Abstract
Purpose
Although doxorubicin is widely used to treat cancer, severe side effects limit its clinical use. Combination of standard chemotherapy with natural products can increase the efficacy and attenuate the side effects of current therapies. Here we studied the anticancer effects of a combined regimen comprising doxorubicin and [10]-gingerol against triple-negative breast cancer, which does not respond to hormonal or targeted therapies.
Methods
Cytotoxicity was evaluated by MTT assay, cell cycle progression and apoptosis were analyzed by flow cytometry and signaling pathways were analyzed by Western blotting in human and murine triple negative breast cancer cell systems. The anticancer/antimetastatic and toxic effects of the combined regimen was evaluated using syngeneic and xenograft orthotopic models.
Results
The combination of doxorubicin and [10]-gingerol significantly increased the number of apoptotic cells, compared to each compound alone. In 4T1Br4 cells, the combined regimen was the only condition able to increase the levels of active caspase 3 and γH2AX and to decrease the level of Cdk-6 cyclin. In vivo, doxorubicin (3 mg/Kg, D3) and [10]-gingerol (10 mg/Kg, G10) resulted in a significant reduction in the volume of primary tumors and a decrease in the number of circulating tumor cells (CTCs). Interestingly, only the combined regimen led to decreased tumor burdens to distant organs (i.e., metastasis) and reduced chemotherapy-induced weight loss and hepatotoxicity in tumor-bearing animals. Likewise, in a xenograft model, only the combined regimen was effective in significantly reducing the primary tumor volume and the prevalence of CTCs.
Conclusions
Our data indicate that [10]-gingerol has potential to be used as a neoadjuvant or in combined therapy with doxorubicin, to improve its anticancer activity.






Similar content being viewed by others
References
D.R. Welch, D.R. Hurst, Defining the hallmarks of metastasis. Cancer Res. 79, 3011-3027 (2019). https://doi.org/10.1158/0008-5472.CAN-19-0458
S.A. Eccles, D.R. Welch, Metastasis: recent discoveries and novel treatment strategies. Lancet 369, 1742–1757 (2007). https://doi.org/10.1016/S0140-6736(07)60781-8
C. Yam, S.A. Mani, S.L. Moulder, Targeting the molecular subtypes of triple negative breast cancer: Understanding the diversity to progress the field. Oncologist 22, 1086–1093 (2017). https://doi.org/10.1634/theoncologist.2017-0095
P. Samadi, S. Saki, F.K. Dermani, M. Pourjafar, M. Saidijam, Emerging ways to treat breast cancer: will promises be met? Cell. Oncol. 41, 605–621 (2018). https://doi.org/10.1007/s13402-018-0409-1
C. Neophytou, P. Boutsikos, P. Papageorgis, Molecular mechanisms and emerging therapeutic targets of triple-negative breast cancer metastasis. Front. Oncol. 8, 31 (2018). https://doi.org/10.3389/fonc.2018.00031
M. Yousefi, R. Nosrati, A. Salmaninejad, S. Dehghani, A. Shahryari, A. Saberi, Organ-specific metastasis of breast cancer: molecular and cellular mechanisms underlying lung metastasis. Cell. Oncol. 41, 123–140 (2018). https://doi.org/10.1007/s13402-018-0376-6
C.L. Shapiro, A. Recht, Side effects of adjuvant treatment of breast cancer. N. Engl. J. Med. 344, 1997–2008 (2001). https://doi.org/10.1056/NEJM200106283442607
A. Bosch, P. Eroles, R. Zaragoza, J.R. Vina, A. Lluch, Triple-negative breast cancer: molecular features, pathogenesis, treatment and current lines of research. Cancer Treat. Rev. 36, 206–215 (2010). https://doi.org/10.1016/j.ctrv.2009.12.002
C.F. Thorn, C. Oshiro, S. Marsh, T. Hernandez-Boussard, H. McLeod, T.E. Klein, R.B. Altman, Doxorubicin pathways: pharmacodynamics and adverse effects. Pharmacogenet. Genomics 21, 440–446 (2011). https://doi.org/10.1097/FPC.0b013e32833ffb56
S. Zhang, X. Liu, T. Bawa-Khalfe, L.S. Lu, Y.L. Lyu, L.F. Liu, E.T. Yeh, Identification of the molecular basis of doxorubicin-induced cardiotoxicity. Nat. Med. 18, 1639–1642 (2012). https://doi.org/10.1038/nm.2919
K.F. Hofland, A.V. Thougaard, M. Sehested, P.B. Jensen, Dexrazoxane protects against myelosuppression from the DNA cleavage-enhancing drugs etoposide and daunorubicin but not doxorubicin. Clin. Cancer Res. 11, 3915–3924 (2005). https://doi.org/10.1158/1078-0432.CCR-04-2343
L.A.A. Gilliam, K.H. Fisher-Wellman, C.T. Lin, J.M. Maples, B.L. Cathey, P.D. Neufer, The anticancer agent doxorubicin disrupts mitochondrial energy metabolism and redox balance in skeletal muscle. Free Radic. Biol. Med. 65, 988–996 (2013). https://doi.org/10.1016/j.freeradbiomed.2013.08.191
S.M. Swain, F.S. Whaley, M.S. Ewer, Congestive heart failure in patients treated with doxorubicin: a retrospective analysis of three trials. Cancer 97, 2869–2879 (2003). https://doi.org/10.1002/cncr.11407
J.A. Beutler, Natural products as a foundation for drug discovery. Curr. Protoc. Pharmacol. 86, e67 (2019). https://doi.org/10.1002/cpph.67
J.A. Beutler, Natural products as a foundation for drug discovery, Curr. Protoc. Pharmacol. 46, 9 11 11–19 11 21 (2009) https://doi.org/10.1002/0471141755.ph0911s46
G.M. Cragg, D.J. Newman, Medicinals for the millennia: the historical record. Ann. N. Y. Acad. Sci. 953, 3–25 (2001). https://doi.org/10.1111/j.1749-6632.2001.tb11356.x
G.M. Cragg, D.J. Newman, S.S. Yang, Bioprospecting for drugs. Nature 393, 301 (1998). https://doi.org/10.1038/30586
S. Mitra, R. Dash, Natural products for the management and prevention of breast cancer. Evid. Based Complement Alternat. Med. 2018, 8324696 (2018). https://doi.org/10.1155/2018/8324696
J. Poltronieri, A.B. Becceneri, A.M. Fuzer, J.C. Cesar, A.C.B.M. Martin, P.C. Vieira, N. Pouliot, M.R. Cominetti, [6]-gingerol as a cancer chemopreventive agent: A review of its activity on different steps of the metastatic process. Mini-Rev. Med. Chem. 14, 313–321 (2014). https://doi.org/10.2174/1389557514666140219095510
R.B. Semwal, D.K. Semwal, S. Combrinck, A.M. Viljoen, Gingerols and shogaols: Important nutraceutical principles from ginger. Phytochemistry 117, 554–568 (2015). https://doi.org/10.1016/j.phytochem.2015.07.012
A.M. Fuzer, S.Y. Lee, J.D. Mott, M.R. Cominetti, [10]-Gingerol reverts malignant phenotype of breast cancer cells in 3D culture. J. Cell. Biochem. 118, 2693–2699 (2017). https://doi.org/10.1002/jcb.25906
A. Martin, A.M. Fuzer, A.B. Becceneri, J.A. da Silva, R. Tomasin, D. Denoyer, S.H. Kim, K.A. McIntyre, H.B. Pearson, B. Yeo, A. Nagpal, X. Ling, H.S. Selistre-de-Araujo, P.C. Vieira, M.R. Cominetti, N. Pouliot, [10]-gingerol induces apoptosis and inhibits metastatic dissemination of triple negative breast cancer in vivo. Oncotarget 8, 72260–72271 (2017). https://doi.org/10.18632/oncotarget.20139
S.H. Kim, R.P. Redvers, L.H. Chi, X. Ling, A.J. Lucke, R.C. Reid, D.P. Fairlie, A. Martin, R.L. Anderson, D. Denoyer, N. Pouliot, Identification of brain metastasis genes and therapeutic evaluation of histone deacetylase inhibitors in a clinically relevant model of breast cancer brain metastasis, Dis. Model Mech. 11, (2018) https://doi.org/10.1242/dmm.034850
C.N. Johnstone, A.D. Pattison, K.L. Gorringe, P.F. Harrison, D.R. Powell, P. Lock, D. Baloyan, M. Ernst, A.G. Stewart, T.H. Beilharz, R.L. Anderson, Functional and genomic characterisation of a xenograft model system for the study of metastasis in triple-negative breast cancer, Dis. Model Mech. 11, (2018) https://doi.org/10.1242/dmm.032250
X.Z. Chang, D.Q. Li, Y.F. Hou, J. Wu, J.S. Lu, G.H. Di, W. Jin, Z.L. Ou, Z.Z. Shen, Z.M. Shao, Identification of the functional role of AF1Q in the progression of breast cancer. Breast Cancer Res. Treat. 111, 65–78 (2008). https://doi.org/10.1007/s10549-007-9761-y
J. Almada da Silva, A.B. Becceneri, H. Sanches Mutti, A.C. Moreno Martin, M.F. Fernandes da Silva, J.B. Fernandes, P.C. Vieira, M.R. Cominetti, Purification and differential biological effects of ginger-derived substances on normal and tumor cell lines. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 903, 157–162 (2012). https://doi.org/10.1016/j.jchromb.2012.07.013
T. Mosmann, Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J. Immunol. Methods 65, 55–63 (1983)
T.-C. Chou, P. Talalay, Analysis of combined drug effects: a new look at a very old problem. Trends Pharmacol. Sci. 4, 450–454 (1983)
T.C. Chou, P. Talalay, Quantitative analysis of dose-effect relationships: the combined effects of multiple drugs or enzyme inhibitors. Adv. Enzyme Regul. 22, 27–55 (1984). https://doi.org/10.1016/0065-2571(84)90007-4
B.L. Eckhardt, B.S. Parker, R.K. van Laar, C.M. Restall, A.L. Natoli, M.D. Tavaria, K.L. Stanley, E.K. Sloan, J.M. Moseley, R.L. Anderson, Genomic analysis of a spontaneous model of breast cancer metastasis to bone reveals a role for the extracellular matrix. Mol. Cancer Res. 3, 1–13 (2005)
J. Ozer, M. Ratner, M. Shaw, W. Bailey, S. Schomaker, The current state of serum biomarkers of hepatotoxicity. Toxicology 245, 194–205 (2008). https://doi.org/10.1016/j.tox.2007.11.021
V. Valero, E. Perez, V. Dieras, Doxorubicin and taxane combination regimens for metastatic breast cancer: focus on cardiac effects. Semin. Oncol. 28, 15–23 (2001)
D. Outomuro, D.R. Grana, F. Azzato, J. Milei, Adriamycin-induced myocardial toxicity: new solutions for an old problem? Int. J. Cardiol. 117, 6–15 (2007). https://doi.org/10.1016/j.ijcard.2006.05.005
G. Damodar, T. Smitha, S. Gopinath, S. Vijayakumar, Y. Rao, An evaluation of hepatotoxicity in breast cancer patients receiving injection Doxorubicin. Ann. Med. Health Sci. Res. 4, 74–79 (2014). https://doi.org/10.4103/2141-9248.126619
S.F. Llesuy, S.L. Arnaiz, Hepatotoxicity of mitoxantrone and doxorubicin. Toxicology 63, 187–198 (1990)
H.J. Broxterman, K.J. Gotink, H.M. Verheul, Understanding the causes of multidrug resistance in cancer: a comparison of doxorubicin and sunitinib. Drug Resist. Updat. 12, 114–126 (2009). https://doi.org/10.1016/j.drup.2009.07.001
R. Roskoski Jr., Cyclin-dependent protein serine/threonine kinase inhibitors as anticancer drugs. Pharmacol. Res. 139, 471–488 (2019). https://doi.org/10.1016/j.phrs.2018.11.035
F. Zhang, K. Thakur, F. Hu, J.G. Zhang, Z.J. Wei, 10-Gingerol, a phytochemical derivative from “Tongling white ginger”, inhibits cervical cancer: insights into the molecular mechanism and inhibitory targets. J. Agric. Food Chem. 65, 2089–2099 (2017). https://doi.org/10.1021/acs.jafc.7b00095
M.J. Ryu, H.S. Chung, [10]-Gingerol induces mitochondrial apoptosis through activation of MAPK pathway in HCT116 human colon cancer cells. In Vitro Cell. Dev. Biol. Anim. 51, 92–101 (2015). https://doi.org/10.1007/s11626-014-9806-6
O. Fernandez-Capetillo, A. Lee, M. Nussenzweig, A. Nussenzweig, H2AX: the histone guardian of the genome. DNA Repair 3, 959–967 (2004). https://doi.org/10.1016/j.dnarep.2004.03.024
I. Durak, H.S. Ozturk, M. Kavutcu, M. Birey, M. Yel, T. Guven, E. Olcay, M. Kacmaz, O. Canbolat, Protective role of antioxidant vitamins on adriamycin-induced free radical production and cardiotoxicity in guinea pigs. Cancer Res. Ther. Control 5, 133–141 (1998)
S. Kalender, Y. Kalender, A. Ates, M. Yel, E. Olcay, S. Candan, Protective role of antioxidant vitamin E and catechin on idarubicin-induced cardiotoxicity in rats. Braz. J. Med. Biol. Res. 35, 1379–1387 (2002). https://doi.org/10.1590/S0100-879×2002001100017
M.J. Tisdale, Cachexia in cancer patients. Nat. Rev. Cancer 2, 862–871 (2002). https://doi.org/10.1038/nrc927
K. Fearon, F. Strasser, S.D. Anker, I. Bosaeus, E. Bruera, R.L. Fainsinger, A. Jatoi, C. Loprinzi, N. MacDonald, G. Mantovani, M. Davis, M. Muscaritoli, F. Ottery, L. Radbruch, P. Ravasco, D. Walsh, A. Wilcock, S. Kaasa, V.E. Baracos, Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 12, 489–495 (2011). https://doi.org/10.1016/S1470-2045(10)70218-7
K. Wang, Y.T. Shan, L. Ma, K.Y. Yang, B.J. Hua, W. Yin, F.Z. Yin, Y. Chen, Natural product toosendanin reverses the resistance of human breast cancer cells to adriamycin as a novel PI3K inhibitor. Biochem. Pharmacol. 152, 153–164 (2018). https://doi.org/10.1016/j.bcp.2018.03.022
N. Kusuma, D. Denoyer, J.A. Eble, R.P. Redvers, B.S. Parker, R. Pelzer, R.L. Anderson, N. Pouliot, Integrin-dependent response to laminin-511 regulates breast tumor cell invasion and metastasis. Int. J. Cancer 130, 555–566 (2012). https://doi.org/10.1002/ijc.26018
K. Tao, M. Fang, J. Alroy, G.G. Sahagian, Imagable 4T1 model for the study of late stage breast cancer, BMC Cancer 30, (2008) Artn 228 1186/1471-2407-8-228
I. Daphu, T. Sundstrom, S. Horn, P.C. Huszthy, S.P. Niclou, P.O. Sakariassen, H. Immervoll, H. Miletic, R. Bjerkvig, F. Thorsen, vivo animal models for studying brain metastasis: value and limitations. Clin. Exp. Metastasis 30, 695–710 (2013). https://doi.org/10.1007/s10585-013-9566-9
N. Erin, S. Kale, G. Tanriover, S. Koksoy, O. Duymus, A.F. Korcum, Differential characteristics of heart, liver, and brain metastatic subsets of murine breast carcinoma. Breast Cancer Res. Treat. 139, 677–689 (2013). https://doi.org/10.1007/s10549-013-2584-0
D.V. Gopal, H.R. Rosen, Abnormal findings on liver function tests. Interpreting results to narrow the diagnosis and establish a prognosis. Postgrad. Med. 107, 100–102 (2000). https://doi.org/10.3810/pgm.2000.02.869
N.S. Rawson, J. Peto, An overview of prognostic factors in small cell lung cancer. A report from the Subcommittee for the Management of Lung Cancer of the United Kingdom Coordinating Committee on Cancer Research. Br. J. Cancer 61, 597–604 (1990). https://doi.org/10.1038/bjc.1990.133
X. Tan, K. Xiao, W. Liu, S. Chang, T. Zhang, H. Tang, Prognostic factors of distal cholangiocarcinoma after curative surgery: a series of 84 cases. Hepatogastroenterology 60, 1892–1895 (2013)
M. Tewes, M.W. Peis, S. Bogner, J.M. Theysohn, M.P. Reinboldt, M. Schuler, A. Welt, Hepatic arterial infusion chemotherapy for extensive liver metastases of breast cancer: efficacy, safety and prognostic parameters. J. Cancer Res. Clin. Oncol. 143, 2131–2141 (2017). https://doi.org/10.1007/s00432-017-2462-y
M.J. Proctor, D. Talwar, S.M. Balmar, D.S. O’Reilly, A.K. Foulis, P.G. Horgan, D.S. Morrison, D.C. McMillan, The relationship between the presence and site of cancer, an inflammation-based prognostic score and biochemical parameters. Initial results of the Glasgow Inflammation Outcome Study. Br. J. Cancer 103, 870–876 (2010). https://doi.org/10.1038/sj.bjc.6605855
S. Maheswaran, D.A. Haber, Ex vivo culture of CTCs: An emerging resource to guide cancer therapy. Cancer Res. 75, 2411–2415 (2015). https://doi.org/10.1158/0008-5472.CAN-15-0145
M. Puchalapalli, X. Zeng, L. Mu, A. Anderson, L. Hix Glickman, M. Zhang, M.R. Sayyad, S. Mosticone Wangensteen, C.V. Clevenger, J.E. Koblinski, NSG mice provide a better spontaneous model of breast cancer metastasis than athymic (nude) mice. PLoS One 11, e0163521 (2016). https://doi.org/10.1371/journal.pone.0163521
D.L. Waning, T.A. Guise, Molecular mechanisms of bone metastasis and associated muscle weakness. Clin. Cancer Res. 20, 3071–3077 (2014). https://doi.org/10.1158/1078-0432.CCR-13-1590
F. Ahmadabadi, M. Saghebjoo, C.J. Huang, I. Saffari, M. Zardast, The effects of high-intensity interval training and saffron aqueous extract supplementation on alterations of body weight and apoptotic indices in skeletal muscle of 4T1 breast cancer-bearing mice with cachexia. Appl. Physiol. Nutr. Metab. (2020). https://doi.org/10.1139/apnm-2019-0352
Acknowledgements
We would like to thank Dr. Normand Pouliot and Dr. Richard Redvers from ONJCRI, Melbourne, Australia for providing the 4T1Br4 and MDA-MB-231 HTML.6 cells lines used in this work. This work was supported by the Sao Paulo Research Foundation (FAPESP grant numbers 2015/24940-8 and 2013/00760-3), the National Council for Scientific and Technological Development (CNPq grant number 401506/2016-9) and the Coordinating Support for Higher Education (CAPES grant number 001). ACBMM has a post-doctoral fellowship from FAPESP (2016/23202-6), RT had a post-doctoral fellowship from CNPq (403568/2015-3) B. Annabi holds a research Chair in Cancer Prevention and Treatment at UQAM.
Author information
Authors and Affiliations
Contributions
ACBM Martin and R Tomasin: conception and design of the study, acquisition of data, analysis and interpretation of data, drafting the article and revising it critically for important intellectual content, final approval of the version to be submitted. L Luna-Dulcey, AE Graminha, MA Naves, RAG Teles, VD Silva, JA Silva, PC Vieira and B Annabi: analysis and interpretation of data, drafting the article and revising it critically for important intellectual content, final approval of the version to be submitted. MR Cominetti: funding acquisition, project administration, analysis and interpretation of data, drafting the article and revising it critically for important intellectual content, final approval of the version to be submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
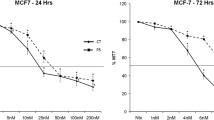
Supplementary Fig. 1
IC50 curves and values for doxorubicin and [10]-gingerol in different cell lines after 72 h of treatment. aPublished by Martin et al. (2017) [22]. (PNG 4550 kb)
Supplementary Fig. 2
Representative cell cycle plots of (A) 4T1Br4 and (B) MDA-MB-231 HMTL.6 cells of each indicated treatment. (PNG 3192 kb)
Supplementary Fig. 3
Representative dot plots from apoptosis assay in (A) 4T1Br and in (B) MDA-MB-231 HMTL.6 of each indicated treatment. Total apoptosis was evaluated from the sum of early and late apoptosis in (C) 4T1Br4 and (D) MDA-MB-231 HMTL.6 cell lines. Data are presented as mean±SEM. One-way ANOVA followed by Bonferroni’s post-test, *p<0.0001. (PNG 5237 kb)
Supplementary Fig. 4
Western blotting quantifications and representative membranes for Cdk-1, 2, 4 and 6, pro-caspase-3, active caspase-3 and γ-H2AX of each indicated treatment in (A) 4T1Br4. Representative membranes for endogenous control β-actin for (B) cell cycle proteins and (C) cell death and DNA damage. Western blotting quantifications and representative membranes for Cdk-1, 2, 4 and 6, pro-caspase-3, active caspase-3 and γ-H2AX in (D) MDA-MB-231 HMTL.6. Representative membranes for endogenous control β-actin for (E) cell cycle proteins and (F) cell death and DNA damage. The treatments in the western blotting membranes are in the following order: Lane 1: precision plus protein kaleidoscope (10–250 kDa), lane 2: Control, lane 3: G50, lane 4: D50, lane 5: G50D50, lane 6: G30D20, lane 7: G20D30. Data are presented as mean± SEM. One-way ANOVA followed by Dunnet’s post-test, ***p<0.0001, **p<0.001 and *p<0.01. (PNG 4011 kb)
Supplementary Fig. 5
Orthotopic syngeneic metastasis model (n = 15–16 in each group). (A) Spleen and (B) lung weight collected at the endpoint (28 days after IMFP injection) from syngeneic orthotopic experiments of each indicated treatment. Data are presented as mean±SEM. One-way ANOVA followed by Dunnett’s post-test, **p<0.0001. (PNG 1310 kb)
Supplementary Table 1
(DOCX 12 kb)
Rights and permissions
About this article
Cite this article
Baptista Moreno Martin, A.C., Tomasin, R., Luna-Dulcey, L. et al. [10]-Gingerol improves doxorubicin anticancer activity and decreases its side effects in triple negative breast cancer models. Cell Oncol. 43, 915–929 (2020). https://doi.org/10.1007/s13402-020-00539-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13402-020-00539-z