Abstract
Hyperglycemia is commonly encountered in both diabetic and non-diabetic patients in acute ischemic stroke. Hyperglycemia in stroke has been associated with poor clinical outcome, a phenomenon that has been studied in experimental models, where hyperglycemia was shown to enhance cortical toxicity, increase infarct volumes, promote inflammation, and affect the cerebral vasculature. This has led to many trials attempting to modulate the hyperglycemic response as a therapeutic and neuroprotective strategy. Intensive glycemic control has been evaluated in stroke patients, with conflicting results. The evidence linking hyperglycemia with neurotoxicity coupled with the failure of intensive glucose control regimens to improve functional outcomes in stroke suggests that novel approaches should be devised. Recent attention has been paid to another related phenomenon, that of glycemic variability, which has been proven to be a predictor of outcome in critically ill patients; however, its the impact in stroke has not been evaluated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute hyperglycemia has been consistently associated with poor clinical outcome in stroke studies, a phenomenon that had been extensively studied in experimental models, where hyperglycemia was shown to enhance cortical toxicity, increase infarct volumes, promote inflammation, and affect the cerebral vasculature [1].
Intensive glycemic control has been evaluated in stroke patients, with conflicting results. The initial enthusiasm for intensive insulin therapy (IIT) in the intensive care unit has disappeared because currently available evidence-based data fail to identify any clinical benefit at the time of continuing to outline the high risk of hypoglycemia [2].
The evidence linking hyperglycemia with neurotoxicity coupled with the failure of intensive glucose control regimens to improve functional outcomes in stroke suggests that novel approaches should be devised. Recent attention has been paid to another related phenomenon, that of glycemic variability (GV), which takes into account the constant fluctuations of glycemia, including episodes of hyper- and hypoglycemia, even in a single day [3].
Although a relatively new parameter, as well as with somewhat of a controversy surrounding its measurement, GV has proven to be a predictor of outcome independent of mean glucose levels or glycosylated hemoglobin values in critically ill patients [4]. However, the impact of GV in stroke has not been evaluated, and recent evidence suggests it could be important both as a predictor as well as a treatment goal. In this review, we will examine this evidence.
Epidemiology and Financial Burden
In 2008, after years of being the third leading cause of death in the USA, stroke dropped to the fourth. The Center for Disease Control and Prevention reports a general decline in mortality for stroke over the past half century [5]. In the USA alone, approximately 800,000 people experience a stroke every year; on average, every 40 s, someone has a stroke [6–8].
Worldwide, stroke consumes about 2–4 % of total health-care costs, and in industrialized countries, stroke accounts for more than 4 % of direct health-care costs. The total costs to society have been variously estimated at £7.6 billion in the UK at 1995 prices and Australian $1.3 billion in Australia [9, 10]. The direct and indirect cost of stroke in 2009 was $38.6 billion in USA [7].
The mean lifetime cost of ischemic stroke in the USA is estimated at $140,048, including inpatient care, rehabilitation, and follow-up cares necessary for lasting deficits [11]. The total cost of stroke from 2005 to 2050, in 2005 dollars, is projected to be $1.52 trillion for non-Hispanic whites, $313 billion for Hispanics, and $379 billion for blacks. The per capita cost of stroke estimate is highest in blacks ($25,782), followed by Hispanics ($17,201) and non-Hispanic whites ($15.597) [12].
Diabetes mellitus is a common problem whose prevalence is increasing. It is estimated that 2.8 % of the worldwide population has diabetes, a number expected to rise to 4.4 % (or around 366 million people) in 2030 [13]. Furthermore, diabetes and ischemic stroke are intimately connected. People with diabetes have more than double the risk of stroke after correction of other risk factor compared with non-diabetics, and hyperglycemia is present in 30–40 % of patients with acute ischemic stroke [14].
Diabetic and non-diabetic patients alike are worsened by hyperglycemia [15]; however, ischemic stroke patients without a history of diabetes appear most affected by high admission glucose [16]. Diabetes is estimated to be present in 10–25 % of patients with stroke, and approximately 20 % of patients with diabetes will ultimately die of stroke [17]. In non-diabetic stroke patients, up to 37 % show impaired glucose metabolism on admission, a number that rises to 58 % when reassessed at 3 months after hospitalization [18]. However, observational data likely underestimate the true prevalence of diabetes in an acute stroke cohort. It is estimated that up to half of the patients with diabetes are undiagnosed [19].
The Deleterious Effects of Hyperglycemia
Animal and human studies have confirmed that there is an association between hyperglycemia and aggravated cerebral injury after stroke (Fig. 1). Studies using transcranial Doppler imaging have demonstrated that hyperglycemia is associated with persistent occlusion in patients with ischemic stroke treated with recombinant tissue plasminogen activator (rtPa) [20], confirming preclinical evidence that shown both hyperglycemia and hyperinsulinemia decrease the activity of rtPa in animal models of ischemic stroke [21].
Besides the effects of hyperglycemia on rtPa in human studies, it is demonstrated that hyperglycemia stimulates coagulation by increasing the production of thrombin–antithrombin complexes and by stimulating the tissue factor pathway [22, 23], whereas hyperinsulinemia decreases fibrinolytic activity by increasing the production of plasminogen activator inhibitor [24, 25].
Hyperglycemia also leads to changes in cerebral hemodynamics. Hemispheric cerebral blood flow is reduced by as much as 37 % in hyperglycemic compared with normoglycemic rats [26]. Furthermore, in a cat model of acute ischemic stroke, it was shown that hyperglycemia led to decreased penumbra blood flow after recanalization [27].
The inhibition of vasodilatation is an important mechanism by which hyperglycemia reduces cerebral blood flow. In humans, glucose infusion has been shown to reduce endothelium-dependent vasodilatation [28, 29]. Vasodilatation is predominantly mediated by endothelium-derived nitric oxide [30, 31], which is synthesized by endothelial nitric oxide synthase, whose expression is reduced with a hyperglycemic environment [32, 33].
Although restoration of blood flow to the ischemic tissue is essential for penumbral salvage, reperfusion itself can also induce injury, the phenomenon known as “ischemia–reperfusion injury” [34]. Some of the best-studied mechanisms of ischemia–reperfusion involve an intense inflammatory response and the generation of oxidative stress, and both of these mechanisms are enhanced in the setting of a hyperglycemic environment [35, 36].
Hyperglycemia increases the production of reactive oxygen species (ROS) through a protein kinase C-mediated pathway and by increasing the production of NADPH, which can lead to neuron death [37]. Hyperglycemia is known to be associated with increased expression of nuclear factor κB, known to stimulate inflammatory cytokine production, inflammatory cell function, and endothelial injury [38–40], factors ultimately resulting in increased injury and infarct size [41].
Deleterious effects of hyperglycemia over cellular homeostasis are also thought to participate in the aggravated injury response to ischemia. Hyperglycemia leads to increased lactic acid production and promotes an acidotic intracellular environment, causing mitochondrial dysfunction [42]. Support for this idea comes from a human study showing that hyperglycemia could correlate positively with increased cerebral lactate concentrations and reduced penumbral salvage after stroke [43].
Hyperglycemia in Patients With Acute Ischemic Stroke With and Without Diabetes
Glucose enters the brain microvascular endothelial cells from the blood side through GLUT1, a protein of 12 transmembrane domains that act as uniports, driving glucose down its concentration gradient [44]. Once glucose moves from the blood across the microvascular endothelial cell, it diffuses through the basal lamina and interstitial fluid to neurons, where it serves as the major cerebral energy substrate, and supports the complex metabolic interactions between neurons and astrocytes, essential for normal brain function and survival [45]. Although both hyperglycemia and hypoglycemia can affect brain function, despite variations in glucose flux (fed state, fasting state, etc.), blood glucose is maintained in a narrow range through a series of hormonal and physiological responses [46].
The best predictors of stroke recovery at 3 months are the initial neurological deficit and age; other factors include hyperglycemia, body temperature, and previous stroke [47]. Approximately a third of ischemic strokes occur in subjects with diabetes [48].
Several studies have shown that admission blood glucose is elevated in >40 % of patients with acute ischemic stroke, most commonly among patients with a history of diabetes [16, 49, 50]. A systematic review of 33 studies reported that 8–63 % of non-diabetic and 39–83 % of patients with diabetes and ischemic stroke had admission hyperglycemia [51]. Blood glucose levels seem to decline within the first 24 h after stroke onset [52], but they rise again after 24–88 h, regardless of whether the patient has diabetes mellitus [53].
A substantial proportion of patients with ischemic stroke without a documented history of diabetes have insulin resistance or diabetes at follow-up [54–57]. Furthermore, 27–37 % of patients admitted to hospital with stroke and concurrent hyperglycemia and no history of diabetes mellitus (DM) were shown to have impaired glucose tolerance 3 months after the initial stroke, and approximately one third of these cases had developed diabetes by this time point [54, 55, 57].
Serious illnesses, including stroke, are accompanied by a generalized stress reaction that involves the activation of the hypothalamic–pituitary–adrenal axis [58, 59], which leads to increased levels of serum glucocorticoids, and activation of the sympathetic autonomic nervous system [60], leading to excessive glucose production [61, 62], and insulin resistance with hyperinsulinemia [63–65].
Stroke is also associated with an increased inflammatory response and the release of cytokines [66, 67], which have been shown to activate the hypothalamic–pituitary–adrenal axis [68] and have also been associated with the development of insulin resistance [69–71].
Animals with ischemic stroke and hyperglycemia tend to have more brain edema, hemorrhagic transformation of infarcts, brain herniation, and death; the exacerbated damage with hyperglycemia is usually seen with reperfusion and occurs less with permanent occlusion [26, 38, 72–74].
Almost 30 years ago the relationship between hyperglycemia and poor clinical outcome after stroke was identified [75]; it was also demonstrated in recent studies [16, 76] and was also showed that this association is independent from other predictors of poor clinical outcome such as age, stroke severity, infarct size, or diabetic status [77–79].
A recent systematic review has revealed that hyperglycemic non-diabetic patients with ischemic stroke have an increased risk of mortality at early time points [16]. By contrast, no association between high blood glucose levels and short-term mortality was demonstrated in ischemic stroke patients with diabetes [80, 81]. In non-diabetic patients with acute ischemic stroke, hyperglycemia resulting from stroke seems to be associated with a high inhospital mortality risk and hyperglycemia that relates to a diagnosis of diabetes is not [82, 83].
Two studies have indicated that an association between hyperglycemia and poor stroke outcome exists in patients with cortical stroke, but not in patients with lacunar stroke [84, 85], and a post hoc analysis of three large clinical trials revealed that high levels of blood glucose were associated with good rather than poor clinical outcome after lacunar infarction [86].
Some studies have shown that hyperglycemia on admission to hospital also predicts poor outcome in patients with acute ischemic stroke treated with rtPa and is more pronounced than in non-rtPa-treated patients [85, 87–90]. With all this evidence, it is reasonable to expect that better control of acute hyperglycemia may improve the outcome in acute ischemic stroke patients.
Tight Glycemic Control
Aggressive correction of hyperglycemia has been studied in multiple acute illnesses in randomized trials with varied results. The most convincing trial was the surgical intensive care unit trial [91]. Patients treated aggressively had better clinical outcomes than patients under usual care. The benefits associated with aggressive hyperglycemia correction included decreased mortality, shorter time on ventilator, fewer bloodstream infections, and less critical illness polyneuropathy. A similar trial with patients in the medical intensive care unit showed less convincing results without a statistically significant difference in mortality as a primary outcome [92].
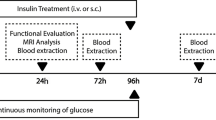
Small clinical trials have demonstrated that aggressive lowering of hyperglycemia during acute stroke is feasible and relatively safe. In one trial, glucose levels were about 30 mg/dL lower with IV insulin than with subcutaneous insulin and no serious adverse events occurred [93]. In another trial, glucose levels were 66 mg/dL lower with IV insulin than with subcutaneous insulin [94]. Patients in the aggressive treatment arm of this pilot trial had somewhat better clinical outcomes, but not statistically significant.
In the Glucose Insulin Stroke Trial—United Kingdom Trial [51], 933 acute stroke patients were randomized within 24 h after stroke onset to normal saline or insulin infusions. The mean admission glucose level was similar in the two treatment groups (137–141 mg/dL), and during treatment, the difference in mean glucose levels between the two treatment groups was only 10 mg/dL. No significant differences occurred in clinical outcomes between the two treatment groups. Four small, randomized trials were not powered to demonstrate a clinical benefit, but all showed that IIT induced a high risk of hypoglycemia in patients with acute stroke [95–98].
Despite the overwhelming evidence that hyperglycemia is statistically associated with poor functional outcome and increased mortality in patients with acute stroke, the current randomized controlled trials do not support the use of IIT. Further therapies are needed for more efficient and safer methods of improving blood glucose control.
The Deleterious Effects of Hypoglycemia
The main unwanted side effect of IIT in diabetes, hypoglycemia, is also a factor capable of aggravating cerebral ischemic injury. Even a single episode of severe hypoglycemia (<40 mg/dL or 2.2 mmol/L) or even much milder degrees of hypoglycemia (<81 mg/dL or 4.5 mmol/L) has been found to be independently associated with increased mortality in general ICU patients [99, 100].
Retinal cells have been shown to show increased susceptibility to ischemia when cultured in low-glucose mediums [101]. Cultured neurons also show increased cell death in response to ischemia when exposed to recurrent hypoglycemia in vitro [102], findings that were then confirmed in a rat model of cerebral ischemia, where recurrent hypoglycemia led to a 70 % increase in infarct size [103].
Independently of the mechanism of hypoglycemia (fasting-induced or insulin-induced), brain cells subjected to ischemia in these conditions show impaired energy metabolism and increased exposure to oxidative stress [104]. Besides oxidative stress, other mechanisms implicated in hypoglycemia-induced neurotoxicity during ischemia include mitochondrial dysfunction and increased calcium influx, but the precise pathways involved remain to be elucidated [105].
Considering the accumulating evidence showing that episodes of hypoglycemia in the context of intensive glucose-lowering therapy in critically ill patients are associated with increased mortality [99, 100, 106], the implementation of such strategies should be carefully considered and great care taken to avoid episodes of hypoglycemia.
The fact that both hyperglycemia and hypoglycemia can aggravate brain injury after stroke could partly explain the negative results of IIT trials but, importantly, also highly suggests that other more dynamic measures of glycemic control, such as GV, could more accurately predict outcome and be a suitable therapeutic objective.
Glycemic Variability
Oxidative stress, the putative mediator of diabetes complications [107], has been reported to be greater for intermittent as opposed to sustained hyperglycemia under experimental conditions [108] with confirmation in clinical studies [109, 110]. The potential role for GV in DM complications appears, therefore, to be an open question.
The Diabetes Control and Complications Trial (DCCT) demonstrated that lowering A1C significantly reduces the incidence and progression of microvascular complications in type 1 diabetes. A comparison of patients in both groups with identical A1C levels shows significant differences, as an example the risk of retinopathy in control patients with an A1C of 9 % was approximately 2.5 times greater than the risk of experimental patients with a 9 % A1C [111].
The only significant difference between these groups is that almost all patients of the control group were on twice daily NPH insulin, whereas subjects in the experimental group were on basal-bolus therapy or an insulin pump. This analysis of the data strongly suggests that the findings relate more to the impact of GV rather than to absolute A1C value [112].
A consensus on the gold standard method to measure glucose variability in clinical practice and research is still lacking, although a number of indicators have been proposed. The easiest way to get an impression of the GV in an individual patient is to calculate the standard deviation (SD) of plasma glucose measurements and/or the coefficient of variation (CV), if one wishes to correct for the mean [113].
A prospective observational study in 100 type 1 diabetes patients confirmed no relationship between short-term GV measured as SD and microvascular complications [114]. However, they found that GV was significantly related to the presence of peripheral neuropathy and was a borderline predictor of its incidence (hazard ratio, 1.73; P = 0.07), suggesting that the nervous system may be vulnerable to GV.
Three retrospective studies analyzed GV as a predictor of mortality at the adult ICU [115–117] concluding that GV, measured as SD, was a significant predictor of mortality independently from the severity of illness. A subgroup analysis of patients with diabetes displayed no relation with survival in contrast to patients without diabetes [116]. These results may suggest that patients with diabetes “get accustomed” to fluctuating glucose levels, making them less devastating.
A retrospective study of 935 patients showed that an increased GV, assessed by the SD and CV, is independently associated with longer length of stay and greater 90-day mortality in non-critically ill patients. These associations were independent of age, race, service of care, previous diagnosis of diabetes, A1C, body mass index, the use of regular insulin, mean plasma glucose, and hypoglycemia [118].
In the neurocritical care setting, a study showed that in patients with traumatic brain injury, GV, defined by SD and percentage of excursion from the preset range glucose level, was significantly associated with poorer long-term functional outcome [119] (Table 1).
Conclusions and Future Considerations
Exenatide, a glucagon-like peptide-1 (GLP-1) agonist, has shown in clinical studies that could minimize the risk for GV to a greater degree than insulin glargine or glimepiride treatment, even with identical average glucose levels [120, 121]. Exenatide has been shown to be neuroprotective in animal models of acute ischemic stroke. Both diabetic and non-diabetic exenatide-treated animals showed reduced infarct volume, reduced oxidative stress, inflammation, and apoptosis after ischemic stroke, an effect partially mediated trough reduced intracellular levels of cAMP and the protein kinase A pathway [122–125].
A study has shown that the addition of a dipeptidyl peptidase (DPP)-4 inhibitor to metformin therapy in diabetic patients significantly reduced GV, albeit mostly trough a reduction in basal hyperglycemia [126]. DPP-4 inhibitor administration to diabetic and non-diabetic rats led to reduced infarct volumes in models of transient middle cerebral artery occlusion, in a glucose-independent pathway likely involving GLP-1 and brain-derived growth factor production [127, 128].
Ultra-long-acting and high-strength formulations of new basal insulin analogs like insulin degludec, which differs from human insulin by deletion of threonine at position B30 and the attachment of a 16-carbon fatty diacid to the lysine residue at position B29 via a gamma-glutamic acid spacer [129], PEGylated Lispro, insulin lispro that has been site-specifically PEGylated with 20-kDa moiety at lysine B28, via a urethane bond [130], and glargine U300, a new formulation containing glargine at a concentration of 300 U/mL rather than the usual 100 U/mL [131], have the potential for less glycemic variability, less (nocturnal) hypoglycemia, and greater weight loss [132–134].
Despite there is no consensus on how to measure the GV, it is being demonstrated that an increase in this parameter leads to worse outcomes in many clinical settings. In stroke patients, the worst outcomes associated with hyperglycemia and the lack of benefit from IIT must be followed to a search for better ways to manage hyperglycemia. There are some strategies that are associated with an improvement in GV, and these strategies, in some animal models, have a neuroprotective role in stroke.
References
Kruyt ND, Biessels GJ, Devries JH, Roos YB. Hyperglycemia in acute ischemic stroke: pathophysiology and clinical management. Nat Rev Neurol. 2010;6(3):145–55.
Piironen K, Putaala J, Rosso C, Samson Y. Glucose and acute stroke: evidence for an interlude. Stroke J Cereb Circ. 2012;43(3):898–902.
Monnier L, Colette C. Glycemic variability: should we and can we prevent it? Diabetes Care. 2008;31 Suppl 2:S150–4.
Ceriello A, Ihnat MA. ‘Glycaemic variability’: a new therapeutic challenge in diabetes and the critical care setting. Diabet Med J Br Diabet Assoc. 2010;27(8):862–7.
Jauch EC, Saver JL, Adams Jr HP, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke J Cereb Circ. 2013;44(3):870–947.
Kung HC, Hoyert DL, Xu J, Murphy SL. Deaths: final data for 2005. National vital statistics reports : from the Centers for Disease Control and Prevention, National Center for Health Statistics. Natl Vital Stat Syst. 2008;56(10):1–120.
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127(1):e6–245.
Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, et al. Heart disease and stroke statistics—2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119(3):e21–181.
Donnan GA, Fisher M, Macleod M, Davis SM. Stroke Lancet. 2008;371(9624):1612–23.
Dewey HM, Thrift AG, Mihalopoulos C, Carter R, Macdonell RA, McNeil JJ, et al. Cost of stroke in Australia from a societal perspective: results from the North East Melbourne Stroke Incidence Study (NEMESIS). Stroke J Cereb Circ. 2001;32(10):2409–16.
Taylor TN, Davis PH, Torner JC, Holmes J, Meyer JW, Jacobson MF. Lifetime cost of stroke in the United States. Stroke J Cereb Circ. 1996;27(9):1459–66.
Brown DL, Boden-Albala B, Langa KM, Lisabeth LD, Fair M, Smith MA, et al. Projected costs of ischemic stroke in the United States. Neurology. 2006;67(8):1390–5.
Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–53.
Luitse MJ, Biessels GJ, Rutten GE, Kappelle LJ. Diabetes, hyperglycaemia, and acute ischaemic stroke. Lancet Neurol. 2012;11(3):261–71.
Pulsinelli WA, Levy DE, Sigsbee B, Scherer P, Plum F. Increased damage after ischemic stroke in patients with hyperglycemia with or without established diabetes mellitus. Am J Med. 1983;74(4):540–4.
Capes SE, Hunt D, Malmberg K, Pathak P, Gerstein HC. Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview. Stroke J Cereb Circ. 2001;32(10):2426–32.
Hewitt J, Castilla Guerra L, Fernandez-Moreno Mdel C, Sierra C. Diabetes and stroke prevention: a review. Stroke Res Treat. 2012;2012:673187.
Dave JA, Engel ME, Freercks R, Peter J, May W, Badri M, et al. Abnormal glucose metabolism in non-diabetic patients presenting with an acute stroke: prospective study and systematic review. QJM Mon J Assoc Phys. 2010;103(7):495–503.
Harris MI. Undiagnosed NIDDM: clinical and public health issues. Diabetes Care. 1993;16(4):642–52.
Ribo M, Molina C, Montaner J, Rubiera M, Delgado-Mederos R, Arenillas JF, et al. Acute hyperglycemia state is associated with lower tPA-induced recanalization rates in stroke patients. Stroke J Cereb Circ. 2005;36(8):1705–9.
Pandolfi A, Giaccari A, Cilli C, Alberta MM, Morviducci L, De Filippis EA, et al. Acute hyperglycemia and acute hyperinsulinemia decrease plasma fibrinolytic activity and increase plasminogen activator inhibitor type 1 in the rat. Acta Diabetol. 2001;38(2):71–6.
Gentile NT, Vaidyula VR, Kanamalla U, DeAngelis M, Gaughan J, Rao AK. Factor VIIa and tissue factor procoagulant activity in diabetes mellitus after acute ischemic stroke: impact of hyperglycemia. Thromb Haemost. 2007;98(5):1007–13.
Stegenga ME, van der Crabben SN, Levi M, de Vos AF, Tanck MW, Sauerwein HP, et al. Hyperglycemia stimulates coagulation, whereas hyperinsulinemia impairs fibrinolysis in healthy humans. Diabetes. 2006;55(6):1807–12.
Festa A, D’Agostino Jr R, Mykkanen L, Tracy RP, Zaccaro DJ, Hales CN, et al. Relative contribution of insulin and its precursors to fibrinogen and PAI-1 in a large population with different states of glucose tolerance. The Insulin Resistance Atherosclerosis Study (IRAS). Arterioscler Thromb Vasc Biol. 1999;19(3):562–8.
Meigs JB, Mittleman MA, Nathan DM, Tofler GH, Singer DE, Murphy-Sheehy PM, et al. Hyperinsulinemia, hyperglycemia, and impaired hemostasis: the Framingham Offspring Study. JAMA J Am Med Assoc. 2000;283(2):221–8.
Quast MJ, Wei J, Huang NC, Brunder DG, Sell SL, Gonzalez JM, et al. Perfusion deficit parallels exacerbation of cerebral ischemia/reperfusion injury in hyperglycemic rats. J Cereb Blood Flow Metab Off J Int Soc Cereb Blood Flow Metabol. 1997;17(5):553–9.
Venables GS, Miller SA, Gibson G, Hardy JA, Strong AJ. The effects of hyperglycaemia on changes during reperfusion following focal cerebral ischaemia in the cat. J Neurol Neurosurg Psychiatry. 1985;48(7):663–9.
Beckman JA, Goldfine AB, Gordon MB, Garrett LA, Creager MA. Inhibition of protein kinase Cbeta prevents impaired endothelium-dependent vasodilation caused by hyperglycemia in humans. Circ Res. 2002;90(1):107–11.
Williams SB, Goldfine AB, Timimi FK, Ting HH, Roddy MA, Simonson DC, et al. Acute hyperglycemia attenuates endothelium-dependent vasodilation in humans in vivo. Circulation. 1998;97(17):1695–701.
Vallance P, Collier J, Moncada S. Effects of endothelium-derived nitric oxide on peripheral arteriolar tone in man. Lancet. 1989;2(8670):997–1000.
Fleming I, Busse R. Molecular mechanisms involved in the regulation of the endothelial nitric oxide synthase. Am J Physiol Regul Integr Comp Physiol. 2003;284(1):R1–12.
Ding Y, Vaziri ND, Coulson R, Kamanna VS, Roh DD. Effects of simulated hyperglycemia, insulin, and glucagon on endothelial nitric oxide synthase expression. Am J Physiol Endocrinol Metab. 2000;279(1):E11–7.
Du XL, Edelstein D, Dimmeler S, Ju Q, Sui C, Brownlee M. Hyperglycemia inhibits endothelial nitric oxide synthase activity by posttranslational modification at the Akt site. J Clin Invest. 2001;108(9):1341–8.
McCord JM. Oxygen-derived free radicals in postischemic tissue injury. N Engl J Med. 1985;312(3):159–63.
Kamada H, Yu F, Nito C, Chan PH. Influence of hyperglycemia on oxidative stress and matrix metalloproteinase-9 activation after focal cerebral ischemia/reperfusion in rats: relation to blood-brain barrier dysfunction. Stroke J Cereb Circ. 2007;38(3):1044–9.
Wei J, Huang NC, Quast MJ. Hydroxyl radical formation in hyperglycemic rats during middle cerebral artery occlusion/reperfusion. Free Radic Biol Med. 1997;23(7):986–95.
Suh SW, Shin BS, Ma H, Van Hoecke M, Brennan AM, Yenari MA, et al. Glucose and NADPH oxidase drive neuronal superoxide formation in stroke. Ann Neurol. 2008;64(6):654–63.
Martini SR, Kent TA. Hyperglycemia in acute ischemic stroke: a vascular perspective. J Cereb Blood Flow Metab Off J Int Soc Cereb Blood Flow Metab. 2007;27(3):435–51.
Garg R, Chaudhuri A, Munschauer F, Dandona P. Hyperglycemia, insulin, and acute ischemic stroke: a mechanistic justification for a trial of insulin infusion therapy. Stroke J Cereb Circ. 2006;37(1):267–73.
Bemeur C, Ste-Marie L, Montgomery J. Increased oxidative stress during hyperglycemic cerebral ischemia. Neurochem Int. 2007;50(7–8):890–904.
Bemeur C, Ste-Marie L, Desjardins P, Vachon L, Butterworth RF, Hazell AS, et al. Dehydroascorbic acid normalizes several markers of oxidative stress and inflammation in acute hyperglycemic focal cerebral ischemia in the rat. Neurochem Int. 2005;46(5):399–407.
Anderson RE, Tan WK, Martin HS, Meyer FB. Effects of glucose and PaO2 modulation on cortical intracellular acidosis, NADH redox state, and infarction in the ischemic penumbra. Stroke J Cereb Circ. 1999;30(1):160–70.
Parsons MW, Barber PA, Desmond PM, Baird TA, Darby DG, Byrnes G, et al. Acute hyperglycemia adversely affects stroke outcome: a magnetic resonance imaging and spectroscopy study. Ann Neurol. 2002;52(1):20–8.
Lee WL, Klip A. Shuttling glucose across brain microvessels, with a little help from GLUT1 and AMP kinase. Focus on “AMP kinase regulation of sugar transport in brain capillary endothelial cells during acute metabolic stress”. Am J Physiol Cell Physiol. 2012;303(8):C803–5.
Amaral AI. Effects of hypoglycaemia on neuronal metabolism in the adult brain: role of alternative substrates to glucose. J Inherit Metab Dis. 2013;36(4):621–34.
Sprague JE, Arbelaez AM. Glucose counterregulatory responses to hypoglycemia. Pediatr Endocrinol Rev: PER. 2011;9(1):463–73. quiz 74-5.
Weimar C, Ziegler A, Konig IR, Diener HC. Predicting functional outcome and survival after acute ischemic stroke. J Neurol. 2002;249(7):888–95.
Woo D, Gebel J, Miller R, Kothari R, Brott T, Khoury J, et al. Incidence rates of first-ever ischemic stroke subtypes among blacks: a population-based study. Stroke J Cereb Circ. 1999;30(12):2517–22.
Gentile NT, Seftchick MW, Huynh T, Kruus LK, Gaughan J. Decreased mortality by normalizing blood glucose after acute ischemic stroke. Acad Emerg Med Off J Soc Acad Emerg Med. 2006;13(2):174–80.
Williams LS, Rotich J, Qi R, Fineberg N, Espay A, Bruno A, et al. Effects of admission hyperglycemia on mortality and costs in acute ischemic stroke. Neurology. 2002;59(1):67–71.
Gray CS, Hildreth AJ, Sandercock PA, O’Connell JE, Johnston DE, Cartlidge NE, et al. Glucose-potassium-insulin infusions in the management of post-stroke hyperglycaemia: the UK Glucose Insulin in Stroke Trial (GIST-UK). Lancet Neurol. 2007;6(5):397–406.
Yong M, Kaste M. Dynamic of hyperglycemia as a predictor of stroke outcome in the ECASS-II trial. Stroke J Cereb Circ. 2008;39(10):2749–55.
Allport L, Baird T, Butcher K, Macgregor L, Prosser J, Colman P, et al. Frequency and temporal profile of poststroke hyperglycemia using continuous glucose monitoring. Diabetes Care. 2006;29(8):1839–44.
Gray CS, Scott JF, French JM, Alberti KG, O’Connell JE. Prevalence and prediction of unrecognised diabetes mellitus and impaired glucose tolerance following acute stroke. Age Ageing. 2004;33(1):71–7.
Kernan WN, Viscoli CM, Inzucchi SE, Brass LM, Bravata DM, Shulman GI, et al. Prevalence of abnormal glucose tolerance following a transient ischemic attack or ischemic stroke. Arch Intern Med. 2005;165(2):227–33.
Matz K, Keresztes K, Tatschl C, Nowotny M, Dachenhausen A, Brainin M, et al. Disorders of glucose metabolism in acute stroke patients: an underrecognized problem. Diabetes Care. 2006;29(4):792–7.
Vancheri F, Curcio M, Burgio A, Salvaggio S, Gruttadauria G, Lunetta MC, et al. Impaired glucose metabolism in patients with acute stroke and no previous diagnosis of diabetes mellitus. QJM : Mon J Assoc Phys. 2005;98(12):871–8.
Gauna C, van den Berghe GH, van der Lely AJ. Pituitary function during severe and life-threatening illnesses. Pituitary. 2005;8(3–4):213–7.
Vanhorebeek I, Langouche L, Van den Berghe G. Endocrine aspects of acute and prolonged critical illness. Nat Clin Pract Endocrinol Metab. 2006;2(1):20–31.
Van den Berghe G. Novel insights into the neuroendocrinology of critical illness. Eur J Endocrinol Eur Fed Endocr Soc. 2000;143(1):1–13.
Barth E, Albuszies G, Baumgart K, Matejovic M, Wachter U, Vogt J, et al. Glucose metabolism and catecholamines. Crit Care Med. 2007;35(9 Suppl):S508–18.
Seematter G, Binnert C, Martin JL, Tappy L. Relationship between stress, inflammation and metabolism. Curr Opin Clin Nutr Metab Care. 2004;7(2):169–73.
Gearhart MM, Parbhoo SK. Hyperglycemia in the critically ill patient. AACN Clin Issues. 2006;17(1):50–5.
Hunt DG, Ivy JL. Epinephrine inhibits insulin-stimulated muscle glucose transport. J Appl Physiol. 2002;93(5):1638–43. Bethesda, Md : 1985.
O’Neill PA, Davies I, Fullerton KJ, Bennett D. Stress hormone and blood glucose response following acute stroke in the elderly. Stroke J Cereb Circ. 1991;22(7):842–7.
Tarkowski E, Rosengren L, Blomstrand C, Wikkelso C, Jensen C, Ekholm S, et al. Early intrathecal production of interleukin-6 predicts the size of brain lesion in stroke. Stroke J Cereb Circ. 1995;26(8):1393–8.
Vila N, Castillo J, Davalos A, Chamorro A. Proinflammatory cytokines and early neurological worsening in ischemic stroke. Stroke J Cereb Circ. 2000;31(10):2325–9.
Chrousos GP. The hypothalamic-pituitary-adrenal axis and immune-mediated inflammation. N Engl J Med. 1995;332(20):1351–62.
del Aguila LF, Claffey KP, Kirwan JP. TNF-alpha impairs insulin signaling and insulin stimulation of glucose uptake in C2C12 muscle cells. Am J Physiol. 1999;276(5 Pt 1):E849–55.
Rask-Madsen C, Dominguez H, Ihlemann N, Hermann T, Kober L, Torp-Pedersen C. Tumor necrosis factor-alpha inhibits insulin’s stimulating effect on glucose uptake and endothelium-dependent vasodilation in humans. Circulation. 2003;108(15):1815–21.
Plomgaard P, Bouzakri K, Krogh-Madsen R, Mittendorfer B, Zierath JR, Pedersen BK. Tumor necrosis factor-alpha induces skeletal muscle insulin resistance in healthy human subjects via inhibition of Akt substrate 160 phosphorylation. Diabetes. 2005;54(10):2939–45.
Bruno A, Williams LS, Kent TA. How important is hyperglycemia during acute brain infarction? Neurologist. 2004;10(4):195–200.
de Courten-Myers G, Myers RE, Schoolfield L. Hyperglycemia enlarges infarct size in cerebrovascular occlusion in cats. Stroke J Cereb Circ. 1988;19(5):623–30.
Kent TA, Soukup VM, Fabian RH. Heterogeneity affecting outcome from acute stroke therapy: making reperfusion worse. Stroke J Cereb Circ. 2001;32(10):2318–27.
Melamed E. Reactive hyperglycaemia in patients with acute stroke. J Neurol Sci. 1976;29(2–4):267–75.
McCormick MT, Muir KW, Gray CS, Walters MR. Management of hyperglycemia in acute stroke: how, when, and for whom? Stroke J Cereb Circ. 2008;39(7):2177–85.
Baird TA, Parsons MW, Phan T, Butcher KS, Desmond PM, Tress BM, et al. Persistent poststroke hyperglycemia is independently associated with infarct expansion and worse clinical outcome. Stroke J Cereb Circ. 2003;34(9):2208–14.
Allport LE, Butcher KS, Baird TA, MacGregor L, Desmond PM, Tress BM, et al. Insular cortical ischemia is independently associated with acute stress hyperglycemia. Stroke J Cereb Circ. 2004;35(8):1886–91.
Fuentes B, Castillo J, San Jose B, Leira R, Serena J, Vivancos J, et al. The prognostic value of capillary glucose levels in acute stroke: the GLycemia in Acute Stroke (GLIAS) study. Stroke J Cereb Circ. 2009;40(2):562–8.
Stollberger C, Exner I, Finsterer J, Slany J, Steger C. Stroke in diabetic and non-diabetic patients: course and prognostic value of admission serum glucose. Ann Med. 2005;37(5):357–64.
Stead LG, Gilmore RM, Bellolio MF, Mishra S, Bhagra A, Vaidyanathan L, et al. Hyperglycemia as an independent predictor of worse outcome in non-diabetic patients presenting with acute ischemic stroke. Neurocrit Care. 2009;10(2):181–6.
Egi M, Bellomo R, Stachowski E, French CJ, Hart GK, Hegarty C, et al. Blood glucose concentration and outcome of critical illness: the impact of diabetes. Crit Care Med. 2008;36(8):2249–55.
Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002;87(3):978–82.
Kruyt ND, Nys GM, van der Worp HB, van Zandvoort MJ, Kappelle LJ, Biessels GJ. Hyperglycemia and cognitive outcome after ischemic stroke. J Neurol Sci. 2008;270(1–2):141–7.
Bruno A, Levine SR, Frankel MR, Brott TG, Lin Y, Tilley BC, et al. Admission glucose level and clinical outcomes in the NINDS rt-PA Stroke Trial. Neurology. 2002;59(5):669–74.
Uyttenboogaart M, Koch MW, Stewart RE, Vroomen PC, Luijckx GJ, De Keyser J. Moderate hyperglycaemia is associated with favourable outcome in acute lacunar stroke. Brain J Neurol. 2007;130(Pt 6):1626–30.
Alvarez-Sabin J, Molina CA, Ribo M, Arenillas JF, Montaner J, Huertas R, et al. Impact of admission hyperglycemia on stroke outcome after thrombolysis: risk stratification in relation to time to reperfusion. Stroke J Cereb Circ. 2004;35(11):2493–8.
Leigh R, Zaidat OO, Suri MF, Lynch G, Sundararajan S, Sunshine JL, et al. Predictors of hyperacute clinical worsening in ischemic stroke patients receiving thrombolytic therapy. Stroke J Cereb Circ. 2004;35(8):1903–7.
Alvarez-Sabin J, Molina CA, Montaner J, Arenillas JF, Huertas R, Ribo M, et al. Effects of admission hyperglycemia on stroke outcome in reperfused tissue plasminogen activator–treated patients. Stroke J Cereb Circ. 2003;34(5):1235–41.
Saposnik G, Young B, Silver B, Di Legge S, Webster F, Beletsky V, et al. Lack of improvement in patients with acute stroke after treatment with thrombolytic therapy: predictors and association with outcome. JAMA J Am Med Assoc. 2004;292(15):1839–44.
van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345(19):1359–67.
Van den Berghe G, Wilmer A, Hermans G, Meersseman W, Wouters PJ, Milants I, et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354(5):449–61.
Walters MR, Weir CJ, Lees KR. A randomised, controlled pilot study to investigate the potential benefit of intervention with insulin in hyperglycaemic acute ischaemic stroke patients. Cerebrovasc Dis. 2006;22(2-3):116–22. Basel, Switzerland.
Bruno A, Kent TA, Coull BM, Shankar RR, Saha C, Becker KJ, et al. Treatment of hyperglycemia in ischemic stroke (THIS): a randomized pilot trial. Stroke J Cereb Circ. 2008;39(2):384–9.
Kreisel SH, Berschin UM, Hammes HP, Leweling H, Bertsch T, Hennerici MG, et al. Pragmatic management of hyperglycaemia in acute ischaemic stroke: safety and feasibility of intensive intravenous insulin treatment. Cerebrovasc Dis. 2009;27(2):167–75. Basel, Switzerland.
Johnston KC, Hall CE, Kissela BM, Bleck TP, Conaway MR. Glucose Regulation in Acute Stroke Patients (GRASP) trial: a randomized pilot trial. Stroke J Cereb Circ. 2009;40(12):3804–9.
Staszewski J, Brodacki B, Kotowicz J, Stepien A. Intravenous insulin therapy in the maintenance of strict glycemic control in nondiabetic acute stroke patients with mild hyperglycemia. J Stroke Cerebrovasc Dis Off J Natl Stroke Assoc. 2011;20(2):150–4.
McCormick M, Hadley D, McLean JR, Macfarlane JA, Condon B, Muir KW. Randomized, controlled trial of insulin for acute poststroke hyperglycemia. Ann Neurol. 2010;67(5):570–8.
Krinsley JS, Grover A. Severe hypoglycemia in critically ill patients: risk factors and outcomes. Crit Care Med. 2007;35(10):2262–7.
Egi M, Bellomo R, Stachowski E, French CJ, Hart GK, Taori G, et al. Hypoglycemia and outcome in critically ill patients. Mayo Clin Proc. 2010;85(3):217–24.
Casson RJ, Wood JP, Osborne NN. Hypoglycaemia exacerbates ischaemic retinal injury in rats. Br J Ophthalmol. 2004;88(6):816–20.
Dave KR, Tamariz J, Desai KM, Brand FJ, Liu A, Saul I, et al. Recurrent hypoglycemia exacerbates cerebral ischemic damage in streptozotocin-induced diabetic rats. Stroke J Cereb Circ. 2011;42(5):1404–11.
Dave KR, Pileggi A, Raval AP. Recurrent hypoglycemia increases oxygen glucose deprivation-induced damage in hippocampal organotypic slices. Neurosci Lett. 2011;496(1):25–9.
Chang YS, Park WS, Ko SY, Kang MJ, Han JM, Lee M, et al. Effects of fasting and insulin-induced hypoglycemia on brain cell membrane function and energy metabolism during hypoxia-ischemia in newborn piglets. Brain Res. 1999;844(1–2):135–42.
Rehni AK, Nautiyal N, Perez-Pinzon MA, Dave KR. Hyperglycemia/hypoglycemia-induced mitochondrial dysfunction and cerebral ischemic damage in diabetics. Metab Brain Dis. 2014.
Bagshaw SM, Bellomo R, Jacka MJ, Egi M, Hart GK, George C. The impact of early hypoglycemia and blood glucose variability on outcome in critical illness. Crit Care. 2009;13(3):R91. London, England.
Brownlee M. Biochemistry and molecular cell biology of diabetic complications. Nature. 2001;414(6865):813–20.
Ceriello A, Esposito K, Piconi L, Ihnat MA, Thorpe JE, Testa R, et al. Oscillating glucose is more deleterious to endothelial function and oxidative stress than mean glucose in normal and type 2 diabetic patients. Diabetes. 2008;57(5):1349–54.
Monnier L, Colette C, Mas E, Michel F, Cristol JP, Boegner C, et al. Regulation of oxidative stress by glycaemic control: evidence for an independent inhibitory effect of insulin therapy. Diabetologia. 2010;53(3):562–71.
Monnier L, Mas E, Ginet C, Michel F, Villon L, Cristol JP, et al. Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA J Am Med Assoc. 2006;295(14):1681–7.
The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–86.
Hirsch IB. Glycemic variability: it’s not just about A1C anymore! Diabetes Technol Ther. 2005;7(5):780–3.
Siegelaar SE, Holleman F, Hoekstra JB, DeVries JH. Glucose variability; does it matter? Endocr Rev. 2010;31(2):171–82.
Bragd J, Adamson U, Backlund LB, Lins PE, Moberg E, Oskarsson P. Can glycaemic variability, as calculated from blood glucose self-monitoring, predict the development of complications in type 1 diabetes over a decade? Diabetes Metab. 2008;34(6 Pt 1):612–6.
Dossett LA, Cao H, Mowery NT, Dortch MJ, Morris Jr JM, May AK. Blood glucose variability is associated with mortality in the surgical intensive care unit. Am Surg. 2008;74(8):679–85. discussion 85.
Egi M, Bellomo R, Stachowski E, French CJ, Hart G. Variability of blood glucose concentration and short-term mortality in critically ill patients. Anesthesiology. 2006;105(2):244–52.
Krinsley JS. Glycemic variability: a strong independent predictor of mortality in critically ill patients. Crit Care Med. 2008;36(11):3008–13.
Mendez CE, Mok KT, Ata A, Tanenberg RJ, Calles-Escandon J, Umpierrez GE. Increased glycemic variability is independently associated with length of stay and mortality in noncritically ill hospitalized patients. Diabetes Care. 2013;36(12):4091–7.
Matsushima K, Peng M, Velasco C, Schaefer E, Diaz-Arrastia R, Frankel H. Glucose variability negatively impacts long-term functional outcome in patients with traumatic brain injury. J Crit Care. 2012;27(2):125–31.
McCall AL, Cox DJ, Brodows R, Crean J, Johns D, Kovatchev B. Reduced daily risk of glycemic variability: comparison of exenatide with insulin glargine. Diabetes Technol Ther. 2009;11(6):339–44.
Irace C, Fiorentino R, Carallo C, Scavelli F, Gnasso A. Exenatide improves glycemic variability assessed by continuous glucose monitoring in subjects with type 2 diabetes. Diabetes Technol Ther. 2011;13(12):1261–3.
Lee CH, Yan B, Yoo KY, Choi JH, Kwon SH, Her S, et al. Ischemia-induced changes in glucagon-like peptide-1 receptor and neuroprotective effect of its agonist, exendin-4, in experimental transient cerebral ischemia. J Neurosci Res. 2011;89(7):1103–13.
Teramoto S, Miyamoto N, Yatomi K, Tanaka Y, Oishi H, Arai H, et al. Exendin-4, a glucagon-like peptide-1 receptor agonist, provides neuroprotection in mice transient focal cerebral ischemia. J Cereb Blood Flow Metab Off J Int Soc Cereb Blood Flow Metab. 2011;31(8):1696–705.
Briyal S, Gulati K, Gulati A. Repeated administration of exendin-4 reduces focal cerebral ischemia-induced infarction in rats. Brain Res. 2012;1427:23–34.
Darsalia V, Mansouri S, Ortsater H, Olverling A, Nozadze N, Kappe C, et al. Glucagon-like peptide-1 receptor activation reduces ischaemic brain damage following stroke in type 2 diabetic rats. Clin Sci. 2012;122(10):473–83. London, England : 1979.
Guerci B, Monnier L, Serusclat P, Petit C, Valensi P, Huet D, et al. Continuous glucose profiles with vildagliptin versus sitagliptin in add-on to metformin: results from the randomized Optima study. Diabetes Metab. 2012;38(4):359–66.
Darsalia V, Ortsater H, Olverling A, Darlof E, Wolbert P, Nystrom T, et al. The DPP-4 inhibitor linagliptin counteracts stroke in the normal and diabetic mouse brain: a comparison with glimepiride. Diabetes. 2013;62(4):1289–96.
Yang D, Nakajo Y, Iihara K, Kataoka H, Yanamoto H. Alogliptin, a dipeptidylpeptidase-4 inhibitor, for patients with diabetes mellitus type 2, induces tolerance to focal cerebral ischemia in non-diabetic, normal mice. Brain Res. 2013;1517:104–13.
Jonassen I, Havelund S, Hoeg-Jensen T, Steensgaard DB, Wahlund PO, Ribel U. Design of the novel protraction mechanism of insulin degludec, an ultra-long-acting basal insulin. Pharm Res. 2012;29(8):2104–14.
Bergenstal RM, Rosenstock J, Bastyr 3rd EJ, Prince MJ, Qu Y, Jacober SJ. Lower glucose variability and hypoglycemia measured by continuous glucose monitoring with novel long-acting insulin LY2605541 versus insulin glargine. Diabetes Care. 2014;37(3):659–65.
Steinstraesser A, Schmidt R, Bergmann K, Dahmen R, Becker RH. Investigational new insulin glargine 300 U/ml has the same metabolism as insulin glargine 100 U/ml. Diabetes Obes Metab. 2014.
Maiorino MI, Petrizzo M, Capuano A, Giugliano D, Esposito K. The development of new basal insulins: is there any clinical advantage with their use in type 2 diabetes? Expert Opin Biol Ther. 2014;14(6):799–808.
Garber AJ. Will the next generation of basal insulins offer clinical advantages? Diabetes Obes Metab. 2014;16(6):483–91.
Owens DR, Matfin G, Monnier L. Basal insulin analogues in the management of diabetes mellitus: what progress have we made? Diabetes Metab Res Rev. 2014;30(2):104–19.
Compliance with Ethics Requirements
This article does not contain any studies with human or animal subjects.
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
González-Moreno, E.I., Cámara-Lemarroy, C.R., González-González, J.G. et al. Glycemic Variability and Acute Ischemic Stroke: The Missing Link?. Transl. Stroke Res. 5, 638–646 (2014). https://doi.org/10.1007/s12975-014-0365-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-014-0365-7