Abstract
Introduction
Most asthma patients have mild disease, although the burden of mild asthma is not well understood nor studied. Some evidence suggests that many patients with mild asthma experience suboptimal symptom control and exacerbations. This study characterizes the burden of illness and treatment patterns among patients with a confirmed diagnosis of mild asthma, defined as GINA Step 1 or Step 2, and residing in China, France, Germany, Italy, Japan, Spain, the United Kingdom, or the United States.
Methods
The Respiratory Disease-Specific Programme prospective cross-sectional survey was conducted with primary care and specialty physicians in each of the eight countries. Physician and patient surveys assessed demographic and clinical characteristics, frequency and timing of asthma symptoms, exacerbations, and rescue inhaler usage, the most recent FEV1% predicted, and healthcare utilization. GINA Step was determined by prescribed treatment regimen. GINA Step 1 patients were prescribed as-needed reliever medication and Step 2 required treatment with a low-dose inhaled corticosteroid, leukotriene receptor antagonist, or theophylline. Treatment adherence was assessed with the Morisky Medication Adherence scale, disease control with the Asthma Control Test, and work and activity impairments with the Work Productivity and Activity Impairment scale.
Results
The sample included 1115 GINA Step 1 and 2 patients, with 53% classified as Step 2. Overall asthma control was suboptimal, with reports of nocturnal symptoms (40.6%), symptom worsening (10.5%), and rescue inhaler usage in the last 4 weeks (33.6%). 25% of patients were uncontrolled. The overall mean number of exacerbations in the last 12 months was 0.4, with a higher frequency of exacerbations in Step 2 patients who also experienced more exacerbations requiring treatment intensification, an emergency department visit, or hospitalization.
Conclusion
Mild asthma imposes a substantial burden on patients, establishing the need for comprehensive management plans and ongoing support for treatment adherence.
Funding
AstraZeneca.
Similar content being viewed by others
Introduction
Asthma is a common, chronic respiratory disease estimated to affect 235–334 million people worldwide [1]. Characteristic symptoms include wheezing, shortness of breath, chest tightness and/or cough, and expiratory airflow limitation, with symptoms typically varying over time in frequency and intensity [1, 2]. Treatment goals emphasize symptom control, maintenance of normal activity levels, and reduced risk of future exacerbations, fixed airflow limitations, and medication side effects. Importantly, treatment options are guided by disease severity [2, 3].
According to the Global Initiative for Asthma (GINA), severity can be determined after several months of controller treatment based on the type of therapy required for optimal control of symptoms and exacerbations [2]. Mild asthma is asthma that is well controlled with GINA Step 1 or Step 2 treatment with as-needed reliever medication monotherapy or low-intensity controller treatment, such as low-dose inhaled corticosteroids (ICS), leukotriene receptor antagonists (LTRAs), or theophylline [2].
Severe asthma is viewed as a major unmet health need and is the focus of research and international guidelines, consensus statements, and recommendations to improve patient management and outcomes [2, 4–6]. Results from epidemiologic studies typically do not distinguish between categories of asthma severity, although it is widely accepted that most patients have mild or very mild disease, fewer have moderate disease and fewer still have severe disease [7]. As many as 70% of all asthmatics are thought to have mild persistent disease, [8] with one population-based cohort study of more than 150,000 patients from British Columbia from 1996 to 2000 reporting mild asthma in 67.1% of patients [9].
Of note, the burden of mild asthma is not well understood nor studied, although some evidence suggests control is suboptimal and potentially due to inadequate treatment [10]. Patients with mild or moderate asthma experience exacerbations [11], and approximately 40% of almost 2000 patients with mild asthma reported days with symptoms [12].
While optimal control and prevention of future complications is important for all levels of asthma severity [13], this survey characterizes the global treatment patterns and the burden of illness among individuals with mild asthma who consulted physicians for routine care, with patients residing in China, France, Italy, Japan, Spain, the United Kingdom, or the United States.
Methods
Study Design
Data were analyzed from the Respiratory Disease-Specific Programme (DSP), a large, multinational, prospective, cross-sectional survey that collects real-world data from primary care and specialist physicians and their patients, with a full description of methods reported previously [14].
Surveys were undertaken in France, Germany, Italy, Spain, the UK, and the USA (2013), Japan (2012) and China (2010). Consenting physicians completed patient record forms for five consecutive patients diagnosed with asthma, with these patients then invited to complete a patient questionnaire at the end of their visit with the physician. Consenting patients responded to the survey confidentially. Unique identification numbers assigned to physicians and patients permitted linked analysis of the completed surveys. Physician- and patient-completed forms were collected by local fieldworkers, with identifying information removed before submission of surveys for analysis.
The research was conducted as a market research survey in accordance with the amended Declaration of Helsinki, adhering to the ICC/ESOMAR International code on observational research, and performed in full accordance with the rules of the US Health Insurance Portability and Accountability Act 1996. IRB approval was not necessary nor sought.
Study Participants
Physician eligibility criteria included completion of medical training in the last 5–35 years, treatment of patients with asthma, and responsible for the care of at least three patients with asthma per month. Inclusion criteria for patients were 12 years or older with a physician-confirmed diagnosis of mild asthma, categorized as GINA Step 1 (intermittent based on as-needed reliever medication) or GINA Step 2 (mild persistent asthma requiring treatment with a low-dose ICS, LTRA, or theophylline) [2]. Patients who declined to respond to the survey for whom a physician-completed form was obtained were not excluded from analyses.
Variables and Assessments
The survey obtained physician- and patient-reported demographic and clinical characteristics including age, smoking history, employment status, education, body mass index (BMI), comorbidities, and results of the most recent FEV1% predicted. GINA Step was determined by patient’s prescribed treatment regimen at the time of survey completion based on the medical record.
Physicians reported the frequency and timing of asthma symptoms during the past 4-week interval. This information was obtained during their examination and interaction with patients and based on patient report of symptoms. Exacerbations were defined as physician-confirmed worsening of symptoms beyond normal day-to-day variation, and treatment(s) prescribed for exacerbations including hospitalizations, emergency department (ED) visits, and use of rescue inhalers. Physicians reported the number of asthma exacerbations during the 12 months preceding the survey, which was intended to reduce the likelihood of variations in exacerbation rates that could be attributed to different allergy seasons in each country.
Physician- and patient-reported perceptions of asthma control were recorded on a five-point scale ranging from not at all controlled to completely controlled. The validated Asthma Control Test (ACT) [15] was also used to assess patient-reported control of their disease. ACT scores less than 20 indicated not well-controlled or poorly-controlled asthma. Patient-reported adherence to their asthma treatment was assessed with the Morisky Medication Adherence scale (MMAS-8) [16], which was modified in accordance with information provided by Dr. Morisky to adapt the scale for other chronic diseases. The MMAS-8 has been validated for use in several different countries and in patients with various chronic health conditions [17] including hypertension [18, 19], diabetes [20, 21], and osteoporosis [22]. The 8-item questionnaire assesses general adherence to medications that are taken daily and provided a measure of adherence among GINA Step 2 patients to their prescribed controller therapy [16]. The MMAS-8 and ACT were not completed by patients in Japan or China because validated translations were not available.
Patients also reported frequency of rescue inhaler use and exacerbations in the last 4 weeks, the number of visits related to their asthma or asthma symptoms to any physician in the preceding 12 months, and the number of lost days at work. The Work Productivity and Activity Impairment (WPAI) Specific Health Problem questionnaire was completed by patients, which yields four types of scores for absenteeism, presenteeism, total work productivity loss, and total activity impairment in the last 7 days. Higher scores indicated greater impairment and less productivity [23].
Statistical Methods
Descriptive statistics were reported for all variables. The maximum sample available for each variable was used. There was no replacement of subjects if they did not respond to the survey. Results were stratified by GINA Steps 1 and 2. All analyses were performed with Stata 13.1 [24].
Results
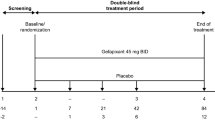
Eligible physicians completed 5811 physician-reported surveys. The eligible study sample included 1115 patients for whom a physician-reported form was completed. Of these, 595 patients declined to participate in the survey and 520 patients completed surveys (Fig. 1). A comparison of demographic and clinical characteristics for patients who completed the survey and those who declined to participate in this research revealed few differences with respect to sex, race, ethnicity, BMI, smoking status, comorbid health conditions, the occurrence of exacerbations, and medication adherence. Survey respondents were slightly younger with a mean age of 36.8 years compared to 40.4 years for nonrespondents. A higher proportion of nonrespondents (39.2%) were prescribed ICS compared to 29.6% of survey participants.
GINA Step 1 patients comprised 47% of the total sample. The highest percentage of patients on rescue-only medications and classified as GINA Step 1 was 64.3% in Germany, whereas the highest percentage of GINA Step 2 patients resided in Japan at 78.9% and the UK at 76.9% (Table 1).
Demographic and Clinical Characteristics
The mean patient age was 38.4 years. Slightly more than 50% of the overall sample was female, with approximately three-quarters categorised as White/Caucasian. A higher percentage of Step 1 patients were current smokers at 12.5% versus 8.2% of GINA Step 2 patients (Table 2).
FEV1 lung function evaluations indicated a higher percent predicted for patients at GINA Step 1. Approximately one-third of all patients had no physician-confirmed comorbid health conditions. Allergic rhinitis was the most frequently diagnosed comorbidity among patients (38.8%). Physicians identified asthma as the primary health concern for approximately 75% of patients (Table 2).
Asthma Treatment Regimens and Adherence
Almost two-thirds of GINA Step 2 patients were currently prescribed low-dose ICS (Table 3). Xanthine monotherapy was used by only 5.6% of Step 2 patients, with the majority of these residing in Japan and China. Primary care physicians were the sole provider of care for 47.3% of patients overall, with a slightly lower proportion of GINA Step 2 patients treated only by primary care clinicians. Treatment adherence rates based on the MMAS-8 [16] for all GINA Step 2 patients who were prescribed regular maintenance medication were low for 35.6% of patients, medium for 38.1%, and high for 26.3%.
Asthma Control
There were minimal differences between patient groups with respect to patients identifying themselves as having poorly-controlled asthma. Only 2.9% of patients overall, 2.9% of GINA Step 1, and 2.8% of GINA Step 2 patients self-classified as poorly controlled or uncontrolled. Physician ratings indicated that 3.5% of Step 1 patients and 7.1% of Step 2 patients had poorly-controlled or uncontrolled asthma (Fig. 2i, ii). However, ACT scores for patients revealed that 25.3% overall had scores less than 20, indicating that they were not well controlled. Patients with lower ACT scores accounted for a higher proportion of those using reliever inhalers ≥3 times a week (Fig. 3).
There were some demographic and clinical differences between patients who were well controlled and those who were poorly controlled or uncontrolled based on ACT scores (Table 4). Poorly-controlled patients were more likely to be female (58.1%) and current smokers (12.4%) compared to 50.7% female and 8.5% current smokers of those classified as well controlled. Mean BMI was higher at 25.6 mg/kg2 (SD 5.3) for poorly-controlled asthmatics compared to 24.4 mg/kg2 (SD 4.4) for those with well-controlled disease. Patients with poorly-controlled asthma were more likely to have comorbid anxiety (8.5%) and depression (10.1%) versus 4.5% with anxiety and 2.1% with depression in patients who were well controlled. A higher percentage of patients who reported poor asthma control on the ACT were treated with ICS alone (40.3%) while 54.5% of well-controlled patients were prescribed short-acting beta2-agonist (SABA) or short-acting muscarinic antagonist (SAMA) monotherapy.
ACT scores for all GINA Step 2 patients revealed low adherence for 43.9% of poorly-controlled patients compared to 32.1% of those with ACT scores indicating good control. Medium adherence was evident for 37.9% and 37.7% of poorly- and well-controlled GINA Step 2 patients, respectively. High adherence was reported by 18.2% of poorly-controlled patients and 30.2% of those who were well controlled.
Asthma Symptoms
The most frequently reported symptom was shortness of breath during exertion for 30.9% of patients overall, 28.4% of GINA Step 1, and 33.0% of GINA Step 2 patients. Overall, 40.6% of patients reported nocturnal symptoms, including symptoms occurring equally during the day and night, primarily during the night, and nighttime only. This was slightly higher than the prevalence of physician-reported nocturnal symptoms at 36.5% for these same three categories. Nocturnal symptoms during the day and night, primarily during the night, and nighttime only were indicated by 36.8% of Step 1 patients and 44.6% of those at Step 2 compared with physician-reported rates of 34.3% and 38.4%, respectively (Table 5).
Among patients prescribed rescue therapy, 8.5% of Step 1 and 10.9% of Step 2 patients reported rescue inhaler use >2 times per week in the 4 weeks preceding the survey. The frequency of rescue inhaler use was similar between Step 1 and 2 patients with the exception of daily use, which was reported twice as frequently by Step 2 patients (Table 5). Mean overall work impairment due to asthma was 13.3%, while mean activity impairment was 14.2% (Table 5).
Asthma Exacerbations
The majority of patients reported no significant worsening of asthma symptoms in the last 4 weeks. However, 9.1% of Step 1 and 11.7% of Step 2 patients indicated increased symptom severity at least once or twice per week during the 4 weeks preceding the survey. The mean number of exacerbations of any severity occurring in the last 12 months for both Step 1 and Step 2 patients was 0.4, with 19% of all patients experiencing one or more exacerbations (Table 6).
The overall mean number of moderate-to-severe exacerbations (requiring oral corticosteroids, antibiotics, treatment in the ED or hospital admission) was 0.2. Overall, 12.5% of patients had at least one moderate-to-severe exacerbation, with a higher percentage of GINA Step 2 patients experiencing exacerbations that required temporary intensification of medical therapy with oral corticosteroids or antibiotics, treatment in the ED, or hospitalization (Table 6).
Discussion
Extensive research and clinical emphasis has been placed on evaluation of the impact of severe asthma on patients and healthcare systems, with new biologic treatments in development specifically to address the unmet needs of these patients [3, 25]. Patients with mild asthma defined by GINA Steps 1 or 2 are generally expected to have good or complete control of symptoms and have a low risk for exacerbations.
Our results indicate similarities between physician and patient evaluations of asthma control. Only 2.9% of patients overall considered themselves poorly controlled, while 3.5% of Step 1 patients and 7.1% of Step 2 patients were considered poorly controlled by their physicians. However, a relatively large proportion of patients were not well controlled according to the ACT, a validated, objective assessment of asthma control.
Other assessments of asthma symptoms and exacerbations included overall patient-reported occurrence of nocturnal symptoms (40.6%), one or more significant worsening of symptoms in the last 4 weeks (10.5%), and rescue inhaler usage more than twice per week (9.7%). Further, assessment of asthma control revealed that approximately 25% of patients fell below the threshold of 20 on the ACT, which is considered an indication of poorly-controlled asthma. Other research incorporating objective assessments of asthma control and risk for exacerbations reveals that a significant proportion of patients with mild asthma are symptomatic, experience exacerbations, and are not well controlled [9, 11, 13].
For example, an observational, cross-sectional, community-based study evaluated the level of control in 950 adult patients with mild asthma who were regularly treated by general practitioners, with more than 80% prescribed ICS [10]. Of these, only 13.7% were considered totally controlled (ACT score of 25), 51.0% well controlled (ACT score of 20–24), and 35.3% were classified as not well controlled or poorly controlled (ACT score ≤19) [10]. Patients with poorly-controlled asthma were at significantly greater risk for asthma-related unscheduled visits to specialists, ED, and hospital admissions [10].
Research suggests many patients perceive their asthma as controlled and not serious despite the occurrence of symptoms and exacerbations [26–28]. It has been suggested that patients with mild disease may accept their symptoms and have lower adherence to preventive therapy, possibly due to a lack of understanding that therapy will control current symptoms and reduce the risk of future disease progression [13, 28].
Frequency of rescue inhaler usage, although subject to variability, can be a useful proxy for asthma control. Patients may use as-needed relievers frequently but consider themselves well controlled because rescue therapy prevents their symptom escalation. However, clinicians perceive the use of rescue therapy as an indicator of poor asthma control. Our results show less frequent use of rescue inhalers was associated with better control characterized by higher ACT scores. This suggests that accurate information about the frequency of rescue inhaler usage can be a useful proxy to assess control in the absence of reported symptoms. One or more exacerbations in the preceding 12 months was reported by 19% of mild asthma patients overall experienced. This suggests that approximately one in five patients with mild asthma might benefit from treatment intensification [2]. These results are consistent with those reported from an earlier Respiratory DSP survey [29] and highlight the persistence of unmet needs for a significant proportion of mild asthma patients.
Approximately half of patients were employed full-time and about 20% were full-time students. While the mean level of absenteeism was low, the mean impact of asthma on productivity, overall work impairment, and activity impairment ranged from 12% to 16%. This provides an indication of the indirect economic costs and restrictions on patient’s ability to perform normal daily activities due to mild asthma. GINA Step 1 patients reported less work-related impairments compared to those classified as GINA Step 2, suggesting higher indirect costs and greater disease burden for Step 2 patients.
Low adherence was evident for approximately a third of patients in this survey. Further, a substantial proportion of patients were considered by their physician to underestimate the seriousness of their condition (data not shown). This is consistent with findings from an international survey of more than 10,000 asthma patients, which found that self-reported classification of symptom control was not aligned with guideline-based classification of control [30]. These findings may reflect low patient concern about their condition, placing them at increased risk for future worsening of their disease.
It is conceivable that patients are unaware of the distinction between poor and good asthma control and may not understand how their symptoms could be better controlled with appropriate medical therapy. 64.4% of GINA Step 2 patients were classified as of medium or high adherence. This is slightly higher than adherence rates reported in other studies, which estimate that 50% of patients diagnosed with mild, moderate, and severe asthma adhered to their treatment regimen, [31] but is dependent on the measurement of adherence. Improved adherence may be achieved through implementation and ongoing review of asthma action plans and ongoing patient education regarding the importance of adherence and is recommended by treatment guidelines for patients with asthma of all degrees of severity [2, 32].
Written personalized asthma action plans are considered an essential component of a self-management program for people with asthma [32, 33]. An evidence-based review found that individualized written plans were associated with decreases in hospital admissions, ED visits, unscheduled outpatient appointments and improvements in markers of asthma control and patient quality of life [32, 34]. While we did not collect information about asthma action plans in this survey, patients with action plans were not excluded from participation. Future surveys will include questions to assess whether patients have asthma action plans and any associations between such plans, treatment modifications, and the management of mild asthma.
Limitations
Patients included in the Respiratory DSP sample were not a true random sample, since study methods specified inclusion of five consecutive patients who consulted their physician and met study eligibility criteria. However, prospective consecutive sampling does limit bias that might be attributable to pre-selection of patients by the physician.
Our findings are representative of patients consulting a primary care physician or specialist for routine care, which may limit generalizability to the general population of mild asthmatics. There is the possibility of differences between patients who agreed to complete the survey and those who declined.
The diagnosis of asthma was confirmed by physicians and dependent on their diagnostic skills. However, this is a common and well-accepted method for the identification and recruitment of samples in real-world research. More than one-half of patients overall did not have results for pre-bronchodilation FEV1% and 66.3% of all patients had missing results for post-bronchodilation FEV1% data, with similar proportions of missing data for Step 1 and 2 patients. This is consistent with general clinical practice where it has been reported that spirometry is infrequently used to assess asthma control and treatment effectiveness in community-dwelling patients with asthma [35–37].
Data on asthma symptoms were not collected at a universally-recognized allergy season, which was not possible given the number of countries and variations between countries in the timing of the allergy season. Therefore, the burden related to asthma symptoms described here could be an underestimation compared with the asthma burden associated with allergy season.
The quality of the data depended on accurate reporting by physicians and patients. Physicians were permitted to refer to patient records, which was intended to reduce errors in reporting treatment, clinical events and comorbidities. The majority of patient questions focused on current or recent circumstances, which helped reduce recall bias.
Physician inclusion in our study was potentially influenced by their willingness to participate. We imposed minimal eligibility criteria associated with the number of asthma patients seen and active involvement in the management of asthma patients. Thus, physicians were likely to be representative of the general population of clinicians caring for patients with asthma.
Conclusion
While patients with mild asthma are expected to have good or complete control of symptoms and a low risk for exacerbations, our results suggest a sizeable number are not well controlled according to objective assessments. Treatment adherence was suboptimal for approximately three-quarters of Step 2 patients. Interventions to promote adherence have the potential to improve outcomes for some of these patients, although it remains a possibility that treatment intensification may offer additional clinical benefits.
References
The Global Asthma Report 2014. Auckland, New Zealand: Global Asthma Network.
Global Initiative for Asthma. Global strategy for asthma management and prevention. 2015. www.ginasthma.org.
Reddel HK, Taylor DR, Bateman ED, et al. American thoracic society/european respiratory society task force on asthma control and exacerbations. An official American thoracic society/European respiratory society statement: asthma control and exacerbations: standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med. 2009;180(1):59–99.
Bel EH, Sousa A, Fleming L, et al. Unbiased biomarkers for the prediction of respiratory disease outcome (U-BIOPRED) consortium, consensus generation. Diagnosis and definition of severe refractory asthma: an international consensus statement from the Innovative Medicine Initiative (IMI). Thorax. 2011;66(10):910–7.
Chung KF, Wenzel SE, Brozek JL, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43(2):343–73.
Jarjour NN, Erzurum SC, Bleecker ER, et al. NHLBI Severe asthma research program (SARP). Severe asthma: lessons learned from the national heart, lung, and blood institute severe asthma research program. Am J Respir Crit Care Med. 2012;185(4):356–62.
Chapman KR. Impact of ‘mild’ asthma on health outcomes: findings of a systematic search of the literature. Respir Med. 2005;99(11):1350–62.
O’Byrne PM. How much is too much? The treatment of mild asthma. Eur Respir J. 2007;30(3):403–6.
Sadatsafavi M, Lynd L, Marra C, et al. Direct health care costs associated with asthma in British Columbia. Can Respir J. 2010;17(2):74–80.
Caminati M, Bettoncelli G, Magnoni MS, et al. The level of control of mild asthma in general practice: an observational community-based study. J Asthma. 2014;51(1):91–6.
Dennis RJ, Solarte I, Rodrigo G. Asthma in adults. BMJ Clin Evid. 2011 (pii: 1512).
O’Byrne PM, Barnes PJ, Rodriguez-Roisin R, et al. Low dose inhaled budesonide and formoterol in mild persistent asthma: the OPTIMA randomized trial. Am J Respir Crit Care Med. 2001;164(8 Pt 1):1392–7.
Shahidi N, Fitzgerald JM. Current recommendations for the treatment of mild asthma. J Asthma Allergy. 2010;3:169–76.
Anderson P. Real-world physician and patient behavior across countries: disease-Specific Programmes—a means to understand. Curr Med Res Opin. 2008;24(11):3063–72.
Morisky DE, Ang A, Krousel-Wood M, Ward H. Predictive validity of a medication adherence measure for hypertension control. J Clin Hypertens. 2008;10(5):348–54.
Plakas S, Mastrogiannis D, Mantzorou M, et al. Validation of the 8-item Morisky Medication Adherence Scale in chronically ill ambulatory patients in rural Greece. Open J Nurs. 2016;6:158–69.
de Oliveira-Filho AD, Morisky DE, Neves SJ, Costa FA, de Lyra DP Jr. The 8-item Morisky medication adherence scale: validation of a Brazilian-Portuguese version in hypertensive adults. Res Soc Adm Pharm. 2014;10(3):554–61.
Korb-Savoldelli V, Gillaizeau F, Pouchot J, et al. Validation of a French version of the 8-item Morisky medication adherence scale in hypertensive adults. J Clin Hypertens (Greenwich). 2012;14(7):429–34.
Sakthong P, Chabunthom R, Charoenvisuthiwongs R. Psychometric properties of the Thai version of the 8-item Morisky Medication Adherence Scale in patients with type 2 diabetes. Ann Pharmacother. 2009;43(5):950–7.
Wong MC, Wu CH, Wang HH, et al. Association between the 8-item Morisky medication adherence scale (MMAS-8) score and glycaemic control among Chinese diabetes patients. J Clin Pharmacol. 2015;55(3):279–87.
Reynolds K, Viswanathan HN, O’Malley CD, et al. Psychometric properties of the Osteoporosis-specific Morisky Medication Adherence Scale in postmenopausal women with osteoporosis newly treated with bisphosphonates. Ann Pharmacother. 2012;46(5):659–70.
Nathan RA, Sorkness CA, Kosinski M, et al. Development of the asthma control test: A survey for assessing asthma control. J Allergy Clin Immunol. 2004;113(1):59–65.
Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. PharmacoEconomics. 1993;4(5):353–65.
StataCorp. Stata statistical software: release 13. College Station: StataCorp LP; 2013.
Kupczyk M, Wenzel S. US and European severe asthma cohorts: what can they teach us about severe asthma? J Intern Med. 2012;272(2):121–32.
Price D, Fletcher M, van der Molen T. Asthma control and management in 8,000 European patients: the REcognise Asthma and LInk to symptoms and experience (REALISE) survey. NPJ Prim Care Respir Med. 2014;24:14009.
Price D, David-Wang A, Cho SH, et al. Time for a new language for asthma control: results from REALISE Asia. J Asthma Allergy. 2015;8:93–103.
Rabe KF, Adachi M, Lai CK, et al. Worldwide severity and control of asthma in children and adults: the global asthma insights and reality surveys. J Allergy Clin Immunol. 2004;114(1):40–7.
Roberts J, Williams A. Quality of life and asthma control with low-dose inhaled corticosteroids. Br J Nurs. 2004;13(19):1124–9.
Nathan RA, Thompson PJ, Price D, et al. Taking aim at asthma around the world: global results of the asthma insight and management survey in the Asia-Pacific Region, Latin America, Europe, Canada, and the United States. J Allergy Clin Immunol Pract. 2015;3(5):734–42.
Chiu KC, Boonsawat W, Cho SH, et al. Patient’s beliefs and behaviors related to treatment adherence in patients with asthma requiring maintenance treatment in Asia. J Asthma. 2014;51(6):652–9.
Pinnock H. Supported self-management for asthma. Breathe (Sheff). 2015;11(2):98–109.
Ring N, Malcolm C, Wyke S, et al. Promoting the use of personal asthma action plans: a systematic review. Prim Care Respir J. 2007;16(5):271–83.
Gibson PG, Powell H. Written action plans for asthma: an evidence-based review of the key components. Thorax. 2004;59(2):94–9.
Dennis SM, Zwar NA, Marks GB. Diagnosing asthma in adults in primary care: a qualitative study of Australian GPs’ experiences. Prim Care Respir J. 2010;19(1):52–6.
Kaplan A, Stanbrook M. Must family physicians use spirometry in managing asthma patients?YES. Can Fam Phys. 2010;56(2):126–8 (130, 132).
Merghani TH. Patterns of spirometry in asthmatic patients presenting with respiratory symptoms. Int J Med Sci Public Health. 2017;6(2):337–40.
Acknowledgements
Data collection was undertaken by Adelphi Real World as part of a syndicated survey, entitled the Respiratory Disease-Specific Programme, sponsored by multiple pharmaceutical companies of which one was AstraZeneca. AstraZeneca did not influence the original survey through either contribution to the design of questionnaires or data collection. The study reported in this manuscript was funded by AstraZeneca and AstraZeneca funded all publication charges. All authors contributed to the design, interpretation of the data, the writing of the report and the decision to submit the paper for publication. All authors meet the International Committee of Medical Journal Editors criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published. Carole Alison Chrvala, PhD of Health Matters, Inc., funded by AstraZeneca, is acknowledged for her assistance with writing and editing this manuscript. The authors wish to thank Adam Roughley for the analytical support provided for this study. Preliminary results of this study were previously presented at a poster discussion session at the European Respiratory Society Congress 2016
Compliance with Ethics Guidelines
The research was conducted as a market research survey in accordance with the amended Declaration of Helsinki, adhering to the ICC/ESOMAR International code on observational research and performed in full accordance with the rules of the US Health Insurance Portability and Accountability Act 1996. IRB approval was not necessary or sought.”
Disclosures
Bo Ding is an employee of AstraZeneca. Mark Small is an employee of Adelphi Real World.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available due their proprietary nature but are available from the corresponding author on reasonable request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/1608F0602758B0F4.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Ding, B., Small, M. Disease Burden of Mild Asthma: Findings from a Cross-Sectional Real-World Survey. Adv Ther 34, 1109–1127 (2017). https://doi.org/10.1007/s12325-017-0520-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-017-0520-0