. Am J Public Health. 2015;105(3):591–7. https://doi.org/10.2105/AJPH.2014.302285.
Cedillo YE, Murillo AL, Fernández JR. The association between allostatic load and anthropometric measurements among a multiethnic cohort of children. Pediatr Obes. 2019;14(6):e12501. https://doi.org/10.1111/ijpo.12501.
Cullin JM. Biological normalcy and body fat: obesity prevalence, fat stigma, and allostatic load among late adolescents and young adults. Am J Biol Anthropol. 2023 Aug;181(4):575–587. https://doi.org/10.1002/ajpa.24752. Epub 2023 Apr 25. PMID: 37096804.
Calcaterra V, Vinci F, Casari G, et al. Evaluation of allostatic load as a marker of chronic stress in children and the importance of excess weight. Front Pediatr. 2019 Aug 7;7:335. https://doi.org/10.3389/fped.2019.00335. PMID: 31440490; PMCID: PMC6693076.
Premji SS, Pana GS, Cuncannon A, Ronksley PE, Dosani A, Hayden KA, Lalani S, Musana JW, Shaikh K, Yim IS; Maternal-infant Global Health Team (MiGHT) Collaborators in Research. Prenatal allostatic load and preterm birth: a systematic review. Front Psychol. 2022 Oct 4;13:1004073. https://doi.org/10.3389/fpsyg.2022.1004073. PMID: 36267082; PMCID: PMC9577361.
Barry MC, Zimmer C, Halpern CT. Biomarkers of pre-pregnancy allostatic load and subsequent adverse birth outcomes. SSM Popul Health. 2022;18:101099. https://doi.org/10.1016/j.ssmph.2022.101099.
Morrison S, Shenassa ED, Mendola P, Wu T, Schoendorf K. Allostatic load may not be associated with chronic stress in pregnant women, NHANES 1999–2006. Ann Epidemiol. 2013;23(5):294–7. https://doi.org/10.1016/j.annepidem.2013.03.006.
Baicker K, Chandra A, Skinner JS, Wennberg JE. Who you are and where you live: how race and geography affect the treatment of Medicare beneficiaries. Health Aff. 2004;23(Suppl2):VAR-33. https://doi.org/10.1377/hlthaff.var.33
Minges KE, Chao A, Nam S, Grey M, Whittemore R. Weight Status, gender, and race/ethnicity: are there differences in meeting recommended health behavior guidelines for adolescents? J Sch Nurs. 2015;31(2):135–45. https://doi.org/10.1177/1059840514554089.
Styne DM, Arslanian SA, Connor EL, et al. Pediatric obesity—assessment, treatment, and prevention: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2017;102(3):709–57. https://doi.org/10.1210/jc.2016-2573.
Thornton RLJ, Hernandez RG, Cheng TL. Putting the US preventive services task force recommendation for childhood obesity screening in context. JAMA. 2017;317(23):2378–80. https://doi.org/10.1001/jama.2017.3434.
Rajjo T, Mohammed K, Alsawas M, et al. Treatment of pediatric obesity: an umbrella systematic review. J Clin Endocrinol Metab. 2017;102(3):763–75. https://doi.org/10.1210/jc.2016-2574.
• Epstein LH, Wilfley DE, Kilanowski C, et al. Family-based behavioral treatment for childhood obesity implemented in pediatric primary care: a randomized clinical trial. JAMA. 2023;329(22):1947–56. https://doi.org/10.1001/jama.2023.8061. This recent randomized trial sets a standard for practical interventions for childhood obesity - family centered and in primary care settings. It also finds lower efficacy among Black children enrolled.
Johnson VR, Acholonu NO, Dolan AC, Krishnan A, Wang EHC, Stanford FC. Racial disparities in obesity treatment among children and adolescents. Curr Obes Rep. 2021;10(3):342–50. https://doi.org/10.1007/s13679-021-00442-0.
Schell CJ, Dyson K, Fuentes TL, et al. The ecological and evolutionary consequences of systemic racism in urban environments. Science. 2020;369(6510):eaay4497. https://doi.org/10.1126/science.aay4497.
Satcher LA. Multiply-deserted areas: environmental racism and food, pharmacy, and greenspace access in the Urban South. Environ Sociol. 2022;8(3):279–91. https://doi.org/10.1080/23251042.2022.2031513.
Nardone A, Rudolph KE, Morello-Frosch R, Casey JA. Redlines and greenspace: the relationship between historical redlining and, 2010 greenspace across the United States. Environ Health Perspect. 129(1):017006. https://doi.org/10.1289/EHP7495.
Timmons BW, Naylor PJ, Pfeiffer KA. Physical activity for preschool children — how much and how? This article is part of a supplement entitled Advancing physical activity measurement and guidelines in Canada: a scientific review and evidence-based foundation for the future of Canadian physical activity guidelines co-published by Applied Physiology, Nutrition, and Metabolism and the Canadian Journal of Public Health. It may be cited as Appl. Physiol. Nutr. Metab. 32(Suppl. 2E) or as Can. J. Public Health 98(Suppl. 2). Appl Physiol Nutr Metab. 2007;32(S2E):S122–S134. https://doi.org/10.1139/H07-112.
• Frakes MD, Gruber J. Racial concordance and the quality of medical care: evidence from the military. 2022. https://doi.org/10.3386/w30767. This study leverages an innovative migration-based study design to causally identify returns to physician-patient racial concordance in chronic disease management.
Alsan M, Wanamaker M. Tuskegee and the health of Black men. Q J Econ. 2018;133(1):407–55. https://doi.org/10.1093/qje/qjx029.
Alsan M, Garrick O, Graziani G. Does diversity matter for health? experimental evidence from Oakland. Am Econ Rev. 2019;109(12):4071–111. https://doi.org/10.1257/aer.20181446.
Bajaj SS, Stanford FC. Beyond Tuskegee — vaccine distrust and everyday racism. N Engl J Med. 2021;384(5):e12. https://doi.org/10.1056/NEJMpv2035827.
Taveras EM, Marshall R, Sharifi M, et al. Comparative effectiveness of clinical-community childhood obesity interventions: a randomized clinical trial. JAMA Pediatr. 2017;171(8):e171325. https://doi.org/10.1001/jamapediatrics.2017.1325.
Armstrong SC, Bolling CF, Michalsky MP, et al. Pediatric metabolic and bariatric surgery: evidence, barriers, and best practices. Pediatrics. 2019;144(6):e20193223. https://doi.org/10.1542/peds.2019-3223.
Pratt JSA, Browne A, Browne NT, et al. ASMBS pediatric metabolic and bariatric surgery guidelines, 2018. Surg Obes Relat Dis. 2018;14(7):882–901. https://doi.org/10.1016/j.soard.2018.03.019.
Nunez Lopez O, Jupiter DC, Bohanon FJ, Radhakrishnan RS, Bowen-Jallow KA. Health disparities in adolescent bariatric surgery: nationwide outcomes and utilization. J Adolesc Health. 2017;61(5):649–56. https://doi.org/10.1016/j.jadohealth.2017.05.028.
Bouchard ME, Tian Y, Linton S, et al. Utilization trends and disparities in adolescent bariatric surgery in the United States 2009–2017. Child Obes. 2022;18(3):188–96. https://doi.org/10.1089/chi.2021.0201.
Steinberger AE, Youngwirth LM, Kim SE, et al. Adolescent bariatric surgery: racial disparities in 30-day outcomes using the MBSAQIP from 2015 to 2018. Obes Surg. 2021;31(8):3776–85. https://doi.org/10.1007/s11695-021-05500-z.
Wood MH, Carlin AM, Ghaferi AA, et al. Association of race with bariatric surgery outcomes. JAMA Surg. 2019;154(5):e190029. https://doi.org/10.1001/jamasurg.2019.0029.
• Weghuber D, Barrett T, Barrientos-Pérez M, et al. Once-weekly semaglutide in adolescents with obesity. N Engl J Med. 2022;387(24):2245–57. https://doi.org/10.1056/NEJMoa2208601. A recent randomized trial of pharamcologic therapy for childhood obesity shows high efficacy.
Eberly LA, Yang L, Essien UR, et al. Racial, ethnic, and socioeconomic inequities in glucagon-like peptide-1 receptor agonist use among patients with diabetes in the US. JAMA Health Forum. 2021;2(12):e214182. https://doi.org/10.1001/jamahealthforum.2021.4182.
Azad MB, Vehling L, Chan D, et al. Infant feeding and weight gain: separating breast milk from breastfeeding and formula from food. Pediatrics. 2018;142(4):e20181092. https://doi.org/10.1542/peds.2018-1092.
Brown A, Lee M. Breastfeeding during the first year promotes satiety responsiveness in children aged 18–24 months. Pediatr Obes. 2012;7(5):382–90. https://doi.org/10.1111/j.2047-6310.2012.00071.x.
Katzmarzyk PT, Barlow S, Bouchard C, et al. An evolving scientific basis for the prevention and treatment of pediatric obesity. Int J Obes. 2014;38(7):887–905. https://doi.org/10.1038/ijo.2014.49.
Beauregard JL, Hamner HC, Chen J, Avila-Rodriguez W, Elam-Evans LD, Perrine CG. Racial disparities in breastfeeding initiation and duration among U.S. infants born in 2015. MMWR Morb Mortal Wkly Rep. 2019;68(34):745–748. https://doi.org/10.15585/mmwr.mm6834a3.
Jones KM, Power ML, Queenan JT, Schulkin J. Racial and ethnic disparities in breastfeeding. Breastfeed Med. 2015;10(4):186–96. https://doi.org/10.1089/bfm.2014.0152.
Chiang KV, Li R, Anstey EH, Perrine CG. Racial and ethnic disparities in breastfeeding initiation ─ United States, 2019. MMWR Morb Mortal Wkly Rep. 2021;70(21):769–774. https://doi.org/10.15585/mmwr.mm7021a1.
Baker RS. Ethno-racial variation in single motherhood prevalences and penalties for child poverty in the United States, 1995–2018. Ann Am Acad Pol Soc Sci. 2022;702(1):20–36. https://doi.org/10.1177/00027162221120759.
Mclanahan S, Percheski C. Family structure and the reproduction of inequalities. Ann Rev Sociol. 2008;34:257–76.
Alghamdi S, Horodynski M, Stommel M. Racial and ethnic differences in breastfeeding, maternal knowledge, and self-efficacy among low-income mothers. Appl Nurs Res. 2017;37:24–7. https://doi.org/10.1016/j.apnr.2017.07.009.
•• Merewood A, Bugg K, Burnham L, Krane K, Nickel N, Broom S, Edwards R, Feldman-Winter L. Addressing racial inequities in breastfeeding in the southern United States. Pediatrics. 2019;143(2):e20181897. doi.org/10.1542/peds.2018-1897. This innovative study documents the rollout of comprehensive initiatives to increase the initiation of breastfeeding in a series of hospitals in the Southern US. While the results may have implications for obesity, it also provides large-scale evidence that typifies the type of comprehensive, community and hospital-based interventions that may address the manifestations of racism at multiple points.
Hemingway S, Forson-Dare Z, Ebeling M, Taylor SN. Racial Disparities in sustaining breastfeeding in a baby-friendly designated Southeastern United States hospital: an opportunity to investigate systemic racism. Breastfeed Med. 2021 Feb;16(2):150–155. https://doi.org/10.1089/bfm.2020.0306. Epub 2021 Feb 4. PMID: 33539272.
Wang YC, Bleich SN, Gortmaker SL. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among US children and adolescents, 1988–2004. Pediatrics. 2008;121(6):e1604–14. https://doi.org/10.1542/peds.2007-2834.
Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet. 2001;357(9255):505–8. https://doi.org/10.1016/S0140-6736(00)04041-1.
Bowman SA, Gortmaker SL, Ebbeling CB, Pereira MA, Ludwig DS. Effects of fast-food consumption on energy intake and diet quality among children in a national household survey. Pediatrics. 2004;113(1):112–8. https://doi.org/10.1542/peds.113.1.112.
Taveras EM, Gillman MW, Kleinman K, Rich-Edwards JW, Rifas-Shiman SL. Racial/ethnic differences in early-life risk factors for childhood obesity. Pediatrics. 2010;125(4):686–95. https://doi.org/10.1542/peds.2009-2100.
Darmon N, Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev. 2015;73(10):643–60. https://doi.org/10.1093/nutrit/nuv027.
Allcott H, Diamond R, Dubé JP, Handbury J, Rahkovsky I, Schnell M. Food deserts and the causes of nutritional inequality. Q J Econ. 2019;134(4):1793–844. https://doi.org/10.1093/qje/qjz015.
Alviola PA, Nayga RM, Thomsen MR, Danforth D, Smartt J. The effect of fast-food restaurants on childhood obesity: a school level analysis. Econ Hum Biol. 2014;12:110–9. https://doi.org/10.1016/j.ehb.2013.05.001.
Currie J, DellaVigna S, Moretti E, Pathania V. The effect of fast food restaurants on obesity and weight gain. Am Econ J Econ Pol. 2010;2(3):32–63. https://doi.org/10.1257/pol.2.3.32.
• Gertler P, Gracner T. The sweet life: the long-term effects of a sugar-rich early childhood. 2022. https://doi.org/10.3386/w30799. This study creatively uses changes in early life sugar availability due to rationing to examine the long-term effects on health, and the persistence of dietary preferences formed in childhood.
Taber DR, Chriqui JF, Powell L, Chaloupka FJ. Association between state laws governing school meal nutrition content and student weight status: implications for new USDA school meal standards. JAMA Pediatr. 2013;167(6):513–9. https://doi.org/10.1001/jamapediatrics.2013.399.
Smith TA, Mojduszka EM, Chen S. Did the new school meal standards improve the overall quality of children’s diets? Appl Econ Perspect Policy. 2021;43(4):1366–84. https://doi.org/10.1002/aepp.13074.
Haughton CF, Wang ML, Lemon SC. Racial/ethnic disparities in meeting 5-2-1-0 recommendations among children and adolescents in the United States. J Pediatr. 2016;175:188-194.e1. https://doi.org/10.1016/j.jpeds.2016.03.055.
Peña MM, Rifas-Shiman SL, Gillman MW, Redline S, Taveras EM. Racial/ethnic and socio-contextual correlates of chronic sleep curtailment in childhood. Sleep. 2016;39(9):1653–61. https://doi.org/10.5665/sleep.6086.
Franzini L, Taylor W, Elliott MN, et al. Neighborhood characteristics favorable to outdoor physical activity: disparities by socioeconomic and racial/ethnic composition. Health Place. 2010;16(2):267–74. https://doi.org/10.1016/j.healthplace.2009.10.009.
Carroll-Scott A, Gilstad-Hayden K, Rosenthal L, et al. Disentangling neighborhood contextual associations with child body mass index, diet, and physical activity: the role of built, socioeconomic, and social environments. Soc Sci Med. 2013;95:106–14. https://doi.org/10.1016/j.socscimed.2013.04.003.
Fuller-Rowell TE, Curtis DS, El-Sheikh M, Chae DH, Boylan JM, Ryff CD. Racial disparities in sleep: the role of neighborhood disadvantage. Sleep Med. 2016;27–28:1–8. https://doi.org/10.1016/j.sleep.2016.10.008.
Johnson DA, Billings ME, Hale L. Environmental determinants of insufficient sleep and sleep disorders: implications for population health. Curr Epidemiol Rep. 2018;5(2):61–9. https://doi.org/10.1007/s40471-018-0139-y.
Gillis BT, Shimizu M, Philbrook LE, El-Sheikh M. Racial disparities in adolescent sleep duration: physical activity as a protective factor. Cultur Divers Ethnic Minor Psychol. 2021;27(1):118–22. https://doi.org/10.1037/cdp0000422.
Hong YH, Lee JE. Large for gestational age and obesity-related comorbidities. J Obes Metab Syndr. 2021;30(2):124–31. https://doi.org/10.7570/jomes20130.
Yu ZB, Han SP, Zhu GZ, et al. Birth weight and subsequent risk of obesity: a systematic review and meta-analysis. Obes Rev. 2011;12(7):525–42. https://doi.org/10.1111/j.1467-789X.2011.00867.x.
Thompson JA, Suter MA. Estimating racial health disparities among adverse birth outcomes as deviations from the population rates. BMC Pregnancy Childbirth. 2020;20(1):1–7. https://doi.org/10.1186/s12884-020-2847-9.
Tyrrell J, Richmond RC, Palmer TM, et al. Genetic evidence for causal relationships between maternal obesity-related traits and birth weight. JAMA. 2016;315(11):1129–40. https://doi.org/10.1001/jama.2016.1975.
Oken E. Maternal and child obesity: the causal link. Obstet Gynecol Clinics. 2009;36(2):361–77. https://doi.org/10.1016/j.ogc.2009.03.007.
Buss C, Entringer S, Moog NK, et al. Intergenerational transmission of maternal childhood maltreatment exposure: implications for fetal brain development. J Am Acad Child Adolesc Psychiatry. 2017;56(5):373–82. https://doi.org/10.1016/j.jaac.2017.03.001.
Jones NL, Gilman SE, Cheng TL, Drury SS, Hill CV, Geronimus AT. Life course approaches to the causes of health disparities. Am J Public Health. 2019;109(S1):S48–55. https://doi.org/10.2105/AJPH.2018.304738.
Santavirta T, Santavirta N, Gilman SE. Association of the World War II Finnish evacuation of children with psychiatric hospitalization in the next generation. JAMA Psychiat. 2018;75(1):21–7. https://doi.org/10.1001/jamapsychiatry.2017.3511.
Funding
This study was supported by the National Institutes of Health NIDDK U24 DK132733, NIDDK UE5 DK137285 and P30 DK040561 (FCS).
Author information
Authors and Affiliations
Contributions
RIL and FCS both wrote the main manuscript text.
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Fatima Cody Stanford has served as a paid consultant/advisor for Novo Nordisk, Eli Lilly, Pfizer, Boheringer Ingelheim, Currax, Gelesis, Rhythm, Calibrate, Sweetch, Vida Health, and Ilant Health.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lawton, R.I., Stanford, F.C. The Role of Racism in Childhood Obesity. Curr Obes Rep 13, 98–106 (2024). https://doi.org/10.1007/s13679-023-00538-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13679-023-00538-9