Abstract
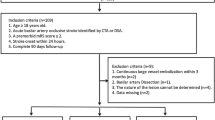
The current study aimed to evaluate whether patients with different pathologic subtypes of basilar artery occlusion (BAO) stroke could affect the clinical outcome after receiving endovascular treatment (EVT). A total of 187 consecutive patients with acute BAO receiving endovascular treatment (EVT) from January 2012 to July 2018 at the Beijing Tiantan Hospital were recruited in this study. The patients were categorized into three groups: embolism without vertebral artery (VA) steno-occlusion (group 1), in situ atherosclerotic thrombosis (group 2), and embolism from tandem VA steno-occlusion (group 3). Among the 187 patients, 4 patients with embolic combined with ICAS and 1 patient with tandem VA steno-occlusion combined with ICAS were excluded. Of the remaining 182 patients (153 men and 29 women; mean age, 60 years), 43 (23.6%) had embolism without vertebral artery (VA) steno-occlusion (group 1), 116 (63.7%) showed in situ atherosclerotic thrombosis (group 2), and 23 (12.6%) had embolism from tandem VA steno-occlusion (group 3). Overall, successful recanalization (modified thrombolysis in cerebral infarction grade 2b or 3) was achieved in 95.3%, 86.2%, and 60.9% in groups 1, 2, and 3, respectively. The favorable outcome (90-day modified Rankin scale score, 0–3) in the three groups was 51.2%, 52.6%, and 30.4%, respectively. Mortality was higher in group 3 (47.8%) as compared with groups 1 (16.3%) (p = 0.009) and 2 (17.2%) (p = 0.004). Embolism from tandem VA steno-occlusion (group 3) seems to be associated with a lower rate of recanalization and significantly higher rate of mortality as compared with another pathological mechanism of BAO.



Similar content being viewed by others
References
Schonewille WJ, Wijman CA, Michel P, Rueckert CM, Weimar C, Mattle HP, et al. Treatment and outcomes of acute basilar artery occlusion in the Basilar Artery International Cooperation Study (BASICS): a prospective registry study. Lancet Neurol. 2009;8:724–30.
Schonewille WJ, Algra A, Serena J, Molina CA, Kappelle LJ. Outcome in patients with basilar artery occlusion treated conventionally. J Neurol Neurosurg Psychiatry. 2005;76:1238–41.
Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–31.
Bracard S, Ducrocq X, Mas JL, Soudant M, Oppenheim C, Moulin T, et al. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol. 2016;15:1138–47.
Glass TA, Hennessey PM, Pazdera L, Chang HM, Wityk RJ, Dewitt LD, et al. Outcome at 30 days in the New England Medical Center Posterior Circulation Registry. Arch Neurol. 2002;59:369–76.
De Marchis GM, Kohler A, Renz N, Arnold M, Mono ML, Jung S, et al. Posterior versus anterior circulation strokes: comparison of clinical, radiological and outcome characteristics. J Neurol Neurosurg Psychiatry. 2011;82:33–7.
Mattle HP, Arnold M, Lindsberg PJ, Schonewille WJ, Schroth G. Basilar artery occlusion. Lancet Neurol. 2011;10:1002–14.
Singer OC, Berkefeld J, Nolte CH, Bohner G, Haring HP, Trenkler J, et al. Mechanical recanalization in basilar artery occlusion: the ENDOSTROKE study. Ann Neurol. 2015;77:415–24.
Ecker RD, Tsujiura CA, Baker CB, Cushing D. Endovascular reconstruction of vertebral artery occlusion prior to basilar thrombectomy in a series of six patients presenting with acute symptomatic basilar thrombosis. J Neurointerv Surg. 2014;6:379–83.
Hacke W, Zeumer H, Ferbert A, Bruckmann H, del Zoppo GJ. Intra-arterial thrombolytic therapy improves outcome in patients with acute vertebrobasilar occlusive disease. Stroke. 1988;19:1216–22.
Brandt T, von Kummer R, Muller-Kuppers M, Hacke W. Thrombolytic therapy of acute basilar artery occlusion. Variables affecting recanalization and outcome. Stroke. 1996;27:875–81.
Voetsch B, DeWitt LD, Pessin MS, Caplan LR. Basilar artery occlusive disease in the New England Medical Center Posterior Circulation Registry. Arch Neurol. 2004;61:496–504.
Kim YW, Hong JM, Park DG, Choi JW, Kang DH, Kim YS, et al. Effect of intracranial atherosclerotic disease on endovascular treatment for patients with acute vertebrobasilar occlusion. AJNR Am J Neuroradiol. 2016;37:2072–8.
Eckert B, Kucinski T, Pfeiffer G, Groden C, Zeumer H. Endovascular therapy of acute vertebrobasilar occlusion: early treatment onset as the most important factor. Cerebrovasc Dis. 2002;14:42–50.
Lee JS, Lee SJ, Yoo JS, Hong JH, Kim CH, Kim YW, et al. Prognosis of acute intracranial atherosclerosis-related occlusion after endovascular treatment. J Stroke. 2018;20:394–403.
Wang Y, Zhao X, Liu L, Soo YO, Pu Y, Pan Y, et al. Prevalence and outcomes of symptomatic intracranial large artery stenoses and occlusions in China: the Chinese Intracranial Atherosclerosis (CICAS) Study. Stroke. 2014;45:663–9.
Huang YN, Gao S, Li SW, Huang Y, Li JF, Wong KS, et al. Vascular lesions in Chinese patients with transient ischemic attacks. Neurology. 1997;48:524–5.
Mattioni A, Cenciarelli S, Biessels G, van Seeters T, Algra A, Ricci S. Prevalence of intracranial large artery stenosis and occlusion in patients with acute ischaemic stroke or TIA. Neurol Sci. 2014;35:349–55.
De Silva DA, Woon FP, Lee MP, Chen CP, Chang HM, Wong MC. South Asian patients with ischemic stroke: intracranial large arteries are the predominant site of disease. Stroke. 2007;38:2592–4.
Baik SH, Park HJ, Kim JH, Jang CK, Kim BM, Kim DJ. Mechanical thrombectomy in subtypes of basilar artery occlusion: relationship to recanalization rate and clinical outcome. Radiology. 2019;291:730–7.
Gao F, Lo WT, Sun X, Mo DP, Ma N, Miao ZR. Combined use of mechanical thrombectomy with angioplasty and stenting for acute basilar occlusions with underlying severe intracranial vertebrobasilar stenosis: preliminary experience from a single Chinese center. AJNR Am J Neuroradiol. 2015;36:1947–52.
Funding
Beijing Municipal Science and Technology Commision (Z18110000171837) and the National Key Research and Development Program of China (2016YFC1301501) funded the current study.
Author information
Authors and Affiliations
Contributions
XS, XT, YMD, GTM, LGS, LL, and XCH acquired the data. ZRM, NM, and FG were involved in the study design and data interpretation. XS and R drafted the article. XT conducted the statistical analysis. All authors commented on the manuscript regarding the intellectual content.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interests.
Ethics Approval
This study was reviewed and approved by our Institutional Review Board and procedures followed were in accordance with the institutional guidelines and the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(DOCX 37 kb)
Rights and permissions
About this article
Cite this article
Sun, X., Raynald, Tong, X. et al. Analysis of Treatment Outcome After Endovascular Treatment in Different Pathological Subtypes of Basilar Artery Occlusion: a Single Center Experience. Transl. Stroke Res. 12, 230–238 (2021). https://doi.org/10.1007/s12975-020-00833-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-020-00833-w