Abstract
Purpose of Review
To describe what is known about the association between obesity and attention-deficit hyperactivity disorder (ADHD) in children along with the co-occurring conditions of sleep dysfunction, loss of control/binge eating disorder (LOC-ED/BED), and anxiety.
Recent Findings
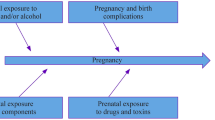
Obesity and ADHD share common brain pathways (hypothalamic, executive, and reward centers) with pathophysiology in these areas manifesting in partial or complete expression of these diseases. Sleep dysfunction, LOC-ED/BED, and anxiety share similar pathways and are associated with this disease dyad.
Summary
The association of obesity and ADHD with sleep dysfunction, LOC-ED/BED, and anxiety is discussed. An algorithm outlining decision pathways for patients with obesity and with and without ADHD is presented. Future research exploring the complex pathophysiology of both obesity and ADHD as well as co-occurring conditions is needed to develop clinical guidelines and ultimately assist in providing the best evidence-based care.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Sayal K, Prasad V, Daley D, Ford T, Coghill D. ADHD in children and young people: prevalence, care pathways, and service provision. Lancet Psychiatry. 2018;5:175–86. https://doi.org/10.1016/S2215-0366(17)30167-0.
Apovian CM. Obesity: definition, comorbidities, causes, and burden. Am J Manag Care. 2016;22(7 Suppl):s176–85.
Kim J, Lee GH, Sung SM, Jung DS, Pak K. Prevalence of attention deficit hyperactivity disorder symptoms in narcolepsy: a systematic review. Sleep Med. 2020;65:84–8. https://doi.org/10.1016/j.sleep.2019.07.022.
Kumar S, Kelly AS. Review of childhood obesity: from epidemiology, etiology, and comorbidities to clinical assessment and treatment. Mayo Clin Proc. 2017;92(2):251–65. https://doi.org/10.1016/j.mayocp.2016.09.017.
Ranum BM, Wichstrøm L, Pallesen S, Falch-Madsen J, Halse M, Steinsbekk S. Association between objectively measured sleep duration and symptoms of psychiatric disorders in middle childhood. JAMA Netw Open. 2019;2(12):e1918281. Published 2019 Dec 2. https://doi.org/10.1001/jamanetworkopen.2019.18281.
Sciberras E, Efron D, Patel P, Mulraney M, Lee KJ, Mihalopoulos C, et al. Does the treatment of anxiety in children with attention-deficit/hyperactivity disorder (ADHD) using cognitive behavioral therapy improve child and family outcomes? Protocol for a randomized controlled trial. BMC Psychiatry. 2019;19(1):359. https://doi.org/10.1186/s12888-019-2276-3.
Sharma V, Coleman S, Nixon J, Sharples L, Hamilton-Shield J, Rutter H, et al. A systematic review and meta-analysis estimating the population prevalence of comorbidities in children and adolescents aged 5 to 18 years. Obes Rev. 2019;20(10):1341–9. https://doi.org/10.1111/obr.12904.
Obesity. World Health Organization. https://www.who.int/health-topics/obesity#tab=tab_1 Updated 2020. Accessed Jun 30, 2020.
Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, et al. CDC growth charts: United States. Adv Data. 2000;314:1–27.
Gulati AK, Kaplan DW, Daniels SR. Clinical tracking of severely obese children: a new growth chart. Pediatrics. 2012;130(6):1136–40.
Kelly AS, Barlow SE, Rao G, Inge TH, Hayman LL, Steinberger J, et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 2013;128(15):1689–712. https://doi.org/10.1161/CIR.0b013e3182a5cfb3.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington: Author.
Visser SN, Zablotsky B, Holbrook JR, Danielson ML, Bitsko RH. Diagnostic experiences of children with attention-deficit/hyperactivity disorder. Natl Health Stat Rep. 2015;81:1–7.
Molina BSG, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, et al. The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study. J Am Acad Child Adolesc Psychiatry. 2009;48(5):484–500. https://doi.org/10.1097/CHI.0b013e31819c23d0.
Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015;56(3):345–65. https://doi.org/10.1111/jcpp.12381.
Thomas R, Sanders S, Doust J, Beller E, Glasziou P. Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics. 2015;135(4):e994–1001. https://doi.org/10.1542/peds.2014-3482.
Wolraich ML, McKeown RE, Visser SN, Bard D, Cuffe S, Neas B, et al. The prevalence of ADHD: its diagnosis and treatment in four school districts across two states. J Atten Disord. 2014;18(7):563–75. https://doi.org/10.1177/1087054712453169.
Rowland AS, Skipper BJ, Umbach DM, Rabiner DL, Campbell RA, Naftel AJ, et al. The prevalence of ADHD in a population-based sample. J Atten Disord. 2015;19(9):741–54. https://doi.org/10.1177/1087054713513799.
•• Cortese S. The association between ADHD and obesity: intriguing, progressively more investigated, but still puzzling. Brain Sci. 2019;9(10):256. https://doi.org/10.3390/brainsci9100256Most recent review of literature describing the association between obesity and ADHD.
Cortese S, Moreira-Maia CR, St Fleur D, Morcillo-Peñalver C, Rohde LA, Faraone SV. Association between ADHD and obesity: a systematic review and meta-analysis. Am J Psychiatry. 2016;173(1):34–43. https://doi.org/10.1176/appi.ajp.2015.15020266.
Nigg JT, Johnstone JM, Musser ED, Long HG, Willoughby MT, Shannon J. Attention-deficit/hyperactivity disorder (ADHD) and being overweight/obesity: New data and meta-analysis. Clin Psychol Rev. 2016;43:67–79. https://doi.org/10.1016/j.cpr.2015.11.005.
Khalife N, Kantomaa M, Glover V, Tammelin T, Laitinen J, Ebeling H, et al. Childhood attention-deficit/hyperactivity disorder symptoms are risk factors for obesity and physical inactivity in adolescence. J Am Acad Child Adolesc Psychiatry. 2014;53(4):425–36. https://doi.org/10.1016/j.jaac.2014.01.009.
Aguirre Castaneda RL, Kumar S, Voigt RG, Leibson CL, Barbaresi WJ, Weaver AL, et al. Childhood attention-deficit/hyperactivity disorder, sex, and obesity: a longitudinal population-based study. Mayo Clin Proc. 2016;3:61. https://doi.org/10.1016/j.mayocp.2015.09.017.
Bowling AB, Tiemeier HW, Jaddoe VWV, Barker ED, Jansen PW. ADHD symptoms and body composition changes in childhood: a longitudinal study evaluating directionality of associations. Pediatr Obes. 2018:567–75. https://doi.org/10.1111/ijpo.12288.
Seymour KE, Reinblatt SP, Benson L, Carnell S. Overlapping neurobehavioral circuits in ADHD, obesity, and binge eating: evidence from neuroimaging research. CNS Spectr. 2015;20(4):401–11. https://doi.org/10.1017/S1092852915000383.
Martins-Silva T, Vaz JDS, Hutz MH, Salatino-Oliveira A, Genro JP, Hartwig FP, et al. Assessing causality in the association between attention-deficit/hyperactivity disorder and obesity: a Mendelian randomization study. Int J Obes. 2019;43(12):2500–8. https://doi.org/10.1038/s41366-019-0346-8.
Cortese S, Angriman M, Comencini E, Vincenzi B, Maffeis C. Association between inflammatory cytokines and ADHD symptoms in children and adolescents with obesity: a pilot study. Psychiatry Res. 2019;278:7–11. https://doi.org/10.1016/j.psychres.2019.05.030.
Nousen EK, Franco JG, Sullivan EL. Unraveling the mechanisms responsible for the comorbidity between metabolic syndrome and mental health disorders. Neuroendocrinology. 2013;98(4):254–66. https://doi.org/10.1159/000355632.
•• Berthoud HR, Münzberg H, Morrison CD. Blaming the brain for obesity: integration of hedonic and homeostatic mechanisms. Gastroenterology. 2017;152(7):1728–38. https://doi.org/10.1053/j.gastro.2016.12.050New conceptual framework of human energy regulation addressing how hedonic controls interact with homeostatic controls to regulate body weight in a flexible and adaptive manner that takes environmental conditions into account.
Schwartz MW, Seeley RJ, Zeltser LM, Drewnowski A, Ravussin E, Redman LM, et al. Obesity pathogenesis: an endocrine society scientific statement. Endocr Rev. 2017;4:267–96. https://doi.org/10.1210/er.2017-00111.
Roh E, Kim MS. Brain regulation of energy metabolism. Endocrinol Metab (Seoul). 2016;31(4):519–24. https://doi.org/10.3803/EnM.2016.31.4.519.
Verbeken S, Braet C, Goossens L, van der Oord S. Executive function training with game elements for obese children: a novel treatment to enhance self-regulatory abilities for weight-control. Behav Res Ther. 2013;51(6):290–9. https://doi.org/10.1016/j.brat.2013.02.006.
Davis C, Levitan RD, Muglia P, Bewell C, Kennedy JL. Decision-making deficits and overeating: a risk model for obesity. Obes Res. 2004;12(6):929–35. https://doi.org/10.1038/oby.2004.113.
Yang Y, Shields GS, Guo C, Liu Y. Executive function performance in obesity and overweight individuals: a meta-analysis and review. Neurosci Biobehav Rev. 2018;84:225–44. https://doi.org/10.1016/j.neubiorev.2017.11.020.
Laurent JS, Watts R, Adise S, Allgaier N, Chaarani B, Garavan H, et al. Associations among body mass index, cortical thickness, and executive function in children. JAMA Pediatr. 2019;174(2):170–7. https://doi.org/10.1001/jamapediatrics.2019.4708.
Heinitz S, Reinhardt M, Piaggi P, Weise CM, Diaz E, Stinson EJ, et al. Neuromodulation directed at the prefrontal cortex of subjects with obesity reduces snack food intake and hunger in a randomized trial. Am J Clin Nutr. 2017;106(6):1347–57. https://doi.org/10.3945/ajcn.117.158089.
Münzberg H, Qualls-Creekmore E, Yu S, Morrison CD, Berthoud HR. Hedonics act in unison with the homeostatic system to unconsciously control body weight. Front Nutr. 2016;3:6. https://doi.org/10.3389/fnut.2016.00006.
Brooks SJ, Cedernaes J, Schiöth HB. Increased prefrontal and parahippocampal activation with reduced dorsolateral prefrontal and insular cortex activation to food images in obesity: a meta-analysis of fMRI studies. PLoS One. 2013;8(4):e60393. https://doi.org/10.1371/journal.pone.0060393.
Bruce AS, Holsen LM, Chambers RJ, Martin LE, Brooks WM, Zarcone JR, et al. Obese children show hyperactivation to food pictures in brain networks linked to motivation, reward and cognitive control. Int J Obes. 2010;34(10):1494–500. https://doi.org/10.1038/ijo.2010.84.
Stice E, Figlewicz DP, Gosnell BA, Levine AS, Pratt WE. The contribution of brain reward circuits to the obesity epidemic. Neurosci Biobehav Rev. 2013;37(9 Pt A):2047–58. https://doi.org/10.1016/j.neubiorev.2012.12.001.
Blum K, Thanos PK, Gold MS. Dopamine and glucose, obesity, and reward deficiency syndrome. Front Psychol. 2014;5:919. Published 2014 Sep 17. https://doi.org/10.3389/fpsyg.2014.00919.
Zhang Y, Liu J, Yao J, Ji G, Qian L, Wang J, et al. Obesity: pathophysiology and intervention. Nutrients. 2014;6(11):5153–83. https://doi.org/10.3390/nu6115153.
Timper K, Brüning JC. Hypothalamic circuits regulating appetite and energy homeostasis: pathways to obesity. Dis Model Mech. 2017;10(6):679–89. https://doi.org/10.1242/dmm.026609.
Cortese S. The neurobiology and genetics of attention-deficit/hyperactivity disorder (ADHD): what every clinician should know. Eur J Paediatr Neurol. 2012;16(5):422–33. https://doi.org/10.1016/j.ejpn.2012.01.009.
•• Koss KJ, Gunnar MR. Annual research review: early adversity, the hypothalamic-pituitary-adrenocortical axis, and child psychopathology. J Child Psychol Psychiatry. 2018;59(4):327–46. https://doi.org/10.1111/jcpp.12784Review of neurobiology of hypothalamic-pituitary-adrenocortical (HPA) axis and relationship between early adversity-HPA axis activity and HPA axis activity-psychopathology. Also, discusses the role of regulatory mechanisms and sensitive periods in development.
Koss KJ, Mliner SB, Donzella B, Gunnar MR. Early adversity, hypocortisolism, and behavior problems at school entry: a study of internationally adopted children. Psychoneuroendocrinology. 2016;66:31–8. https://doi.org/10.1016/j.psyneuen.2015.12.018.
Cherkasova MV, Hechtman L. Neuroimaging in attention-deficit hyperactivity disorder: beyond the frontostriatal circuitry. Can J Psychiatr. 2009;54(10):651–64. https://doi.org/10.1177/070674370905401002.
Giedd JN, Rapoport JL. Structural MRI of pediatric brain development: what have we learned and where are we going? Neuron. 2010;67(5):728–34. https://doi.org/10.1016/j.neuron.2010.08.040.
Shaw P, Lerch J, Greenstein D, Sharp W, Clasen L, Evans A, et al. Longitudinal mapping of cortical thickness and clinical outcome in children and adolescents with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2006;63(5):540–9. https://doi.org/10.1001/archpsyc.63.5.540.
Sowell ER, Thompson PM, Welcome SE, Henkenius AL, Toga AW, Peterson BS. Cortical abnormalities in children and adolescents with attention-deficit hyperactivity disorder. Lancet. 2003;362(9397):1699–707. https://doi.org/10.1016/S0140-6736(03)14842-8.
Shaw P, Gilliam M, Liverpool M, Weddle C, Malek M, Sharp W, et al. Cortical development in typically developing children with symptoms of hyperactivity and impulsivity: support for a dimensional view of attention deficit hyperactivity disorder. Am J Psychiatry. 2011;168(2):143–51. https://doi.org/10.1176/appi.ajp.2010.10030385.
Plessen KJ, Bansal R, Zhu H, Whiteman R, Amat J, Quackenbush GA, et al. Hippocampus and amygdala morphology in attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2006;63(7):795–807. https://doi.org/10.1001/archpsyc.63.7.795.
Ivanov I, Bansal R, Hao X, Zhu H, Kellendonk C, Miller L, et al. Morphological abnormalities of the thalamus in youths with attention deficit hyperactivity disorder. Am J Psychiatry. 2010;167(4):397–408. https://doi.org/10.1176/appi.ajp.2009.09030398.
Dickstein SG, Bannon K, Castellanos FX, Milham MP. The neural correlates of attention deficit hyperactivity disorder: an ALE meta-analysis. J Child Psychol Psychiatry. 2006;47(10):1051–62. https://doi.org/10.1111/j.1469-7610.2006.01671.x.
Shaw P, Eckstrand K, Sharp W, Blumenthal J, Lerch JP, Greenstein D, et al. Attention-deficit/hyperactivity disorder is characterized by a delay in cortical maturation. Proc Natl Acad Sci U S A. 2007;104(49):19649–54. https://doi.org/10.1073/pnas.0707741104.
Mackie S, Shaw P, Lenroot R, Pierson R, Greenstein DK, Nugent TF 3rd, et al. Cerebellar development and clinical outcome in attention deficit hyperactivity disorder. Am J Psychiatry. 2007;164(4):647–55. https://doi.org/10.1176/ajp.2007.164.4.647.
Clerkin SM, Schulz KP, Berwid OG, Fan J, Newcorn JH, Tang CY, et al. Thalamo-cortical activation and connectivity during response preparation in adults with persistent and remitted ADHD. Am J Psychiatry. 2013;170(9):1011–9. https://doi.org/10.1176/appi.ajp.2013.12070880.
Shaw P, Malek M, Watson B, Greenstein D, de Rossi P, Sharp W. Trajectories of cerebral cortical development in childhood and adolescence and adult attention-deficit/hyperactivity disorder. Biol Psychiatry. 2013;74(8):599–606. https://doi.org/10.1016/j.biopsych.2013.04.007.
Francx W, Oldehinkel M, Oosterlaan J, Heslenfeld D, Hartman CA, Hoekstra PJ, et al. The executive control network and symptomatic improvement in attention-deficit/hyperactivity disorder. Cortex. 2015;73:62–72. https://doi.org/10.1016/j.cortex.2015.08.012.
Halperin JM, Trampush JW, Miller CJ, Marks DJ, Newcorn JH. Neuropsychological outcome in adolescents/young adults with childhood ADHD: profiles of persisters, remitters and controls. J Child Psychol Psychiatry. 2008;49(9):958–66. https://doi.org/10.1111/j.1469-7610.2008.01926.x.
Rajendran K, Rindskopf D, O'Neill S, Marks DJ, Nomura Y, Halperin JM. Neuropsychological functioning and severity of ADHD in early childhood: a four-year cross-lagged study. J Abnorm Psychol. 2013;122(4):1179–88. https://doi.org/10.1037/a0034237.
Del Campo N, Chamberlain SR, Sahakian BJ, Robbins TW. The roles of dopamine and noradrenaline in the pathophysiology and treatment of attention-deficit/hyperactivity disorder. Biol Psychiatry. 2011;69(12):e145–57. https://doi.org/10.1016/j.biopsych.2011.02.036.
Prince J. Catecholamine dysfunction in attention-deficit/hyperactivity disorder: an update. J Clin Psychopharmacol. 2008;28(3 Suppl 2):S39–45. https://doi.org/10.1097/JCP.0b013e318174f92a.
Patte KA, Davis CA, Levitan RD, Kaplan AS, Carter-Major J, Kennedy JL. A behavioral genetic model of the mechanisms underlying the link between obesity and symptoms of ADHD. J Atten Disord. 2016;1087054715618793:1425–36. https://doi.org/10.1177/1087054715618793.
Lundahl A, Nelson TD. Attention deficit hyperactivity disorder symptomatology and pediatric obesity: psychopathology or sleep deprivation? J Health Psychol. 2016 Jun;21(6):1055–65. https://doi.org/10.1177/1359105314544991.
Hakim F, Kheirandish-Gozal L, Gozal D. Obesity and altered sleep: a pathway to metabolic derangements in children? Semin Pediatr Neurol. 2015;22(2):77–85. https://doi.org/10.1016/j.spen.2015.04.006.
• Fang CT, Chen VC, Ma HT, Chao HH, Ho MC, Gossop M. Attentional bias, "cool" and "hot" executive functions in obese patients: roles of body mass index, binge eating, and eating style. J Clin Psychopharmacol. 2019;39(2):145–52. https://doi.org/10.1097/JCP.0000000000001016Study examined "cool" (inhibitory control and mental flexibility) and "hot" (affective decision making) executive functions (EFs) in relation to body mass index, binge-eating tendency, and eating styles.
Lindberg L, Hagman E, Danielsson P, Marcus C, Persson M. Anxiety and depression in children and adolescents with obesity: a nationwide study in Sweden. BMC Med. 2020;18(1):30. https://doi.org/10.1186/s12916-020-1498-z.
Chihara Y, Akamizu T, Azuma M, Murase K, Harada Y, Tanizawa K, et al. Among metabolic factors, significance of fasting and postprandial increases in acyl and desacyl ghrelin and the acyl/desacyl ratio in obstructive sleep apnea before and after treatment. J Clin Sleep Med. 2015;11(8):895–905. https://doi.org/10.5664/jcsm.4942.
Gileles-Hillel A, Kheirandish-Gozal L, Gozal D. Biological plausibility linking sleep apnoea and metabolic dysfunction. Nat Rev Endocrinol. 2016;12(5):290–8. https://doi.org/10.1038/nrendo.2016.22.
Tankersley CG, O'Donnell C, Daood MJ, Watchko JF, Mitzner W, Schwartz A, et al. Leptin attenuates respiratory complications associated with the obese phenotype. J Appl Physiol (1985). 1998;85(6):2261–9. https://doi.org/10.1152/jappl.1998.85.6.2261.
Aygun AD, Gungor S, Ustundag B, Gurgoze MK, Sen Y. Proinflammatory cytokines and leptin are increased in serum of prepubertal obese children. Mediat Inflamm. 2005;2005(3):180–3. https://doi.org/10.1155/MI.2005.180.
Halbower AC, Mahone EM. Neuropsychological morbidity linked to childhood sleep-disordered breathing. Sleep Med Rev. 2006;10(2):97–107. https://doi.org/10.1016/j.smrv.2005.10.002.
Vgontzas AN, Bixler EO, Chrousos GP. Obesity-related sleepiness and fatigue: the role of the stress system and cytokines. Ann N Y Acad Sci. 2006;1083:329–44.
Turkoglu S, Cetin FH. The relationship between chronotype and obesity in children and adolescent with attention deficit hyperactivity disorder. Chronobiol Int. 2019;36:1138–47.
Matherne CE, Tanofsky-Kraff M, Altschul AM, Shank LM, Schvey NA, Brady SM, et al. A preliminary examination of loss of control eating disorder (LOC-ED) in middle childhood. Eat Behav. 2015;18:57–61. https://doi.org/10.1016/j.eatbeh.2015.04.001.
Kalarchian MA, Marcus MD. Psychiatric comorbidity of childhood obesity. Int Rev Psychiatry. 2012;24(3):241–6. https://doi.org/10.3109/09540261.2012.678818.
Furlong TM, Jayaweera HK, Balleine BW, Corbit LH. Binge-like consumption of a palatable food accelerates habitual control of behavior and is dependent on activation of the dorsolateral striatum. J Neurosci. 2014;14:5012–22. https://doi.org/10.1523/JNEUROSCI.3707-13.2014.
• Puhl RM, Himmelstein MS, Pearl RL. Weight stigma as a psychosocial contributor to obesity. Am Psychol. 2020;75(2):274–89. https://doi.org/10.1037/amp0000538Overview of recent evidence examining links between weight stigma and weight-related behaviors and health including health consequences and implications for treatment.
Dias-Ferreira E, Sousa JC, Melo I, Morgado P, Mesquita AR, Cerqueira JJ, et al. Chronic stress causes frontostriatal reorganization and affects decision-making. Science. 2009;325(5940):621–5. https://doi.org/10.1126/science.1171203.
•• Stern A, Agnew-Blais JC, Danese A, Fisher HL, Matthews T, Polanczyk GV, et al. Associations between ADHD and emotional problems from childhood to young adulthood: a longitudinal genetically sensitive study. J Child Psychol Psychiatry. 2020. https://doi.org/10.1111/jcpp.13217Review of developmental associations between ADHD and childhood emotional problems; examined the genetic and environmental contributions.
Overgaard KR, Aase H, Torgersen S, Zeiner P. Co-occurrence of ADHD and anxiety in preschool children. J Atten Disord. 2016;20(7):573–80. https://doi.org/10.1177/1087054712463063.
Jarrett MA, Wolff JC, Davis TE 3rd, Cowart MJ, Ollendick TH. Characteristics of children with ADHD and anxiety. J Atten Disord. 2016;20(7):636–44. https://doi.org/10.1177/1087054712452914.
Özcan Ö, Arslan M, Güngör S, Yüksel T, Selimoğlu MA. Plasma leptin, adiponectin, neuropeptide Y levels in drug naive children with ADHD. J Atten Disord. 2018;22(9):896–900. https://doi.org/10.1177/1087054715587095.
• Barker ED, Ing A, Biondo F, Jia T, Pingault JB, Du Rietz E, et al. Do ADHD-impulsivity and BMI have shared polygenic and neural correlates? Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0444-yExamined the neural and polygenic correlates between obesity and ADHD; found a common neural substrate that may account for shared genetic underpinnings of ADHD and obesity along with the manifestation of their (observable) phenotypic association.
Hanc T, Dmitrzak-Weglarz M, Borkowska A, Wolanczyk T, Pytlinska N, Rybakowski F, et al. Overweight in boys with ADHD is related to candidate genes and not to deficits in cognitive functions. J Atten Disord. 2018;22:1158–72.
Albayrak Ö, Pütter C, Volckmar AL, Cichon S, Hoffmann P, Nöthen MM, et al. Psychiatric GWAS Consortium: ADHD Subgroup. Common obesity risk alleles in childhood attention-deficit/hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet. 2013;162B(4):295–305. https://doi.org/10.1002/ajmg.b.32144.
Chervin RD, Dillon JE, Bassetti C, Ganoczy DA, Pituch KJ. Symptoms of sleep disorders, inattention, and hyperactivity in children. Sleep. 1997;20(12):1185–92. https://doi.org/10.1093/sleep/20.12.1185.
Guerdjikova AI, Blom TJ, Mori N, Matthews A, Cummings T, Casuto LL, et al. Lisdexamfetamine in pediatric binge eating disorder: a retrospective chart review. Clin Neuropharmacol. 2019;42(6):214–6. https://doi.org/10.1097/WNF.0000000000000367.
Fleck DE, Eliassen JC, Guerdjikova AI, Mori N, Williams S, Blom TJ, et al. Effect of lisdexamfetamine on emotional network brain dysfunction in binge eating disorder. Psychiatry Res Neuroimaging. 2019;286:53–9. https://doi.org/10.1016/j.pscychresns.2019.03.003.
Guerdjikova AI, Mori N, Casuto LS, McElroy SL. Novel pharmacologic treatment in acute binge eating disorder - role of lisdexamfetamine. Neuropsychiatr Dis Treat. 2016;12:833–41. https://doi.org/10.2147/NDT.S80881.
Srivastava G, O'Hara V, Browne N. Use of lisdexamfetamine to treat obesity in an adolescent with severe obesity and binge eating. Children (Basel). 2019;6(2):22. https://doi.org/10.3390/children6020022.
Sheinbein DH, Stein RI, Hayes JF, Brown ML, Balantekin KN, Conlon RPK, et al. Factors associated with depression and anxiety symptoms among children seeking treatment for obesity: A social-ecological approach. Pediatr Obes. 2019;14(8):e12518. https://doi.org/10.1111/ijpo.12518.
Eiraldi RB, Mautone JA, Power TJ. Strategies for implementing evidence-based psychosocial interventions for children with attention-deficit/hyperactivity disorder. Child Adolesc Psychiatr Clin N Am. 2012;21(1):145-x. https://doi.org/10.1016/j.chc.2011.08.012.
Wolraich ML, Hagan JF Jr, Allan C, et al. Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents [published correction appears in Pediatrics. 2020 Mar;145(3):]. Pediatrics. 2019;144(4):e20192528. https://doi.org/10.1542/peds.2019-2528.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Childhood Obesity
Rights and permissions
About this article
Cite this article
O’Hara, V.M., Curran, J.L. & Browne, N.T. The Co-occurrence of Pediatric Obesity and ADHD: an Understanding of Shared Pathophysiology and Implications for Collaborative Management. Curr Obes Rep 9, 451–461 (2020). https://doi.org/10.1007/s13679-020-00410-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13679-020-00410-0