Abstract
In intracerebral hemorrhage (ICH) with pathology-proven etiology, we performed a systematic review and meta-analysis to elucidate the association between cerebral amyloid angiopathy (CAA) and arteriolosclerosis, and directly compared MRI and pathological changes of markers of cerebral small vessel disease (CSVD). Studies enrolling primary ICH who had received an etiological diagnosis through biopsy or autopsy were searched using Ovid MEDLINE, PubMed, and Web of Science from inception to June 8, 2022. We extracted pathological changes of CSVD for each patient whenever available. Patients were grouped into CAA + arteriolosclerosis, strict CAA, and strict arteriolosclerosis subgroups. Of 4155 studies identified, 28 studies with 456 ICH patients were included. The frequency of lobar ICH (p<0.001) and total microbleed number (p=0.015) differed among patients with CAA + arteriolosclerosis, strict CAA, and strict arteriolosclerosis. Concerning pathology, severe CAA was associated with arteriolosclerosis (OR 6.067, 95% CI 1.107–33.238, p=0.038), although this association was not statistically significant after adjusting for age and sex. Additionally, the total microbleed number (median 15 vs. 0, p=0.006) was higher in ICH patients with CAA evidence than those without CAA. The pathology of CSVD imaging markers was mostly investigated in CAA-ICH. There was inconsistency concerning CAA severity surrounding microbleeds. Small diffusion-weighted imaging lesions could be matched to acute microinfarct histopathologically. Studies that directly correlated MRI and pathology of lacunes, enlarged perivascular spaces, and atrophy were scarce. Arteriolosclerosis might be associated with severe CAA. The pathological changes of CSVD markers by ICH etiology are needed to be investigated further.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary intracerebral hemorrhage (ICH) results in high morbidity and disability. Cerebral small vessel disease (CSVD) is the major cause of primary ICH [1]: arteriolosclerosis, which is closely associated with hypertension [2], mainly accounts for deep ICH, and cerebral amyloid angiopathy (CAA) accounts for lobar ICH. Notably, CAA and arteriolosclerosis coexist frequently. Previous studies have found that lobar ICH/microbleed and deep ICH/microbleed could coexist in a patient [3]. Additionally, animal studies have found that an increase in systolic blood pressure promotes the occurrence of ICH in Tg2576 mice characterized by amyloid beta (Aβ) deposition [4]. And in a clinical study, subgroup analysis of the PROGRESS study has shown that antihypertensive treatment (vs. placebo) reduced the risk of ICH in CAA patients [5]. However, there is currently a lack of systematic reviews that assess the association between CAA and arteriolosclerosis in ICH patients with pathology-proven evidence.
On the other hand, increasing evidence has demonstrated that imaging markers of CSVD are related to the presence and prognosis of primary ICH [6, 7]. However, the characteristics of CSVD markers in patients with pathological evidence for arteriolosclerosis- and CAA-related ICH, and the underlying pathological changes of theses markers, remain unclear. Although a previous study [8] reviewed the pathological substrates of CSVD such as cerebral microbleeds (CMB) and white matter changes, the majority of included studies investigated Alzheimer’s disease. Despite 80~97% of patients with Alzheimer’s disease have CAA at autopsy, most of them do not suffer from symptomatic ICH [9, 10]. We, therefore, performed a systematic review and meta-analysis to elucidate (1) the association between arteriolosclerosis and CAA and their imaging characteristics, and (2) the imaging and pathological correlations of CSVD markers in primary ICH patients to better understand the mechanisms underlying primary ICH.
Methods
Search Strategy
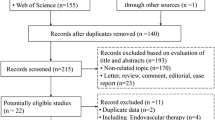
Our study was approved by the Ethics Committee on Biomedical Research, West China Hospital of Sichuan University, and was registered in PROSPERO (CRD42022343347). We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses [11] guidelines. We systematically searched PubMed, Ovid Medline, and Web of Science for studies investigating the neuropathology of CSVD in patients with primary ICH until 8 June 2022. The following terms were used: “(cerebral hemorrhage) OR (intracranial hemorrhage)” AND “(patholog*) OR (postmortem) OR (autopsy) OR (biopsy)” AND “(cerebral small vessel diseases) OR (microvessel) OR (white matter) OR (microinfarct) OR (lacune) OR (perivascular space) OR (microbleed) OR (microhemorrhage) OR (atrophy).” Additionally, references to relevant studies were searched. The details of the study selection process are presented in Fig. 1.
Eligibility Criteria
The included criteria were as follows: investigating adult patients (age≥18 years) with primary ICH; having autopsy or biopsy to confirm the etiology for arteriolosclerosis and CAA; with or without CSVD markers, including white matter changes, CMB, cerebral microinfarcts (CMI), lacunes, enlarged perivascular spaces (EPVS), brain atrophy, and the total CSVD burden. Abstract, review, editorial, and basic research were excluded. This systematic review only focused on primary ICH, not on hemorrhage into the subarachnoid space, epidural space, or subdural space. Pure intraventricular hemorrhage, ICH secondary to trauma, structural vascular lesions, inflammation, infections, inherited or genetic small vessel diseases, and hemorrhagic transformation after ischemic stroke were beyond the scope of this review. We only included studies that were published in English.
Data Extraction
Two authors (Mangmang Xu and Xindi Song) independently searched the literature and extracted data. Any disagreement was resolved by consensus. A data extraction form was developed using SPSS. For each included study, we extracted the family name of the first author, publication year, country of origin, the sample size of primary ICH, examination method (autopsy or biopsy), patient demographics (male sex, age at death or biopsy), pathology diagnosis (CAA or arteriolosclerosis), ICH location (lobe, deep, cerebellum), and CSVD imaging markers including white matter changes, lacunes, CMB, CMI, EPVS, atrophy, and total CSVD burden. For studies that investigated ICH with CAA evidence, we additionally extracted information on the diagnostic method of CAA, CAA-related small vessel wall changes (SVWCs), the coexistence of arteriolosclerosis, senile plaques, and blood vessel changes in or around the hematoma.
Definitions
Lobar ICH included hemorrhages originating from the frontal, temporal, parietal, or occipital lobes of the brain. For the two studies [12, 13] that enrolled clinically diagnosed CAA-ICH according to the modified Boston criteria without reporting ICH location, we regarded those cases as having lobe ICH. Deep ICH was considered when originating from the basal ganglia, thalamus, internal capsule, external capsule, or brain stem. Biology included brain biopsy and biopsy at hematoma evacuation in this study.
Severe CAA in histopathology was defined as follows: (1) a CAA score of 9–12 for the study [12] that used a cumulative cortical CAA score with a range of 0–12 by calculating the basis of Aβ stained sections from four areas, (2) a CAA score of 3–4 for those studies [14,15,16,17] that used the grading scale by Greenberg and Vonsattel with a range of 0–4, (3) a CAA score of 3+ indicating that many lesions were visible [18] in a scale of 1+~3+, or as per the original study authors’ definition [19,20,21,22].
Arteriolosclerosis was defined if there existed lipofibrohyalinosis [20], lipohyalinosis [21, 23], arteriolosclerosis [13, 18, 19, 24,25,26,27,28], or hypertensive vasculopathy [12, 13, 17] on pathology. For the study [21] that performed a pathological examination and concluded that there were no other possible causes of ICH except CAA, we considered those cases as strict CAA.
Statistical Analysis
Most of the included studies were case reports, so we extracted individual patient data from those cases. The demographic data in the study by Ter Telgte [12] were the same as that in the study by van Veluw [13]; therefore, we only extracted data from the latter. For CMB analysis, we extracted CMB number in ex vivo MRI in the study by van Veluw 2016 [17], under the other two studies [13, 20]. Independent-samples T test, one-way ANOVA, Mann-Whitney U test, or Kruskal-Wallis H test were used for continuous variables, and Pearson chi-squared test or Fisher’s exact test for categorical variables, when appropriate. Multivariate analysis was performed using binary logistic regression. For the statistical analysis in our present study, hemorrhage in the cerebellum was categorized as lobar ICH. All statistical analyses were performed using IBM SPSS Statistics (version 23), and a p value of ≤0.05 was considered statistically significant.
Results
Study Characteristics
A total of 4155 citations and 509 full texts were screened (Fig. 1). Of these, 28 studies with 456 participants were included [12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39]. The characteristics of included studies are shown in Table 1. Most of the studies were conducted in the USA (39.3%, 11/28), followed by Japan (28.6%, 8/28). Three hundred twenty patients had CAA with or without arteriolosclerosis; 48 patients had strict CAA while 19 had CAA + arteriolosclerosis. CAA-related SVWCs were investigated in 17 studies [14,15,16,17,18,19,20,21,22, 24, 29,30,31,32,33, 38, 39], and their detailed pathological changes are summarized in the Supplementary table.
The Association Between Arteriolosclerosis and CAA
Ten studies [13, 17,18,19,20,21, 23,24,25, 33] with 79 cases assessed both CAA and arteriolosclerosis histopathologically. CAA + arteriolosclerosis accounted for 21.5% (17/79) of cases. The frequency of lobar ICH differed among CAA + arteriolosclerosis, strict CAA, and strict arteriolosclerosis (82.4%, 100%, 38.9%, respectively; p<0.001), so did the total number of CMB (median 7, 161, 0, respectively; p=0.015).
Ten studies [13,14,15,16,17,18,19,20,21,22] with 76 cases assessed the presence and severity of CAA on pathology. Data showed that severe SVWCs due to CAA were highly prevalent (67.6%, 53/76), which was found to be associated with arteriolosclerosis when compared with CAA without severe SVWCs (58.3 vs. 18.8%, p=0.050; OR 6.067, 95% CI 1.107–33.238, p=0.038). However, this association was not significant after correcting for age and sex (adjusted OR 4.959, 95% CI 0.734–33.521, p=0.101).
The Clinical and Imaging Characteristics of Arteriolosclerosis and CAA
As shown in Table 2, all cases of ICH due to strict CAA aged > 55 years and had lobar ICH. CAA presence was associated with a higher number of CMB (CAA vs. non-CAA: 15 (2–104) vs. 0 (0–3), p=0.006, calculated from 7 studies [13, 16, 17, 20, 25, 31, 34] with 29 participants), as well as a higher number of CMI (CAA vs. non-CAA: 29 (3.5–56.25) vs. 0 (0–0), p=0.064, calculated from 3 studies [13, 17, 25] with 10 participants), although without reaching a statistically significant difference for the latter. And patients with strict CAA were more likely to have a higher number of total CMB (OR 1.016, 95% CI 1.002–1.030, p=0.029, as determined by binary logistic regression) than those with strict arteriolosclerosis or CAA+ arteriolosclerosis; this association remained significant after adjusting for age and sex (adjusted OR 1.015, 95% CI 1.001–1.029, p=0.040). There existed conflicting results regarding the association between ICH etiology and CMB number by location [20, 32]. For cerebellar CMB, CAA-ICH had more superficial cerebellar CMB, while non-CAA-ICH had more deep/mixed cerebellar CMB [37].
For patients with ICH due to strict arteriolosclerosis, the majority (61.1%) of ICH were located in deep regions of the brain. The presence of arteriolosclerosis was significantly associated with hypertension (percentage of hypertension in arteriosclerosis vs. non-arteriolosclerosis: 74.6 vs. 36.4%, p=0.001). This association remained significant after correcting for age and sex (adjusted OR 3.329, 95% CI 1.056–10.495, p=0.040).
The Correlation Between MRI and Pathological Changes of CSVD Markers in Primary ICH
White Matter Changes
Overall, six studies [15, 18, 20, 30, 32, 36] investigated white matter changes on CT or MRI. Of these, three studies [18, 20, 30] examined the correlation between MRI and pathological changes in white matter lesions (Table 3). White matter changes were associated with rarefaction of myelin staining, diffuse or patchy myelin loss, diffuse white matter edema, and even advanced white matter loss [20, 30]. Histologically, the white matter appeared vacuolated and was accompanied by swollen oligodendrocytes and astrocytic proliferation [18, 30]. Amyloid plaques that were positive for Aβ were occasionally observed in the white matter [18]. However, CAA-associated vasculopathy did not always result in ischemic white matter lesions [18].
Cerebral Microbleed
Twelve studies [13, 15,16,17, 20, 22, 25, 31, 32, 34, 35, 37] investigated CMB on MRI, and nine [13, 16, 17, 20, 22, 25, 31, 34, 35] of them retrieved CMB for histopathological analysis. The pathological changes of CMB in primary ICH are presented in Table 4. There existed inconsistencies in CAA severity around a CMB [13, 25]. The vessels involved in CMB were enlarged and fibrinoid necrotic, with extensive remodeling of the vessel wall [13]. On the other hand, a high CMB count was associated with an increased wall thickness of amyloid-positive vessels, and this increased thickness of vessel walls might be more prone to CMB formation than macrobleed formation [34].
Cerebral Microinfarct
Four studies [12, 13, 17, 25] investigated CMI, and all four investigated pathological changes of CMI, as detailed in Table 4. The findings suggested that small DWI lesions could be matched to acute CMI histopathologically, characterized by tissue pallor consisting of eosinophilic neurons, absent or only mild reactive astrocytes, and absent or fragmented microglia. And chronic cortical CMI was associated with tissue loss or central cavitation, as well as many reactive astrocytes around the lesions and few reactive or amoeboid microglia [12]. CAA was found to be severe surrounding a CMI, particularly for CMI in those with lobar ICH.
Lacunes, EPVS, and Brain Atrophy
Each of the three imaging markers was investigated in a separate study (Table 1). Patients with brain atrophy corresponded to amyloid deposition in the parenchyma and small vessels [15]. However, the pathological changes of lacune and EPVS in primary ICH were not investigated.
Total CSVD Burden
Two studies [26, 36] investigated the total CSVD burden (Table 4). A direct histopathological-MRI study demonstrated that the total CAA burden of CSVD, as determined by summing the four most characteristic MRI markers of CAA, was associated with the presentation of symptomatic CAA-related ICH (versus CAA without ICH) and CAA-related microangiopathy on pathology [36].
Discussion
We presented here a comprehensive systematic review of published articles that investigated ICH with pathology-proven evidence for arteriolosclerosis and CAA. Our study directly compared MRI and pathology to clarify the pathological changes of CSVD imaging markers. To the best of our knowledge, this is the first review to assess the interaction between arteriolosclerosis and CAA by summarizing published cases with a pathology diagnosis of CAA or arteriolosclerosis in ICH. Our findings provide pathological evidence that there might be differences in lobar ICH and total microbleed number among CAA + arteriolosclerosis, strict CAA, and strict arteriolosclerosis, and there might be an association between arteriolosclerosis and severe CAA, which needs to be investigated further in future studies.
Although the SVWCs in CAA-ICH were found to be similar to those in CAA without ICH, in terms of the location of Aβ deposition and the changes in the lumen [40], our findings suggest that severe CAA (usually characterized by double barreling and/or fibrinoid necrosis) is highly prevalent in CAA-ICH. Our results, together with the findings of Vonsattel et al. [21], indicate that a severe degree of CAA represents an important feature of CAA-ICH [21].
Regarding the CSVD markers in ICH, we found that patients with CAA had higher number of total CMB, particularly for patients with strict CAA, as compared to those without CAA on pathology. This finding was in line with previous study by Edip Gurol et al. that found that patients with CAA-ICH had higher number of total CMB as compared to those with non-CAA related ICH [41]. In addition, the total CAA burden assessed in neuroimaging was associated with the presentation of symptomatic CAA-related ICH and CAA-related microangiopathy on pathology. Therefore, it might be reasonable to speculate that higher individual CSVD markers indicate greater Aβ severity. However, our analysis of individual patient data showed that severe CAA was not associated with CMB number, which is in line with the findings of another study that found CMB to be frequently located around Aβ negative small vasculature [42]. In addition, one amyloid positron emission tomography study evaluating CAA burden in both the ICH-affected hemisphere and the ICH-free hemisphere indicated that amyloid burden was similarly distributed and ICH was unlikely to be directly linked to amyloid burden [43]. Taken together, these findings challenge the hypothesis that the ruptured vessel reflects a significant Aβ load [42].
As expected, hypertension was significantly associated with arteriolosclerosis, which was highly prevalent in CAA-ICH as well. It is widely accepted that lobar hemorrhage is required for CAA diagnosis per the Boston Criteria [44]. In this study, we found that all cases of strict CAA-ICH were located in the lobes. However, we also found that in some patients with the coexistence of CAA and arteriolosclerosis on pathology, the hemorrhage could be located in deep territories, suggesting that the presence of deep ICH could not preclude the possibility of amyloid angiopathy in the elderly patients.
Overall, the pathology of CSVD markers in ICH was under-researched, with most studies focusing on CAA-ICH. While the majority of CMBs observed on MRI could be confirmed histopathologically, several CMBs could not be confirmed, with no abnormality or small cavities at neuropathological amination [20, 35]. Compared with standard histopathological sections, MRI tends to underestimate the total burden of CMB [20], as well as CMI [13]. The lesions that could not be retrieved for histological analysis were generally too small [25]. Therefore, future studies with high-field MRI scanners are warranted to capture the total burden of these two markers [20, 35]. Of note, CMB on MRI was traditionally recognized to represent foci of past hemorrhage [20, 22]. However, this review found that CMB could also correspond to recent microhemorrhage with small bleeds in patients with ICH [35].
Another interesting finding was the inconsistency in CAA severity around CMB [13, 25]. This inconsistency might be attributed to the different methodologies used by the two studies. Jolink et al. [25] investigated CAA severity for each patient by taking samples with multiple lesions, while van Veluw et al. [13] assessed CAA for each section that contained CMB. Studies that directly correlated MRI and pathology of lacunes, EPVS, and atrophy were scarce. Thus, future studies are warranted to further elucidate the CAA pathology around CMB and CMI, and to assess the pathology of lacunes, EPVS, and atrophy in ICH.
Strength and Limitation
The present systematic review provided the most recent and comprehensive overview of the pathology of CSVD in primary ICH. Studies were comprehensively searched from databases using a systematic search strategy, as well as from handsearching of references of relevant studies. However, the majority of included studies only assessed the presence of CAA on pathology, without information on arteriolosclerosis, resulting in a relatively small number of cases with CAA + arteriolosclerosis, strict CAA, and strict arteriolosclerosis. Despite this, our study has the largest number of ICH cases with pathology-proven etiology across the literature and firstly provides the clinical and imaging information for CAA+arteriolosclerosis, strict CAA, and strict arteriolosclerosis.
Conclusion and Considerations for Future Research
In summary, our study provides synthesized pathological evidence for the hypothesis that there might be an interaction between CAA and arteriolosclerosis. Future studies are needed to verify our findings. The pathological changes of CSVD features in neuroimaging are heterogeneous, and MRI-histopathological correlation studies of lacunes and EPVS remain scarce. Therefore, further investigation is needed to explore the pathological changes of CSVD markers by ICH etiology. Additionally, studies using advanced MRI techniques with a high spatial resolution to visualize structural and functional brain changes of CSVD in ICH are also warranted.
References
Gross BA, Jankowitz BT, Friedlander RM. Cerebral intraparenchymal hemorrhage: a review. Jama. 2019;321:1295–303.
Blevins BL, Vinters HV, Love S, Wilcock DM, Grinberg LT, Schneider JA, et al. Brain arteriolosclerosis. Acta Neuropathol. 2021;141:1–24.
Pasi M, Charidimou A, Boulouis G, Auriel E, Ayres A, Schwab KM, et al. Mixed-location cerebral hemorrhage/microbleeds: underlying microangiopathy and recurrence risk. Neurology. 2018;90:e119–e26.
Passos GF, Kilday K, Gillen DL, Cribbs DH, Vasilevko V. Experimental hypertension increases spontaneous intracerebral hemorrhages in a mouse model of cerebral amyloidosis. J Cereb Blood Flow Metabol : Official J The Inter Soc Cereb Blood Flow Metabol. 2016;36:399–404.
Arima H, Tzourio C, Anderson C, Woodward M, Bousser MG, MacMahon S, et al. Effects of perindopril-based lowering of blood pressure on intracerebral hemorrhage related to amyloid angiopathy: the PROGRESS trial. Stroke. 2010;41:394–6.
Charidimou A, Imaizumi T, Moulin S, Biffi A, Samarasekera N, Yakushiji Y, et al. Brain hemorrhage recurrence, small vessel disease type, and cerebral microbleeds: a meta-analysis. Neurology. 2017;89:820–9.
Xu M, Li B, Zhong D, Cheng Y, Wu Q, Zhang S, et al. Cerebral small vessel disease load predicts functional outcome and stroke recurrence after intracerebral hemorrhage: a median follow-up of 5 years. Front Aging Neurosci. 2021;13:628271.
Gouw AA, Seewann A, van der Flier WM, Barkhof F, Rozemuller AM, Scheltens P, et al. Heterogeneity of small vessel disease: a systematic review of MRI and histopathology correlations. J Neurol Neurosurg Psychiatry. 2011;82:126–35.
Beckmann N, Doelemeyer A, Zurbruegg S, Bigot K, Theil D, Frieauff W, et al. Longitudinal noninvasive magnetic resonance imaging of brain microhemorrhages in BACE inhibitor-treated APP transgenic mice. Neurobiol Aging. 2016;45:50–60.
Jellinger KA, Attems J. Incidence of cerebrovascular lesions in Alzheimer’s disease: a postmortem study. Acta Neuropathol. 2003;105:14–7.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ (Clinical research ed). 2021;372:n160.
Ter Telgte A, Scherlek AA, Reijmer YD, van der Kouwe AJ, van Harten T, Duering M, et al. Histopathology of diffusion-weighted imaging-positive lesions in cerebral amyloid angiopathy. Acta Neuropathol. 2020;139:799–812.
van Veluw SJ, Scherlek AA, Freeze WM, Ter Telgte A, van der Kouwe AJ, Bacskai BJ, et al. Different microvascular alterations underlie microbleeds and microinfarcts. Ann Neurol. 2019;86:279–92.
Lin CM, Arishima H, Kikuta KI, Naiki H, Kitai R, Kodera T, et al. Pathological examination of cerebral amyloid angiopathy in patients who underwent removal of lobar hemorrhages. J Neurol. 2018;265:567–77.
Poyuran R, Mahadevan A, Arimappamagan A, Nandeesh BN, Nagappa M, Saini J, et al. Cerebrovascular pathology in cerebral amyloid angiopathy presenting as intracerebral haemorrhage. Virchows Archiv : Inter J Pathol. 2019;474:235–45.
Schrag M, McAuley G, Pomakian J, Jiffry A, Tung S, Mueller C, et al. Correlation of hypointensities in susceptibility-weighted images to tissue histology in dementia patients with cerebral amyloid angiopathy: a postmortem MRI study. Acta Neuropathol. 2010;119:291–302.
van Veluw SJ, Charidimou A, van der Kouwe AJ, Lauer A, Reijmer YD, Costantino I, et al. Microbleed and microinfarct detection in amyloid angiopathy: a high-resolution MRI-histopathology study. Brain J Neurol. 2016;139:3151–62.
Oide T, Takahashi H, Yutani C, Ishihara T, Ikeda S. Relationship between lobar intracerebral hemorrhage and leukoencephalopathy associated with cerebral amyloid angiopathy: clinicopathological study of 64 Japanese patients. Amyloid : The Inter J Exp Clin Invest : The Official J The Inter Soc Amyloid. 2003;10:136–43.
Ishii N, Nishihara Y, Horie A. Amyloid angiopathy and lobar cerebral haemorrhage. J Neurol Neurosurg Psychiatry. 1984;47:1203–10.
Fazekas F, Kleinert R, Roob G, Kleinert G, Kapeller P, Schmidt R, et al. Histopathologic analysis of foci of signal loss on gradient-echo T2*-weighted MR images in patients with spontaneous intracerebral hemorrhage: evidence of microangiopathy-related microbleeds. AJNR Am J Neuroradiol. 1999;20:637–42.
Vonsattel JP, Myers RH, Hedley-Whyte ET, Ropper AH, Bird ED, Richardson EP Jr. Cerebral amyloid angiopathy without and with cerebral hemorrhages: a comparative histological study. Ann Neurol. 1991;30:637–49.
Hernandez-Guillamon M, Martinez-Saez E, Delgado P, Domingues-Montanari S, Boada C, Penalba A, et al. MMP-2/MMP-9 plasma level and brain expression in cerebral amyloid angiopathy-associated hemorrhagic stroke. Brain pathol (Zurich, Switzerland). 2012;22:133–41.
Cordonnier C, Leys D, Dumont F, Deramecourt V, Bordet R, Pasquier F, et al. What are the causes of pre-existing dementia in patients with intracerebral haemorrhages? Brain J Neurol. 2010;133:3281–9.
Takeda S, Onda K, Yoshida Y. Immunohistochemical analysis of intrasulcal hematoma due to cerebral amyloid angiopathy in a brain-dead patient. Neuropathology : official journal of the Japanese Society of. Neuropathology. 2018;
Jolink WMT, van Veluw SJ, Zwanenburg JJM, Rozemuller AJM, van Hecke W, Frosch MP, et al. Histopathology of cerebral microinfarcts and microbleeds in spontaneous intracerebral hemorrhage. Transl Stroke Res. 2022;
Pasi M, Rocha E, Samore W, Frosch MP, Viswanathan A, Singhal AB. Premature vascular disease in young adult stroke: a pathology-based case series. J Neurol. 2020;267:1063–9.
Mastaglia FL, Edis B, Kakulas BA. Medullary haemorrhage: a report of two cases. J Neurol Neurosurg Psychiatry. 1969;32:221–5.
Takebayashi S, Kaneko M. Electron microscopic studies of ruptured arteries in hypertensive intracerebral hemorrhage. Stroke. 1983;14:28–36.
Takeda S, Hinokuma K, Yamazaki K, Onda K, Miyakawa T, Ikuta F, et al. The hemorrhage caused by sporadic-type cerebral amyloid angiopathy occurs primarily in the cerebral sulci. Neuropathol : Official J The Japanese Soc Neuropathol. 2012;32:38–43.
Gray F, Dubas F, Roullet E, Escourolle R. Leukoencephalopathy in diffuse hemorrhagic cerebral amyloid angiopathy. Ann Neurol. 1985;18:54–9.
Shelton JS, Davis LT, Peebles RS, Tillman BF, Mobley BC. Cerebral amyloid angiopathy presenting with synchronous bilateral intracerebral macrohemorrhages. Case Reports In Neurol. 2015;7:233–7.
Doden T, Sato H, Sasahara E, Murata T, Yako T, Kitazawa K, et al. Clinico-radiological characteristics and pathological diagnosis of cerebral amyloid angiopathy-related intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2016;25:1736–45.
Gilbert JJ, Vinters HV. Cerebral amyloid angiopathy: incidence and complications in the aging brain. I Cereb Hemo Stroke. 1983;14:915–23.
Greenberg SM, Nandigam RN, Delgado P, Betensky RA, Rosand J, Viswanathan A, et al. Microbleeds versus macrobleeds: evidence for distinct entities. Stroke. 2009;40:2382–6.
Guidoux C, Hauw JJ, Klein IF, Labreuche J, Berr C, Duyckaerts C, et al. Amyloid angiopathy in brain hemorrhage: a postmortem neuropathological-magnetic resonance imaging study. Cerebrovasc Dis (Basel, Switzerland). 2018;45:124–31.
Charidimou A, Martinez-Ramirez S, Reijmer YD, Oliveira-Filho J, Lauer A, Roongpiboonsopit D, et al. Total magnetic resonance imaging burden of small vessel disease in cerebral amyloid angiopathy: an imaging-pathologic study of concept validation. JAMA Neurol. 2016;73:994–1001.
Pasi M, Pongpitakmetha T, Charidimou A, Singh SD, Tsai HH, Xiong L, et al. Correction to: cerebellar microbleed distribution patterns and cerebral amyloid angiopathy: a magnetic resonance imaging and pathology-based study. Stroke. 2019;50:e240.
van Etten ES, Auriel E, Haley KE, Ayres AM, Vashkevich A, Schwab KM, et al. Incidence of symptomatic hemorrhage in patients with lobar microbleeds. Stroke. 2014;45:2280–5.
Yoshimura M, Yamanouchi H, Kuzuhara S, Mori H, Sugiura S, Mizutani T, et al. Dementia in cerebral amyloid angiopathy: a clinicopathological study. J Neurol. 1992;239:441–50.
Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. The Lancet Neurol. 2010;9:689–701.
Pasi M, Boulouis G, Fotiadis P, Auriel E, Charidimou A, Haley K, et al. Distribution of lacunes in cerebral amyloid angiopathy and hypertensive small vessel disease. Neurology. 2017;88:2162–8.
Schreiber S, Wilisch-Neumann A, Schreiber F, Assmann A, Scheumann V, Perosa V, et al. Invited review: the spectrum of age-related small vessel diseases: potential overlap and interactions of amyloid and nonamyloid vasculopathies. Neuropathol Appl Neurobiol. 2020;46:219–39.
Planton M, Pariente J, Nemmi F, Albucher JF, Calviere L, Viguier A, et al. Interhemispheric distribution of amyloid and small vessel disease burden in cerebral amyloid angiopathy-related intracerebral hemorrhage. Eur J Neurol. 2020;27:1664–71.
Linn J, Halpin A, Demaerel P, Ruhland J, Giese AD, Dichgans M, et al. Prevalence of superficial siderosis in patients with cerebral amyloid angiopathy. Neurology. 2010;74:1346–50.
Acknowledgements
We acknowledged Assistant Professor William Robert Kwapong for his invaluable assistance in refining the writing throughout the manuscript.
Data Availability
The datasets analyzed during the current study are available in the ScienceDB repository (https://www.scidb.cn/en/s/UjiIfy).
Funding
This study was supported by the National Natural Science Foundation of China (82001250), the China Postdoctoral Science Foundation (2020M683322, 2021T140488), and the 1.3.5 Project for Disciplines of Excellence, West China Hospital, Sichuan University (ZYGD18009).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics Approval
Our study was approved by the Ethics Committee on Biomedical Research, West China Hospital of Sichuan University.
Consent to Participate
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 27 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xu, M., Zhu, Y., Song, X. et al. Pathological Changes of Small Vessel Disease in Intracerebral Hemorrhage: a Systematic Review and Meta-analysis. Transl. Stroke Res. (2023). https://doi.org/10.1007/s12975-023-01154-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12975-023-01154-4