Abstract
Objective
This study was aimed at determining the minimum acquisition count to provide diagnosable image quality (DIQ) and investigating the usefulness of preset count acquisition (PCA) for planar images of pediatric 99mTc-dimercaptosuccinic acid (DMSA) scintigraphy.
Methods
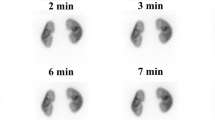
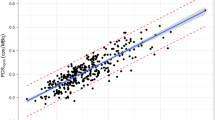
First, we calculated a coefficient of variation (CV) for DIQ with the shortest acquisition time through visual evaluation in 12 pediatric patients who underwent 99mTc-DMSA scintigraphy. Second, a minimum acquisition count to achieve the CV for DIQ was determined with the single regression analysis using CV as an explanatory variable and the total acquisition count as an objective variable in 81 pediatric patients. Finally, we compared PCA images based on the minimum acquisition count and preset time acquisition (PTA) images for 5 min in terms of the acquisition time, CV, and renal uptake ratio in another 23 pediatric patients.
Results
The visual evaluation showed that the CV corresponding to DIQ with the shortest acquisition time was 27.1%. The total acquisition count corresponding to DIQ was revealed to be 299,764 in the single regression analysis and was determined to be 300,000 after rounding. The CV and its standard deviation in PCA at 300,000 counts and PTA for 5 min were 26.4 ± 0.6% and 24.8 ± 1.3%, respectively. The standard deviation of CV in PCA at 300,000 counts was smaller than that in PTA for 5 min, indicating little variation in image quality between cases. The acquisition time in PCA at 300,000 counts (3.1 ± 0.7 min) was shorter than that in PTA for 5 min (5.0 ± 0.0 min). The intraclass correlation coefficient between renal uptake ratios for PCA and PTA was 0.98, indicating an extremely high concordance.
Conclusions
The minimum acquisition count required for the DIQ was 300,000. In addition, PCA at 300,000 counts was demonstrated to be useful by providing stable image quality at the shortest acquisition time.



Similar content being viewed by others
References
Karasawa K, Kamiyama H, Hashimoto T, Koizumi K. Survey questionnaire of pediatric nuclear medicine examinations in 14 Japanese institutes. Kaku Igaku. 2013;50(2):61–7.
Nagaki A, Sugimoto K, Nishimura Y, Murakawa K, Andoh T, Ichikawa H, et al. Development of body phantom for evaluation of appropriate administered radioactivities and image quality on 99mTc-DMSA scintigraphy in pediatric nuclear medicine. Nihon Hoshasen Gijutsu Gakkai Zasshi. 2017;73(12):1197–206.
Poli GL, Coca M, Torres L, Fahey F, Lassmann M, Chapple CL, et al. Developing and implementing an imaging optimization study in pediatric nuclear medicine: Experience and recommendations from an IAEA-coordinated research project. J Nucl Med. 2021;62(4):570–6.
Bar-Sever Z, Shammas A, Gheisari F, Vali R. Pediatric nephro-urology: overview and updates in diuretic renal scans and renal cortical scintigraphy. Semin Nucl Med. 2022;52(4):419–31.
Weyer K, Nielsen R, Petersen SV, Christensen EI, Rehling M, Birn H. Renal uptake of 99mTc-dimercaptosuccinic acid is dependent on normal proximal tubule receptor-mediated endocytosis. J Nucl Med. 2013;54(1):159–65.
Lee BH, Lee SH, Choi HJ, Kang HG, Oh SW, Lee DS, et al. Decreased renal uptake of 99mTc-DMSA in patients with tubular proteinuria. Pediatr Nephrol. 2009;24:2211–6.
Rossleigh MA. Renal cortical scintigraphy and diuresis renography in infants and children. J Nucl Med. 2001;42(1):91–5.
Marceau-Grimard M, Marion A, Côté C, Bolduc S, Dumont M, Moore K (2017) Dimercaptosuccinic acid scintigraphy vs. ultrasound for renal parenchymal defects in children. Can Urol Assoc J. 11(8): 260–264
Finkelstein JB, Rague JT, Chow J, Venna A, Logvinenko T, Nelson CP, et al. Accuracy of ultrasound in identifying renal scarring as compared to DMSA scan. Urology. 2020;138:134–7.
Şahin Ö, Taşbent FE. Comparison of DMSA scintigraphy and USG in detecting renal cortical scars in children with urinary tract infection. J Pediatr Infect Dis. 2018;13(3):210–5.
Ayazi P, Mahyar A, Noroozian E, Esmailzadehha N, Barikani A. Comparison of renal ultrasonography and dimercaptosuccinic acid renal scintigraphy in febrile urinary tract infection. Infez Med. 2015;23(4):323–9.
Fahey FH, Treves ST, Adelstein SJ. Minimizing and communicating radiation risk in pediatric nuclear medicine. J Nucl Med Technol. 2012;40(1):13–24.
Koizumi K, Masaki H, Matsuda H, Uchiyama M, Okuno M, Oguma E, et al. Japanese consensus guidelines for pediatric nuclear medicine Part 1: pediatric radiopharmaceutical administered doses (JSNM pediatric dosage card). Part 2: technical considerations for pediatric nuclear medicine imaging procedures. Ann Nucl Med. 2014;28:498–503.
Fujiwara T, Hidaka K, Sugibayashi K, Matsumoto M, Kida T, Shiina K. Investigation of the relation between administered dose and image quality for pediatric 99mTc-DMSA renal scintigraphy: clinical study applying the JSNM (Japanese Society of Nuclear Medicine) pediatric dosage card. Ann Nucl Med. 2019;33:153–9.
Piepsz A, Colarinha P, Gordon I, Hahn K, Olivier P, Roca I, et al. Guidelines on 99mTc – DMSA scintigraphy in children. Eur J Nucl Med. 2001;28(3):BP37-41.
Vali R, Armstrong IS, Bar-Sever Z, Biassoni L, Borgwardt L, Brown J, et al. SNMMI procedure standard/EANM practice guideline on pediatric 99mTc DMSA renal cortical scintigraphy: an update. Clin Transl Imaging. 2022;10:173–84.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethics approval
This study was approved by the Ethics Committee of Shiga University of Medical Science (approval number: R2019-307 on February 18, 2020, and R2021-108 on October 7, 2021).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ohashi, K., Iguchi, H., Nagatani, Y. et al. Usefulness of preset count acquisition in pediatric 99m Tc-DMSA planar imaging. Ann Nucl Med 37, 470–477 (2023). https://doi.org/10.1007/s12149-023-01849-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-023-01849-6