Abstract
Aim
This study analyses the socio-demographic characteristics associated with post-sterilization regret.
Study Design
The study uses cross-sectional data from the fourth round of National Family Health Surveys (2015–2016).
Methods
Simple bivariate and binary logistic regressions analyses were used.
Results
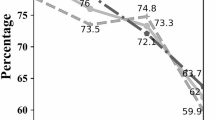
Research shows that 7% of women aged 15–49 reported sterilization regret, which increased by 2% from 2005 to 2016. It was found that factors significantly associated with sterilization regret were years since sterilization, child loss experience, regions of residence, and quality of services. Women who got sterilized at the age of 30 or more were more likely to express regret, than women who were sterilised before 25 years of age, when adjusted for confounding variables (aO.R= 1.006). Women having sons were less likely to report sterilization regret than women who had only daughters (aO.R.=1.3 for each) but on the contrary women having both son and daughter are significantly less likely to express regret in comparison with women having only sons (aO.R. = 0.8 for each. Women who had experienced child loss had higher odds of reporting sterilization regret in rural (aO.R =1.2) as well as in urban (aO.R = 1.3) areas respectively, compared to those who did not experience any child loss.
Conclusion
Women need to be counselled about the permanent nature of sterilization in order to avoid future regret as sterilization is largely dominated by socio-economic conditions. Thus, couples’ decision-making towards using the contraceptive from the basket of choice would help in uplifting the social and cultural status of women in conservative societies and will have a positive effect on contraceptive use. In addition, efforts should be made to educate both the partners equally about contraceptive methods that have higher efficiency. Further, there is also a need to improve the quality of services, both in terms of counselling and service provision. Lastly, health-related policies should tackle disparities in the empowerment, and economic status of women that would result in decreased post-sterilization regret, and will improve sexual relationships following sterilization.
Similar content being viewed by others
Data Sharing Statement
The authors confirm that all data underlying the findings are fully available without restriction. Data are publicly available from the Demographic and Health Survey website: https://dhsprogram.com/data/available-datasets.cfm
References
United Nations, Department of Economic and Social Affairs, Population Division. World Contraceptive Use. [Internet]. 2009 [cited 2019 Apr 26]. https://www.un.org/en/development/desa/population/publications/pdf/family/contraceptive-2009.pdf.
Nervo P, Bawin L, Foidart JM, et al. Regret after tubal sterilization. J Gynecol Obstet Biol Reprod (Paris). 2000;29:485–91.
Schmidt JE, Hillis SD, Marchbanks PA, et al. Requesting information about and obtaining reversal after tubal sterilization: findings from the US Collaborative Review of Sterilization. Fertil Steril. 2000;74:892–8.
Visaria L, Jejeebhoy S, Merrick T. From family planning to reproductive health: challenges facing India. Int Fam Plan Perspect. 1999;25:S44–9.
Srinivasan K. Regulating reproduction in India’s population: efforts, results, and recommendations. Thousand Oaks: Sage Publications; 1995.
Srinivasan K. Population and family planning programmes in India: a review and recommendations. In: Lect 5th Dr C Chandrasekaran Meml Lect Ser Febr. 2006;3.
Jamieson D. Poststerilization regret: findings from India and the United States. Indian J Med Sci. 2007;61:359–60.
Malhotra N, Chanana C, Garg P. Post-sterilization regrets in Indian women. Indian J Med Sci. 2007;61:186–91.
Ludermir AB, Machado KMdM, da Costa AM, et al. Tubal ligation regret and related risk factors: findings from a case-control study in Pernambuco State, Brazil. Cad Saúde Pública. 2009;25:1361–8.
Singh A, Ogollah R, Ram F, et al. Sterilization regret among married women in India: implications for the Indian national family planning program. Int Perspect Sex Reprod Health. 2012;38:187.
Eeckhaut MC, Sweeney MM. The perplexing links between contraceptive sterilization and (dis) advantage in ten low-fertility countries. Popul Stud. 2016;70:39–58.
Dhungana A, Nanthamongkolchai S, Pitikultang S. Factors related to intention to undergo female sterilization among married women in Rural Kathmandu, Nepal. Nepal J Epidemiol. 2016;6:539.
Pallikadavath S, Rajan SI, Wilson C. Impact of low fertility and early age at sterilisation on women’s formal education and skill development in South India. J Popul Res. 2016;33:199–220.
Pallikadavath S, Wilson C. A paradox within a paradox: scheduled caste fertility in Kerala. Econ Polit Wkly. 2005;40:3085–93.
Sample registration system statistical report 2016. Registrar General, India; 2016.
De Oliveira IT, Dias JG, Padmadas SS. Dominance of sterilization and alternative choices of contraception in India: an appraisal of the socioeconomic impact. PLoS ONE. 2014;9:e86654.
Heil SH, Gaalema DE, Herrmann ES. Incentives to promote family planning. Prev Med. 2012;55:S106–12.
Leone T, Padmadas SS. The proliferation of female sterilization in Brazil and India A comparative analysis of the cohort and parity effects. Genus. 2007;LXIII:77–97.
Matthews Z, Padmadas S, Hutter I, et al. Does early childbearing and a sterilization-focused family planning programme in India fuel population growth? Demogr Res. 2009;20:693–720.
Lipetz C, Phillips CJ, Fleming CF. The cost-effectiveness of a long-acting reversible contraceptive (Implanon®) relative to oral contraception in a community setting. Contraception. 2009;79:304–9.
Mavranezouli I. The cost-effectiveness of long-acting reversible contraceptive methods in the UK: analysis based on a decision-analytic model developed for a National Institute for Health and Clinical Excellence (NICE) clinical practice guideline. Hum Reprod. 2008;23:1338–45.
Trussell J, Hassan F, Lowin J, et al. Achieving cost-neutrality with long-acting reversible contraceptive methods. Contraception. 2015;91:49–56.
Health Technology Assessment of Long Acting Reversible Contraceptives in India|Department of Health Research|MoHFW|Government of India [Internet]. [cited 2019 Jul 5]. https://dhr.gov.in/health-technology-assessment-long-acting-reversible-contraceptives-india.
Funding
This research received no grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical Approval
Ethical approval for this study was not sought as this study was based on secondary data.
Informed Consent
The study used the data set that is available online in the public domain; hence, there was no need to seek ethical consent to publish this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Gargi Pal is a Research Associate in National Council of Applied Economic Research, New Delhi, India; Himanshu Chaurasia is a Scientist B (Statistician) in National Institute for Research in Reproductive Health, ICMR, Parel, Mumbai, India.
Rights and permissions
About this article
Cite this article
Pal, G., Chaurasia, H. Revisiting Post-Sterilization Regret in India. J Obstet Gynecol India 70, 295–303 (2020). https://doi.org/10.1007/s13224-020-01309-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-020-01309-5