Abstract
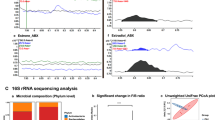
Our previous work has shown that reproductively senescent (or middle-aged; 10–12-month-old) Sprague–Dawley female rats, that are naturally estrogen-deficient, have worse stroke outcomes as compared to normally estrous-cycling adult (5–6-month-old) females. Paradoxically, estrogen replacement to this middle-aged group exacerbates stroke outcomes, while it is neuroprotective in adult females. Recent studies reveal an important role for the gut microbiome and gut metabolites in cardiovascular health, including stroke outcomes. To determine whether gut dysbiosis underlies stroke severity in reproductive senescent females, and underlies the anomalous effects of estrogen on stroke, we compared the gut microbiota and gut metabolites pre and post stroke in (a) gonadally intact adult and middle-aged females, (b) in ovariectomized and estrogen-treated (OVX+E) adult and OVX+E middle-aged females, and (c) in middle-aged OVX+E females after fecal microbiome transfer. Our data show significant gut dysbiosis in reproductive senescent females at baseline and after stroke as indicated by an elevated ratio of the major phyla, Firmicutes/Bacteroidetes (F:B), reduced alpha diversity, and significant shifts in beta diversity as compared with adult females. Specific bacterial families were also altered as a result of reproductive aging, as well as gut metabolites, including elevated serum endotoxin levels and decreased short-chain fatty acids (SCFAs), with a concomitant increase in IL-17A, indicating that reproductive senescence significantly affects gut communities under pathologic conditions. Despite the differences in gonadally intact adult and middle-aged females, estrogen-treated ovariectomized (OVX+E) females of either age group displayed no differences in the major phyla, but there was increased abundance in specific bacterial taxa, including Prevotella and Lactobacillus. The SCFA butyrate was significantly reduced at baseline in the middle-aged OVX+E females, while circulating endotoxin LPS were elevated in this group after stroke, suggesting that gut metabolites were differently affected by estrogen treatment in the two age groups. A fecal transfer from adult OVX+E females to middle-aged OVX+E females significantly reduced infarct volume, improved behavioral recovery and transiently reduced IL-17A expression. These data provide the first evidence that microbial gut communities and metabolites are altered by reproductive senescence in female rats at baseline and after stroke, and suggest that estrogen may impact stroke recovery differently in adult and reproductive senescent females due to an age-specific effect on gut microbiota and metabolites.











Similar content being viewed by others
Change history
27 January 2022
A Correction to this paper has been published: https://doi.org/10.1007/s12975-022-00990-0
References
Reeves MJ, Bushnell CD, Howard G, Gargano JW, Duncan PW, Lynch G, et al. Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol. 2008;7(10):915–26.
Wassertheil-Smoller S, Hendrix SL, Limacher M, Heiss G, Kooperberg C, Baird A, et al. Effect of estrogen plus progestin on stroke in postmenopausal women: the Women's Health Initiative: a randomized trial. Jama. 2003;289(20):2673–84.
Selvamani A, Sohrabji F. Reproductive age modulates the impact of focal ischemia on the forebrain as well as the effects of estrogen treatment in female rats. Neurobiol Aging. 2010;31(9):1618–28.
Leon RL, Li X, Huber JD, Rosen CL. Worsened outcome from middle cerebral artery occlusion in aged rats receiving 17beta-estradiol. Endocrinology. 2012;153(7):3386–93.
Liu F, Benashski SE, Xu Y, Siegel M, McCullough L. Effects of chronic and acute oestrogen replacement therapy in aged animals after experimental stroke. J Neuroendocrinol. 2012;24(2):319–30.
Butto LF, Haller D. Dysbiosis in intestinal inflammation: cause or consequence. Int J Med Microbiol. 2016;306(5):302–9.
Brunkwall L, Orho-Melander M. The gut microbiome as a target for prevention and treatment of hyperglycaemia in type 2 diabetes: from current human evidence to future possibilities. Diabetologia. 2017;60(6):943–51.
Mayer EA, Knight R, Mazmanian SK, Cryan JF, Tillisch K. Gut microbes and the brain: paradigm shift in neuroscience. J Neurosci. 2014;34(46):15490–6.
Scheperjans F, Aho V, Pereira PA, Koskinen K, Paulin L, Pekkonen E, et al. Gut microbiota are related to Parkinson's disease and clinical phenotype. Mov Disord. 2015;30(3):350–8.
Yin, J., et al., Dysbiosis of gut microbiota with reduced trimethylamine-N-oxide level in patients with large-artery atherosclerotic stroke or transient ischemic attack. J Am Heart Assoc, 2015. 4(11).
Singh V, Roth S, Llovera G, Sadler R, Garzetti D, Stecher B, et al. Microbiota dysbiosis controls the neuroinflammatory response after stroke. J Neurosci. 2016;36(28):7428–40.
Houlden A, et al. Brain injury induces specific changes in the caecal microbiota of mice via altered autonomic activity and mucoprotein production. Brain Behav Immun. 2016;57:10–20.
Benakis C, Brea D, Caballero S, Faraco G, Moore J, Murphy M, et al. Commensal microbiota affects ischemic stroke outcome by regulating intestinal gammadelta T cells. Nat Med. 2016;22(5):516–23.
Spychala MS, Venna VR, Jandzinski M, Doran SJ, Durgan DJ, Ganesh BP, et al. Age-related changes in the gut microbiota influence systemic inflammation and stroke outcome. Ann Neurol. 2018;84(1):23–36.
Chen KL, Madak-Erdogan Z. Estrogen and microbiota crosstalk: should we pay attention? Trends Endocrinol Metab. 2016;27(11):752–5.
Baker JM, Al-Nakkash L, Herbst-Kralovetz MM. Estrogen-gut microbiome axis: physiological and clinical implications. Maturitas. 2017;103:45–53.
Blasco-Baque V, Serino M, Vergnes JN, Riant E, Loubieres P, Arnal JF, et al. High-fat diet induces periodontitis in mice through lipopolysaccharides (LPS) receptor signaling: protective action of estrogens. PLoS One. 2012;7(11):e48220.
Benedek G, Zhang J, Nguyen H, Kent G, Seifert HA, Davin S, et al. Estrogen protection against EAE modulates the microbiota and mucosal-associated regulatory cells. J Neuroimmunol. 2017;310:51–9.
Murphy K, Keller MJ, Anastos K, Sinclair S, Devlin JC, Shi Q, et al. Impact of reproductive aging on the vaginal microbiome and soluble immune mediators in women living with and at-risk for HIV infection. PLoS One. 2019;14(4):e0216049.
Santos-Marcos JA, Rangel-Zuñiga OA, Jimenez-Lucena R, Quintana-Navarro GM, Garcia-Carpintero S, Malagon MM, et al. Influence of gender and menopausal status on gut microbiota. Maturitas. 2018;116:43–53.
Vieira AT, et al. Influence of oral and gut microbiota in the health of menopausal women. Front Microbiol. 2017;8:1884.
Selvamani A, Sohrabji F. Mir363-3p improves ischemic stroke outcomes in female but not male rats. Neurochem Int. 2017;107:168–81.
Selvamani A, Sohrabji F. The neurotoxic effects of estrogen on ischemic stroke in older female rats is associated with age-dependent loss of IGF-1. J Neurosci. 2010;30(20):6852–61.
Jezierski M, Sohrabji F. Neurotrophin expression in the reproductively senescent forebrain is refractory to estrogen stimulation. Neurobiol Aging. 2001;22(2):311–21.
Bake S, Sohrabji F. 17beta-estradiol differentially regulates blood-brain barrier permeability in young and aging female rats. Endocrinology. 2004;145(12):5471–5.
Selvamani A, Sohrabji F. The neurotoxic effects of estrogen on ischemic stroke in older female rats is associated with age-dependent loss of insulin-like growth factor-1. J Neurosci. 2010;30(20):6852–61.
Jezierski MK, Sohrabji F. Estrogen enhances retrograde transport of brain-derived neurotrophic factor in the rodent forebrain. Endocrinology. 2003;144(11):5022–9.
Jezierski MK, Sohrabji F. Region- and peptide-specific regulation of the neurotrophins by estrogen. Brain Res Mol Brain Res. 2000;85(1–2):77–84.
Biernaskie J, et al. A serial MR study of cerebral blood flow changes and lesion development following endothelin-1-induced ischemia in rats. Magn Reson Med. 2001;46(4):827–30.
Park MJ, Sohrabji F. The histone deacetylase inhibitor, sodium butyrate, exhibits neuroprotective effects for ischemic stroke in middle-aged female rats. J Neuroinflammation. 2016;13(1):300.
Selvamani A, et al. Circulating miRNA profiles provide a biomarker for severity of stroke outcomes associated with age and sex in a rat model. Clin Sci (Lond). 2014;127(2):77–89.
Okoreeh, A.K., S. Bake, and F. Sohrabji, Astrocyte-specific insulin-like growth factor-1 gene transfer in aging female rats improves stroke outcomes. Glia, 2017.
Caporaso JG, et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods. 2010;7(5):335–6.
Parada AE, Needham DM, Fuhrman JA. Every base matters: assessing small subunit rRNA primers for marine microbiomes with mock communities, time series and global field samples. Environ Microbiol. 2016;18(5):1403–14.
Apprill A, et al. Minor revision to V4 region SSU rRNA 806R gene primer greatly increases detection of SAR11 bacterioplankton. Aquat Microb Ecol. 2015;75(2):129–37.
Isaiah A, et al. The fecal microbiome of dogs with exocrine pancreatic insufficiency. Anaerobe. 2017;45:50–8.
Edgar RC. Search and clustering orders of magnitude faster than BLAST. Bioinformatics. 2010;26(19):2460–1.
DeSantis TZ, et al. Greengenes, a chimera-checked 16S rRNA gene database and workbench compatible with ARB. Appl Environ Microbiol. 2006;72(7):5069–72.
Langille MG, Zaneveld J, Caporaso JG, McDonald D, Knights D, Reyes JA, et al. Predictive functional profiling of microbial communities using 16S rRNA marker gene sequences. Nat Biotechnol. 2013;31(9):814–21.
Bolyen E, Rideout JR, Dillon MR, Bokulich NA, Abnet CC, al-Ghalith GA, et al. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat Biotechnol. 2019;37(8):852–7.
Callahan BJ, McMurdie P, Rosen MJ, Han AW, Johnson AJ, Holmes SP. DADA2: high-resolution sample inference from Illumina amplicon data. Nat Methods. 2016;13(7):581–3.
Douglas, G.M., et al., PICRUSt2: an improved and extensible approach for metagenome inference. 2019.
Lozupone C, Knight R. UniFrac: a new phylogenetic method for comparing microbial communities. Appl Environ Microbiol. 2005;71(12):8228–35.
Bake S, Selvamani A, Cherry J, Sohrabji F. Blood brain barrier and neuroinflammation are critical targets of IGF-1-mediated Neuroprotection in stroke for middle-aged female rats. PLoS One. 2014;9(3):e91427.
Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Royal Stat Socs Series B (Methodological). 1995:289–300.
Sun J, et al. IL-17A is implicated in lipopolysaccharide-induced neuroinflammation and cognitive impairment in aged rats via microglial activation. J Neuroinflammation. 2015;12(1):165.
Patnala R, Arumugam TV, Gupta N, Dheen ST. HDAC inhibitor sodium butyrate-mediated epigenetic regulation enhances neuroprotective function of microglia during ischemic stroke. Mol Neurobiol. 2017;54(8):6391–411.
Cespedes Rubio AE, et al. Sex steroid hormones as neuroprotective elements in ischemia models. J Endocrinol. 2018;237(2):R65–r81.
Tanaka M, et al. Progesterone improves functional outcomes after transient focal cerebral ischemia in both aged male and female rats. Exp Gerontol. 2018;113:29–35.
Alkayed NJ, et al. Gender-linked brain injury in experimental stroke. Stroke. 1998;29(1):159–65 discussion 166.
Braniste V, et al. The gut microbiota influences blood-brain barrier permeability in mice. Sci Transl Med. 2014;6(263):263ra158.
Erny D, Hrabě AL, de Angelis H, Prinz M. Communicating systems in the body: how microbiota and microglia cooperate. Immunology. 2017;150(1):7–15.
Lach G, Schellekens H, Dinan TG, Cryan JF. Anxiety, depression, and the microbiome: a role for gut peptides. Neurotherapeutics. 2018;15(1):36–59.
Li W, et al. Memory and learning behavior in mice is temporally associated with diet-induced alterations in gut bacteria. Physiol Behav. 2009;96(4–5):557–67.
Kang DW, Park JG, Ilhan ZE, Wallstrom G, Labaer J, Adams JB, et al. Reduced incidence of Prevotella and other fermenters in intestinal microflora of autistic children. PLoS One. 2013;8(7):e68322.
Vogt NM, et al. Gut microbiome alterations in Alzheimer’s disease. Sci Rep. 2017;7(1):13537.
Arumugam M, et al. Enterotypes of the human gut microbiome. Nature. 2011;473(7346):174–80.
Al-Bayati AR, et al. Thiamine deficiency presenting as intraventricular hemorrhage. Stroke. 2016;47(6):e95–7.
Blum A, Ovadia M, Rosen G, Simsolo C. Immediate recovery of “anischemic stroke” following treatment with intravenous thiamine (vitamin B1). Isr Med Assoc J. 2014;16(8):518–9.
Giles WH, et al. Serum folate and risk for ischemic stroke. First national health and nutrition examination survey epidemiologic follow-up study. Stroke. 1995;26(7):1166–70.
Endres M, Ahmadi M, Kruman I, Biniszkiewicz D, Meisel A, Gertz K. Folate deficiency increases postischemic brain injury. Stroke. 2005;36(2):321–5.
Poole KE, Loveridge N, Barker PJ, Halsall DJ, Rose C, Reeve J, et al. Reduced vitamin D in acute stroke. Stroke. 2006;37(1):243–5.
Perez-Pardo P, et al. The gut-brain axis in Parkinson's disease: possibilities for food-based therapies. Eur J Pharmacol. 2017;817:86–95.
Brown CT, et al. Gut microbiome metagenomics analysis suggests a functional model for the development of autoimmunity for type 1 diabetes. PLoS One. 2011;6(10):e25792.
Forsyth CB, Shannon KM, Kordower JH, Voigt RM, Shaikh M, Jaglin JA, et al. Increased intestinal permeability correlates with sigmoid mucosa alpha-synuclein staining and endotoxin exposure markers in early Parkinson's disease. PLoS One. 2011;6(12):e28032.
Plovier H, Everard A, Druart C, Depommier C, van Hul M, Geurts L, et al. A purified membrane protein from Akkermansia muciniphila or the pasteurized bacterium improves metabolism in obese and diabetic mice. Nat Med. 2017;23(1):107–13.
Everard A, et al. Cross-talk between Akkermansia muciniphila and intestinal epithelium controls diet-induced obesity. Proc Natl Acad Sci. 2013;110(22):9066–71.
Cani PD, Everard A. Akkermansia muciniphila: a novel target controlling obesity, type 2 diabetes and inflammation? Med Sci (Paris). 2014;30(2):125–7.
Li, J., et al., Akkermansia muciniphila protects against atherosclerosis by preventing metabolic endotoxemia-induced inflammation in Apoe-/-mice. Circulation, 2016: p. CIRCULATIONAHA. 115.019645.
Stanley D, Moore RJ, Wong CH. An insight into intestinal mucosal microbiota disruption after stroke. Sci Rep. 2018;8(1):568.
Reunanen J, et al. Akkermansia muciniphila adheres to enterocytes and strengthens the integrity of the epithelial cell layer. Appl Environ Microbiol. 2015;81(11):3655–62.
Derrien M, Vaughan EE, Plugge CM, de Vos WM. Akkermansia muciniphila gen. nov., sp. nov., a human intestinal mucin-degrading bacterium. Int J Syst Evol Microbiol. 2004;54(Pt 5):1469–76.
Derrien M, Collado MC, Ben-Amor K, Salminen S, de Vos WM. The mucin degrader Akkermansia muciniphila is an abundant resident of the human intestinal tract. Appl Environ Microbiol. 2008;74(5):1646–8.
Larson TA. Sex steroids, adult neurogenesis, and inflammation in CNS homeostasis, degeneration, and repair. Front Endocrinol. 2018;9:205.
Yurkovetskiy L, Burrows M, Khan AA, Graham L, Volchkov P, Becker L, et al. Gender bias in autoimmunity is influenced by microbiota. Immunity. 2013;39(2):400–12.
Plottel CS, Blaser MJ. Microbiome and malignancy. Cell Host Microbe. 2011;10(4):324–35.
Kwa, M., et al., The intestinal microbiome and estrogen receptor-positive female breast cancer. J Natl Cancer Inst, 2016. 108(8).
Moens F, Verce M, De Vuyst L. Lactate- and acetate-based cross-feeding interactions between selected strains of lactobacilli, bifidobacteria and colon bacteria in the presence of inulin-type fructans. Int J Food Microbiol. 2017;241:225–36.
Bennet J, Brinkman M. Treatment of ULCERATIVE colitis by implantation of normal colonic FLORA. Lancet. 1989;333(8630):164.
Tian Z, Liu J, Liao M, Li W, Zou J, Han X, et al. Beneficial effects of fecal microbiota transplantation on ulcerative colitis in mice. Dig Dis Sci. 2016;61(8):2262–71.
Couturier-Maillard A, Secher T, Rehman A, Normand S, de Arcangelis A, Haesler R, et al. NOD2-mediated dysbiosis predisposes mice to transmissible colitis and colorectal cancer. J Clin Invest. 2013;123(2):700–11.
Cruz-Aguliar RM, et al. An open-labeled study on fecal microbiota transfer in irritable bowel syndrome patients reveals improvement in abdominal pain associated with the relative abundance of Akkermansia Muciniphila. Digestion. 2018:1–12.
Bromberg, J.S., et al., Gut microbiota-dependent modulation of innate immunity and lymph node remodeling affects cardiac allograft outcomes. JCI Insight, 2018. 3(19).
Malkki H. Stroke: gut microbiota influence stroke recovery in mice. Nat Rev Neurol. 2016;12(5):252.
Sun J, Wang F, Ling Z, Yu X, Chen W, Li H, et al. Clostridium butyricum attenuates cerebral ischemia/reperfusion injury in diabetic mice via modulation of gut microbiota. Brain Res. 2016;1642:180–8.
den Besten G, et al. The role of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism. J Lipid Res. 2013;54(9):2325–40.
Andoh A, Tsujikawa T, Fujiyama Y. Role of dietary fiber and short-chain fatty acids in the colon. Curr Pharm Des. 2003;9(4):347–58.
Huuskonen J, Suuronen T, Nuutinen T, Kyrylenko S, Salminen A. Regulation of microglial inflammatory response by sodium butyrate and short-chain fatty acids. Br J Pharmacol. 2004;141(5):874–80.
Valapour M, Guo J, Schroeder JT, Keen J, Cianferoni A, Casolaro V, et al. Histone deacetylation inhibits IL4 gene expression in T cells. J Allergy Clin Immunol. 2002;109(2):238–45.
Fu X, Wang X, Duan Z, Zhang C, Fu X, Yang J, et al. Histone H3k9 and H3k27 acetylation regulates IL-4/STAT6-mediated Igepsilon transcription in B lymphocytes. Anat Rec (Hoboken). 2015;298(8):1431–9.
Zhang M, Zhou Q, Dorfman RG, Huang X, Fan T, Zhang H, et al. Butyrate inhibits interleukin-17 and generates Tregs to ameliorate colorectal colitis in rats. BMC Gastroenterol. 2016;16(1):84.
Shekhar S, Cunningham MW, Pabbidi MR, Wang S, Booz GW, Fan F. Targeting vascular inflammation in ischemic stroke: recent developments on novel immunomodulatory approaches. Eur J Pharmacol. 2018;833:531–44.
Chen R, et al. Transplantation of fecal microbiota rich in short chain fatty acids and butyric acid treat cerebral ischemic stroke by regulating gut microbiota. Pharmacol Res. 2019;148:104403.
Acknowledgments
The authors thank Yumna El-Hakim, Dr. Amanda Mahnke and Dr. Rajesh Miranda for careful reading and comments. Dr. Park’s current address: Brain Research Institute, Department of Otolaryngology-Head and Neck Surgery, College of Medicine, Chungnam National University, Daejeon, Republic of Korea.
Funding
This study was supported by funding from NIH/NS074895 and AG042189 to FS.
Author information
Authors and Affiliations
Contributions
MJP and RP are co-first authors. MJP: conceptualized/hypothesized, designed, performed the experiments; analyzed data and prepared figures; and wrote the manuscript. RP: performed metagenomic analyses, assisted with data interpretation, prepared figures, and wrote the manuscript. BS: assisted with metagenomic analysis. AP: performed the FMT experiments. SP: assisted with experiments and performed behavioral tests. JS: assisted with experimental design and data interpretation. FS: refined hypothesis and experimental design, data analysis and interpretation, and wrote the manuscript.
Corresponding author
Ethics declarations
All experimental protocols were approved by Texas A&M University Institutional Animal Care and Use Committee. All animal care and use was conducted in accordance with the Guide for the Care and Use of Laboratory Animals (National Research Council).
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary Fig. 1
Reproductive aging affects behavioral outcomes after stroke. The latency (in seconds) to tape removal from the forepaw was evaluated by the adhesive tape test before (pre) or after (2d and 5d) MCAO. Post-stroke performance in both adult and middle-aged animals was not significantly impaired in the ipsilesional forepaw. a. In adult females, there was no detectable change in latency due to stroke. b. In middle-aged females, latency for adhesive removal was severely affected on the contralesional side after stroke. N = 5, All graphs represent mean ± S.E.M. a, main effect of side, p < 0.0001; b, main effect of stroke, p = 0.0028; c, interaction, p = 0.015. Key: Ipsi: ipsilesional paw, contra: contralesional paw. (PNG 519 kb)
Supplementary Fig. 2
Estrogen replacement to ovariectomized adult and middle-aged females. a. Estrogen replacement (OVX + E) to ovariectomized females significantly increased uterine weight as compared to ovariectomized (OVX) females in both adult and middle-aged female groups. b. Normalized feed consumption was similar in adult and middle-aged rats. a: main effect of treatment. (PNG 396 kb)
Supplementary Fig 3
The latency (in seconds) to tape removal from the forepaw was evaluated by the adhesive tape test before (0 day) or after (2 days and 5 days) MCAO. Post-stroke performance in both adult and middle-aged animals was not significantly impaired in the ipsilesional forepaw a. In adult females, both OVX + Placebo and OVX + Estrogen groups displayed a significant increase in latency on the contralesional paw after stroke, however at 5d after stroke latency in both groups was lower than at 2d after stroke. b. In middle-aged females, both OVX + Placebo and OVX + Estrogen groups displayed a significant increase in latency on the contralesional paw after stroke, however there was no improvement in latency between 2d and 5d in either group. Key: Ipsi: ipsilesional paw, contra: contralesional paw, OVX + Pl: ovariectomized with placebo pellet, OVX + E: ovariectomized with estradiol pellet. All graphs represent mean ± S.E.M. * p < 0.05; ns: not significant. (PNG 632 kb)
Supplementary Fig. 4
Timeline for procedures related to the Fecal Microbiome Transfer study. OVX + E: ovariectomized females treated with estrogen, MCAo: middle cerebral artery occlusion. (PNG 306 kb)
ESM 1
(XLSX 34 kb)
ESM 2
(XLSX 33 kb)
ESM 3
(XLSX 33 kb)
ESM 4
(XLSX 33 kb)
ESM 5
(XLSX 33 kb)
ESM 6
(XLSX 34 kb)
ESM 7
(XLSX 54 kb)
ESM 8
(XLSX 31 kb)
ESM 9
(XLSX 35 kb)
ESM 10
(XLSX 18 kb)
ESM 11
(XLSX 17 kb)
Rights and permissions
About this article
Cite this article
Park, M.J., Pilla, R., Panta, A. et al. Reproductive Senescence and Ischemic Stroke Remodel the Gut Microbiome and Modulate the Effects of Estrogen Treatment in Female Rats. Transl. Stroke Res. 11, 812–830 (2020). https://doi.org/10.1007/s12975-019-00760-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-019-00760-5