Abstract
The cerebellum is traditionally known to subserve motor functions. However, for several decades, the concept of the “cerebellar cognitive affective syndrome” has evolved. Studies in healthy participants and patients have confirmed the cerebellar role in language. The exact involvement of the cerebellum regarding cerebellar aphasia remains uncertain. We included 43 cerebellar stroke patients who were tested at 3 months post-onset with the Boston Naming Test (BNT), the Token Test (TT), and the Diagnostic Instrument for Mild Aphasia (DIMA). Lesion side (left/right) and volume (cm3) were investigated. Patients significantly deviated on the following: BNT (p<0.001), TT (p<0.05), DIMA subtests: sentences repetition (p=0.001), semantic odd-picture-out (p<0.05), sentence completion (p<0.05) without an effect of lesion location (left/right) or volume (cm3) (p>0.05). Our clinical study confirms a non-lateralized cerebellar aphasia post-stroke, characterized by impairments in word retrieval, phonology, semantics, and syntax resembling cerebral-induced aphasia. The integral cerebellum appears to interact with eloquent cortico-subcortical language areas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The cerebellum is traditionally known to play a role in motor control [1]. However, for about three decades, the concept of “cerebellar neurocognition” has evolved. In seminal work from Schmahmann and Sherman [2], a consistent pattern of cognitive and affective deficits was described in patients with focal cerebellar lesions and was coined as the “cerebellar cognitive affective syndrome” (CCAS). This condition was characterized by impairments in executive functions (e.g., set-shifting, planning, abstract reasoning), visuo-spatial cognition, personality changes (e.g., flattening or blunting of affect, disinhibited or inappropriate behavior), and a variety of linguistic deficits (e.g., dysprosodia, agrammatism, decreased verbal fluency, and mild anomia). Next, several case studies of patients with a cerebellar lesion and (experimental) functional neuroimaging studies in healthy participants contributed to knowledge about cerebellar function in the context of neurocognition and CCAS [3]. Most patient group studies were heterogeneous (e.g., tumor, degenerative, stroke). Only one study specifically included isolated cerebellar stroke patients, but post-onset times varied from acute to chronic stage (up to more than a year) [4]. It is therefore difficult to draw solid conclusions about the role of the cerebellum with respect to characteristics of CCAS. Generally, the effect of lesions is expected to be more subtle than cortical lesions since the cerebellum acts as a parallel system to fine-tune motor behavior rather than generating direct motor output.
Although considerable evidence has been gathered with regard to neurocognitive functions and the cerebellum, the exact role of the so-called linguistic cerebellum is still under debate. Experimental, neurophysiological, and neuroimaging studies have confirmed that the cerebellum is involved in several linguistic functions, such as grammar processing, verbal fluency [5, 6], and reading and writing [7]. Cerebellar-induced aphasia has also been described in several case studies. Mariën et al. [8] reported a 73-year-old, right-handed patient who suffered from word finding difficulties, lack of spontaneous speech initiation, expressive and receptive grammatical difficulties, and reading and writing deficits which led to the term cerebellar-induced aphasia. Single photon emission computed tomography (SPECT) studies in this patient showed a significant hypoperfusion not only in the right cerebellum, but also in the prefrontal language region of the left dominant hemisphere. Follow-up data showed paralleled patterns between perfusion change and neurolinguistic results confirming the role of cerebellum in language [9]. In addition, a lateralized involvement of lateral posterior cerebellar regions (including lobules VI and Crus I/II) was found in anatomo-clinical studies of patients with focal cerebellar lesions and linguistic impairments. In non-clinical populations, a relation between the cerebellum and the cerebral cortex with regard to language functioning has also been found ([10]; and for meta analyses, see [11]). This points to crossed cerebello-cerebral connections between the cortical language network and the cerebellum. In patient populations, which were often heterogeneous or only case studies, aphasia-like symptoms were not consistently present after cerebellar disease. Increased reaction times in a verb generation task were found, whereas performance on Aachener Aphasia subtests was intact or without aphasic characteristics in spontaneous speech [12, 13]. It has been suggested that cerebellar-induced aphasia is transient and most prominent in the acute phase ([7, 14]. Possibly, aphasia tests, designed for “classical” stroke population, are not sensitive enough to capture (mild) language deficits in cerebellar stroke patients. Correct diagnostics is of crucial importance, as not only moderate to severe aphasia but also mild aphasia can have detrimental effects on patients’ quality of life [15].
In this study, part of a large prospective study on Cognitive Deficits after Cerebellar Stroke (CODECS) [16], we investigated language functioning in a homogenous patient group with an isolated vascular cerebellar lesion, confirmed by imaging, by means of an extensive neurolinguistic protocol including tests designed for mild aphasia at 3 months post stroke onset. We hypothesized that a new test for mild aphasia would identify impairments, whereas standard aphasia tests would be less sensitive to detect disturbances. Finally, we expected that language impairments would be more pronounced in patients with right cerebellar stroke.
Materials and Methods
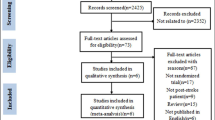
We included patients with focal cerebellar lesions admitted to the Department of Neurology at the Erasmus MC University Medical Center Rotterdam between April 2015 and April 2019. Exclusion criteria consisted of extra-cerebellar lesions, pre-existent neurocognitive or psychiatric disorders, and age younger than 18 years. Approval by the local Medical Ethics Committee was obtained (MEC-2013-462). All patients gave written informed consent and were given a standard neurological evaluation. After 3 months post-stroke, each patient underwent structural neuroimaging by means of computed tomography (CT) and/or magnetic resonance imaging (MRI) scan to confirm an isolated cerebellar lesion. All patients were investigated by means of a neurolinguistic assessment at 3 months. A standard neuropsychological protocol and the International Cooperative Ataxia Rating Scale (ICARS) were used to quantify the cerebellar ataxia as a measure of motor severity (for details see van der Giessen et al., [16].
Language and Cognitive Measures
We used the shortened Token Test [17] to determine the presence and severity of aphasia. To assess word retrieval, the Boston Naming Test (BNT) [18] was administered. The BNT consists of 60 black and white objects ordered in descending level of word frequency. Subtests at the linguistic levels phonology, semantics, and grammar from the recently developed Dutch Diagnostic Instrument for Mild Aphasia (DIMA) [19] were administered: verbal repetition (words, compounds, non-words, sentences), semantic odd-picture-out, sentence completion (see Table 1). Error analyses on deviant language tests were conducted. Errors were calculated into percentages and divided into the following categories: semantic, irrelevant (i.e., not semantically related) or phonematic paraphasia, hesitation, slow response, self-correction, anomia, superordinate, circumlocution, neologism, perseveration, repetition/omission/insertion of words or no reaction.
Nonverbal cognitive abilities were assessed using the Trail Making Test A (TMT-A) [22]. In the TMT-A, the patient connects numbers (1–25) in an ascending order on a paper sheet. The score consists of the time in seconds it takes to finish. Visuo-perceptual speed underlies performance on the TMT-A (scores from TMT-B and BA are not taken into account in this paper).
Statistical Analysis
Based on published normative data, raw test scores of the patients were transformed into z-values to compare the performance of patients and healthy adults (when possible corrected for age, education, and sex). We investigated whether patients’ mean test z-scores differed from the normal population, using a one-sample t-test with 0 (the mean score of the normative group) as test value. To minimize the number of statistical comparisons, only tests of which the mean performance deviated from normal population were selected for further comparisons, such as the influence of lesion location (left/right cerebellum) on language scores with a univariate analysis of variance. Pearson rank correlations were made between scores on the Token Test, deviating DIMA subtests harboring a speed component and TMT-A. Lesion location and volume were extracted from the CT/MRI and lesion volume was calculated in squared centimeters by a neurologist (RG).
Results
Forty-three patients were included in the study. Demographic characteristics are summarized in Table 2. Eighteen (41.9%) patients were men. The majority was right-handed (81.4%). The average age was 62 years (SD 15; range 22–92); mean education was 12 years (SD 3.46; range 6–22). The majority of the lesion was located in the right cerebellum (58.1%) with a mean volume of 15.87 cm3.
Language Measures
Patients’ mean scores were statistically worse compared to normal population on the BNT (z-score = –1.20, t= –4.339, p<0.001) and the Token Test (z-score= –0.56, t=–2.475, p<0.05). No clinically impaired scores were found (z= ≤ −2). For the DIMA subtests, statistical deviations between patients and normal population were found in the following: repetitions of words (z-score= 0.22, t=3.057, p<0.001), repetition of sentences (z-score= −0.68, t=−3.421, p=0.001), semantic odd-picture-out (z-score= −0.64, t=−2.635, p<0.05), and sentence completion (z-score= −0.64, t=−2.113, p<0.05) (see Fig. 1 and Table 3 for an overview). The subtests semantic odd-picture-out and sentence completion were also clinically impaired (z= ≤ −2). There was a significant moderate positive correlation between scores on repetition of sentences, sentence completion, and the Token Test (Pearson r=0.615, Pearson r=0.472, p<0.01 resp.), and a significant weak positive correlation was found between scores on semantic odd-picture out and the Token Test (Pearson r=0.384, p<0.05). Qualitative error analyses on deviant language tests revealed various patterns; see below in Table 4 error percentages per test and total errors in percentages in Fig. 2.
Influence of Lesion Location and Non-linguistic Performance Versus Language Tests
No effect of cerebellar lesion location (left/right) was observed on the deviating language tests (p>0.05). Also lesion volume did not correlate with language performance (p>0.05). To investigate possible influence of non-linguistic slowness on semantic odd-picture-out and sentence completion as high rates of slow reactions (see Table 4) were observed, Pearson rank correlations were conducted with TMT-A. No correlations were found between TMT-A and semantic odd-picture out and sentence completion (Pearson r=0.211, p=0.511; Pearson r=−0.191, p=0.552).
Discussion
We investigated neurolinguistic functioning in a large homogeneous group of patients with isolated cerebellar stroke. Disturbances were found not only in standard aphasia tests (BNT and Token Test) but also in subtests from the Diagnostic Instrument for Mild Aphasia (repetition of sentences, semantic odd-picture-out, and sentence completion), which clearly confirms a role in language functioning for the cerebellum. Our patient group was consistently tested with a neurolinguistic protocol at 3 months post-onset. These findings show that cerebellar-induced aphasia is not just transiently present in the acute phase as commonly described in the literature [7, 14].
Different aspects of language in both production and comprehension were found to be impaired compared to normal population, including word retrieval (object naming), a test for aphasia severity/comprehension (Token Test), phonological production/working memory (repetition of sentences), rapid semantic selection/word retrieval (semantic odd-picture-out), and spontaneous speech in context (sentence completion). Apart from DIMA, also standard aphasia tests were statistically deviant, which suggests that the language profile of cerebellar stroke patients resembles aphasic disturbances caused by a cerebral lesion albeit to a less severe extent.
As for the standard aphasia tests, the Token Test is well-known to determine the presence and severity of aphasia [17]. It could be debated whether in our study the severity was mild, as the Token Test score was statistically deviant but not clinically impaired (cutoff z=−2). Deviating DIMA subtests correlated moderately with the Token Test, indicating that higher scores on DIMA subtests were associated with better performance on the Token Test. The Boston Naming Test was also sensitive for statistical deviations in the cerebellar patient group indicating problems with word retrieval. Our qualitative analysis showed that the most frequently occurring errors concerned semantic paraphasias, circumlocutions, and anomias. These are typical error types in aphasic population (f.i. anomic aphasia). A naming deficit was described earlier in cerebellar patients. Baillieux et al. [23] investigated a heterogeneous cerebellar group (tumor, arteriovenous malformation, infarction) of 18 patients of which 22% presented with a naming deficit. Fabbro et al. [24] also described problems in lexical retrieval in four right-handed cerebellar tumor patients. After surgery, only two patients partially recovered. In vascular case studies, (isolated) word retrieval deficits were also found [8, 25,26,27].
The test-battery for mild disorders, DIMA, also detected deficits in production subtests in the linguistic levels phonology, semantics, and syntax. At the level of phonology, repetition of sentences was impaired. Most commonly produced errors concerned hesitations, phonological, and irrelevant paraphasias which are (partially) different from the commonly reported distorted articulation, motor speech planning (apraxia of speech), or prosody in the context of ataxic dysarthria or verbal apraxia in patients with cerebellar lesions [28, 29] (see also [16], in which a negative correlation between ICAR score and language tests was found). The test items in our subtest are constructed to be phonologically complex as they involve phonemic similarities (tongue twisters), e.g., de Griek ontdekte vier nietjes in de band van zijn fiets (The Greek discovered four staples in the tire of his bike). It was found earlier that this so-called phonological similarity effect causes difficulties in cerebellar (degenerative and focal) lesions and in children with cerebellar tumor removal. Memory for phonologically similar words was worse than for phonologically dissimilar words and that this could have been caused by a deficit in phonological store [30, 31]. In addition, a defect in articulatory rehearsal in light of the forward output model, usually to explain motor function (e.g., prediction of limb state during movement trajectory), may have played a role. It is postulated that this forward output model can also control articulatory trajectory, that is, the prediction of the sequence of articulatory movements needed to rehearse verbal information formed during the initial encoding of the verbal stimuli [32]. The rapid engagement of the phonological loop via such a mechanism could increase the likelihood that the phonological store is refreshed before it has had chance to fade. Apart from computing the correct phonological information into lexical items and articulation, repetition of sentences also makes use of working memory as words need to be temporarily stored in a buffer or phonological loop [33] (see also [34] in which the articulatory side of the “Baddeley-Hitch model” is argued to be premature and less related to articulation). Some studies have demonstrated deviations in working memory, attested with impairments in tests such as digit or letter span forward and backwards [25]. Another test in which working memory also is involved is verbal fluency. Leggio et al. [35] found that in cerebellar patients, phonological fluency performance was worse than semantic fluency performance, due to the absence of reference to meaning in the phonological fluency test; hence, a stimulus has to be maintained in the working memory buffer (produce as many words within 1 m starting with letter “F”). In our larger dataset with the same patients from Van der Giessen et al. [16], verbal fluency (semantic and letter) was also impaired.
The second subtest from DIMA that deviated was the semantic odd-picture out. This is a test in which both semantic judgement and word retrieval have to be executed under time pressure. Apart from semantic fluency, semantic processing has received little attention in the field of cerebellar lesions [7]. Not only in this DIMA subtest, but also in the total number of errors, semantic paraphasias (incorrect selection semantically related item) were most frequently produced, followed by slow and no reactions in the semantic odd-picture-out. Semantic abilities (e.g., decision, discrimination, association) have been described to be impaired in focal cerebellar lesions [36], and to be involved in the right cerebellum in healthy participants with neuroimaging studies [37, 38]. It is remarkable that no reactions and semantic paraphasias were also observed in the BNT, a test for word-retrieval, confirming problems in word retrieval and activation of the wrong lexical item. Slow reactions were exceeding the time span of 4 s per item and seemed to be language specific, thus independent from a more general non-linguistic cognitive processing speed (TMT-A) as no correlations between these tests were found.
The final sensitive DIMA subtest was sentence completion. Sentence completion is a test for spontaneous speech in context and known to be sensitive to detect dynamic aphasia [39]. A loss of spontaneous speech initiation was earlier seen in the reported case study with a cerebellar lesion by Mariën et al. [8]. Most frequently occurring errors in our subtest concerned syntactic errors, slow reactions followed by repetition of a word. A high rate of syntactic errors in the sentence completion test shows that there could be some (mild) form of syntactic production deficit (e.g., errors in word order, inflections) in accordance with several case illustrations [8, 40,41,42]. Silveri et al. [41] found that a syntactic deficit in a cerebellar patient was most prone to morphology (omission of auxiliaries or inflection errors). They argued that the impairment was not considered to affect syntactic competence but is targeted to the online application of syntactic rules to correctly assign grammatical morphemes. This could also be due a problem in a reduction of cognitive resources [43]. However, in our dataset, the lack of a correlation with a more general non-linguistic cognitive processing speed (TMT-A) contradicts this statement.
In contrast to our expectations, we did not find a “lateralized linguistic cerebellum” as no significant differences were found between left and right cerebellar stroke patients. There are other studies who also found that left-sided or bilateral cerebellar lesions can lead to language disruption [40]. Based on this study, it indeed seems that the integral cerebellum interacts with eloquent cortico-subcortical areas related to specific linguistic functions, such as word retrieval in the inferior frontal gyrus, the middle inferior and anterior middle temporal gyrus, and the supramarginal gyrus and the inferior longitudinal fasciculus. Semantics in the posterior superior temporal gyrus and inferior fronto-occipital fasciculus, and spontaneous speech in context (initiation) in the supplementary motor area, the angular gyrus, the frontal aslant tract ([39, 44]. It is also possible that a larger sample size in combination with neuroimaging techniques such as resting-state functional connectivity is needed to demonstrate specific crossed cerebro-cerebellar circuits for language [45]
In addition, a more detailed division according to the functional linguistic topography by Stoodley and Schmahmann [46] could have been more sensitive to detect differences in language performance: that is the anterior lobe, parts of the medial lobule IV, lobule VIII of the posterior lobe, and the interpositus nuclei form the sensorimotor cerebellum, where the cognitive cerebellum consists of lobule VII, parts of lobule VI, Crus I and II, and the ventral part of the dentate nuclei. Lesion studies have confirmed a role for the dentate nucleus within the deep cerebellar nuclei (DCN) in language. Cerebellar mutism was described in a patient following two posterior fossa tumor operations; the first resection the right DCN was partially persevered with intact speech, whereas the second resection concerned bilateral involvement of DCN resulting in mutism [47]. Involvement of the DCN on language performance could be investigated in the future in a larger dataset. On the other hand, it can be argued whether this detailed cerebellar division is practical in clinical use.
Future analyses of the cerebellum serving as a forward output model, usually to explain motor function (i.e., dysmetria), should be expanded to language function or even other cognitive functions (“dysmetria of thought”) and the discussion as to whether or to which extent the cerebellum acts as an error-based learning mechanism in “cognitive cerebro-cerebellar loops” [48]. In the context of language, some psycholinguistic experiments in healthy participants have confirmed the role of the cerebellum in linguistic/semantic prediction [49, 50] in parallel with the more general prediction during both motor control. This may underlie the high occurrence of semantic errors in total and the lowest performance in sentence completion in which a part of the sentence needs to be “predicted.” This more general line of thought may contradict evidence in favor of an aphasia with an actual “loss of linguistic function.” More clinical experiments in cerebellar aphasia including detailed error analyses must be conducted in order to support this viewpoint.
This prospective study clearly confirms the role of the cerebellum in language function at several modalities (production and comprehension) and linguistic levels (word retrieval, phonology, semantics, and syntax) and that patients indeed suffer from a(n) (mild) aphasia. This is relevant information for clinical practice as language deficits can negatively influence patients’ social and professional life. We therefore recommend to administer a (short) neurolinguistic protocol in cerebellar stroke patients in the first months post-onset with preferably complex tests at different modalities and levels (e.g., tests under time pressure). The application of (suitable) language therapy should be investigated further. Other cerebellar diseases need to be investigated in a comparable uniform way in order to draw more solid conclusions about cerebellar-induced aphasia. The modalities reading and writing were not taken into account, but should be studied in the future as a relation between dyslexia and the cerebellum is known [28]. It seems in this study that other cognitive functions, such as non-linguistic processing speed, do not influence language functioning. However, the underlying mechanism of cerebellar-induced aphasia still remains to be elucidated.
Data availability
Not applicable.
References
Manto M, Bower JM, Conforto AB, Delgado-García JM, da Guarda SN, Gerwig M, et al. Consensus paper: roles of the cerebellum in motor control--the diversity of ideas on cerebellar involvement in movement. Cerebellum. 2012;11(2):457–87.
Schmahmann JD, Sherman JC. The cerebellar cognitive affective syndrome. Brain. 1998;121(Pt 4):561–79.
Marien P, Engelborghs S, Fabbro F, De Deyn PP. The lateralized linguistic cerebellum: a review and a new hypothesis. Brain Lang. 2001;79(3):580–600.
Kalashnikova LA, Zueva YV, Pugacheva OV, Korsakova NK. Cognitive impairments in cerebellar infarcts. Neurosci Behav Physiol. 2005;35(8):773–9.
Fiez JA. The cerebellum and language: Persistent themes and findings. Brain Lang. 2016;161:1–3.
Molinari M, Leggio MG, Silveri MC. Verbal fluency and agrammatism. Int Rev Neurobiol. 1997;41:325–39.
Mariën P, Ackermann H, Adamaszek M, Barwood CH, Beaton A, Desmond J, et al. Consensus paper: Language and the cerebellum: an ongoing enigma. Cerebellum. 2014;13(3):386–410.
Mariën P, Saerens J, Nanhoe R, Moens E, Nagels G, Pickut BA, . . . De Deyn PP. Cerebellar induced aphasia: case report of cerebellar induced prefrontal aphasic language phenomena supported by SPECT findings. J Neurol Sci. 1996;144(1-2):34-43.
Marien P, Engelborghs S, Pickut BA, De Deyn PP. Aphasia following cerebellar damage: fact or fallacy? J Neurolinguistics. 2000;13(2):145–71. https://doi.org/10.1016/S0911-6044(00)00009-9.
King M, Hernandez-Castillo CR, Poldrack RA, Ivry RB, Diedrichsen J. Functional boundaries in the human cerebellum revealed by a multi-domain task battery. Nat Neurosci. 2019;22(8):1371–8.
Stoodley CJ, Schmahmann JD. Functional topography in the human cerebellum: a meta-analysis of neuroimaging studies. Neuroimage. 2009;44(2):489–501.
Frank B, Schoch B, Hein-Kropp C, Hövel M, Gizewski ER, Karnath HO, Timmann D. Aphasia, neglect and extinction are no prominent clinical signs in children and adolescents with acute surgical cerebellar lesions. Exp Brain Res. 2008;184(4):511–9.
Richter S, Schoch B, Kaiser O, Groetschel H, Hein-Kropp C, Maschke M, et al. Children and adolescents with chronic cerebellar lesions show no clinically relevant signs of aphasia or neglect. J Neurophysiol. 2005;94(6):4108–20.
Frank B, Maschke M, Groetschel H, Berner M, Schoch B, Hein-Kropp C, et al. Aphasia and neglect are uncommon in cerebellar disease: negative findings in a prospective study in acute cerebellar stroke. Cerebellum. 2010;9(4):556–66.
Hilari K, Cruice M, Sorin-Peters R, Worrall L. Quality of life in aphasia: state of the art. Folia Phoniatr Logop. 2015;67(3):114–8.
Van der Giessen R, Satoer D, P., Koudstaal. The CODECS study: cognitive deficits in cerebellar stroke. Brain and Cognition. 2023;173:106102.
De Renzi E, Faglioni P. Normative data and screening power of a shortened version of the Token Test. Cortex. 1978;14(1):41–9.
Kaplan E, Goodglass H, Weintraub S. The Boston Naming Test. 2nd ed. 2001b . https://doi.org/10.1007/978-0-387-79948-3_869
Satoer D, De Witte E, Bulté B, Bastiaanse R, Smits M, Vincent A, et al. Dutch Diagnostic Instrument for Mild Aphasia (DIMA): standardisation and a first clinical application in two brain tumour patients. Clin Linguist Phon. 2022;36(11):929–53.
Kaplan E, Goodglass H, Weintraub S. Boston Naming Test. Williams and Wilkins: Lippincott; 2001a.
Lezak MD. Neuropsychological Assessment. Oxford University Press; 2004.
Lezak M, Howieson D, Bigler D, Tranel D. Neuropsychological assessment. Oxford University Press; 2012.
Baillieux H, De Smet HJ, Dobbeleir A, Paquier PF, De Deyn PP, Mariën P. Cognitive and affective disturbances following focal cerebellar damage in adults: a neuropsychological and SPECT study. Cortex. 2010;46(7):869–79.
Fabbro F, Moretti R, Bava A. Language impairments in patients with cerebellar lesions. J Neurolinguistics. 2000;13:173–88.
Ackermann H, Mathiak K, Riecker A. The contribution of the cerebellum to speech production and speech perception: clinical and functional imaging data. Cerebellum. 2007;6(3):202–13.
Gasparini M, Di Piero V, Ciccarelli O, Cacioppo MM, Pantano P, Lenzi GL. Linguistic impairment after right cerebellar stroke: a case report. Eur J Neurol. 1999;6(3):353–6.
Hassid EI. A case of language dysfunction associated with cerebellar infarction. J Neurol Rehab. 1995;9(3):157–60. https://doi.org/10.1177/154596839500900304.
Mariën P, Beaton A. The enigmatic linguistic cerebellum: clinical relevance and unanswered questions on nonmotor speech and language deficits in cerebellar disorders. Cerebellum Ataxias. 2014;1:12.
Spencer KA, Slocomb DL. The neural basis of ataxic dysarthria. Cerebellum. 2007;6(1):58–65.
Chiricozzi FR, Clausi S, Molinari M, Leggio MG. Phonological short-term store impairment after cerebellar lesion: a single case study. Neuropsychologia. 2008;46(7):1940–53.
Kirschen MP, Davis-Ratner MS, Milner MW, Chen SH, Schraedley-Desmond P, Fisher PG, Desmond JE. Verbal memory impairments in children after cerebellar tumor resection. Behav Neurol. 2008;20(1-2):39–53.
Chen SH, Desmond JE. Cerebrocerebellar networks during articulatory rehearsal and verbal working memory tasks. Neuroimage. 2005;24(2):332–8.
Baddeley A. Working memory and language: an overview. J Commun Disord. 2003;36(3):189–208.
Justus T, Ravizza SM, Fiez JA, Ivry RB. Reduced phonological similarity effects in patients with damage to the cerebellum. Brain Lang. 2005;95(2):304–18.
Leggio MG, Silveri MC, Petrosini L, Molinari M. Phonological grouping is specifically affected in cerebellar patients: a verbal fluency study. J Neurol Neurosurg Psychiatry. 2000;69(1):102–6.
Whelan B-M, Murdoch BE. Unravelling subcortical linguistic substrates: comparison of thalamic versus cerebellar cognitive-linguistic regulation mechanisms. Aphasiology. 2005;19:1097–106.
D'Mello AM, Turkeltaub PE, Stoodley CJ. Cerebellar tDCS modulates neural circuits during semantic prediction: a combined tDCS-fMRI study. J Neurosci. 2017;37(6):1604–13.
Xiang H, Lin C, Ma X, Zhang Z, Bower JM, Weng X, Gao JH. Involvement of the cerebellum in semantic discrimination: an fMRI study. Hum Brain Mapp. 2003;18(3):208–14.
De Witte E, Satoer D, Robert E, Colle H, Verheyen S, Visch-Brink E, Mariën P. The Dutch Linguistic Intraoperative Protocol: a valid linguistic approach to awake brain surgery. Brain Lang. 2015;140:35–48.
Silveri MC. Contribution of the cerebellum and the basal ganglia to language production: speech, word fluency, and sentence construction-evidence from pathology. Cerebellum. 2021;20(2):282–94.
Silveri MC, Leggio MG, Molinari M. The cerebellum contributes to linguistic production: a case of agrammatic speech following a right cerebellar lesion. Neurology. 1994;44(11):2047–50.
Zettin M, Cappa SF, D'amico A, Rago R, Perino C, Perani D, Fazio F. Agrammatic speech production after a right cerebellar haemorrhage. Neurocase. 1997;3:373–80.
Miceli, G. (2019). Disturbi sintattici e dell’elaborazione di frasi nell’afasia. In P. L. Denes G., Guariglia C., Cappa S., Grossi D., & L. C. (Eds.), Manuale di neuropsicologia, normalità e patologia dei processi cognitivi. (pp. 68–281). Psicologia, Zanichelli.
Dragoy O, Zyryanov A, Bronov O, Gordeyeva E, Gronskaya N, Kryuchkova O, et al. Functional linguistic specificity of the left frontal aslant tract for spontaneous speech fluency: evidence from intraoperative language mapping. Brain Lang. 2020;208:104836.
Zhang X, Chen Z, Li N, Liang J, Zou Y, Wu H, et al. Regional alteration within the cerebellum and the reorganization of the cerebrocerebellar system following poststroke aphasia. Neural Plast. 2022;2022:3481423.
Stoodley CJ, Schmahmann JD. Evidence for topographic organization in the cerebellum of motor control versus cognitive and affective processing. Cortex. 2010;46(7):831–44.
Kusano Y, Tanaka Y, Takasuna H, Wada N, Tada T, Kakizawa Y, Hongo K. Transient cerebellar mutism caused by bilateral damage to the dentate nuclei after the second posterior fossa surgery. Case report. J Neurosurg. 2006;104(2):329–31.
Sokolov AA, Miall RC, Ivry RB. The cerebellum: adaptive prediction for movement and cognition. Trends Cogn Sci. 2017;21(5):313–32.
Lesage E, Hansen PC, Miall RC. Right lateral cerebellum represents linguistic predictability. J Neurosci. 2017;37(26):6231–41.
Lesage E, Morgan BE, Olson AC, Meyer AS, Miall RC. Cerebellar rTMS disrupts predictive language processing. Curr Biol. 2012;22(18):R794–5.
Acknowledgements
The authors want to acknowledge Naziha Bouyakoub-El Ghannouti for her contribution in taking part in the patients’ tests. We are also grateful for Master’s student Michelle van Steijn and her assistance in the qualitative error analysis.
Funding
This study was supported by grant no. 514 of the Fund of Stichting Coolsingel.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
The study was approved by the local Medical Ethics Committee (MEC-2013-462) and all patients gave written informed consent. The study was carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
•Cerebellar stroke causes aphasia and resembles cerebral aphasia
•Cerebellar aphasia is characterized by impairments in all linguistic levels
•Both left and right cerebellar stroke cause aphasia
•An integral cerebellum appears to interact with cortico-subcortical language areas
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Satoer, D., Koudstaal, P.J., Visch-Brink, E. et al. Cerebellar-Induced Aphasia After Stroke: Evidence for the “Linguistic Cerebellum”. Cerebellum (2024). https://doi.org/10.1007/s12311-024-01658-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s12311-024-01658-1