Abstract
Cancer chemotherapies have been improved dramatically over the last two decades. In the case of human breast cancer, the combination chemotherapeutic protocol, cyclophosphamide (CPA), doxorubicin (DOX), and 5-fluorouracil (5-FU) (CDF), is often used. Nevertheless, the clinical usefulness of CDF is limited by its remarkably low therapeutic window and frequent eruption of resistance. These limitations prompted our search for a more effective and safe drug candidate that may raise the therapeutic benefits for breast cancer patients. Gingerols’ wide therapeutic indices as well as their high efficacy in the suppression of carcinogenesis are well established. However, no thorough study to date has profiled their antibreast cancer activities in depth. Therefore, the aims of the present study are to evaluate the antibreast cancer activities of gingerols in comparison to CDF and to gain insight into the structure activity relationships (SARs) responsible for the observed effect using a breast cancer cell model, MCF-7. Our data revealed that 6-gingerol showed the highest anticancer potency that is superior to that of CDF with IC50 = 30.4 μM. Guided by these results, semisynthetic modifications of 6-gingerol have been carried out to characterize 6-gingerol’s SARs. The obtained results showed that the acquisition of free hydroxyl group in the aliphatic side chain of 6-gingerol is essential for the antibreast cancer activity. Likewise, the length of aliphatic side chain in 6-gingerol is optimum for its anticancer activity because any decrease in the side chain length resulted in a dramatic loss of anticancer activity. Additionally, allylation of phenolic group has shown antibreast cancer activity superior to that of 6-gingerol per se. Conversely, methylation or isoprenylation of phenolic group has led to a potential decrease in the anticancer activity, whereas loss of aromaticity resulted in a complete loss of 6-gingerol’s cytotoxic activity. Collectively, the present results would simplify drug design to allow safer and more effective antibreast cancer pharmaceuticals to be designed.
Similar content being viewed by others
Introduction
Forty-three years ago, the USA declared war on breast cancer with the passage of the National Cancer Act of 1971. Since that time, great progress has been made in fighting the disease, but we cannot yet declare victory. Although scientific discovery has given us new insights into breast cancer prevention, detection, and treatment, approximately 425,000 women around the world died from the disease in 2010. At this rate, 10.6 million women will die from breast cancer during the next 25 years [1, 2].
Current treatment modalities involve surgical cytoreduction or radiotherapy followed by chemotherapy treatment. The most common chemotherapeutic drugs used for breast cancer are doxorubicin (DOX) and the taxanes [3]. These may be used in combination with certain other drugs, like 5-fluorouracil (5-FU) and cyclophosphamide (CPA) [2]. Even though breast cancers respond to initial chemotherapy, more than half show drug resistance and recurrence [4, 5]. This frequent eruption of resistance to these agents poses a serious challenge to their efficacy in cancer management. Moreover, clinical usefulness of DOX is limited by its remarkably low therapeutic window. The latter profile triggers an endless series of myriad adverse reactions that can be life-threatening; including cardiotoxicity [6]. These limitations direct toward the finding of more effective and safe drugs, which may raise the therapeutic benefits for breast cancer patients.
Chemoprevention by plant-derived compounds has emerged as an accessible and promising approach to cancer control and management [7–9]. Of the many phytochemicals displaying a wide array of biochemical and pharmacologic activities, gingerols were recently reported to be effective in the suppression of transformation, hyperproliferation, and inflammatory processes that initiate and promote carcinogenesis, as well as the later steps of carcinogenesis, angiogenesis and metastasis [10, 11]. Despite these several lines of evidence supporting the activity of gingerol derivatives against multiple human cancers, no thorough study to date has profiled their antibreast cancer activity in depth. Therefore, the current study aims to evaluate the potential antibreast cancer activity of isolated gingerol derivatives, 6-gingerol, 4-gingerol, 4′-O-methyl-6-gingerol, and 1,2-dihydroxybisabola-3,10-diene, in comparison with standard regimen protocol, cyclophosphamide (CPA), doxorubicin (DOX), and 5-fluorouracil (5-FU) (CDF). Furthermore, this study pursues to delineate the relationships between structure elements of these gingerol derivatives and their antibreast cancer activities.
Materials and methods
Materials
Dulbecco’s modified Eagle’s medium (DMEM) was obtained from Gibco Laboratories (Life Technologies Inc., Grand Island, NY, USA). Nonessential amino acids (NEAA) and fetal calf serum (FCS) were purchased from Hyclone (Logan, UT, USA). Penicillin and streptomycin were purchased from Amresco (Solon, OH, USA). All gingerols were previously either isolated or semisynthesized in the Pharmacognosy Department, Faculty of Pharmacy, Mansoura University, Mansoura, Egypt, and identified by spesctroscopic means as ultraviolet (UV), infrared (IR), mass spectrometry (MS), and nuclear magnetic resonance (NMR). The purity of gingerols was assessed by different chromatographic and spectroscopic methods [12]. Plates of 96 wells were purchased from Corning Costar (Cambridge, MA, USA).
Cell culture
Human drug-resistant breast cancer cells, MCF-7 was purchased from American Type Culture Collection (ATCC; Rockville, MD, USA). MCF-7 cells were cultured in DMEM containing d-glucose (4.5 g/L), NaHCO3 (3.7 g/L), supplemented with 10 % FCS, penicillin (100 U/mL), and streptomycin (100 μg/mL) in an atmosphere of 5 % CO2 and 95 % relative humidity at 37 °C. Cells used in this study were between passages 50 and 62. The concentrations of the studied gingerols were in the range from 50 to 250 μM. They were dissolved in 100 % dimethylsulfoxide (DMSO; Sigma), and then diluted for the final concentration in serum-free media. In all experiments, control cells were incubated with DMSO alone. The final concentration of DMSO was maintained at 0.2 % (v/v). Cells were incubated with gingerols, CPA, DOX, 5-FU, or CDF for 24, 48, 72, and 96 h.
Cytotoxicity assay
Cytotoxicity was assessed by MTT assay according to the manufacturer’s recommendations (Roche Diagnostics GmbH, Mannheim, Germany). Experiments were repeated three times, and data represented as the mean ± standard deviation (SD). This assay relies on the ability of viable cells to reduce a yellow tetrazolium salt (MTT; Sigma) metabolically to a purple formazan product. This reaction takes place when mitochondrial reductase enzymes are active. Cells were grown in 96-well plates (1 × 104/200 μL/well). After incubation with the reagents, the medium was removed and the cells were treated with 20 μL of MTT (5 mg/mL) for 3 h at 37 °C. Subsequently, 100 μL of DMSO were added, and the solubilized formazan product was spectrophotometrically quantified with the help of a microplate reader, Power Wave XS (BioTek, Winooski, VT, USA), at 540 nm.
Statistical analysis
Data were presented as mean values ± SD. Statistical comparisons between groups were performed by one-way analysis of variance (ANOVA) followed by post hoc Tukey’s test. Value of p < 0.05 was assumed as statistically significant.
Results
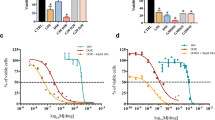
Among all tested compounds, 6-gingerol showed the highest anticancer activity as shown in Fig. 1a. Conversely, 4-gingerol, 4′-O-methyl-6-gingerol, and 1,2-dihydroxybisabola-3,10-diene, proved to be inactive even at concentrations of up to 100 μM (Fig. 1b–d, respectively).
Effect of side chain length, methylation of aromatic OH group, or loss of aromaticity on the cytotoxic activity of isolated gingerols: a IC50 of the most potent gingerol derivative, 6-gingerol. b IC50 of 4-gingerol, which is shorter in side chain length than 6-gingerol. c IC50 of 4′-O-methyl-6-gingerol that has a methylated aromatic OH group in 6-gingerol. d IC50 of 1,2-dihydroxybisabola-3,10-diene (without aromatic ring). These experiments have been done after 72 h incubation with different concentrations of isolated compounds (25, 100, and 200 μM), counted as percentage of untreated control, 0 μM. Data shown are the mean ± SD of three experiments. IC 50 50 % inhibitory concentration
Moving over the molecular structure of the isolated derivatives, it was observed that the length of aliphatic side chain in 6-gingerol is optimum for its antibreast cancer activity. Any decrease in the side chain length causes a total loss of anticancer activity as depicted in Fig. 1b for 4-gingerol (2-carbon less). Likewise, methylation of the phenolic group resulted in a substantial decrease in antibreast cancer activity as illustrated by 4′-O-methyl-6-gingerol, which did not show 50 % inhibition of cell viability after 72 h incubation at the used concentration range (Fig. 1c). Following this further, loss of aromaticity has a greater influence on the antibreast cancer activity of 6-gingerol. This is clearly manifested in 1,2-dihydroxybisabola-3,10-diene in which the cytotoxic activity has been dramatically diminished over the used concentration range (Fig. 1d).
After having shown that 6-gingerol demonstrated a high ability to elicit antitumor activity against MCF-7, we next sought to dissect the structural elements responsible for the observed effect. Therefore, semisynthetic modifications of the parent, 6-gingerol, have been carried out to characterize its structure–activity relationship (SAR). It has been shown that only 4′-O-allyl-6-gingerol derivative had a better antibreast cancer activity than that of 6-gingerol, whereas other derivatives exhibited a significant decrease or even a total loss of anticancer activity, indicating the importance of native functional groups in 6-gingerol for its antibreast cancer activity. By a deeper investigation, it was revealed that the prescence of free alcoholic group at position 5 in aliphatic side chain is the utmost important functional group required for 6-gingerol anticancer activity. This is evidently demonstrated in compound 5-O-methyl-6-gingerol where the blockage of the alcoholic group by methylation led to a significant decrease in 6-gingerol anticancer activity (Fig. 2a). Likewise, loss of the alcoholic group by dehydration as in compounds 6-shogaol as well as 4′-O-prenyl-6-shogaol resulted in a greater decrease in the 6-gingerol anticancer activity (Fig. 2b, c).
The importance of free alcoholic group at position 6 in aliphatic side chain in mediating 6-gingerol anticancer activity: a IC50 of 5-O-methyl-6-gingerol. b IC50 of 6-shogaol that has no alcoholic group in side chain. c IC50 of 4′-O-prenyl-6-shogaol. These experiments have been done after 72 h incubation with different concentrations of the tested compounds (25, 100, and 200 μM), counted as percentage of untreated control, 0 μM. Data shown are the mean ± SD of three experiments. IC 50 50 % inhibitory concentration
In addition to the free alcoholic group in 6-gingerol, the free phenolic group was found to be of great importance because its blockage has led to a significant modulation of 6-gingerol anticancer activity. While allylation of phenolic hydroxyl group in 6-gingerol was a successful structural modification with regard to its anticancer activity (Fig. 3a), the isoprenylation of the same position caused a dramatic decrease in 6-gingerol anticancer activity as in 4′-O-prenyl-6-gingerol (Fig. 3b). This is further supported by the observation that methylation of phenolic hydroxyl group in mono-5-O-methyl-6-gingerol to be dimethyl-6-gingerol decreased the anticancer activity significantly (Fig. 3c). However, the acetylation of 6-gingerol hydoxyl groups instead of methylation has increased its antibreast cancer activity 3.6-fold (Fig. 3d).
Modulation of 6-gingerol anticancer activity by esterfication of free phenolic group: a IC50 of 4′-O-allyl-6-gingerol. b IC50 of 4′-O-prenyl-6-gingerol. c IC50 of 5,4′-O-dimethyl-6-gingerol. d IC50 of 5,4′-O-diacetyl-6-gingerol. These experiments have been done after 72 h incubation with different concentrations of the tested compounds (25, 100, and 200 μM), counted as percentage of untreated control, 0 μM. Data shown are the mean ± SD of three experiments. IC 50 50 % inhibitory concentration
In the light of aforementioned 6-gingerol’s SAR, we next sought to determine whether the length of aliphatic side chain plays a prominent role in the regulation of 6-gingerol anticancer activity. As shown in Fig. 4a, the cleavage of aliphatic side has led to a complete loss of 6-gingerol activity, as depicted in compound methyl zingerone. On the contrary, dimerization of 6-gingerol was surprising, as it has promoted the carcinogenesis of MCF-7 in a dose-dependent manner (Fig. 4b). One-way ANOVA was used to test for statistical differences in antibreast cancer effect at IC50 for each compound after 72 h incubation period, and the means were significantly different across the samples (Fig. 5).
Aliphatic side chain plays a prominent role in the regulation of 6-gingerol anticancer activity: a IC50 of methyl zingerone. b IC50 of 6-gingerol dimer. These experiments have been done after 72 h incubation with different concentrations of the tested compounds (25, 100, and 200 μM), counted as percentage of untreated control, 0 μM. Data shown are the mean ± SD of three experiments. IC 50 50 % inhibitory concentration
Having such valuable SAR data on either 6-gingerols or its semisynthetic analouges in hand, facilitated an initiative work toward preclinical usefulness of gingerol derivatives by comparing their antibreast cancer activities to that of CDF regimen. Using this approach, dose–response and time-course cytotoxicity of this regimen were initially carried out by MTT assay. Individually, the dose response of DOX, 5-FU, or CPA at either 24 or 48 h did not reached the IC50 at any tested concentrations (25–250 μM). The dose response of DOX and 5-FU were more evident after 96 h (IC50; 44.69 and 65.7 μM, respectively) vs at 72 h (IC50 values of 120 and 158.5 μM, respectively) (Fig. 6a–d). However, only 20 % cell death was observed with CPA on Day 4, despite the high concentration used. Co-administration of the three drugs did not produce an effect on Day 1; however, 50 % of the cells had died on Days 2 through 3 (Fig. 7). Therefore, 72 h has been chosen as the optimal incubation period for the dose-viability response of all tested compounds, where 6-gingerol showed the highest anticancer potency that is superior to CDF, the classic reference cytotoxic regimen (Fig. 1a).
Viability of MCF-7 cells after single and combined administration of anticancer drugs: The viability of MCF-7 cells was examined for 4 days after treatment with CPA (200 μM; diamonds), DOX (50 μM; triangles), 5-FU (65 μM; squares), with all three drugs at the above concentrations (error mark). Cell viability is expressed as a mean percentage of untreated control ± SD of three independent experiments. *p value <0.05 for the difference in cell viability between the combined regimen and individual anticancer treatment at the same time point
Discussion
For many years, laboratories from all over the world have been working on finding effective therapies for breast cancer, a disease of the civilization. Despite the clinical success of several newly developed antibreast cancer drugs, some limitations remain, such as high peripheral neurotoxicity, complicated synthetic procedures, and drug resistance conferred by multidrug resistance transporters. Therefore, there has been a great interest in identifying novel antibreast cancer agents with new mode of actions and improved pharmacological profiles particularly with reduced toxicity. The renaissance of natural products as drug candidates was the theme of the recent research in cancer drug discovery and development and has been proved to be a reliable, effective, and safe approach [7, 13, 14]. In the current study, we put forward a new concept pertaining to the use of 6-gingerol and its derivative, allyl 6-gingerol, as potential antibreast cancer agents.
For years, much focus has been placed in the development and use of 6-gingerol, the major active ingredient from Zingiber officinale rhizomes, for the prevention and treatment of cancer [15]. 6-gingerol was found to potentiate the antiproliferation activity of various chemotherapeutic agents [11]. Furthermore, 6-gingerol was capable of inhibiting cellular proliferation and induction of apoptosis in human pancreatic duct cell-derived cancer [16], human hepatocarcinoma [17], human lung carcinoma [18], malignant glioma [19], cervical carcinoma [20], and prostate cancer cell lines [21]. All of this seemingly overwhelming evidence has sculpted the concept of 6-gingerol as potential anticancer agent. To extend the knowledge of the antineoplastic role of 6-gingerol, the current study opens up a new horizon in cancer fighting by shedding the light on the ability of 6-gingerol to induce breast cancer cell death more efficiently than the standard regimen, CDF. Additionally, allyl-6-gingerol, a semisynthetic derivative of 6-gingerol, has shown an antibreast cancer activity superior to that of CDF or 6-gingerol per se. Given these properties, 6-gingerol and its allyl derivative represent promising antibreast cancer agents. This input has originated partly from the study showing that 6-gingerol inhibited the metastasis of MDA-MB-231 human breast cancer cells [22]. In concordance, we observed potent anticancer activities of at least three gingerol-derived compounds against MCF-7. However, this study is the first to mention that although the basic chemical structures of gingerols are similar, the specific functional groups attached at a specific position, can impose remarkably different bioactivities to the resulting compounds. This phenomenon is exemplified here by reporting that allyl 6-gingerol, which is having an allyl group attached to the phenolic group, to be the most active compound to arrest the MCF-7 survival followed by 6-gingerol, diacetyl-6-gingerol, 4′-O-prenyl-6-gingerol, 5-O-methyl-6-gingerol, and finally, dimethyl-6-gingerol. Moreover, the current study portrayed the causal relationship between structure and the activity among these gingerols showing that the acquisition of free hydroxyl group in the aliphatic side chain of gingerol molecule significantly enhanced the anticancer activity. Likewise, the length of aliphatic side chain in 6-gingerol is optimum for the anticancer activity because any decrease in the side chain length resulted in a dramatic loss of anticancer activity. In addition, methylation or isoprenylation of phenolic group, led to a potential decrease in the anticancer activity. Furthermore, loss of aromaticity, resulted in a complete loss of the cytotoxic activity.
Several mechanisms have been proposed regarding gingerols’ anticancer activities. One such mechanism refers to their antioxidant activities, as most of gingerols exhibit antioxidant activities [23], and recent analyses have held that evidence favors an efficacious role for cancer prevention by antioxidants [24, 25]. However, the antioxidative potential of gingerols does not rule out their beneficial effects through nonantioxidative properties. For the “proof of principle,” 6-gingerol in this study displayed an effective antibreast cancer activity without being the most potent antioxidant in ginger constituents [23]. These findings together with the observation that dimerization of 6-gingerol promoted the carcinogenesis of MCF-7, have strengthened the notion that multiple mechanisms appear to be involved in 6-gingerol action beyond its antioxidant properties. These mechanisms have been suggested to be related to Ca2+ and protein kinase C (PKC)-α involved interaction of ER and mitochondria stresses, protein degradation, beta-catenin, and GSK-3beta pathways [26–28]. These effects are demonstrably “nonantioxidative,” which need further investigation to find out which is down to 6-gingerol’s antibreast cancer activity.
An important and as yet unmet goal in the treatment of breast cancer is to develop an effective antitumor agent with minimized metabolic adverse effect that characterizes the existing medications. Considering the risk of emesis that is associated with breast cancer therapy, 6-gingerol has shown beneficial effect in reducing nausea and vomiting due to the inhibition of cholinergic M3 receptors and serotonergic 5-HT3 receptors [29]. These multiple effects of 6-gingerol envision its future clinical amalgamation with existing and promising treatments. Nevertheless, few side effects may have been associated with 6-gingerol, such as decreased melanogenesis [19] as well as its hypotensive and cardio-suppressant effects [30]. These raise theoretical concerns that cases with cardiovascular diseases or those taking skin whitening drugs may consider using gingerol derivatives cautiously.
In conclusion, with the continuing need for novel drug-like leading compounds against the breast cancer, the remarkable anticancer activity of the studied gingerol derivatives compared with the standard therapeutic regimen makes them potential leads for future antibreast cancer agents.
References
Forouzanfar MH, Foreman KJ, Delossantos AM, Lozano R, Lopez AD, Murray CJ, et al. Breast and cervical cancer in 187 countries between 1980 and 2010: a systematic analysis. Lancet. 2011;378(9801):1461–84.
American Cancer Society. Cancer Facts and Figures. Atlanta, GA. 2013
Henderson IC, Berry DA, Demetri GD, Cirrincione CT, Goldstein LJ, Martino S, et al. Improved outcomes from adding sequential Paclitaxel but not from escalating Doxorubicin dose in an adjuvant chemotherapy regimen for patients with node-positive primary breast cancer. J Clin Oncol. 2003;21(6):976–83.
Gonzalez-Angulo AM, Morales-Vasquez F, Hortobagyi GN. Overview of resistance to systemic therapy in patients with breast cancer. Adv Exp Med Biol. 2007;608:1–622.
Guarneri V, Conte PF. The curability of breast cancer and the treatment of advanced disease. Eur J Nucl Med Mol Imaging. 2004;31 Suppl 1:S149–61.
Shaikh AY, Shih JA. Chemotherapy-induced cardiotoxicity. Curr Heart Fail Rep. 2012;9(2):117–27.
Badria FA, Ibrahim AS. Evaluation of natural anthracene-derived compounds as antimitotic agents. Drug Discov Ther. 2013;7(2):84–9.
Ibrahim A, Sobeh M, Ismail A, Alaa A, Sheashaa H, Sobh M, et al. Free B-Ring flavonoids as potential lead compounds for colon cancer therapy. Molecular and Clinical Oncology 2014
Alarif WM, Abdel-Lateff A, Al-Abd AM, Basaif SA, Badria FA, Shams M, et al. Selective cytotoxic effects on human breast carcinoma of new methoxylated flavonoids from Euryops arabicus grown in Saudi Arabia. Eur J Med Chem. 2013;66:204–10.
Bode AM, Dong Z. The Amazing and Mighty Ginger. 2012.
Angelini A, Conti P, Ciofani G, Cuccurullo F, Di Ilio C. Modulation of multidrug resistance p-glycoprotein activity by antiemetic compounds in human doxorubicin-resistant sarcoma cells (MES-SA/Dx-5): implications on cancer therapy. J Biol Regul Homeost Agents. 2013;27(4):1029–37.
El-Naggar MH, Abdel-Bar FM, Amer MM, Badria FA. Isolation, derivatization, and biological evaluation of gingerol derivativaes. M.Sc. thesis [Master], Mansoura; 2014
El-Bakly WM, Louka ML, El-Halawany AM, Schaalan MF. 6-gingerol ameliorated doxorubicin-induced cardiotoxicity: role of nuclear factor kappa B and protein glycation. Cancer Chemother Pharmacol. 2012;70(6):833–41.
Koehn FE. Natural products and cancer drug discovery. New York: Humana Press; 2013.
5Khuda-Bukhsh AR, Das S, Saha SK. Molecular approaches toward targeted cancer prevention with some food plants and their products: inflammatory and other signal pathways. Nutr Cancer 2014
Kim SO, Kim MR. [6]-Gingerol prevents disassembly of cell junctions and activities of MMPs in invasive human pancreas cancer cells through ERK/NF-kappa B/Snail signal transduction pathway. Evid Based Complement Alternat Med 2013; 2013:761852
Weng CJ, Chou CP, Ho CT, Yen GC. Molecular mechanism inhibiting human hepatocarcinoma cell invasion by 6-shogaol and 6-gingerol. Mol Nutr Food Res. 2012;56(8):1304–14.
Tuntiwechapikul W, Taka T, Songsomboon C, Kaewtunjai N, Imsumran A, Makonkawkeyoon L, et al. Ginger extract inhibits human telomerase reverse transcriptase and c-Myc expression in A549 lung cancer cells. J Med Food. 2010;13(6):1347–54.
Huang HC, Chiu SH, Chang TM. Inhibitory effect of [6]-gingerol on melanogenesis in B16F10 melanoma cells and a possible mechanism of action. Biosci Biotechnol Biochem. 2011;75(6):1067–72.
Chakraborty D, Bishayee K, Ghosh S, Biswas R, Mandal SK, Khuda-Bukhsh AR. [6]-Gingerol induces caspase 3 dependent apoptosis and autophagy in cancer cells: drug-DNA interaction and expression of certain signal genes in HeLa cells. Eur J Pharmacol. 2012;694(1–3):20–9.
Brahmbhatt M, Gundala SR, Asif G, Shamsi SA, Aneja R. Ginger phytochemicals exhibit synergy to inhibit prostate cancer cell proliferation. Nutr Cancer. 2013;65(2):263–72.
Lee HS, Seo EY, Kang NE, Kim WK. [6]-Gingerol inhibits metastasis of MDA-MB-231 human breast cancer cells. J Nutr Biochem. 2008;19(5):313–9.
Dugasani S, Pichika MR, Nadarajah VD, Balijepalli MK, Tandra S, Korlakunta JN. Comparative antioxidant and anti-inflammatory effects of [6]-gingerol, [8]-gingerol, [10]-gingerol and [6]-shogaol. J Ethnopharmacol. 2010;127(2):515–20.
Harris HR, Orsini N, Wolk A. Vitamin C and survival among women with breast cancer: a meta-analysis. Eur J Cancer. 2014;50(7):1223–31.
Crawford S. Anti-inflammatory/antioxidant use in long-term maintenance cancer therapy: a new therapeutic approach to disease progression and recurrence. Ther Adv Med Oncol. 2014;6(2):52–68.
Lee SH, Cekanova M, Baek SJ. Multiple mechanisms are involved in 6-gingerol-induced cell growth arrest and apoptosis in human colorectal cancer cells. Mol Carcinog. 2008;47(3):197–208.
Watanabe M, Shigekawa M. [Physiological functions of endoplasmic and sarcoplasmic reticulum Ca pump and pharmacology of inhibitors of the pump]. Nihon Yakurigaku Zasshi. 1993;102(3):171–80.
Chen CY, Chen CH, Kung CH, Kuo SH, Kuo SY. [6]-gingerol induces Ca2+ mobilization in Madin-Darby canine kidney cells. J Nat Prod. 2008;71(1):137–40.
Pertz HH, Lehmann J, Roth-Ehrang R, Elz S. Effects of ginger constituents on the gastrointestinal tract: role of cholinergic M3 and serotonergic 5-HT3 and 5-HT4 receptors. Planta Med. 2011;77(10):973–8.
Ghayur MN, Gilani AH, Afridi MB, Houghton PJ. Cardiovascular effects of ginger aqueous extract and its phenolic constituents are mediated through multiple pathways. Vasc Pharmacol. 2005;43(4):234–41.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Ibrahim, A.S., Sobh, M.A.M., Eid, H.M. et al. Gingerol-derivatives: emerging new therapy against human drug-resistant MCF-7. Tumor Biol. 35, 9941–9948 (2014). https://doi.org/10.1007/s13277-014-2248-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-014-2248-7