Abstract
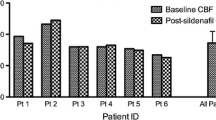
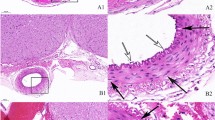
The poor prognosis of subarachnoid hemorrhage (SAH) might be associated with sympathetic nerve activation (catecholamine surge) initiated by hypothalamic injury. As renal denervation (RD) has been shown to exert protective effects on cardiovascular dysfunction by suppressing increased central sympathetic nerve activation, we examined whether RD improved the experimental SAH prognosis in this study. Two hundred thirty-eight male Sprague-Dawley rats were divided into sham-operated and SAH-operated groups, and then each rat was further separated into Sham-operated and RD-operated groups. Bilateral RD was performed approximately 45 min after SAH induction. We examined the effect of RD on early brain injury (EBI) and delayed cerebral ischemia (DCI) as a primary endpoint, and also explored the effect on cerebral vasospasm (CVS) as a secondary endpoint. Although RD did not exert significant effects on primary endpoint, RD significantly prevented CVS and reduced SAH-induced increases in the number of phosphorylated extracellular signal-regulated kinase (ERK)-positive endothelial cells, cyclooxygenase-2 expression, and macrophage infiltration in major cerebral arteries. Moreover, RD significantly decreased the areas displaying dopamine β-hydroxylase and glial fibrillary acidic protein immunopositivity in the paraventricular nucleus of the hypothalamus and serum angiotensin II levels, all of which were increased by SAH. Although RD decreased systolic blood pressure, significant changes in cerebral blood flow were not observed compared with SAH + Sham group. Based on the findings, RD improved CVS by reducing endothelial cell damage and the effects were associated with the stabilization of central sympathetic nerve activation in a SAH model.








Similar content being viewed by others
References
Macdonald RL. Delayed neurological deterioration after subarachnoid haemorrhage. Nat Rev Neurol. 2014;10(1):44–58. https://doi.org/10.1038/nrneurol.2013.246.
Caner B, Hou J, Altay O, Fujii M, Zhang JH. Transition of research focus from vasospasm to early brain injury after subarachnoid hemorrhage. J Neurochem. 2012;123(Suppl 2):12–21. https://doi.org/10.1111/j.1471-4159.2012.07939.x.
Shimamura N, Ohkuma H. Phenotypic transformation of smooth muscle in vasospasm after aneurysmal subarachnoid hemorrhage. Transl Stroke Res. 2014;5(3):357–64. https://doi.org/10.1007/s12975-013-0310-1.
Takemoto Y, Hasegawa Y, Hashiguchi A, Moroki K, Tokuda H, Mukasa A. Predictors for functional outcome in patients with aneurysmal subarachnoid hemorrhage who completed in-hospital rehabilitation in a single institution. J Stroke Cerebrovasc Dis. 2019;28(7):1943–50. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.03.042.
Chen S, Li Q, Wu H, Krafft PR, Wang Z, Zhang JH. The harmful effects of subarachnoid hemorrhage on extracerebral organs. Biomed Res Int. 2014;2014:858496. https://doi.org/10.1155/2014/858496.
Lee VH, Oh JK, Mulvagh SL, Wijdicks EF. Mechanisms in neurogenic stress cardiomyopathy after aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2006;5(3):243–9. https://doi.org/10.1385/ncc:5:3:243.
Naredi S, Lambert G, Eden E, Zall S, Runnerstam M, Rydenhag B, et al. Increased sympathetic nervous activity in patients with nontraumatic subarachnoid hemorrhage. Stroke. 2000;31(4):901–6.
Gao C, Liu X, Shi H, Xu S, Ji Z, Wang C, et al. Relationship between sympathetic nervous activity and inflammatory response after subarachnoid hemorrhage in a perforating canine model. Auton Neurosci. 2009;147(1–2):70–4. https://doi.org/10.1016/j.autneu.2009.01.010.
Cameron MM, Haas RH. Adrenergic blockade in subarachnoid haemorrhage. Acta Neurochir. 1976;34(1–4):261–4.
Lambert G, Naredi S, Eden E, Rydenhag B, Friberg P. Sympathetic nervous activation following subarachnoid hemorrhage: influence of intravenous clonidine. Acta Anaesthesiol Scand. 2002;46(2):160–5.
Esler MD, Krum H, Sobotka PA, Schlaich MP, Schmieder RE, Bohm M. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet. 2010;376(9756):1903–9. https://doi.org/10.1016/s0140-6736(10)62039-9.
Hering D, Lambert EA, Marusic P, Walton AS, Krum H, Lambert GW, et al. Substantial reduction in single sympathetic nerve firing after renal denervation in patients with resistant hypertension. Hypertension. 2013;61(2):457–64. https://doi.org/10.1161/hypertensionaha.111.00194.
Bhatt DL, Kandzari DE, O'Neill WW, D'Agostino R, Flack JM, Katzen BT, et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med. 2014;370(15):1393–401. https://doi.org/10.1056/NEJMoa1402670.
Frame AA, Carmichael CY, Wainford RD. Renal afferents. Curr Hypertens Rep. 2016;18(9):69–7. https://doi.org/10.1007/s11906-016-0676-z.
Schlaich MP, Krum H, Sobotka PA, Esler MD. Renal denervation and hypertension. Am J Hypertens. 2011;24(6):635–42. https://doi.org/10.1038/ajh.2011.35.
Campese VM, Ye S, Zhong H. Downregulation of neuronal nitric oxide synthase and interleukin-1beta mediates angiotensin II-dependent stimulation of sympathetic nerve activity. Hypertension. 2002;39(2 Pt 2):519–24.
Campese VM, Shaohua Y, Huiquin Z. Oxidative stress mediates angiotensin II-dependent stimulation of sympathetic nerve activity. Hypertension. 2005;46(3):533–9. https://doi.org/10.1161/01.hyp.0000179088.57586.26.
Nakagawa T, Hasegawa Y, Uekawa K, Ma M, Katayama T, Sueta D, et al. Renal denervation prevents stroke and brain injury via attenuation of oxidative stress in hypertensive rats. J Am Heart Assoc. 2013;2(5):e000375. https://doi.org/10.1161/jaha.113.000375.
Hasegawa Y, Nakagawa T, Matsui K, Kim-Mitsuyama S. Renal denervation in the acute phase of ischemic stroke provides brain protection in hypertensive rats. Stroke. 2017;48(4):1104–7. https://doi.org/10.1161/strokeaha.116.015782.
Bederson JB, Germano IM, Guarino L. Cortical blood flow and cerebral perfusion pressure in a new noncraniotomy model of subarachnoid hemorrhage in the rat. Stroke. 1995;26(6):1086–91; discussion 91-2. https://doi.org/10.1161/01.str.26.6.1086.
Endo H, Nito C, Kamada H, Yu F, Chan PH. Akt/GSK3beta survival signaling is involved in acute brain injury after subarachnoid hemorrhage in rats. Stroke. 2006;37(8):2140–6. https://doi.org/10.1161/01.str.0000229888.55078.72.
Hasegawa Y, Suzuki H, Altay O, Zhang JH. Preservation of tropomyosin-related kinase B (TrkB) signaling by sodium orthovanadate attenuates early brain injury after subarachnoid hemorrhage in rats. Stroke. 2011;42(2):477–83. https://doi.org/10.1161/strokeaha.110.597344.
Kamp MA, Lieshout JHV, Dibue-Adjei M, Weber JK, Schneider T, Restin T, et al. A systematic and meta-analysis of mortality in experimental mouse models analyzing delayed cerebral ischemia after subarachnoid hemorrhage. Transl Stroke Res. 2017;8(3):206–19. https://doi.org/10.1007/s12975-016-0513-3.
Hasegawa Y, Suzuki H, Uekawa K, Kawano T, Kim-Mitsuyama S. Characteristics of cerebrovascular injury in the hyperacute phase after induced severe subarachnoid hemorrhage. Transl Stroke Res. 2015;6(6):458–66. https://doi.org/10.1007/s12975-015-0423-9.
Hasegawa Y, Uekawa K, Kawano T, Suzuki H, Kim-Mitsuyama S. Blockage of central sphingosine-1-phosphate receptor does not abolish the protective effect of FTY720 in early brain injury after experimental subarachnoid hemorrhage. Curr Drug Deliv. 2017;14(6):861–6. https://doi.org/10.2174/1567201813666160907094401.
Hasegawa Y, Nakagawa T, Uekawa K, Ma M, Lin B, Kusaka H, et al. Therapy with the combination of amlodipine and irbesartan has persistent preventative effects on stroke onset associated with BDNF preservation on cerebral vessels in hypertensive rats. Transl Stroke Res. 2016;7(1):79–87. https://doi.org/10.1007/s12975-014-0383-5.
Dong YF, Kataoka K, Tokutomi Y, Nako H, Nakamura T, Toyama K, et al. Beneficial effects of combination of valsartan and amlodipine on salt-induced brain injury in hypertensive rats. J Pharmacol Exp Ther. 2011;339(2):358–66. https://doi.org/10.1124/jpet.111.182576.
Sugawara T, Ayer R, Jadhav V, Zhang JH. A new grading system evaluating bleeding scale in filament perforation subarachnoid hemorrhage rat model. J Neurosci Methods. 2008;167(2):327–34. https://doi.org/10.1016/j.jneumeth.2007.08.004.
Wu CH, Chi JC, Jerng JS, Lin SJ, Jan KM, Wang DL, et al. Transendothelial macromolecular transport in the aorta of spontaneously hypertensive rats. Hypertension. 1990;16(2):154–61. https://doi.org/10.1161/01.hyp.16.2.154.
Hasegawa Y, Suzuki H, Sozen T, Rolland W, Zhang JH. Activation of sphingosine 1-phosphate receptor-1 by FTY720 is neuroprotective after ischemic stroke in rats. Stroke. 2010;41(2):368–74. https://doi.org/10.1161/strokeaha.109.568899.
Suzuki H, Hasegawa Y, Chen W, Kanamaru K, Zhang JH. Recombinant osteopontin in cerebral vasospasm after subarachnoid hemorrhage. Ann Neurol. 2010;68(5):650–60. https://doi.org/10.1002/ana.22102.
Fassot C, Lambert G, Gaudet-Lambert E, Friberg P, Elghozi JL. Beneficial effect of renin-angiotensin system for maintaining blood pressure control following subarachnoid haemorrhage. Brain Res Bull. 1999;50(2):127–32.
Howe PR, Rogers PF, Morris MJ, Chalmers JP, Smith RM. Plasma catecholamines and neuropeptide-Y as indices of sympathetic nerve activity in normotensive and stroke-prone spontaneously hypertensive rats. J Cardiovasc Pharmacol. 1986;8(6):1113–21.
Kishi T, Hirooka Y, Kimura Y, Ito K, Shimokawa H, Takeshita A. Increased reactive oxygen species in rostral ventrolateral medulla contribute to neural mechanisms of hypertension in stroke-prone spontaneously hypertensive rats. Circulation. 2004;109(19):2357–62. https://doi.org/10.1161/01.cir.0000128695.49900.12.
Hansen-Schwartz J. Cerebral vasospasm: a consideration of the various cellular mechanisms involved in the pathophysiology. Neurocrit Care. 2004;1(2):235–46. https://doi.org/10.1385/ncc:1:2:235.
Luo H, Song WX, Jiang JW, Zhao JL, Rong WL, Li MH. Effects of preadmission beta-blockers on neurogenic stunned myocardium after aneurysmal subarachnoid hemorrhage: a meta- analysis. Clin Neurol Neurosurg. 2017;158:77–81. https://doi.org/10.1016/j.clineuro.2017.04.022.
Schebesch KM, Brawanski A, Kagerbauer SM, Martin J, Bele S, Herbst A, et al. The possible role of neuropeptide Y after spontaneous subarachnoid hemorrhage. Acta Neurochir. 2011;153(8):1663–8; discussion 8. https://doi.org/10.1007/s00701-011-1056-8.
Audibert G, Steinmann G, de Talance N, Laurens MH, Dao P, Baumann A, et al. Endocrine response after severe subarachnoid hemorrhage related to sodium and blood volume regulation. Anesth Analg. 2009;108(6):1922–8. https://doi.org/10.1213/ane.0b013e31819a85ae.
Strack AM, Sawyer WB, Platt KB, Loewy AD. CNS cell groups regulating the sympathetic outflow to adrenal gland as revealed by transneuronal cell body labeling with pseudorabies virus. Brain Res. 1989;491(2):274–96.
Cruz JC, Flor AF, Franca-Silva MS, Balarini CM, Braga VA. Reactive oxygen species in the paraventricular nucleus of the hypothalamus alter sympathetic activity during metabolic syndrome. Front Physiol. 2015;6:384. https://doi.org/10.3389/fphys.2015.00384.
Crompton MR. Hypothalamic lesions following the rupture of cerebral berry aneurysms. Brain. 1963;86:301–14.
Schneider HJ, Kreitschmann-Andermahr I, Ghigo E, Stalla GK, Agha A. Hypothalamopituitary dysfunction following traumatic brain injury and aneurysmal subarachnoid hemorrhage: a systematic review. Jama. 2007;298(12):1429–38. https://doi.org/10.1001/jama.298.12.1429.
Patel KP, Xu B, Liu X, Sharma NM, Zheng H. Renal denervation improves exaggerated sympathoexcitation in rats with heart failure: a role for neuronal nitric oxide synthase in the paraventricular nucleus. Hypertension. 2016;68(1):175–84. https://doi.org/10.1161/hypertensionaha.115.06794.
Hasegawa S, Hasegawa Y, Miura M. Current therapeutic drugs against cerebral vasospasm after subarachnoid hemorrhage: a comprehensive review of basic and clinical studies. Curr Drug Deliv. 2017;14(6):843–52. https://doi.org/10.2174/1567201813666160808100937.
Ansar S, Vikman P, Nielsen M, Edvinsson L. Cerebrovascular ETB, 5-HT1B, and AT1 receptor upregulation correlates with reduction in regional CBF after subarachnoid hemorrhage. Am J Physiol Heart Circ Physiol. 2007;293(6):H3750–8. https://doi.org/10.1152/ajpheart.00857.2007.
Wanderer S, Mrosek J, Vatter H, Seifert V, Konczalla J. Crosstalk between the angiotensin and endothelin system in the cerebrovasculature after experimental induced subarachnoid hemorrhage. Neurosurg Rev. 2018;41(2):539–48. https://doi.org/10.1007/s10143-017-0887-z.
Touyz RM, Schiffrin EL. Signal transduction mechanisms mediating the physiological and pathophysiological actions of angiotensin II in vascular smooth muscle cells. Pharmacol Rev. 2000;52(4):639–72.
Macdonald RL, Higashida RT, Keller E, Mayer SA, Molyneux A, Raabe A, et al. Clazosentan, an endothelin receptor antagonist, in patients with aneurysmal subarachnoid haemorrhage undergoing surgical clipping: a randomised, double-blind, placebo-controlled phase 3 trial (CONSCIOUS-2). Lancet Neurol. 2011;10(7):618–25. https://doi.org/10.1016/s1474-4422(11)70108-9.
Hasegawa Y, Suzuki H, Altay O, Chen H, Zhang JH. Treatment with sodium orthovanadate reduces blood-brain barrier disruption via phosphatase and tensin homolog deleted on chromosome 10 (PTEN) phosphorylation in experimental subarachnoid hemorrhage. J Neurosci Res. 2012;90(3):691–7. https://doi.org/10.1002/jnr.22801.
Maddahi A, Povlsen GK, Edvinsson L. Regulation of enhanced cerebrovascular expression of proinflammatory mediators in experimental subarachnoid hemorrhage via the mitogen-activated protein kinase kinase/extracellular signal-regulated kinase pathway. J Neuroinflammation. 2012;9:274. https://doi.org/10.1186/1742-2094-9-274.
Suzuki H, Hasegawa Y, Kanamaru K, Zhang JH. Mitogen-activated protein kinases in cerebral vasospasm after subarachnoid hemorrhage: a review. Acta Neurochir Suppl. 2011;110(Pt 1):133–9. https://doi.org/10.1007/978-3-7091-0353-1_23.
Munakata A, Naraoka M, Katagai T, Shimamura N, Ohkuma H. Role of cyclooxygenase-2 in relation to nitric oxide and endothelin-1 on pathogenesis of cerebral vasospasm after subarachnoid hemorrhage in rabbit. Transl Stroke Res. 2016;7(3):220–7. https://doi.org/10.1007/s12975-016-0466-6.
Beg SA, Hansen-Schwartz JA, Vikman PJ, Xu CB, Edvinsson LI. ERK1/2 inhibition attenuates cerebral blood flow reduction and abolishes ET(B) and 5-HT(1B) receptor upregulation after subarachnoid hemorrhage in rat. J Cereb Blood Flow Metab. 2006;26(6):846–56. https://doi.org/10.1038/sj.jcbfm.9600236.
Rabinstein AA, Lanzino G, Wijdicks EF. Multidisciplinary management and emerging therapeutic strategies in aneurysmal subarachnoid haemorrhage. Lancet Neurol. 2010;9(5):504–19. https://doi.org/10.1016/s1474-4422(10)70087-9.
Wijdicks EF, Vermeulen M, Murray GD, Hijdra A, van Gijn J. The effects of treating hypertension following aneurysmal subarachnoid hemorrhage. Clin Neurol Neurosurg. 1990;92(2):111–7.
Vergouwen MD, Vermeulen M, van Gijn J, Rinkel GJ, Wijdicks EF, Muizelaar JP, et al. Definition of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage as an outcome event in clinical trials and observational studies: proposal of a multidisciplinary research group. Stroke. 2010;41(10):2391–5. https://doi.org/10.1161/strokeaha.110.589275.
Etminan N, Vergouwen MD, Ilodigwe D, Macdonald RL. Effect of pharmaceutical treatment on vasospasm, delayed cerebral ischemia, and clinical outcome in patients with aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. J Cereb Blood Flow Metab. 2011;31(6):1443–51. https://doi.org/10.1038/jcbfm.2011.7.
Hasegawa Y, Suzuki H, Nakagawa T, Uekawa K, Koibuchi N, Kawano T, et al. Assessment of the correlations between brain weight and brain edema in experimental subarachnoid hemorrhage. Acta Neurochir Suppl. 2016;121:89–92. https://doi.org/10.1007/978-3-319-18497-5_15.
Funding
This study was supported by JSPS KAKENHI Grant Number 15K10309 and 19K09459.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving animals were conducted in accordance with the ethical standards of the institution or practice at which the studies were conducted.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1.
Supplemental Fig. 1: Schematic illustrating the protocols used in the experiments (a) and the study profile (b) in experiment 1. Abbreviations used include CBF, cerebral blood flow; NF, neurological functions; Op., operation; RD, renal denervation; S, sham; SAH, subarachnoid hemorrhage; WB, western blot. Supplemental Fig. 2: Schematic illustrating the protocols used in the experiments (a) and the study profile (b) in experiment 2. Abbreviations used include BP, blood pressure; BWC, brain water content; CBF, cerebral blood flow; NF, neurological functions; Op., operation; RD, renal denervation; S, Sham; SAH, subarachnoid hemorrhage. Supplemental Fig. 3: Schematic illustrating the protocols used in the experiments (a) and the study profile (b) in experiment 3. Abbreviations used include BP, blood pressure; BWC, brain water content; CBF, cerebral blood flow; CVS, cerebral vasospasm; EBI, early brain injury; ELISA, Enzyme-linked immunosorbent assay; IHC, immunohistochemistry; NF, neurological functions; Op., operation; RD, renal denervation; S, Sham; SAH, subarachnoid hemorrhage; WB, western blot. Supplemental Fig. 4: Difference in the SBP (a), HR (b), modified Garcia neurological score (c), latency to fall in the accelerating rotarod test (d), and CBF (e) at 24 hours after SAH among the S+Sham, SAH+Sham, and SAH+RD groups. Values are presented as means ± SEM. Asterisk indicates P<0.05. Abbreviations used include CBF, cerebral blood flow; HR, heart rate; RD, renal denervation; S, Sham; SAH, subarachnoid hemorrhage; SBP, systolic blood pressure. (PDF 87 kb)
Rights and permissions
About this article
Cite this article
Takemoto, Y., Hasegawa, Y., Hayashi, K. et al. The Stabilization of Central Sympathetic Nerve Activation by Renal Denervation Prevents Cerebral Vasospasm after Subarachnoid Hemorrhage in Rats. Transl. Stroke Res. 11, 528–540 (2020). https://doi.org/10.1007/s12975-019-00740-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-019-00740-9