Abstract
Background
Liraglutide, an analogue of glucagon-like peptide 1 (GLP-1), indicated for the treatment of type 2 diabetes mellitus (T2DM), has shown the effect on loss of weight and adipose deposits. The study was to evaluate the effect of liraglutide on epicardial adipose tissue (EAT) with echocardiography in patients with obese T2DM controlled on liraglutide monotherapy.
Methods
A single-arm follow-up research was performed in our study. Thirty-six subjects with obese T2DM were enrolled in the study, who were administered with liraglutide monotheraphy daily. The study period was 3 months. EAT thickness was measured with echocardiography both before and after treatment in each subject; meanwhile, anthropometrics and biochemicals (fasting blood glucose and hemoglobinA1c) were also conducted.
Results
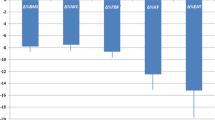
EAT thickness decreased significantly after three-month treatment, from 9.14 ± 2.39 to 6.42 ± 1.48 mm (p < 0.05). Anthropometrics including body weight, body mass index (BMI), waist circumference (WC), hip circumference (HC), and some biochemicals including fasting blood glucose (FBG), hemoglobinA1c (HbA1c), C-peptide, insulin, HOMA-IR, AST, ALT, and urinary albumin significantly improved (totally p< 0.05). Interestingly, the variation of EAT thickness had positive correlation with the variations of WC, HC, and BMI.
Conclusions
Liraglutide is beneficial to the decrease of EAT. EAT thickness can be measured with echocardiography to evaluate the effect of liraglutide in obese T2DM patients.




Similar content being viewed by others
References
Gao Y, Wang YC, Lu CQ, Zeng C, Chang D, Ju S. Correlations between the abdominal fat-related parameters and severity of coronary artery disease assessed by computed tomography. Quant Imaging Med Surg. 2018;8(6):579–87. https://doi.org/10.21037/qims.2018.07.06.
Iacobellis G, Bianco AC. Epicardial adipose tissue: emerging physiological, pathophysiological and clinical features. Trends Endocrinol Metab. 2011;22(11):450–7. https://doi.org/10.1016/j.tem.2011.07.003.
Song DK, Hong YS, Lee H, Oh JY, Sung YA, Kim Y. Increased epicardial adipose tissue thickness in type 2 diabetes mellitus and obesity. Diabetes Metab J. 2015;39(5):405–13. https://doi.org/10.4093/dmj.2015.39.5.405.
Patel VB, Shah S, Verma S, Oudit GY. Epicardial adipose tissue as a metabolic transducer: role in heart failure and coronary artery disease. Heart Fail Rev. 2017;22(6):889–902. https://doi.org/10.1007/s10741-017-9644-1.
Ansari MA, Mohebati M, Poursadegh F, Foroughian M, Shamloo AS. Is echocardiographic epicardial fat thickness increased in patients with coronary artery disease? A systematic review and meta-analysis. Electron Physician. 2018;10(9):7249–58. https://doi.org/10.19082/7249.
Pierdomenico SD, Pierdomenico AM, Cuccurullo F, Iacobellis G. Meta-analysis of the relation of echocardiographic epicardial adipose tissue thickness and the metabolic syndrome. Am J Cardiol. 2013;111(1):73–8. https://doi.org/10.1016/j.amjcard.2012.08.044.
Dagvasumberel M, Shimabukuro M, Nishiuchi T, Ueno J, Takao S, Fukuda D, et al. Gender disparities in the association between epicardial adipose tissue volume and coronary atherosclerosis: a 3-dimensional cardiac computed tomography imaging study in Japanese subjects. Cardiovasc Diabetol. 2012;11:106. https://doi.org/10.1186/1475-2840-11-106.
Bouchi R, Terashima M, Sasahara Y, Asakawa M, Fukuda T, Takeuchi T, et al. Luseogliflozin reduces epicardial fat accumulation in patients with type 2 diabetes: a pilot study. Cardiovasc Diabetol. 2017;16(1):32. https://doi.org/10.1186/s12933-017-0516-8.
Iacobellis G, Assael F, Ribaudo MC, Zappaterreno A, Alessi G, Di Mario U, et al. Epicardial fat from echocardiography: a new method for visceral adipose tissue prediction. Obes Res. 2003;11(2):304–10. https://doi.org/10.1038/oby.2003.45.
Lee YS, Lee C, Choung JS, Jung HS, Jun HS. Glucagon-like peptide 1 increases beta-cell regeneration by promoting alpha- to beta-cell transdifferentiation. 2018;67(12):2601–14. https://doi.org/10.2337/db18-0155.
Doyle ME, Egan JM. Mechanisms of action of glucagon-like peptide 1 in the pancreas. Pharmacol Ther. 2007;113(3):546–93. https://doi.org/10.1016/j.pharmthera.2006.11.007.
Lee YS, Jun HS. Anti-diabetic actions of glucagon-like peptide-1 on pancreatic beta-cells. Metabolism. 2014;63(1):9–19. https://doi.org/10.1016/j.metabol.2013.09.010.
Russell-Jones D, Vaag A, Schmitz O, Sethi BK, Lalic N, Antic S, et al. Liraglutide vs insulin glargine and placebo in combination with metformin and sulfonylurea therapy in type 2 diabetes mellitus (LEAD-5 met+SU): a randomised controlled trial. Diabetologia. 2009;52(10):2046–55. https://doi.org/10.1007/s00125-009-1472-y.
Rondanelli M, Perna S, Astrone P, Grugnetti A, Solerte SB, Guido D. Twenty-four-week effects of liraglutide on body composition, adherence to appetite, and lipid profile in overweight and obese patients with type 2 diabetes mellitus. Patient Prefer Adherence. 2016;10:407–13. https://doi.org/10.2147/ppa.s97383.
Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JF, Nauck MA, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375(4):311–22. https://doi.org/10.1056/NEJMoa1603827.
Morano S, Romagnoli E, Filardi T, Nieddu L, Mandosi E, Fallarino M, et al. Short-term effects of glucagon-like peptide 1 (GLP-1) receptor agonists on fat distribution in patients with type 2 diabetes mellitus: an ultrasonography study. Acta Diabetol. 2015;52(4):727–32. https://doi.org/10.1007/s00592-014-0710-z.
Iacobellis G, Mohseni M, Bianco SD, Banga PK. Liraglutide causes large and rapid epicardial fat reduction. Obesity (Silver Spring, Md). 2017;25(2):311–6. https://doi.org/10.1002/oby.21718.
Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–8. https://doi.org/10.1037//0033-2909.86.2.420.
Wang T, Zhang R, Ma X, Wang S, He Z, Huang Y, et al. Causal association of overall obesity and abdominal obesity with type 2 diabetes: a mendelian randomization. Analysis. 2018;26(5):934–42. https://doi.org/10.1002/oby.22167.
Alvehus M, Buren J, Sjostrom M, Goedecke J, Olsson T. The human visceral fat depot has a unique inflammatory profile. Obesity (Silver Spring, Md). 2010;18(5):879–83. https://doi.org/10.1038/oby.2010.22.
Lee MJ, Wu Y, Fried SK. Adipose tissue heterogeneity: implication of depot differences in adipose tissue for obesity complications. Mol Asp Med. 2013;34(1):1–11. https://doi.org/10.1016/j.mam.2012.10.001.
Ngo DT, Gokce N. Epicardial adipose tissue: a benign consequence of obesity? Circ Cardiovasc Imaging. 2015;8(3). https://doi.org/10.1161/circimaging.115.003156.
Lima-Martinez MM, Blandenier C, Iacobellis G. Epicardial adipose tissue: more than a simple fat deposit? Endocrinol Nutr. 2013;60(6):320–8. https://doi.org/10.1016/j.endonu.2012.08.001.
Iacobellis G. Local and systemic effects of the multifaceted epicardial adipose tissue depot. Nat Rev Endocrinol. 2015;11(6):363–71. https://doi.org/10.1038/nrendo.2015.58.
Mahabadi AA, Berg MH, Lehmann N, Kalsch H, Bauer M, Kara K, et al. Association of epicardial fat with cardiovascular risk factors and incident myocardial infarction in the general population: the Heinz Nixdorf Recall Study. J Am Coll Cardiol. 2013;61(13):1388–95. https://doi.org/10.1016/j.jacc.2012.11.062.
Matloch Z, Kotulak T, Haluzik M. The role of epicardial adipose tissue in heart disease. Physiol Res. 2016;65(1):23–32.
Drapkina OM, Zyatenkova EV. Evaluation of cardiovascular remodeling and epicardial fat thickness in patients with chronic heart failure and metabolic syndrome. Ter Arkh. 2016;88(2):64–70. https://doi.org/10.17116/terarkh201688264-70.
Kim BJ, Kim HS, Kang JG, Kim BS, Kang JH. Association of epicardial fat volume and nonalcoholic fatty liver disease with metabolic syndrome: from the CAESAR study. J Clin Lipidol. 2016;10(6):1423–30.e1. https://doi.org/10.1016/j.jacl.2016.09.007.
Hirata Y, Kurobe H, Akaike M, Chikugo F, Hori T, Bando Y, et al. Enhanced inflammation in epicardial fat in patients with coronary artery disease. Int Heart J. 2011;52(3):139–42.
Zhou Y, Wei Y, Wang L, Wang X, Du X, Sun Z, et al. Decreased adiponectin and increased inflammation expression in epicardial adipose tissue in coronary artery disease. Cardiovasc Diabetol. 2011;10:2. https://doi.org/10.1186/1475-2840-10-2.
Hayes MR, De Jonghe BC, Kanoski SE. Role of the glucagon-like-peptide-1 receptor in the control of energy balance. Physiol Behav. 2010;100(5):503–10. https://doi.org/10.1016/j.physbeh.2010.02.029.
Kanoski SE, Rupprecht LE, Fortin SM, De Jonghe BC, Hayes MR. The role of nausea in food intake and body weight suppression by peripheral GLP-1 receptor agonists, exendin-4 and liraglutide. Neuropharmacology. 2012;62(5–6):1916–27. https://doi.org/10.1016/j.neuropharm.2011.12.022.
Vendrell J, El Bekay R, Peral B, Garcia-Fuentes E, Megia A, Macias-Gonzalez M, et al. Study of the potential association of adipose tissue GLP-1 receptor with obesity and insulin resistance. Endocrinology. 2011;152(11):4072–9. https://doi.org/10.1210/en.2011-1070.
Beiroa D, Imbernon M, Gallego R, Senra A, Herranz D, Villarroya F, et al. GLP-1 agonism stimulates brown adipose tissue thermogenesis and browning through hypothalamic AMPK. Diabetes. 2014;63(10):3346–58. https://doi.org/10.2337/db14-0302.
Li CJ, Yu Q, Yu P, Yu TL, Zhang QM, Lu S, et al. Changes in liraglutide-induced body composition are related to modifications in plasma cardiac natriuretic peptides levels in obese type 2 diabetic patients. Cardiovasc Diabetol. 2014;13:36. https://doi.org/10.1186/1475-2840-13-36.
Kawasaki S, Aoki K, Hasegawa O, Numata K, Tanaka K, Shibata N, et al. Sonographic evaluation of visceral fat by measuring para- and perirenal fat. J Clin Ultrasound. 2008;36(3):129–33. https://doi.org/10.1002/jcu.20426.
Koda M, Senda M, Kamba M, Kimura K, Murawaki Y. Sonographic subcutaneous and visceral fat indices represent the distribution of body fat volume. Abdom Imaging. 2007;32(3):387–92. https://doi.org/10.1007/s00261-006-9082-3.
Acknowledgments
This work was supported by the Department of Ultrasound and Endocrinology of the Second Affiliated Hospital of Dalian Medical University, Dalian, China.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All the subjects submitted written informed consent after in detail understanding the study protocol and possible risks. The design proposal, methods of material collection, and data analysis were consistent with the declaration of Helsinki and were approved by the Ethics Committee of The Second Affiliated Hospital of Dalian Medical University (Dalian, China; Approval number, KY2015-128).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, Y., Liu, X., Li, G. et al. Effect of liraglutide on epicardial adipose tissue thickness with echocardiography in patients with obese type 2 diabetes mellitus. Int J Diabetes Dev Ctries 40, 500–506 (2020). https://doi.org/10.1007/s13410-020-00820-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-020-00820-9