Abstract
Objectives
Type 2 diabetes mellitus (T2DM), a major metabolic disorder, is expanding at a rapidly rising worldwide prevalence and has emerged as one of the most common chronic diseases. Suboptimal health status (SHS) is considered a reversible intermediate state between health and diagnosable disease. We hypothesized that the time frame between the onset of SHS and the clinical manifestation of T2DM is the operational area for the application of reliable risk assessment tools, such as immunoglobulin G (IgG) N-glycans. From the viewpoint of predictive, preventive, and personalized medicine (PPPM/3PM), the early detection of SHS and dynamic monitoring by glycan biomarkers could provide a window of opportunity for targeted prevention and personalized treatment of T2DM.
Methods
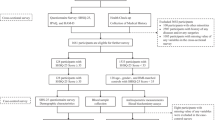
Case–control and nested case–control studies were performed and consisted of 138 and 308 participants, respectively. The IgG N-glycan profiles of all plasma samples were detected by an ultra-performance liquid chromatography instrument.
Results
After adjustment for confounders, 22, five, and three IgG N-glycan traits were significantly associated with T2DM in the case–control setting, baseline SHS, and baseline optimal health participants from the nested case–control setting, respectively. Adding the IgG N-glycans to the clinical trait models, the average area under the receiver operating characteristic curves (AUCs) of the combined models based on repeated 400 times fivefold cross-validation differentiating T2DM from healthy individuals were 0.807 in the case–control setting and 0.563, 0.645, and 0.604 in the pooled samples, baseline SHS, and baseline optimal health samples of nested case–control setting, respectively, which presented moderate discriminative ability and were generally better than models with either glycans or clinical features alone.
Conclusions
This study comprehensively illustrated that the observed altered IgG N-glycosylation, i.e., decreased galactosylation and fucosylation/sialylation without bisecting GlcNAc, as well as increased galactosylation and fucosylation/sialylation with bisecting GlcNAc, reflects a pro-inflammatory state of T2DM. SHS is an important window period of early intervention for individuals at risk for T2DM; glycomic biosignatures as dynamic biomarkers have the ability to identify populations at risk for T2DM early, and the combination of evidence could provide suggestive ideas and valuable insight for the PPPM of T2DM.





Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
The software or software package used for the data analysis is indicated in the text, and the code used for the specific analysis can be obtained from the corresponding author.
Abbreviations
- ADCC :
-
Antibody-dependent cell-mediated cytotoxicity
- ALT :
-
Alanine aminotransferase
- AP :
-
Attributable proportion due to interaction
- AST :
-
Aspartate aminotransferase
- AUC :
-
Area under the ROC curve
- BH :
-
Benjamini–Hochberg
- BMI :
-
Body mass index
- CCA :
-
Canonical correlation analysis
- CNY :
-
Chinese Yuan
- Cr :
-
Creatinine
- CVD :
-
Cardiovascular disease
- DBP :
-
Diastolic blood pressures
- DG :
-
Derived glycan
- EUR :
-
Euro
- FcγRs :
-
Fragment crystallizable γ receptors
- FDR :
-
False discovery rate
- FPG :
-
Fasting plasma glucose
- GlcNAc :
-
N-acetylglucosamine
- GP :
-
Glycan peak
- HbA1c :
-
Glycosylated hemoglobin A1c
- HDL :
-
High-density lipoprotein cholesterol
- HILIC :
-
Hydrophilic interaction liquid chromatography
- IDF :
-
International Diabetes Federation
- IgG :
-
Immunoglobulin G
- LASSO :
-
Least absolute shrinkage and selection operator
- LC–MS :
-
Liquid chromatography–mass spectrometry
- LDL :
-
Low-density lipoprotein cholesterol
- NCDs :
-
Non-communicable diseases
- OGTT :
-
Oral glucose tolerance tests
- PBG :
-
Postprandial blood glucose
- RERI :
-
Relative excess risk due to interaction
- ROC :
-
Receiver operating characteristic
- SBP :
-
Systolic blood pressures
- SD :
-
Standard deviation
- SHS :
-
Suboptimal health status
- SHSQ-25 :
-
SHS questionnaire 25 items
- S index :
-
Synergy index
- TC :
-
Total cholesterol
- TGs :
-
Total triglycerides
- T2DM :
-
Type 2 diabetes mellitus
- UA :
-
Uric acid
- UPLC :
-
Ultra-performance liquid chromatography
- USD :
-
United States dollar
- WHO :
-
World Health Organization
- WHR :
-
Waist-to-hip ratio
- 2-AB :
-
2-Aminobenzamide
- 3PM/PPPM :
-
Predictive, preventive, and personalized medicine
References
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119. https://doi.org/10.1016/j.diabres.2021.109119.
Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. 2018;14(2):88–98. https://doi.org/10.1038/nrendo.2017.151.
Heald AH, Stedman M, Davies M, Livingston M, Alshames R, Lunt M, et al. Estimating life years lost to diabetes: outcomes from analysis of National Diabetes Audit and Office of National Statistics data. Cardiovasc Endocrinol Metab. 2020;9(4):183–5. https://doi.org/10.1097/xce.0000000000000210.
Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X, et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep. 2020;10(1):14790. https://doi.org/10.1038/s41598-020-71908-9.
American Diabetes Association. Economic costs of diabetes in the US in 2017. Diabetes Care. 2018;41(5):917–28.
Pradeepa R, Mohan V. Prevalence of type 2 diabetes and its complications in India and economic costs to the nation. Eur J Clin Nutr. 2017;71(7):816–24. https://doi.org/10.1038/ejcn.2017.40.
Shen C, Ge J. Epidemic of cardiovascular disease in China: current perspective and prospects for the future. Circulation. 2018;138(4):342–4. https://doi.org/10.1161/circulationaha.118.033484.
Ogurtsova K, Guariguata L, Barengo NC, Ruiz PL, Sacre JW, Karuranga S, et al. IDF diabetes Atlas: Global estimates of undiagnosed diabetes in adults for 2021. Diabetes Res Clin Pract. 2022;183:109118. https://doi.org/10.1016/j.diabres.2021.109118.
American Diabetes Association Professional Practice Committee. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2022. Diabetes Care. 2022;45(Suppl 1):S17-s38. https://doi.org/10.2337/dc22-S002.
Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15(7):539–53. https://doi.org/10.1002/(sici)1096-9136(199807)15:7%3c539::Aid-dia668%3e3.0.Co;2-s.
Wang W, Russell A, Yan Y. Traditional Chinese medicine and new concepts of predictive, preventive and personalized medicine in diagnosis and treatment of suboptimal health. EPMA J. 2014;5(1):4. https://doi.org/10.1186/1878-5085-5-4.
Wang W, Yan Y. Suboptimal health: a new health dimension for translational medicine. Clin Transl Med. 2012;1(1):28. https://doi.org/10.1186/2001-1326-1-28.
Wang W, Yan Y, Guo Z, Hou H, Garcia M, Tan X, et al All around suboptimal health - a joint position paper of the Suboptimal Health Study Consortium and European Association for Predictive, Preventive and Personalised Medicine 2021 EPMA J. 1–31. https://doi.org/10.1007/s13167-021-00253-2.
Ge S, Xu X, Zhang J, Hou H, Wang H, Liu D, et al. Suboptimal health status as an independent risk factor for type 2 diabetes mellitus in a community-based cohort: the China suboptimal health cohort study. EPMA J. 2019;10(1):65–72. https://doi.org/10.1007/s13167-019-0159-9.
Wang Y, Liu X, Qiu J, Wang H, Liu D, Zhao Z, et al. Association between Ideal Cardiovascular Health Metrics and Suboptimal Health Status in Chinese Population. Sci Rep. 2017;7(1):14975. https://doi.org/10.1038/s41598-017-15101-5.
Yan YX, Dong J, Liu YQ, Yang XH, Li M, Shia G, et al. Association of suboptimal health status and cardiovascular risk factors in urban Chinese workers. J Urban Health. 2012;89(2):329–38. https://doi.org/10.1007/s11524-011-9636-8.
Adua E, Roberts P, Wang W. Incorporation of suboptimal health status as a potential risk assessment for type II diabetes mellitus: a case-control study in a Ghanaian population. EPMA J. 2017;8(4):345–55. https://doi.org/10.1007/s13167-017-0119-1.
Tabák AG, Herder C, Rathmann W, Brunner EJ, Kivimäki M. Prediabetes: a high-risk state for diabetes development. Lancet. 2012;379(9833):2279–90. https://doi.org/10.1016/s0140-6736(12)60283-9.
Golubnitschaja O, Baban B, Boniolo G, Wang W, Bubnov R, Kapalla M, et al. Medicine in the early twenty-first century: paradigm and anticipation - EPMA position paper 2016. EPMA J. 2016;7(1):23. https://doi.org/10.1186/s13167-016-0072-4.
Golubnitschaja O, Kinkorova J, Costigliola V. Predictive, preventive and personalised medicine as the hardcore of “Horizon 2020”: EPMA position paper. EPMA J. 2014;5(1):6. https://doi.org/10.1186/1878-5085-5-6.
Hirata T, Kizuka Y. N-Glycosylation. Adv Exp Med Biol. 2021;1325:3–24. https://doi.org/10.1007/978-3-030-70115-4_1.
Ohtsubo K, Marth JD. Glycosylation in cellular mechanisms of health and disease. Cell. 2006;126(5):855–67. https://doi.org/10.1016/j.cell.2006.08.019.
Moremen KW, Tiemeyer M, Nairn AV. Vertebrate protein glycosylation: diversity, synthesis and function. Nat Rev Mol Cell Biol. 2012;13(7):448–62. https://doi.org/10.1038/nrm3383.
Yu X, Wang Y, Kristic J, Dong J, Chu X, Ge S, et al. Profiling IgG N-glycans as potential biomarker of chronological and biological ages: a community-based study in a Han Chinese population. Medicine (Baltimore). 2016;95(28):e4112. https://doi.org/10.1097/md.0000000000004112.
Reily C, Stewart TJ, Renfrow MB, Novak J. Glycosylation in health and disease. Nat Rev Nephrol. 2019;15(6):346–66. https://doi.org/10.1038/s41581-019-0129-4.
Cobb BA. The history of IgG glycosylation and where we are now. Glycobiology. 2020;30(4):202–13. https://doi.org/10.1093/glycob/cwz065.
Gudelj I, Lauc G, Pezer M. Immunoglobulin G glycosylation in aging and diseases. Cell Immunol. 2018;333:65–79. https://doi.org/10.1016/j.cellimm.2018.07.009.
Frkatovic A, Zaytseva OO, Klaric L. Genetic Regulation of Immunoglobulin G Glycosylation. Exp Suppl. 2021;112:259–87. https://doi.org/10.1007/978-3-030-76912-3_8.
Liu D, Li Q, Dong J, Li D, Xu X, Xing W, et al. The association between normal BMI with central adiposity and proinflammatory potential immunoglobuliN G N-glycosylation. Diabetes Metab Syndr Obes. 2019;12:2373–85. https://doi.org/10.2147/dmso.S216318.
Wang Y, Klarić L, Yu X, Thaqi K, Dong J, Novokmet M, et al. The association between glycosylation of immunoglobulin G and hypertension: a multiple ethnic cross-sectional study. Medicine (Baltimore). 2016;95(17):e3379. https://doi.org/10.1097/md.0000000000003379.
Liu D, Zhao Z, Wang A, Ge S, Wang H, Zhang X, et al. Ischemic stroke is associated with the pro-inflammatory potential of N-glycosylated immunoglobulin G. J Neuroinflammation. 2018;15(1):123. https://doi.org/10.1186/s12974-018-1161-1.
Benešová I, Paulin Urminský A, Halámková J, Hernychová L. Changes of serum protein N-glycosylation in cancer. Klin Onkol. 2022;35(3):174–80. https://doi.org/10.48095/ccko2022174.
Silsirivanit A. Glycosylation markers in cancer. Adv Clin Chem. 2019;89:189–213. https://doi.org/10.1016/bs.acc.2018.12.005.
Li X, Wang H, Russell A, Cao W, Wang X, Ge S, et al. Type 2 Diabetes Mellitus is Associated with the Immunoglobulin G N-Glycome through Putative Proinflammatory Mechanisms in an Australian Population. OMICS. 2019;23(12):631–9. https://doi.org/10.1089/omi.2019.0075.
Liu J, Dolikun M, Stambuk J, Trbojevic-Akmacic I, Zhang J, Zhang J, et al. Glycomics for Type 2 Diabetes Biomarker Discovery: Promise of Immunoglobulin G Subclass-Specific Fragment Crystallizable N-glycosylation in the Uyghur Population. OMICS. 2019. https://doi.org/10.1089/omi.2019.0052.
Lemmers RFH, Vilaj M, Urda D, Agakov F, Šimurina M, Klaric L, et al. IgG glycan patterns are associated with type 2 diabetes in independent European populations. Biochim Biophys Acta Gen Subj. 2017;1861(9):2240–9. https://doi.org/10.1016/j.bbagen.2017.06.020.
Wu Z, Li H, Liu D, Tao L, Zhang J, Liang B, et al. IgG glycosylation profile and the glycan score are associated with type 2 diabetes in independent chinese populations: a case-control study. J Diabetes Res. 2020;2020:5041346. https://doi.org/10.1155/2020/5041346.
Wang Y, Ge S, Yan Y, Wang A, Zhao Z, Yu X, et al. China suboptimal health cohort study: rationale, design and baseline characteristics. J Transl Med. 2016;14(1):291. https://doi.org/10.1186/s12967-016-1046-y.
Yan YX, Liu YQ, Li M, Hu PF, Guo AM, Yang XH, et al. Development and evaluation of a questionnaire for measuring suboptimal health status in urban Chinese. J Epidemiol. 2009;19(6):333–41. https://doi.org/10.2188/jea.je20080086.
Simunovic J, Vilaj M, Trbojevic-Akmacic I, Momcilovic A, Vuckovic F, Gudelj I, et al. Comprehensive N-glycosylation analysis of immunoglobulin G from dried blood spots. Glycobiology. 2019. https://doi.org/10.1093/glycob/cwz061.
Huffman JE, Pucic-Bakovic M, Klaric L, Hennig R, Selman MH, Vuckovic F, et al. Comparative performance of four methods for high-throughput glycosylation analysis of immunoglobulin G in genetic and epidemiological research. Mol Cell Proteomics. 2014;13(6):1598–610. https://doi.org/10.1074/mcp.M113.037465.
Trbojević-Akmačić I, Ugrina I, Lauc G. Comparative analysis and validation of different steps in glycomics studies. Methods Enzymol. 2017;586:37–55. https://doi.org/10.1016/bs.mie.2016.09.027.
Assmann SF, Hosmer DW, Lemeshow S, Mundt KA. Confidence intervals for measures of interaction. Epidemiology. 1996;7(3):286–90. https://doi.org/10.1097/00001648-199605000-00012.
Antza C, Kostopoulos G, Mostafa S, Nirantharakumar K, Tahrani A. The links between sleep duration, obesity and type 2 diabetes mellitus. J Endocrinol. 2021;252(2):125–41. https://doi.org/10.1530/joe-21-0155.
Li K, Feng T, Wang L, Chen Y, Zheng P, Pan P, et al. Causal associations of waist circumference and waist-to-hip ratio with type II diabetes mellitus: new evidence from Mendelian randomization. Mol Genet Genomics. 2021;296(3):605–13. https://doi.org/10.1007/s00438-020-01752-z.
Zhou H, Zhang C, Ni J, Han X. Prevalence of cardiovascular risk factors in non-menopausal and postmenopausal inpatients with type 2 diabetes mellitus in China. BMC Endocr Disord. 2019;19(1):98. https://doi.org/10.1186/s12902-019-0427-7.
Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289(1):76–9. https://doi.org/10.1001/jama.289.1.76.
Wang TT. IgG Fc Glycosylation in Human Immunity. Curr Top Microbiol Immunol. 2019;423:63–75. https://doi.org/10.1007/82_2019_152.
Raju TS. Terminal sugars of Fc glycans influence antibody effector functions of IgGs. Curr Opin Immunol. 2008;20(4):471–8. https://doi.org/10.1016/j.coi.2008.06.007.
Liu D, Chu X, Wang H, Dong J, Ge SQ, Zhao ZY, et al. The changes of immunoglobulin G N-glycosylation in blood lipids and dyslipidaemia. J Transl Med. 2018;16(1):235. https://doi.org/10.1186/s12967-018-1616-2.
Lu JP, Knezevic A, Wang YX, Rudan I, Campbell H, Zou ZK, et al. Screening novel biomarkers for metabolic syndrome by profiling human plasma N-glycans in Chinese Han and Croatian populations. J Proteome Res. 2011;10(11):4959–69. https://doi.org/10.1021/pr2004067.
Indellicato R, Trinchera M. Epigenetic Regulation of Glycosylation in Cancer and Other Diseases. Int J Mol Sci. 2021;22(6). https://doi.org/10.3390/ijms22062980.
Zoldoš V, Novokmet M, Bečeheli I, Lauc G. Genomics and epigenomics of the human glycome. Glycoconj J. 2013;30(1):41–50. https://doi.org/10.1007/s10719-012-9397-y.
Nikolac Perkovic M, Pucic Bakovic M, Kristic J, Novokmet M, Huffman JE, Vitart V, et al. The association between galactosylation of immunoglobulin G and body mass index. Prog Neuropsychopharmacol Biol Psychiatry. 2014;48:20–5. https://doi.org/10.1016/j.pnpbp.2013.08.014.
Seeling M, Brückner C, Nimmerjahn F. Differential antibody glycosylation in autoimmunity: sweet biomarker or modulator of disease activity? Nat Rev Rheumatol. 2017;13(10):621–30. https://doi.org/10.1038/nrrheum.2017.146.
Malhotra R, Wormald MR, Rudd PM, Fischer PB, Dwek RA, Sim RB. Glycosylation changes of IgG associated with rheumatoid arthritis can activate complement via the mannose-binding protein. Nat Med. 1995;1(3):237–43. https://doi.org/10.1038/nm0395-237.
Karsten CM, Pandey MK, Figge J, Kilchenstein R, Taylor PR, Rosas M, et al. Anti-inflammatory activity of IgG1 mediated by Fc galactosylation and association of FcγRIIB and dectin-1. Nat Med. 2012;18(9):1401–6. https://doi.org/10.1038/nm.2862.
Axford JS, Mackenzie L, Lydyard PM, Hay FC, Isenberg DA, Roitt IM. Reduced B-cell galactosyltransferase activity in rheumatoid arthritis. Lancet. 1987;2(8574):1486–8. https://doi.org/10.1016/s0140-6736(87)92621-3.
Wang TT, Ravetch JV. Functional diversification of IgGs through Fc glycosylation. J Clin Invest. 2019;129(9):3492–8. https://doi.org/10.1172/jci130029.
Hmiel LK, Brorson KA, Boyne MT 2nd. Post-translational structural modifications of immunoglobulin G and their effect on biological activity. Anal Bioanal Chem. 2015;407(1):79–94. https://doi.org/10.1007/s00216-014-8108-x.
Nakano M, Mishra SK, Tokoro Y, Sato K, Nakajima K, Yamaguchi Y, et al. Bisecting GlcNAc Is a General Suppressor of Terminal Modification of N-glycan. Mol Cell Proteomics. 2019;18(10):2044–57. https://doi.org/10.1074/mcp.RA119.001534.
Komaromy A, Reider B, Jarvas G, Guttman A. Glycoprotein biomarkers and analysis in chronic obstructive pulmonary disease and lung cancer with special focus on serum immunoglobulin G. Clin Chim Acta. 2020;506:204–13. https://doi.org/10.1016/j.cca.2020.03.041.
Kaneko Y, Nimmerjahn F, Ravetch JV. Anti-inflammatory activity of immunoglobulin G resulting from Fc sialylation. Science. 2006;313(5787):670–3. https://doi.org/10.1126/science.1129594.
Quast I, Keller CW, Maurer MA, Giddens JP, Tackenberg B, Wang LX, et al. Sialylation of IgG Fc domain impairs complement-dependent cytotoxicity. J Clin Invest. 2015;125(11):4160–70. https://doi.org/10.1172/jci82695.
Meng X, Wang B, Xu X, Song M, Hou H, Wang W, et al. Glycomic biomarkers are instrumental for suboptimal health status management in the context of predictive, preventive, and personalized medicine. EPMA J. 2022;13(2):195–207. https://doi.org/10.1007/s13167-022-00278-1.
Acknowledgements
The authors acknowledge the participants and their families who donated their time and effort in helping to make this study possible.
Funding
The study was supported by grants from the China-Australian Collaborative Grant (NSFC 81561128020-NHMRC APP1112767) and the National Natural Science Foundation of China (81872920). The funding organization had the role in the design and conduct of the study and the collection, management, analysis, and interpretation of the data.
Author information
Authors and Affiliations
Contributions
QZ, WW, and YW contributed to the conception and design. XM, FW, XG, BW, and XX contributed to the acquisition and analysis of the data. XM and FW drafted the manuscript. All authors made important contributions to editing and critically revising the manuscript for important intellectual content. WW, QZ, and YW guarantee this work, have full access to all of the data, and take responsibility for the integrity of the data.
Corresponding authors
Ethics declarations
Ethics approval
Ethical approval was granted by the Ethics Committee of the Chinese PLA General Hospital (no. S2016-0681-01), according to the Helsinki Declaration.
Consent to participate
All subjects agreed to participate in the study and signed written informed consent.
Consent for publication
All authors have approved the final version to be published.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Meng, X., Wang, F., Gao, X. et al. Association of IgG N-glycomics with prevalent and incident type 2 diabetes mellitus from the paradigm of predictive, preventive, and personalized medicine standpoint. EPMA Journal 14, 1–20 (2023). https://doi.org/10.1007/s13167-022-00311-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13167-022-00311-3