Abstract
Background and Objective
Unbound daptomycin concentrations are responsible for pharmacologically beneficial and adverse effects, although most previous reports have been limited to the use of total concentrations. We developed a population pharmacokinetic model to predict both total and unbound daptomycin concentrations.
Methods
Clinical data were collected from 58 patients with methicillin-resistant Staphylococcus aureus including patients undergoing hemodialysis. A total of 339 serum total and 329 unbound daptomycin concentrations were used for model construction.
Results
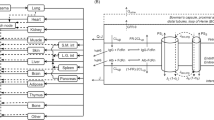
Total and unbound daptomycin concentration was explained by a model that assumed first-order distribution with two compartments, and first-order elimination. Normal fat body mass was identified as covariates. Renal function was incorporated as a linear function of renal clearance and independent non-renal clearance. The unbound fraction was estimated to be 0.066 with a standard albumin of 45 g/L and standard creatinine clearance of 100 mL/min. Simulated unbound daptomycin concentration was compared with minimum inhibitory concentration as a measure of clinical effectiveness and exposure-level-related induction of creatine phosphokinase elevation. The recommended doses were 4 mg/kg for patients with severe renal function [creatinine clearance (CLcr) ≤ 30 mL/min] and 6 mg/kg for patients with mild to moderate renal function (CLcr > 30 and ≤ 60 mL/min). A simulation indicated that dose adjusted by body weight and renal function improved target attainment.
Conclusions
This population pharmacokinetics model for unbound daptomycin could help clinicians to select the appropriate dose regimen for patients undergoing daptomycin treatment and reduce associated adverse effects.


Similar content being viewed by others
References
Tally FP, DeBruin MF. Development of daptomycin for Gram-positive infections. J Antimicrob Chemother. 2000;46:523–6. https://doi.org/10.1093/jac/46.4.523.
Gregoire N, Chauzy A, Buyck J, Rammaert B, Couet W, Marchand S. Clinical pharmacokinetics of daptomycin. Clin Pharmacokinet. 2021;60:271–81. https://doi.org/10.1007/s40262-020-00968-x.
Seaton RA, Menichetti F, Dalekos G, Beiras-Fernandez A, Nacinovich F, Pathan R, et al. Evaluation of effectiveness and safety of high-dose daptomycin: results from patients included in the European Cubicin((R)) Outcomes Registry and Experience. Adv Ther. 2015;32:1192–205. https://doi.org/10.1007/s12325-015-0267-4.
Jones TW, Jun AH, Michal JL, Olney WJ. High-dose daptomycin and clinical applications. Ann Pharmacother. 2021;55:1363–78. https://doi.org/10.1177/1060028021991943.
Garreau R, Montange D, Grillon A, Jehl F, Ferry T, Bourguignon L, et al. Daptomycin physiology-based pharmacokinetic modeling to predict drug exposure and pharmacodynamics in skin and bone tissues. Clin Pharmacokinet. 2022;61:1443–56. https://doi.org/10.1007/s40262-022-01168-5.
Haselden M, Leach M, Bohm N. Daptomycin dosing strategies in patients receiving thrice-weekly intermittent hemodialysis. Ann Pharmacother. 2013;47:1342–7. https://doi.org/10.1177/1060028013503110.
Patel N, Cardone K, Grabe DW, Meola S, Hoy C, Manley H, et al. Use of pharmacokinetic and pharmacodynamic principles to determine optimal administration of daptomycin in patients receiving standardized thrice-weekly hemodialysis. Antimicrob Agents Chemother. 2011;55:1677–83. https://doi.org/10.1128/AAC.01224-10.
Gould IM, Miro JM, Rybak MJ. Daptomycin: the role of high-dose and combination therapy for Gram-positive infections. Int J Antimicrob Agents. 2013;42:202–10. https://doi.org/10.1016/j.ijantimicag.2013.05.005.
Vilay AM, Grio M, Depestel DD, Sowinski KM, Gao L, Heung M, et al. Daptomycin pharmacokinetics in critically ill patients receiving continuous venovenous hemodialysis. Crit Care Med. 2011;39:19–25. https://doi.org/10.1097/CCM.0b013e3181fa36fb.
Dvorchik B, Arbeit RD, Chung J, Liu S, Knebel W, Kastrissios H. Population pharmacokinetics of daptomycin. Antimicrob Agents Chemother. 2004;48:2799–807. https://doi.org/10.1128/AAC.48.8.2799-2807.2004.
Ogami C, Tsuji Y, Kasai H, Hiraki Y, Yamamoto Y, Matsunaga K, et al. Evaluation of pharmacokinetics and the stability of daptomycin in serum at various temperatures. Int J Infect Dis. 2017;57:38–43. https://doi.org/10.1016/j.ijid.2017.01.017.
Di Paolo A, Tascini C, Polillo M, Gemignani G, Nielsen EI, Bocci G, et al. Population pharmacokinetics of daptomycin in patients affected by severe Gram-positive infections. Int J Antimicrob Agents. 2013;42:250–5. https://doi.org/10.1016/j.ijantimicag.2013.06.006.
Falcone M, Russo A, Cassetta MI, Lappa A, Tritapepe L, d’Ettorre G, et al. Variability of pharmacokinetic parameters in patients receiving different dosages of daptomycin: is therapeutic drug monitoring necessary? J Infect Chemother. 2013;19:732–9. https://doi.org/10.1007/s10156-013-0559-z.
Sancak B, Yagci S, Gur D, Gulay Z, Ogunc D, Soyletir G, et al. Vancomycin and daptomycin minimum inhibitory concentration distribution and occurrence of heteroresistance among methicillin-resistant Staphylococcus aureus blood isolates in Turkey. BMC Infect Dis. 2013;13:583. https://doi.org/10.1186/1471-2334-13-583.
Bailey EM, Rybak MJ, Kaatz GW. Comparative effect of protein binding on the killing activities of teicoplanin and vancomycin. Antimicrob Agents Chemother. 1991;35:1089–92. https://doi.org/10.1128/AAC.35.6.1089.
Bhavnani SM, Ambrose PG, Hammel JP, Rubino CM, Drusano GL. Evaluation of daptomycin exposure and efficacy and safety endpoints to support risk-versus-benefit considerations. Antimicrob Agents Chemother. 2015;60:1600–7. https://doi.org/10.1128/AAC.02967-15.
Xie F, Li S, Cheng Z. Population pharmacokinetics and dosing considerations of daptomycin in critically ill patients undergoing continuous renal replacement therapy. J Antimicrob Chemother. 2020;75:1559–66. https://doi.org/10.1093/jac/dkaa028.
Gregoire N, Marchand S, Ferrandiere M, Lasocki S, Seguin P, Vourc’h M, et al. Population pharmacokinetics of daptomycin in critically ill patients with various degrees of renal impairment. J Antimicrob Chemother. 2019;74:117–25. https://doi.org/10.1093/jac/dky374.
Samura M, Takada K, Yamamoto R, Ito H, Nagumo F, Uchida M, et al. Population pharmacokinetic analysis and dosing optimization based on unbound daptomycin concentration and cystatin C in nonobese elderly patients with hypoalbuminemia and chronic kidney disease. Pharm Res. 2021;38:1041–55. https://doi.org/10.1007/s11095-021-03058-0.
Ulldemolins M, Roberts JA, Rello J, Paterson DL, Lipman J. The effects of hypoalbuminaemia on optimizing antibacterial dosing in critically ill patients. Clin Pharmacokinet. 2011;50:99–110. https://doi.org/10.2165/11539220-000000000-00000.
Storset E, Holford N, Hennig S, Bergmann TK, Bergan S, Bremer S, et al. Improved prediction of tacrolimus concentrations early after kidney transplantation using theory-based pharmacokinetic modelling. Br J Clin Pharmacol. 2014;78:509–23. https://doi.org/10.1111/bcp.12361.
Gonzalez-Sales M, Holford N, Bonnefois G, Desrochers J. Wide size dispersion and use of body composition and maturation improves the reliability of allometric exponent estimates. J Pharmacokinet Pharmacodyn. 2022;49:151–65. https://doi.org/10.1007/s10928-021-09788-3.
Anderson BJ, Holford NH. What is the best size predictor for dose in the obese child? Paediatr Anaesth. 2017;27:1176–84. https://doi.org/10.1111/pan.13272.
Holford NHG, Anderson BJ. Allometric size: the scientific theory and extension to normal fat mass. Eur J Pharm Sci. 2017;109:59-S64. https://doi.org/10.1016/j.ejps.2017.05.056.
Matthews I, Kirkpatrick C, Holford N. Quantitative justification for target concentration intervention–parameter variability and predictive performance using population pharmacokinetic models for aminoglycosides. Br J Clin Pharmacol. 2004;58:8–19. https://doi.org/10.1111/j.1365-2125.2004.02114.x.
Kirkpatrick CM, Duffull SB, Begg EJ. Pharmacokinetics of gentamicin in 957 patients with varying renal function dosed once daily. Br J Clin Pharmacol. 1999;47:637–43. https://doi.org/10.1046/j.1365-2125.1999.00938.x.
Schwartz GJ. Does kL/PCr estimate GFR, or does GFR determine k? Pediatr Nephrol. 1992;6:512–5. https://doi.org/10.1007/bf00866487.
Kaur RGV, Ray P, Singh G, Singhal L, Tiwari R. Daptomycin susceptibility of methicillin resistant Staphylococcus aureus (MRSA). Indian J Med Res. 2012;136:676–7.
Bhavnani SM, Rubino CM, Ambrose PG, Drusano GL. Daptomycin exposure and the probability of elevations in the creatine phosphokinase level: data from a randomized trial of patients with bacteremia and endocarditis. Clin Infect Dis. 2010;50:1568–74. https://doi.org/10.1086/652767.
Woodworth JRNEJ, Brier GL, Wolny JD, Black HR. Single-dose pharmacokinetics and antibacterial activity of daptomycin, a new lipopeptide antibiotic, in healthy volunteers. Antimicrob Agents Chemother. 1992;36:318.
Schneider EK, Huang JX, Carbone V, Han M, Zhu Y, Nang S, et al. Plasma protein binding structure-activity relationships related to the N-terminus of daptomycin. ACS Infect Dis. 2017;3:249–58. https://doi.org/10.1021/acsinfecdis.7b00015.
Lim SY, Lewis T, Woo S, Turman M, Bourne DWA, Burton ME, et al. Daptomycin pharmacokinetics in adolescents undergoing hemodialysis and peritoneal dialysis: a case series with pharmacokinetic modeling. J Pediatr Pharmacol Ther. 2021;26:123–32. https://doi.org/10.5863/1551-6776-26.2.123.
Lee BL, Sachdeva M, Chambers HF. Effect of protein binding of daptomycin on MIC and antibacterial activity. Antimicrob Agents Chemother. 1991;35:2505–8. https://doi.org/10.1128/AAC.35.12.2505.
Dasgupta A, Havlik D. Elevated free fosphenytoin concentrations in uremic sera: uremic toxins hippuric acid and indoxyl sulfate do not account for the impaired protein binding of fosphenytoin. Ther Drug Monit. 1998;20:658–62. https://doi.org/10.1097/00007691-199812000-00013.
Holford N, Heo YA, Anderson B. A pharmacokinetic standard for babies and adults. J Pharm Sci. 2013;102:2941–52. https://doi.org/10.1002/jps.23574.
Falcone M, Russo A, Venditti M, Novelli A, Pai MP. Considerations for higher doses of daptomycin in critically ill patients with methicillin-resistant Staphylococcus aureus bacteremia. Clin Infect Dis. 2013;57:1568–76. https://doi.org/10.1093/cid/cit582.
Santimaleeworagun W, Changpradub D, Hemapanpairoa J, Thunyaharn S. Optimization of linezolid dosing regimens for treatment of vancomycin-resistant enterococci infection. Infect Chemother. 2021;53:503–11. https://doi.org/10.3947/ic.2021.0034.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by the Japan Society for the Promotion of Science (JSPS) KAKENHI Grant Number JP20K07189 and the Nihon University Multidisciplinary Research Grant for 2020. The funding organization did not participate in the study design, collection, analysis, and interpretation of data, writing of the report, or decision to submit the article for publication.
Conflict of Interest
The authors have no conflicts of interest to declare.
Ethical Approval
The present study was conducted with the approval of the ethics committees of the University of Toyama (approval number: R2012133 revised) and Nihon University (School of Pharmacy, approval numbers: 20–005 and 20–012) and was conducted in compliance with the Declaration of Helsinki.
Consent to Participate
Informed consent was obtained to participate in the study.
Consent for Publication
Not applicable.
Availability of Data and Material
No data are available.
Code Availability
A NONMEM code of population pharmacokinetics model will be made available on reasonable request.
Author Contributions
S.T., Y.T., and C.O. contributed to the acquisition of data, participated in the study design, analyzed and interpreted the data, and drafted the manuscript. N.H. helped with writing the manuscript. H.K. (Hidefumi Kasai) and H.T. contributed to the conception, design, and interpretation of the data. H.K. (Hitoshi Kawasuji) and Y.Y. were the clinical investigators of the trial and were responsible for the medical care of the trial participants, communication with the research ethics committee, protocol, informed consent, data integrity, and reporting. All the authors meet the ICME authorship criteria. All the authors approved the final version of the manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Takahashi, S., Tsuji, Y., Holford, N. et al. Population Pharmacokinetic Model for Unbound Concentrations of Daptomycin in Patients with MRSA Including Patients Undergoing Hemodialysis. Eur J Drug Metab Pharmacokinet 48, 201–211 (2023). https://doi.org/10.1007/s13318-023-00820-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-023-00820-0