Abstract
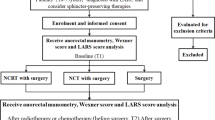
The detailed process of anorectal function recovery of the patients after sphincter-saving resection is unclear. We aimed to achieve detailed anorectal function recovery data of the patients after sphincter-saving resection and explore the relationship between the two frequently used anorectal function evaluation methods. A total of 72 eligible cases who underwent the sphincter-saving resection were divided into 3 groups according to the distal tumor margin distance from the anal verge. “L” replaced the distance; group 1: L ≤ 4 cm, group 2: 4 cm < L ≤ 6 cm, group 3: below the peritoneal reflection L > 6 cm. The anorectal function recovery outcomes of the 3 groups before and after the operation were compared. According to Wexner scores, the patients could achieve a satisfactory anorectal function at 3 months after surgery in group 2 and group 3. The patients required 4–5 months after surgery to achieve a satisfactory anorectal function in group 1. According to the ARM, in group 1 to group 3, the time at which the patients’ ARP and MSP after surgery started to show no significant decreases (p > 0.05) compared with preoperative levels were 12 months, 6 months, and 3 months after surgery, respectively. By combining the two methods, although the patients’ ARM indexes did not reach preoperative level (p < 0.05) at 6 months, 9 months, and 3 months in group 1 and group 2, respectively, their Wexner score showed a satisfactory anorectal condition. To all patients, when their ARP and MSP were basically returned to preoperative levels (p > 0.05), their average Wexner score was ≤ 4 or so. According to different rectal tumor locations, we had drawn the different anorectal function recovery curves with time, which could provide a reference for many treatments, such as the time of ileostomy closure. And we found the two anorectal function evaluation methods were not completely identical.



Similar content being viewed by others
References
Rullier E, Laurent C, Bretagnol F et al (2005) Sphincter-saving resection for all rectal carcinomas: the end of the 2-cm distal rule. Ann Surg 241:465–469
Schiessel R, Karner-Hanusch J, Herbst F et al (2010) Intersphincteric resection for low rectal tumors. Br J Surg 81(9):1376–1378
Park JS, Choi GS, Jun SH, Hasegawa S, Sakai Y (2011) Laparoscopic versus open intersphincteric resection and coloanal anastomosis for low rectal cancer: intermediate-term oncologic outcomes. Ann Surg 254:941–946
Akagi Y, Kinugasa T, Shirouzu K (2013) Intersphincteric resection for very low rectal cancer: a systematic review. Surg Today 43:838–847
Motoi K, Akihiro M, Yoshiyuki S et al (2014) Long-term clinical and functional results of intersphincteric resection for lower rectal cancer. Ann Surg Oncol null:S422–S428
Chau I, Brown G, Cunningham D, Tait D, Wotherspoon A, Norman AR, Tebbutt N, Hill M, Ross PJ, Massey A, Oates J (2006) Neoadjuvant capecitabine and oxaliplatin followed by synchronous chemoradiation and total mesorectal excision in magnetic resonance imaging-defined poor-risk rectal cancer. J Clin Oncol 24:668–674
Nordlinger B, Sorbye H, Glimelius B, Poston GJ, Schlag PM, Rougier P, Bechstein WO, Primrose JN, Walpole ET, Finch-Jones M, Jaeck D, Mirza D, Parks RW, Collette L, Praet M, Bethe U, van Cutsem E, Scheithauer W, Gruenberger T (2008) Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet 371:1007–1016
Rothenberg ML, Cox JV, Butts C, Navarro M, Bang YJ, Goel R, Gollins S, Siu LL, Laguerre S, Cunningham D (2008) Capecitabine plus oxaliplatin (XELOX) versus 5-fluorouracil/folinic acid plus oxaliplatin (FOLFOX-4) as second-line therapy in metastatic colorectal cancer: a randomized phase III noninferiority study. Ann Oncol 19:1720–1726
Bossé D, Mercer J, Raissouni S, Dennis K, Goodwin R, Jiang D, Powell E, Kumar A, Lee-Ying R, Price-Hiller J, Heng DYC, Tang PA, MacLean A, Cheung WY, Vickers MM (2016) PROSPECT eligibility and clinical outcomes: results from the Pan-Canadian rectal cancer consortium. Clin Colorectal Cancer 15:243–249
Keinchi K, Yuji N, Motohiro K et al (2016) Association between pathologic features of peripheral nerves and postoperative anal function after neoadjuvant therapy for low rectal cancer. Int J Color Dis 31:1845–1852
Hasegawa S, Goto S, Matsumoto T et al (2017) A multicenter phase 2 study on the feasibility and efficacy of neoadjuvant chemotherapy without radiotherapy for locally advanced rectal cancer. Ann Surg Oncol 24:1–9
Heald MRJ, Karanjia ND (1992) Results of radical surgery for rectal cancer. World J Surg 16:848–857
Krzysztof B, Andrzej R, Chang George J et al (2012) Is the 1-cm rule of distal bowel resection margin in rectal cancer based on clinical evidence? A systematic review. Indian J Surg Oncol 3:139–146
Jorge JM, Wexner SD (1993) Etiology and management of fecal incontinence. Dis Colon Rectum 36:77–97
Badic B, Joumond A, Thereaux J, Gancel CH, Bail JP (2018) Long-term functional and oncological results after sphincter-saving resection for rectal cancer-cohort study. Int J Surg 52:1–6
Mirnezami A, Mirnezami R, Chandrakumaran K, Sasapu K, Sagar P, Finan P (2011) Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg 253:890–899
Matthiessen P, Hallbã ÃKO, Rutegã Rd J et al (2007) Defunctioning stoma reduces symptomatic anastomotic leakage after low anterior resection of the rectum for cancer: a randomized multicenter trial. Ann Surg 247:207–214
Bax TW, Mcnevin MS (2007) The value of diverting loop ileostomy on the high-risk colon and rectal anastomosis. Am J Surg 193:585–588
Stephens RJ, Thompson LC, Quirke P, Steele R, Grieve R, Couture J, Griffiths GO, Sebag-Montefiore D (2010) Impact of short-course preoperative radiotherapy for rectal cancer on patients’ quality of life: data from the Medical Research Council CR07/National Cancer Institute of Canada Clinical Trials Group C016 randomized clinical trial. J Clin Oncol 28:4233–4239
Zhu X, Lou Z, Gong H et al (2016) Influence of neoadjuvant chemoradiotherapy on the anal sphincter: ultrastructural damage may be critical. Int J Color Dis 31:1–4
Nishizawa Y, Fujii S, Saito N, Ito M, Ochiai A, Sugito M, Kobayashi A, Nishizawa Y (2011) The association between anal function and neural degeneration after preoperative chemoradiotherapy followed by intersphincteric resection. Dis Colon Rectum 54:1423–1429
Kollmorgen CF, Meagher AP, Wolff BG, Pemberton JH, Martenson JA, Ilstrup DM (1994) The long-term effect of adjuvant postoperative chemoradiotherapy for rectal carcinoma on bowel function. Ann Surg 220:676–682
Da SG, Berho M, Wexner SD et al (2003) Histologic analysis of the irradiated anal sphincter. Dis Colon Rectum 46:1492–1497
Raja S, Okeke FC, Stein EM et al (2017) Three-dimensional anorectal manometry enhances diagnostic gain by detecting sphincter defects and puborectalis pressure. Dig Dis Sci 62:1–6
Konanz J, Herrle F, Weiss C, Post S, Kienle P (2013) Quality of life of patients after low anterior, intersphincteric, and abdominoperineal resection for rectal cancer--a matched-pair analysis. Int J Color Dis 28:679–688
Frenckner B, Euler CV (1975) Influence of pudendal block on the function of the anal sphincters. Gut 16:482–489
Ha HT, Fleshman JW, Smith M, Read TE, Kodner IJ, Birnbaum EH (2001) Manometric squeeze pressure difference parallels functional outcome after overlapping sphincter reconstruction. Dis Colon Rectum 44:655–660
Author information
Authors and Affiliations
Contributions
X H, Zc H, and Zg X contributed to the conception and design; Wz L performed the anorectal manometry (ARM); X H, W Y, and S C did the acquisition of data; X H drafted the article; X H and Zc H did the critical revision of the article.
Corresponding authors
Ethics declarations
Ethical approval for the study was obtained from the ethics committee of Hunan Provincial People’s Hospital, and informed consent from all individual participants included in the study were obtained.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, X., Xiao, Z., Yan, W. et al. Anorectal Function Recovery Curve of the Patients with Different Tumor Locations After Sphincter-Saving Resection for Low Rectal Cancer. Indian J Surg 82, 338–344 (2020). https://doi.org/10.1007/s12262-019-01958-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-019-01958-5