Abstract
Objectives
The prognostic value of preimplantation nutritional status is not yet known for older diabetic patients that received right ventricular pacing (RVP). The study aimed to investigate the clinical value of the four malnutrition screening tools for the prediction of heart failure hospitalization (HFH) in older diabetic patients that received RVP.
Design
Retrospective observational cohort study.
Setting and Participants
This study was conducted between January 2017 and January 2018 at the Fuwai Hospital, Beijing, China, and included older (age ≥ 65 years) diabetic patients that received RVP for the first time
Measurements
The Prognostic Nutritional Index (PNI), Geriatric Nutritional Risk Index (GNRI), Naples Prognostic Score (NPS), and the Controlling Nutritional Status (CONUT) score were used to estimate the preimplantation nutritional status of the patients. Univariate and multivariate Cox proportional hazard regression analyses were performed to investigate the association between preimplantation malnutrition and HFH.
Results
Overall, 231 older diabetic patients receiving RVP were included. The median follow-up period after RVP was 53 months. HFH was reported for 19.9% of the included patients. Our results showed preimplantation malnutrition for 18.2%, 15.2%, 86.6% and 66.2% of the included patients based on the PNI, GNRI, NPS, and CONUT score, respectively. The cumulative rate of HFH during follow-up period was significantly higher for patients in the preimplantation malnutrition group based on the PNI (log-rank = 13.0, P = 0.001), GNRI (log-rank = 8.5, P = 0.01), and NPS (log-rank = 15.7, P < 0.001) compared to the normal nutrition group, but was not statistically significant for those in the preimplantation malnutrition group based on the CONUT score (log-rank = 2.7, P = 0.3). As continuous variables, all the nutritional indices showed significant correlation with HFH (all P < 0.05). However, multivariate analysis showed that only GNRI was independently associated with HFH (HR = 0.97, 95% CI: 0.937–0.997, P = 0.032). As categorical variables, PNI, GNRI, and NPS showed significant correlation with HFH. After adjustment of confounding factors, moderate-to-severe degree of malnutrition was an independent predictor of HFH based on the PNI (HR = 4.66, 95% CI: 1.03-21.00, P = 0.045) and GNRI (HR = 3.02, 95% CI: 1.02-9.00, P = 0.047).
Conclusion
Preimplantation malnutrition was highly prevalent in older diabetic patients that received RVP. The malnutrition prediction tools, PNI and GNRI, showed significant prognostic value in accurately predicting HFH in older diabetic patients with RVP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The number of patients receiving permanent pacemaker implantation (PPMI) has grown significantly because of the constantly increasing global aging population. According to current estimates, approximately 1 million pacemaker devices are implanted every year (1). Right ventricular pacing (RVP) is a conventional PPMI strategy that involves single-site pacemaker implantation in the right ventricular septum (RVS) or the right ventricular apex (RVA) (2). However, RVP is associated with deterioration of left ventricular function because of prolonged asynchronous patterns of left ventricular contractions (3–5).
More than 80% of patients receiving PPMI are older than 65 years (2). Furthermore, patients with type 2 diabetes mellitus are associated with an increased risk of bradyarrhythmia. Rautio et al reported that the incidence of PPMI in diabetic patients was 242.2 /10,000 person-years compared to 152.5/10,000 person-years in the control subjects (6). Both advanced age (7) and diabetes mellitus (8) are associated with an increased risk of heart failure (HF) progression. Therefore, there is an urgent need to identify risk factors that can be used for accurate prediction of HF so that patients with greater risk of heart failure hospitalization (HFH) among the elderly diabetic patients receiving RVP can receive early interventions.
Malnutrition is associated with cardiac remodeling and unfavorable clinical outcomes in general population and in patients with heart failure (9, 10). Malnutrition and underweight are associated with a higher risk of adverse events in patients that have undergone PPMI (11–14). The Prognostic Nutritional Index (PNI), the Geriatric Nutritional Risk Index (GNRI), the Naples Prognostic Score (NPS), and the Controlling Nutritional Status (CONUT) score are malnutrition screening tools that use easily available clinical information and biomarkers to estimate the nutritional status. However, the prognostic value of preimplantation nutritional status is not yet known for older diabetic patients receiving RVP.
A critical research hypothesis was generated that the preimplantation malnutrition status was associated with increased rate of HFH in older diabetic patients that received RVP. The study aimed to investigate the clinical value of the four malnutrition screening tools for the prediction of HFH in older diabetic patients that received RVP.
Materials and Methods
Ethic approval and study population
This retrospective observational cohort study was conducted between January 2017 and January 2018 at the Fuwai Hospital, Beijing, China. It was approved by the Ethics Committee of the Chinese Academy of Medical Sciences, Fuwai Hospital (Approval No. IRB2012-BG-006). The written informed consent was obtained from all the patients included in this study.
The inclusion criteria were as follows: (1) age ≥ 65 years; (2) diagnosed with diabetes mellitus; (3) underwent RVP for the first time. The diagnosis of diabetes mellitus was based on the previous history of hypoglycemic drugs or more than two records of fasting blood glucose levels ≥ 7.0 mmol/L during hospitalization. Initially, 1937 patients that received PPMI were enrolled during the study period. Then, we excluded patients with (1) age < 65 years (n = 742); (2) pacemaker upgrade or replacement (n = 297); (3) without diabetes mellitus (n = 665); and (4) values missing for total cholesterol (n = 2). Finally, 231 patients were included in our study (Figure 1).
Assessment of nutritional status
The nutritional status of the included study subjects were assessed with four malnutrition screening indices using the clinical information and biomarkers acquired during admission.
PNI was calculated for all the patients using the following formula: 10 × albumin (g/dl) + 0.005 × total lymphocyte count (/mm3) (15). The patients were then categorized into the following groups: normal (PNI ≥ 45), mild (35 ≤ PNI < 45), and moderate-to-severe (PNI < 35) degree of malnutrition.
GNRI was calculated using the following formula: 1.489 × albumin (g/L) + 41.7 × current body weight/ideal body weight (16). The ideal body weight for males was defined as height (cm) − 100 − [height (cm) − 150]/4. The ideal body weight for females was defined as height (cm) − 100 − [height (cm) − 150]/2.5. Then, the patients were categorized into the following groups: normal (GNRI ≥ 98), mild (92 ≤ GNRI < 98), and moderate-to-severe (GNRI < 92) degree of malnutrition.
NPS scores were based on the following serum parameters: albumin, total cholesterol, neutrophil-to-lymphocyte ratio, and platelet-to-lymphocyte ratio (17). Patients were then categorized into the following groups: normal (NPR = 0), mild (NPR = 1–2), and moderate-to-severe (NPR = 3–4) degree of malnutrition. CONUT scores were estimated based on serum albumin, total cholesterol, and total lymphocyte counts (18). Patients were then categorized into the following groups: normal (CONUT = 0–1), mild (CONUT = 2–4), and moderate-to-severe (CONUT = 5–12) degree of malnutrition.
Data collection
Trained study coordinators extracted the following clinical information for all the included patients from the electronic medical recording system: (1) demographic parameters such as age, gender, weight, height, body mass index (BMI), body fat proportion, smoke, and drink history; (2) clinical parameters such as heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), and New York Heart Association (NYHA) classification; (3) past medical history, including sinus node dysfunction (SND), atrioventricular block (AVB), atrial fibrillation (AF), and heart failure (HF); (4) medical therapy, including statin, angiotensin-converting enzyme inhibitor/ angiotensin receptor blocker (ACEi/ARB), β blocker, diuretic, insulin, a glucosidase, and metformin; (5) laboratory results for blood parameters, including the counts of white blood cells, neutrophils, lymphocytes, red blood cells, and platelets, as well as the serum levels of hemoglobin, albumin, total bilirubin, direct bilirubin, fasting blood glucose, estimated glomerular filtration rate (eGFR), blood urea nitrogen (BUN), total cholesterol (TC), high-density lipoprotein cholesterol (HDLC), low-density lipoprotein cholesterol (LDL-C), hemoglobin A1C (HbA1C), and N-terminal pro-brain natriuretic peptide (NT-pro BNP); (6) echocardiographic features such as left atrium diameter (LAD) and left ventricular ejection fraction (LVEF); and (7) details of RVS pacing, RVA pacing, and ventricular pacing burden.
Follow-up and study endpoints
All the patients were followed up for any reports of HFH, which was defined as an unplanned outpatient or emergency department visit, or hospitalization because of new onset or worsening symptoms and signs of HF that required diuretic therapy and was accompanied with significantly elevated levels of N-terminal pro-B natriuretic peptide (NT-pro BNP). The duration of follow-up was measured from the date of receiving RVP to the date of the first HFH, or date of the follow-up deadline (January 30, 2022). The median follow-up duration was 53 months.
Statistical analysis
Given an anticipated incidence rate of 20% for HF among older diabetic patients receiving right ventricular pacing (19), and targeting a statistical power of 80% at an alpha level of 0.05 in a two-sided hypothesis test, the study was designed to include 231 patients. The sample size calculation considers potential dropouts and non-response rates.
Continuous variables with normal distribution were represented as means ± standard deviation, and were compared using the independent sample t test. Continuous variables with skewed distribution were represented as median (25th quartile, 75th quartile), and were compared using the Wilcoxon rank sum test. Categorical variables were expressed as number (percentages) and were compared using the chi-squared test. Kaplan-Meier plots were used to determine the differences in the cumulative rates of HFH during the follow-up period in the normal, mild, and moderate-to-severe malnutrition groups. The survival data was compared using the log-rank test. Univariate Cox proportional hazard regression analysis was performed to identify the variables that showed significant correlation with HFH. These variables were then incorporated into the multivariate Cox regression models to determine the independent effects of malnutritional status on HFH based on the assessments from the four screening tools. The statistical data was analyzed using the R statistical software version 4.3.1. Two-tailed P value < 0.05 was considered statistically significant.
Results
Baseline clinical characteristics
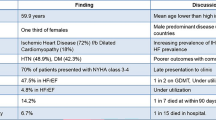
This study included 231 older diabetic patients (51.5% males and 48.5% females) that had received RVP for the first time. The median age was 76 years. The median fasting blood glucose and HbA1C concentrations were 6.7 mmol/L (25th quartile = 5.6 mmol/L, 75th quartile = 8.3 mmol/L) and 6.9% (6.3%, 7.7%), respectively. The pacing leads were placed within the RVS and the RVA in 35.1% and 64.9% of the study subjects, respectively. The ventricular pacing percentage ≥ 40% was observed in 71.4% of the study subjects. In the study cohort, 6.1% of patients were classified as NYHA II-IV before implantation. Furthermore, the median NT-pro BNP concentration was 357.7 pg/ml (158.6 pg/ml, 954.6 pg/ml) pg/ml, and the median LVEF was 63.0% (60.0%, 65.0%) before implantation. During the median follow-up period of 53 months, 19.9% of the patients revisited the hospital due to HF (Table 1).
Clinical features of preimplantation malnutrition
As shown in Table 1, 18.2%, 15.2%, 86.6%, and 66.2% of the patients were diagnosed with malnutrition before implantation based on the PNI, GNRI, NPS, and CONUT score, respectively.
Patients with preimplantation malnutrition were associated with older age, higher proportion of males, β blocker usage, preexisting coronary artery disease, HF or AF with slow HR, lower proportion of metformin use and SND, higher values for height, neutrophils, BUN, direct bilirubin, NT-pro BNP, and LAD, lower values for BMI, proportion of body fat, lymphocytes, red blood cells, hemoglobin, platelets, albumin, TC, HDL-C, LDL-C, total bilirubin, and HbA1C (Table 2).
Preimplantation malnutrition is associated with heart failure hospitalization
The cumulative rate of HFH during the follow-up period was significantly higher in patients with preimplantation malnutrition as identified by PNI (log-rank = 13.0, P = 0.001), GNRI (log-rank = 8.5, P = 0.01), and NPS (log-rank = 15.7, P < 0.001) compared to those with normal nutritional status, but was statistically insignificant based on the CONUT score (logrank = 2.7, P = 0.3) (Figure 2).
Univariate Cox proportional hazard regression analysis was performed to assess the prognostic significance of clinical indicators on HFH based on the hazard ratios. Univariate analysis results showed that age (HR = 1.06, 95% CI: 1.01–1.11, P = 0.019), NYHA II-IV (HR = 3.54, 95% CI: 1.59–7.92, P = 0.002), preexisting HF (HR = 4.66, 95% CI: 2.61–8.33, P < 0.001), use of β blocker (HR = 2.17, 95% CI: 1.14–4.12, P = 0.018), lg (NT-pro BNP) level (HR = 2.02, 95% CI: 1.53–2.67, P < 0.001), LAD (HR = 1.11, 95% CI: 1.06–1.16, P < 0.001), and LVEF (HR = 0.91, 95% CI: 0.87–0.95, P < 0.001) were associated with HFH (Table 3).
Subsequently, multivariate Cox proportional regression models were constructed by integrating the significant risk factors for HFH based on the results from the univariate regression analysis and all the nutritional indices. As continuous variables, all the nutritional indices showed significant correlation with HFH (all P < 0.05). However, only GNRI was independently associated with HFH (HR = 0.97, 95% CI: 0.937–0.997, P = 0.032). As categorical variables, PNI, GNRI, and NPS showed significant correlation with HFH (P < 0.05). After adjustment of potential confounding factors, including preexisting HF, use of β blocker, lg (NT-pro BNP) level, LAD, and LVEF, moderate-to-severe degree of malnutrition based on the PNI (HR = 4.66, 95% CI: 1.03–21.00, P = 0.045), and GNRI (HR = 3.02, 95% CI: 1.02–9.00, P = 0.047) were independently associated with HFH (Table 3).
Discussion
This study showed that preimplantation malnutrition was common in older diabetic patients receiving RVP. The cumulative rate of HFH was significantly higher for patients with preimplantation malnutrition according to the PNI, GNRI, and NPS data. As a continuous variable, only GNRI was independently associated with HFH. As categorical variables, after adjusting for the potential confounding covariates, the moderate-to-severe degree of malnutrition assessment based on PNI and GNRI data was independently related with HFH. However, malnutrition assessments based on the NPS and CONUT score were not associated with increased risk for HFH.
RVP is the main pacing strategy for patients with high-degree AVB and SND (2, 20, 21). In several cases, prolonged ventricular pacing caused asynchrony of the left ventricular contraction and gradually reduced cardiac function (22). Advanced age (7) and diabetes mellitus (8) were significant risk factors associated with HF progression. Therefore, early identification of the high-risk population is critical for improving the prognosis in older diabetic patients with RVP.
Malnutrition is associated with adverse clinical outcomes in cardiovascular diseases but is often neglected as a risk factor (9, 10). Echouffo-Tcheugui et al (14) and Yanagisawa et al (23) reported that underweight patients with HF that received implantable cardioverter-defibrillator (ICD) therapy were associated with poorer prognosis. Hsu et al analyzed global population cohort that received ICD and reported significantly higher rate of adverse events in the underweight recipients (13). Balli et al (12) and Yamaguchi et al (11) analyzed patients with bradycardia that received PPMI and demonstrated a positive correlation between the preprocedural malnutritional status and postoperative development of pacing-induced cardiomyopathy and all-cause mortality. However, very few studies have investigated the prognostic value of multiple malnutrition screening tools in older diabetic patients with RVP. In our study population, malnutrition was a common comorbidity in older diabetic patients that received PPMI. Furthermore, the cumulative rate of HFH was significantly higher in the malnutrition group.
Previous studies have reported the relationship between malnutrition and HF development (24, 25). HF is characterized by progressive cardiac remodeling, with inflammation and fibrosis playing a key role (26, 27). Dietary supplementation with n-3 polyunsaturated fatty acids induces anti-inflammatory and anti-oxidative effects that suppress the onset of HF (28). Vitamin D alleviates cardiac hypertrophy, fibrosis, and dysfunction (29, 30). ATP depletion and excessive generation of reactive oxygen species because of thiamine deficiency impaired myocardial contractility and resulted in HF (31, 32).
The risk of malnutrition varies between different settings. Moreover, the prevalence of malnutrition varies based on the type of malnutrition screening tools used. Therefore, it is recommended that an individual nutritional screening approach that is suitable for a specific population should be used to estimate malnutrition with consistency and accuracy (33). Previous studies have demonstrated the prognostic values of various malnutrition screening tools for the prediction of adverse outcomes in patients with PPMI.
GNRI was initially used to evaluate the risk of morbidity and mortality associated with malnutrition in the hospitalized geriatric patients (16, 34). The severe malnutritional status based on the GNRI analysis was an independent predictor of all-cause mortality in patients with bradycardia after receiving PPMI (HR = 4.49, P < 0.001) (11). Our results also showed that moderate-to-severe degree of malnutrition based on GNRI was independently associated with HFH. As a continuous variable, GNRI showed significant negative correlation with HFH.
PNI was originally used for evaluating older patients with cancer that underwent elective surgery (15). Balli et al demonstrated the negative relationship between PNI and pacing-induced cardiomyopathy in patients that underwent PPMI (12). The decreased PNI values relative to the baseline PNI values were independently associated with unfavorable outcomes (35). Likewise, our study demonstrated that moderate-to-severe malnutrition was an independent predictor of HFH.
On the contrary, the NPS value and CONUT score were not associated with HFH. This may be caused by the variables that were used by these tools to estimate the nutritional status. Both NPS and CONUT score use serum total cholesterol as one of the parameters to estimate malnutrition, and total cholesterol levels above 180 mg/dL (4.65 mmol/L) were regarded as normal. However, high cholesterol levels are significantly associated with increased risk of HF (36–38). Furthermore, cumulative prior exposure to LDL-C was significantly associated with an increased risk of incident cardiovascular events, including HF (39). Therefore, HF patients that were considered to have a normal nutritional status based on the NPS and CONUT score, may be at a higher risk of HFH.
Our study has several limitations Firstly, this was a retrospective study. Therefore, the results of this study should be interpreted with caution and would require further analysis in randomized-controlled prospective studies. Secondly, the malnutrition screening tools included in our study incorporated simple acquirable biomarkers from the clinical settings. In the future, information regarding weight loss, mobility, and neuropsychological problems should be assessed for a thorough and detailed evaluation of the nutritional status (40). Finally, although covariates were adjusted to reduce confounding effects in the multivariate regression analyses, there might be residual confounding factors.
Conclusions
Preimplantation malnutrition was highly prevalent in older diabetic patients receiving RVP and was associated with an increased risk of HFH. The prevalence and prognostic value of malnutrition showed significant differences among different malnutrition screening tools compared in this study. Our results showed that the PNI and GNRI could be feasible for rapid evaluation and risk stratification of the patients, based on nutritional status. These malnutrition screening tools showed high prognostic value for accurately predicting HFH in older diabetic patients with RVP.
Data availability statement: The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
References
Mond HG, Proclemer A. The 11th world survey of cardiac pacing and implantable cardioverter-defibrillators: calendar year 2009—a World Society of Arrhythmia’s project. Pacing Clin Electrophysiol 2011;34 (8):1013–27. https://doi.org/10.1111/J.1540-8159.2011.03150.x.
Glikson M, Nielsen JC, Kronborg MB, Michowitz Y, Auricchio A, Barbash IM, et al. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J 2021;42 (35):3427–520. https://doi.org/10.1093/eurheartj/ehab364.
Osiecki A, Kochman W, Witte KK, Manczak M, Olszewski R, Michalkiewicz D. Cardiomyopathy Associated with Right Ventricular Apical Pacing-Systematic Review and Meta-Analysis. J Clin Med 2022;11 (23). https://doi.org/10.3390/jcm11236889.
Safak E, Ince H, Gkouvatsou L, Schultheiss HP, Ortak J, Caglayan E, et al. Pacing-induced cardiomyopathy in chronic right ventricular apical pacing: a midterm follow-up study. Eur J Med Res 2019;24 (1):23. https://doi.org/10.1186/s40001-019-0386-5.
Zhang S, Zhou X, Gold MR. Left Bundle Branch Pacing: JACC Review Topic of the Week. J Am Coll Cardiol 2019;74 (24):3039–49. https://doi.org/10.1016/j.jacc.2019.10.039.
Rautio E, Gadler F, Gudbjornsdottir S, Franzen S, Ryden L, Svensson AM, et al. Patients With Type 2 Diabetes Have an Increased Demand for Pacemaker Treatment: A Comparison With Age- and Sex-Matched Control Subjects From the General Population. Diabetes Care 2020;43 (11):2853–8. https://doi.org/10.2337/dc20-0084.
Li H, Hastings MH, Rhee J, Trager LE, Roh JD, Rosenzweig A. Targeting Age-Related Pathways in Heart Failure. Circ Res 2020;126 (4):533–51. https://doi.org/10.1161/CIRCRESAHA.119.315889.
Rawshani A, Rawshani A, Franzen S, Sattar N, Eliasson B, Svensson AM, et al. Risk Factors, Mortality, and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N Engl J Med 2018;379 (7):633–44. https://doi.org/10.1056/NEJMoa1800256.
Chien SC, Chandramouli C, Lo CI, Lin CF, Sung KT, Huang WH, et al. Associations of obesity and malnutrition with cardiac remodeling and cardiovascular outcomes in Asian adults: A cohort study. PLoS Med 2021;18 (6):e1003661. https://doi.org/10.1371/journal.pmed.1003661.
Wawrzenczyk A, Anaszewicz M, Wawrzenczyk A, Budzynski J. Clinical significance of nutritional status in patients with chronic heart failure-a systematic review. Heart Fail Rev 2019;24 (5):671–700. https://doi.org/10.1007/s10741-019-09793-2.
Yamaguchi T, Nozato T, Miwa N, Sagawa Y, Watanabe K, Nagata Y, et al. Impact of the preprocedural nutrition status on the clinical outcomes of patients after pacemaker implantation for bradycardia. J Cardiol 2019;74 (3):284–9. https://doi.org/10.1016/j.jjcc.2019.02.011.
Balli M, Cetin M, Koksal F, Sag FE, Katkat F, Tekin EE, et al. Predictors of Pacemaker-Induced Cardiomyopathy and Importance of Nutritional Status and Prognostic Nutritional Index. Acta Cardiol Sin 2022;38 (2):151–8. https://doi.org/10.6515/ACS.202203_38(2).20211117A.
Hsu JC, Varosy PD, Bao H, Wang Y, Curtis JP, Marcus GM. Low body mass index but not obesity is associated with in-hospital adverse events and mortality among implantable cardioverter-defibrillator recipients: insights from the National Cardiovascular Data Registry. J Am Heart Assoc 2012;1 (6):e003863. https://doi.org/10.1161/JAHA.112.003863.
Echouffo-Tcheugui JB, Masoudi FA, Bao H, Curtis JP, Heidenreich PA, Fonarow GC. Body mass index and outcomes of cardiac resynchronization with implantable cardioverter-defibrillator therapy in older patients with heart failure. Eur J Heart Fail 2019;21 (9):1093–102. https://doi.org/10.1002/ejhf.1552.
Cadwell JB, Afonso AM, Shahrokni A. Prognostic nutritional index (PNI), independent of frailty is associated with six-month postoperative mortality. J Geriatr Oncol 2020;11 (5):880–4. https://doi.org/10.1016/j.jgo.2020.03.013.
Bouillanne O, Morineau G, Dupont C, Coulombel I, Vincent JP, Nicolis I, et al. Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr 2005;82 (4):777–83. https://doi.org/10.1093/ajcn/82.4.777.
Galizia G, Lieto E, Auricchio A, Cardella F, Mabilia A, Podzemny V, et al. Naples Prognostic Score, Based on Nutritional and Inflammatory Status, is an Independent Predictor of Long-term Outcome in Patients Undergoing Surgery for Colorectal Cancer. Dis Colon Rectum 2017;60 (12):1273–84. https://doi.org/10.1097/DCR.0000000000000961.
Wada H, Dohi T, Miyauchi K, Doi S, Konishi H, Naito R, et al. Prognostic impact of nutritional status assessed by the Controlling Nutritional Status score in patients with stable coronary artery disease undergoing percutaneous coronary intervention. Clin Res Cardiol 2017;106 (11):875–83. https://doi.org/10.1007/s00392-017-1132-z.
Smit MD, Van Dessel PF, Nieuwland W, Wiesfeld AC, Tan ES, Anthonio RL, et al. Right ventricular pacing and the risk of heart failure in implantable cardioverter-defibrillator patients. Heart Rhythm 2006;3 (12):1397–403. https://doi.org/10.1016/j.hrthm.2006.08.006.
Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR, et al. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation 2019;140 (8):e382–e482. https://doi.org/10.1161/CTR.0000000000000628.
Naqvi TZ, Chao CJ. Adverse effects of right ventricular pacing on cardiac function: prevalence, prevention and treatment with physiologic pacing. Trends Cardiovasc Med 2023;33 (2):109–22. https://doi.org/10.1016/j.tcm.2021.10.013.
Merkely B, Hatala R, Wranicz JK, Duray G, Foldesi C, Som Z, et al. Upgrade of right ventricular pacing to cardiac resynchronisation therapy in heart failure: a randomised trial. Eur Heart J 2023. https://doi.org/10.1093/eurheartj/ehad591.
Yanagisawa S, Inden Y, Shimano M, Yoshida N, Ishikawa S, Kato H, et al. Impact of cardiac resynchronization therapy-defibrillator implantation on the association between body mass index and prognosis in patients with heart failure. J Interv Card Electrophysiol 2015;43 (3):269–77. https://doi.org/10.1007/s10840-015-0015-3.
Billingsley HE, Hummel SL, Carbone S. The role of diet and nutrition in heart failure: A state-of-the-art narrative review. Prog Cardiovasc Dis 2020;63 (5):538–51. https://doi.org/10.1016/j.pcad.2020.08.004.
Khan MS, Khan F, Fonarow GC, Sreenivasan J, Greene SJ, Khan SU, et al. Dietary interventions and nutritional supplements for heart failure: a systematic appraisal and evidence map. Eur J Heart Fail 2021;23 (9):1468–76. https://doi.org/10.1002/ejhf.2278.
Murphy SP, Ibrahim NE, Januzzi JL,Jr. Heart Failure With Reduced Ejection Fraction: A Review. JAMA 2020;324 (5):488–504. https://doi.org/10.1001/jama.2020.10262.
Mishra S, Kass DA. Cellular and molecular pathobiology of heart failure with preserved ejection fraction. Nat Rev Cardiol 2021;18 (6):400–23. https://doi.org/10.1038/s41569-020-00480-6.
Oppedisano F, Mollace R, Tavernese A, Gliozzi M, Musolino V, Macri R, et al. PUFA Supplementation and Heart Failure: Effects on Fibrosis and Cardiac Remodeling. Nutrients 2021;13 (9). https://doi.org/10.3390/nu13092965.
Latic N, Erben RG. Vitamin D and Cardiovascular Disease, with Emphasis on Hypertension, Atherosclerosis, and Heart Failure. Int J Mol Sci 2020;21 (18). https://doi.org/10.3390/ijms21186483.
de la Guia-Galipienso F, Martinez-Ferran M, Vallecillo N, Lavie CJ, Sanchis-Gomar F, Pareja-Galeano H. Vitamin D and cardiovascular health. Clin Nutr 2021;40 (5):2946–57. https://doi.org/10.1016/j.clnu.2020.12.025.
Eshak ES, Arafa AE. Thiamine deficiency and cardiovascular disorders. Nutr Metab Cardiovasc Dis 2018;28 (10):965–72. https://doi.org/10.1016/j.numecd.2018.06.013.
Bomer N, Pavez-Giani MG, Grote Beverborg N, Cleland JGF, van Veldhuisen DJ, van der Meer P. Micronutrient deficiencies in heart failure: Mitochondrial dysfunction as a common pathophysiological mechanism? J Intern Med 2022;291 (6):713–31. https://doi.org/10.1111/joim.13456.
Leij-Halfwerk S, Verwijs MH, van Houdt S, Borkent JW, Guaitoli PR, Pelgrim T, et al. Prevalence of protein-energy malnutrition risk in European older adults in community, residential and hospital settings, according to 22 malnutrition screening tools validated for use in adults >/=65 years: A systematic review and meta-analysis. Maturitas 2019;126:80–9. https://doi.org/10.1016/j.maturitas.2019.05.006.
Seron-Arbeloa C, Labarta-Monzon L, Puzo-Foncillas J, Mallor-Bonet T, Lafita-Lopez A, Bueno-Vidales N, et al. Malnutrition Screening and Assessment. Nutrients 2022;14 (12). https://doi.org/10.3390/nu14122392.
Wang K, Lian L, Chen C, Wang M, Chen C, Hu X. The change in nutritional status is related to cardiovascular events in patients with pacemaker implantation: A 4-year follow-up study. Front Nutr 2022;9:986731. https://doi.org/10.3389/fnut.2022.986731.
Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2022;79 (17):e263–e421. https://doi.org/10.1016/j.jacc.2021.12.012.
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation 2019;139 (10):e56–e528. https://doi.org/10.1161/CIR.0000000000000659.
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;73 (24):e285–e350. https://doi.org/10.1016/j.jacc.2018.11.003.
Domanski MJ, Tian X, Wu CO, Reis JP, Dey AK, Gu Y, et al. Time Course of LDL Cholesterol Exposure and Cardiovascular Disease Event Risk. J Am Coll Cardiol 2020;76 (13):1507–16. https://doi.org/10.1016/j.jacc.2020.07.059.
Dent E, Wright ORL, Woo J, Hoogendijk EO. Malnutrition in older adults. Lancet 2023;401 (10380):951–66. https://doi.org/10.1016/S0140-6736(22)02612-5.
Acknowledgements
None
Funding
Funding: No
Author information
Authors and Affiliations
Contributions
Author contribution: WH, BQF, and YY participated in the study design. BQF, YY, SJC, HH, TXL, JWY, MG, CC, XHC, and HXN participated in data collection and data cleaning. BQF and YY performed the statistical analysis and constructed the manuscript, which was revised and approved by all the authors for publication.
Corresponding author
Ethics declarations
Conflict of interest: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethic statement: The study was approved by the Ethics Committee of the Chinese Academy of Medical Sciences, Fuwai Hospital (NO.IRB2012-BG-006), and written informed consents were obtained from all the patients involved in this study.
Rights and permissions
Open Access: This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, duplication, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author (s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
About this article
Cite this article
Fu, B., Yu, Y., Cheng, S. et al. Prognostic Value of Four Preimplantation Malnutrition Estimation Tools in Predicting Heart Failure Hospitalization of the Older Diabetic Patients with Right Ventricular Pacing. J Nutr Health Aging 27, 1262–1270 (2023). https://doi.org/10.1007/s12603-023-2042-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-023-2042-6