Abstract
The advent and uptake of effective antiviral therapies has transformed HIV/AIDS into a chronic manageable illness. The majority of Americans living with HIV are now ages 50 and older. Given the confluence of aging and HIV, chronic pain among older persons living with HIV/AIDS (PLWHA) has emerged as an area of clinical importance. Treatment of pain among this population is complex due to the prevalence of substance abuse and psychiatric illness in the population as well as the challenges of disentangling how inflammation associated with aging and HIV interact to predispose pain. Through a review of the extant literature we examine the complex associations between substance use, mental health, psychosocial issues, and chronic pain using a biopsychosocial framework in order to provide a means of addressing the aging-chronic pain link in older PLWHA. Using this frame, we then consider treatment implications for the population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Major advances have been made in the management of HIV/AIDS. Due to these advances in treatment, HIV/AIDS has now evolved into a chronic and manageable illness, with persons living with HIV/AIDS (PLWHA) living longer and some models suggesting a normal lifespan for those detected and treated upon the onset of infection (Smith et al. 2010). As PLWHA become older adults, defined here as over the age of 50, they become more medically complex due to the physical changes associated with ageing and comorbid HIV (High et al. 2012). These physical changes are often accompanied by an increase in pain related symptoms and conditions (Jiao et al. 2016; McGowan et al. 2017). PLWHA have higher rates of psychiatric and substance use disorders and are frequently prescribed narcotics at higher doses for pain management. Thus, increasing the risk of aberrant substance use (Cunningham 2018). One important aspect of healthy ageing that has not been fully explored is the interplay of substance use, mental health, chronic pain, and ageing.
Pain is one of the most prevalent disabilities in persons living with HIV/AIDS, with estimates across the lifespan of the HIV epidemic varying, but most studies report a prevalence between 31 and 50% (Ghosh et al. 2012). The etiology of pain among PLWHA may be due to multiple causes including the impact of the disease itself on the nervous system (e.g., neuropathies), exposure to pre-combination antiretroviral therapy (cART) era medications, immune suppression, HIV associated disorders, and factors not related to HIV or its treatment (e.g., preexisting health conditions) (Tsao and Soto 2009). Prior to the introduction of cART, HIV related pain was considered a complication of advanced disease progression and was associated with older age, increased viral load, and low CD4 counts (Aziz-Donnelly and Harrison 2017; Cherry et al. 2012). In the post-cART era, associations between pain and disease markers (i.e., viral load and CD4 counts) have not been consistently observed, however the association of older age persists (Aziz-Donnelly and Harrison 2017). Due to this, pain management has become a key challenge to caring for an already physically, emotionally, and socially burdened segment of the United States population.
PLWHA have rates of substance abuse and psychiatric disorders compared to the general population. Within this population, individuals with psychiatric illness are more likely to report pain and pain often co-occurs with substance abuse (Merlin et al. 2012a, b). Research on “triply diagnosed” (i.e., individuals diagnosed conditions of HIV, substance abuse, and psychiatric comorbidities) has found that such persons report more pain than the general population and PLWHA without these diagnoses (Tsao and Soto 2009). Furthermore, triply diagnosed individuals are at higher risk for poor health outcomes, non-adhanerence to ART, and lower treatment retention rates compared to the general HIV population (Tsao et al. 2012). Even more worrisome, older PLWHA are significantly less likely to be offered mental health and substance abuse services (Korthuis et al. 2008; Zanjani et al. 2007). This demonstrates that health care providers (HCPs) perceive older adults as less susceptible to mental health and substance abuse problems.
Patients suffering from chronic pain and substance use disorders require care that is both comprehensive and specialized. Pain patients have frequent health care visits and are at higher risk for developing substance abuse disorders (Edlund et al. 2007; Merlin et al. 2014). Furthermore, pain is a subjective experience that warrants examining life experiences of older PLWHA with consideration to both psychological and social factors in addition to biological factors (Hadjistavropoulos et al. 2011; Merlin et al. 2014). The reciprocal impact of psychiatric, behavioral, psychosocial, cultural, and medical factors should also be addressed within a structural framework that recognizes ageing as well as other cultural/structural variables. For example, stressors such as trauma are related to HIV specific chronic pain conditions and overall poorer health related quality of life (Nightingale et al. 2011). Noting the multi-determined nature of pain as well as its manifestations requires viewing pain within a larger context in order to drive treatment in a way that is efficacious and comprehensive.
In what follows, we first provide a literature overview of the associations between substance use, mental health, psychosocial issues, and chronic pain in older PLWHA. Specifically, this review examines the prevalence and etiology of pain symptomatology among older PLWHA and the roles of ageing, mental health, substance abuse, psychosocial factors, and the relationships that exist between these factors. After the literature review, this article proposes a treatment framework for pain management among older PLWHA. Lastly, treatment implications are discussed based off the findings of the review, the proposed framework, and recent treatment guidelines addressing older adults and PLWHA.
Method of Review
The authors searched for relevant articles published between 2006 and 2017, employing different combinations of the following terms: HIV, pain, neuropathic pain, nociceptive pain, neuropathy, pain treatment, older adults, elderly, above the age of 50, Substance abuse, substance dependence, substance use disorders, and addiction. Multiple databases were used including: AccessMedicine, PILOTS Database, Google Scholar, ProQuest Psychology Database, PsycArticles, PsychINFO, the Cochrane Library, and PubMed (includes MEDLINE). Websites of government organizations and disease specific associations were also used such as the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO). The search generated no articles that directly addressed the issues of HIV, pain, mental health, pain management, and substance abuse among older PLWHA. Research on pain among older PLWHA is a developing body of literature, especially as existing cohorts of PLWHA continue to age, but there is a lag and a paucity of literature in this area. Therefore, research on pain among older adults and PLWHA was complemented by studies that expanded on specific topics for which there was a dearth of literature to provide discussion on topics including substance abuse, psychiatric illness, adherence, and psychosocial issues. Thus, articles that may have focused on substance abuse or mental health and older PLWHA without focusing on pain, or articles that focused on pain and older PLWHA without a focus on substance abuse or mental health were included. In addition, articles that focused on pain, substance abuse, and mental in HIV but did not focus on older adults were also used. Articles that examined chronic pain management, substance use, mental health, and psychosocial issues among older adults were also used to bridge knowledge gaps in subject areas where there was a dearth of existing research. Conclusions were extrapolated from these various literatures.
The goal of developing a conceptual framework was to present a diagram of complex relationships believed to relate to a particular health problem (Earp and Ennett 1991). This is often done by selecting a source model that can be applied to a more specific public health problem or population using relevant research and evidence to direct and select concepts to include in a framework (Earp and Ennett 1991; Merlin et al. 2014). In order to develop a conceptual framework for older PLWHA, literature on existing theories and frameworks on the subjects of pain, pain among PLWHA, substance abuse, mental health, adherence, and older adults was reviewed. Based on the literature reviewed a source model was selected that we felt was most closely aligned with the needs of the population of this research, older PLWHA and pain. Lastly, we modified and expanded upon the source model to meet the unique needs of older PWLHA and pain.
Review of Existing Literature
Terminology
Pain has been defined as an unpleasant subjective sensory and psychological experience occurring from actual or potential damage to tissue and nerves (Boyd et al. 2011). An earlier and broader definition of pain is “Pain is whatever the experiencing person says it is, existing whenever the experiencing person says it does” (McCaffery 1968). Chronic pain is a malignant or non-malignant pain that exists beyond an expected healing timeframe, and in some cases healing will not occur (Manchikanti et al. 2011).
Substance abuse is defined as harmful or hazardous use of psychoactive substances, including alcohol and illicit drugs (World Health Organization (WHO) 2018). Substance dependence is a term used to describe a state characterized by physiologic, behavioral, and cognitive symptoms of needing a substance in which the use of the substance takes on a much higher priority than other behaviors once had (World Health Organization (WHO) 2009).
Substance use disorders is diagnostic term to describe problematic patterns of substance use that causes distress and impairment, such as health problems, disability, and failure to meet major responsibilities (American Psychiatric Association 2013). Substance use disorders are classified on severity of mild, moderate, and severe (American Psychiatric Association 2013). Addiction is a term used to describe the most severe substance-use disorders characterized by compulsive behavior and loss of self-control to the extent that the user (referred to as an addict) has great difficulty in voluntarily ceasing or modifying substance use (Volkow et al. 2016; World Health Organization (WHO) 2009). While the terms substance abuse, substance dependence, and addiction are often used interchangeably, addiction is a more overarching term that is widely used by clinical professionals and the public alike, and is synonymous with the DSM-V diagnosis of severe substance-use disorder (Volkow et al. 2016; World Health Organization (WHO) 2009).
Prevalence and Pathophysiology of Pain in Older PLWHA
Pain is one of the most prevalent disabilities in persons living with HIV/AIDS, impacting 67% of a nationally representative sample of PLWHA (Tsao and Soto 2009). Self-reported pain among PLWHA is estimated to range anywhere from 28 to 97% contingent upon what method of pain assessment is utilized (Basu et al. 2007). One study in 2017 found that of 638 PLWHA attending primary care visits in New York City, 40% had one or more pain diagnoses, with degenerative musculoskeletal disorders the most prevalent followed by neuropathic pain and headaches (Jiao et al. 2016). A survey of 859 PLWHA found 62.8% of the cohort reported pain lasting more than 1 day within the last month, with 63.3% reporting current pain (pain on the day of the survey) (Lawson et al. 2014). Within this cohort 40% had consulted their primary care providers (PCP) and 20% of the entire cohort were currently taking analgesics. Risk factors associated with pain were older age and time since diagnosis (Lawson et al. 2014). In another cohort, Ellis et al. (2010) reported that of 1539 PLWHA, 536 (34.8%) participants reported having symptomatic HIV associated sensory neuropathies (HIV-SN), and among those with sensory neuropathies 335 (62.5%) presented with neuropathic pain. The explanation for high rates of neuropathic pain in the cART era is paradoxical because even in well developed countries where the use of neurotoxic ART medications has been discontinued, neuropathic pain persists (Cherry et al. 2012), suggesting that the etiology of these neuropathies may have more to do with the effects of ageing with HIV.
The range of pain symptomatology of PLWHA has been compared to that of cancer pain due to the neuropathic nature and because it worsens as the disease progresses and with ageing (Bouhassira et al. 2008; Lee et al. 2009). Specifically, in both PLWHA and cancer patients, fatigue, respiratory distress, depression, and nausea are prevalent (Chang et al. 2007). Physical symptomatology of pain in PLWHA can be conceptualized as nociceptive pain, neuropathic pain, or a combination of both (Douaihy 2007b; Haanpää et al. 2009). Nociceptive pain is caused by direct stimulation of nociceptors on tissue as a direct result of injury, such as pain resulting from strain and rheumatologic manifestations (Haanpää et al. 2009). Nociceptive pain also includes pain caused by tissue injury that results in inflammation including infections, autoimmune disorders, and neoplasias such as lymphoma and sarcoma. Table 1 outlines distinct neuropathic pain versus nociceptive pain syndromes. Neuropathic pain is a direct result of a primary lesion or a disease-causing dysfunction or injury to the nervous system and is often chronic and more severe (Treede et al. 2008; Haanpää et al. 2009). Thus, PLWHA suffer from HIV associated sensory neuropathies (HIV-SN), which may cause pain that is a direct consequence of a disease (HIV), its treatment (ART), or lesions affecting the somatosensory system (Ellis et al. 2010; Cherry et al. 2012).
Patients suffering from HIV-SN experience pain symptomatology consisting of tingling, “pins and needles” sensations, and aching and stabbing pain in severe cases (Robinson-Papp et al. 2010). Risk factors associated with HIV-SN include disease progression and exposure to pre-cART era medications, particularly the NRTIs stavudine, didanosine, and zalcitabine (also referred to as the “dNRTIs”). The potential neurotoxicity of NRTIs can result in the development of antiretroviral toxic neuropathy (ATN) (Phillips et al. 2010a, b). HIV-SN is commonly associated with lower quality of life and disability depending on severity (Ellis et al. 2010). Diagnostic challenges arise when HIV-SN develops because the clinical presentation is often the same regardless of the etiology (ATN or distal symmetric polyneuropathy (HIV-DSP)) (Kaku and Simpson 2014; Phillips et al. 2010a, b; Wiebe et al. 2011). Research suggests that there may be an interaction between HIV-DSP and ATN or they may coexist independently (Wiebe et al. 2011). Symptom presentation is variable by patient but research suggests that ATN is more sudden and progressive, whereas HIV-DSP is gradual (Phillips et al. 2010a, b). Although the pathogenesis of HIV-SN is not fully understood, it is clear older adults are at increased risk.
Given the treatment advances in HIV, it might be expected that rates of HIV-SN would decrease with improved HIV screening, early diagnosis, treatment, and adherence to non-toxic cART regimens, thus preventing severe immunodeficiency (Aziz-Donnelly and Harrison 2017). The CNS Antiretroviral Therapy Effects Research (CHARTER) study evaluated new onset HIV-SN in a cohort of 1583 patients that were neuropathy free at baseline between 2003 and 2010 (Malvar et al. 2015). However, painful neuropathies were present in 25% of the cohort over an average of 2 years despite initiation and adherence to cART. However, older age (>50 years old) was significantly associated with developing HIV-SN independent of other risk factors (Malvar et al. 2015). The authors point out the significant implications these findings have on older PLWHA given that the principal reason for seeking medical attention among individuals with a diagnosis of HIV-SN is pain which contributes to lower quality of life and increased medical costs (Malvar et al. 2015).
Pain, Substance Use, Abuse, and Addiction
Older PLWHA are at increased risk for lifetime histories of substance abuse, HIV associated cognitive disorders, and depression (Kohli et al. 2006; Kupprat et al. 2015). Although among the ageing baby-boomer population current substance use, abuse, and tolerance may decrease with age, HCPs should not assume older PLWHA do not engage in substance abuse, misuse, and dependence (Kohli et al. 2006; Green et al. 2010). Older PLWHA are at increased risk for unintended fatal drug overdoses due to metabolic changes and changes in the body fluid-electrolyte balance that can increase drug serum concentrations (Green et al. 2010). One key predictor for illicit drug use and heavy alcohol use among older adults is a psychiatric diagnosis. A longitudinal study among 156 PLWHA found that 61.9% of the cohort reported pain, and pain was more common in patients with either psychiatric illness or substance abuse, especially injection drug use (IDU) (Merlin et al. 2012a, b). PLWHA who report more frequent drug use also report lower mental and physical quality of life, and AIDS associated illness is highest in this group (Green et al. 2010). Thus, the triple diagnosis of HIV, psychiatric disorders, and substance abuse disorders complicates many domains of health including psychiatric, neurocognitive, risk behavior, pain, and disease progression (Durvasula and Miller 2014).
Past research has suggested that HIV related pain in substance abusers is likely to be undertreated because of health care provider’s fears of contributing to addiction and concerns about the veracity of patient reports (Tsao et al. 2012). Patients with a history of drug use have been shown to report more pain and engage in more aberrant use of opioids, whereas patients with no substance abuse history are more likely to use opioids appropriately (Tsao et al. 2007). Research examining pain symptoms and substance use among a cohort of predominantly African American PLWHA with a history of IDU found that pain was associated with prescription opioid use and heroin use, but not the use of alcohol and non-opioid drugs even after controlling for prior drug use (Knowlton et al. 2015). The authors suggest that this selective drug use may represent self-medicating behaviors, highlighting the need for balanced opioid abuse prevention policies in order to mitigate the risk of unintentionally promoting drug abuse and relapse among an already vulnerable population (Knowlton et al. 2015).
Pain and Mental Health
While research has clearly established that PLWHA have higher rates of psychiatric disorders and poorer quality of life compared to the general population (Tsao et al. 2012; Halkitis et al. 2016), little research has examined the relationship between psychiatric conditions and chronic pain in older PLWHA. It is clear that chronic pain is associated with both depression and anxiety disorders (Gormsen et al. 2010), in addition to immune related dysfunctions (Ellis et al. 2010; Wiebe et al. 2011; Cherry et al. 2012). HCPs should expect pain to exacerbate preexisting psychiatric conditions and potentially lead to the development of new psychiatric conditions such as anxiety and depression (Tsao et al. 2012). Individuals may present with elevated pain perceptions, referenced as the ‘sickness response’, potentially due to glial activation and the release of pro-inflammatory cytokines causing inflammation that is accompanied by physiological, hormonal, and behavioral changes (Chapman 2010). Considering the immune compromise due to HIV, it is likely that pain perception is higher within PLWHA presenting with comorbid psychiatric illnesses and pain.
Common psychiatric symptoms related to HIV associated pain include depression, feelings of hopelessness, anhedonia, negativity, sleep disturbances, and eating difficulties (Tsao et al. 2012). Panic disorder, PTSD, and depression have all been found to be related to pain scores (Tsao et al. 2012). To date, no recent research (2006–2017) research has examined chronic pain and Axis I and II disorders among this population. However, some older studies have identified Axis I and II personality pathology as highly prevalent among chronic pain patients, but the explanation for this relationship remains inconclusive (Weisberg 2000). However, theoretical research has proposed the Diathesis-Stress approach, which in short, proposes that pre-existing personality function becomes exacerbated by the onset of pain (Weisberg 2000). Presently, no research has examined the relationship between HIV-associated neurocognitive disorders (HAND) and pain, but HAND is a frequent complication among older PLWHA and research examining HAND among older PLWHA has found poorer adherence and higher rates of psychiatric symptoms including: agitation, depression, anxiety, apathy, irritability (High et al. 2012; Milanini et al. 2017).
Pain, Substance Abuse, Mental Health, and Adherence to cART
The prevalence of pain, undertreatment of pain, and comorbid substance abuse and psychiatric conditions have the potential to critically impact health outcomes in PLWHA such as adherence to ART. For example, Surrat and colleagues (Surratt et al. 2015) examined the associations of pain, treatment of pain, and adherence among a group of PLWHA living in poverty with substance use disorders. Fifty-one percent of this cohort endorsed having pain and among those endorsing pain, 41.5% were untreated. Individuals endorsing pain were more likely to report food and housing insecurity and higher levels of psychological distress including depression and anxiety. In multivariate analyses, individuals with untreated pain, substance dependence symptoms, and patients engaging in ART diversion (selling or trading ART medications) had poorer adherence to ART (below 95%) compared to individuals without pain or treated pain (Surratt et al. 2015). Individuals with untreated pain had a 42% lower odds ratio of achieving optimal medication adherence and higher rates of substance abuse. Berg and colleagues (Berg et al. 2009) examined the relationship between pain and cART adherence while also examining the mediating effects of adherence, self-efficacy, and depression symptom severity among 70 current and former IDUs. Patients reporting pain were 87% less likely to achieve optimal adherence, but neither adherence self-efficacy nor depression symptom severity fully mediated the relationship between pain and adherence. The authors of both of these studies suggest that adequately treating pain may aid in improved ART adherence (Berg et al. 2009; Surratt et al. 2015). Another study examined the association of pain, opioid analgesic use, and opioid analgesic misuse on medication adherence among 296 patients recruited from the Research in Access to Care in the Homeless (REACH) cohort (Jeevanjee et al. 2014). Opioid misuse and illicit substance use were independently associated with poorer adherence, but multivariate analysis adjusting for covariates found that neither pain, receiving prescription opioids was associated with suboptimal adherence. However, opioid analgesic misuse was significantly associated with suboptimal adherence after adjusting for substance use disorders. The authors suggest that opioid misuse reflects a similar phenomenon observed in illicit substance users in which patients’ priorities are fixated on acquiring and using substances at the cost of social and personal obligations such as health maintenance (Jeevanjee et al. 2014).
Merlin et al. (2012a, b) examined the impact of pain alone and in association with mood and substance abuse disorders in relation to no-show visits, urgent care visits, cART adherence, and virologic failure (detectable >200). Interestingly, pain increased the likelihood of a no-show but only among patients without substance abuse, and pain in participants with substance abuse paradoxically appeared to be protective against no-show visits. The authors suggest that lower rates of no-show visits among patients with pain substance abuse may indicate that patients with substance abuse and pain may have more severe pain making them more likely to keep their primary care visit in effort to seek treatment for their pain. It is possible that patients with substance abuse may have more severe and difficult to control pain, as prior substance use may be associated with increased pain severity. As a result, patients with a history of substance abuse may be more likely to keep their HIV primary care appointments because they plan to seek help for their pain from their HIV primary care provider. No significant relationship between mood disorders, substance abuse, or pain was found with virologic failure. The relationship between pain and adherence to cART was minimal but patients with comorbid mood disorders and substance abuse had increased rates of suboptimal adherence to cART than individuals without these disorders (Merlin et al. 2012a, b).
One study examined the relationship of pain catastrophizing and depression to pain, disability, and medication adherence among a cohort of 46 PLWHA living with HIV-SN (Lucey et al. 2011). Pain catastrophizing is defined as a negative cognitive and emotional response to pain characterized by magnification, rumination, and helplessness (Lucey et al. 2011). Patients with higher pain catastrophizing reported a higher severity of neuropathic pain and pain-related disability. However, neither neuropathic pain severity, depressive symptoms, and pain catastrophizing were related to suboptimal adherence. Suboptimal adherence attributed to fear of side effects or forgetfulness was associated with increased severity of pain and depressive symptoms, but catastrophizing was not (Lucey et al. 2011). One additional study by Cervia et al. (2010) examining clinical and demographic factors related to pain in the cART era also found no relationship between pain severity and adherence. The findings from these studies demonstrate that further research is needed examining the complex relationship between substance abuse, psychiatric illness, and adherence to cART.
Psychosocial Issues Related to Pain and Older Adults
Disparities among PLWHA as a function of age, ethnicity, gender, social class, culture, and geography highlight the importance of recognizing the impact of various psychosocial factors on clinical outcomes. Within the United States, the HIV epidemic is increasing among individuals of lower socioeconomic status, ethnic minorities, and women (Miaskowski et al. 2011). These groups are also suggested to have a higher prevalence of pain and are also more likely to experience undertreatment of that pain (Miaskowski et al. 2011). Miaskowski et al. (2011) point out that although opioid analgesic prescription disparities have not been studied among PLWHA, other research suggests that African American and Hispanic/Latino patients are less likely to receive opioid analgesics for pain management in comparison to white patients.
Research demonstrates that women and women of color are disproportionately affected by HIV and pain particularly in sub-Saharan Africa. Special issues affecting women from African countries include: lack of control over sexuality and sexual relationships, poor access to sexual health, neglect of health needs including nutrition, poor access to medical care, delayed HIV/AIDS diagnosis, clinical management being based on clinical outcomes of primarily men, coerced or forced sex, harmful cultural practices such as genital mutilation, and facing stronger discrimination in relation to HIV/AIDS (Gray and Berger 2007). Pain in female PLWHA is often underdiagnosed and undertreated with some research suggesting females are twice as likely to be undertreated in comparison to male counterparts (Gray and Berger 2007). Many pain conditions are also more prevalent among women including endometriosis, complex regional pain syndrome, autoimmune conditions, diabetic neuropathies, headaches, arthritis, osteoporosis, breast cancer, bone fractures, and fibromyalgia (Gray and Berger 2007). Older HIV-positive postmenopausal women have lower CD4 counts after seroconversion compared to premenopausal and significantly higher rates of osteopenia than HIV-negative counterparts. (Gray and Berger 2007).
It should also be noted that within various African societies, barriers such as HIV-stigma itself may prevent certain cultures from acknowledging HIV disease related pain (Alexander et al. 2015). For example, selected Nigerian subcultures believe that ‘non-expression’ demonstrates strength and individuals exhibiting pain externally may be regarded poorly (Alexander et al. 2015).
Not surprisingly, abuse of older adults is rampant and the majority of cases are unreported and undetected by authorities. In 2010, a study in the US found that of 5777 older adults, 11.4% had experienced abuse within the last year (Acierno et al. 2010). Within the group that experienced abuse the types of abuse included: 5.2% financial abuse by a family member, 5.1% potential neglect (need for assistance that no one was actively addressing), 4.6% emotional abuse 1.6% physical abuse, and 0.6% sexual abuse (Acierno et al. 2010). This study did not measure the HIV status of the participants. In fact, elderly abuse among older PLWHA has never been systematically evaluated aside from several case studies however, evidence indicates regardless of age PLWHA experience higher rates of lifetime abuse and neglect (Goel et al. 2018). Medical conditions that often present comorbidly with HIV/AIDS such as diabetes, hypertension, CAD, fractures, stroke, and cancer have been shown to be highly correlated with elderly abuse (Lachs and Pillemer 2015). Within the context of HIV, older adults are at higher risk for HIV associated cognitive disorders (HAND) and individuals with poor cognition have been implicated to be at higher risk for elder abuse (Goel et al. 2018; Lachs and Pillemer 2004; Milanini et al. 2017).
Selection of the Biopsychosocial Framework for Pain Management among Older PLWHA
Given the chronic and complex nature of HIV, pain, substance abuse, and mental health we found the Biopsychosocial Model (BPS) (Engel 1977) to be most aligned with the needs of this population. The BPS model has been applied across a spectrum of chronic illnesses (Gatchel 2004) and is a leading framework for understanding chronic pain and aging with HIV (Gatchel et al. 2007; Merlin et al. 2014; Vance and Robinson 2004). The BPS model originally devised by Engel proposed understanding chronic illness and disease as a complex interaction between biological, psychological, and social factors (Engel 1977). Within the BPS framework, disease is defined as “objective biological event involving the disruption of specific body structures or organ systems caused by either anatomical, pathological, or physiological changes” (Gatchel et al. 2007). Conversely, illness is defined as “how a sick person and members of his or her family live with, and respond to, symptoms of disability” (Gatchel et al. 2007). Gatchel and colleagues point out that the BPS model is appropriate for pain because pain is a subjective experience that results in pain stimulus being transmitted through the patient’s individual genetics, psychiatric status, and past learning and sociocultural experiences (Gatchel et al. 2007). Thus, providers have to understand individual perception and response to pain within the context of biological, social, and psychiatric factors to optimally treat patients suffering from chronic pain.
The existing literature provides support for the BPS model as the leading treatment model for older adults suffering from chronic pain, HIV-related pain, and substance use/abuse (Marcus et al. 2000; Gatchel 2001; Davis and Srivastava 2003; Merlin et al. 2014). Age related factors that impact treatment outcomes among older adults include changes in patient activity, changes in duration of pain, changes in patient attitudes toward pain management goals, and changes in pain related behaviors (Davis and Srivastava 2003). The BPS model recognizes healthy aging as an ability to function in an evolving environment influenced by psychological, biological, spiritual, social, economic, and medical factors (Inui 2003). Within the context of HIV, this approach aligns with how many older PLWHA handled the disease in the absence of effective treatments by attending equally to the physical, emotional, and social domains (Halkitis 2013).
The BPS framework is appropriate for pain management in older PLWHA because it is multimodal, allows for a combination of both pharmacologic and behavioral interventions (Gatchel 2001), and can be modified to the individual needs of the patient. The goal of this approach is to effectively manage pain while addressing HIV related medical and psychiatric factors that may be contributing to or augmenting pain experience, treatment, and disability; and to carry out proactive measures to mitigate the likelihood of substance abuse and dependency (Gatchel 2004; Gatchel et al. 2007). The BPS approach to treatment emphasizes the importance of behavioral interventions as an essential complement to pharmacologic interventions. This integrated framework becomes important because older patients value social and behavioral interventions such as behavioral therapy, massage, topical agents, heat and cold patches, and social strategies such as community engagement (Davis and Srivastava 2003). Non-pharmacologic treatments should not be used as a replacement or substitute for analgesic pain management, but rather as a complement to multifactorial treatment (Marcus et al. 2000). PLWHA face many different kinds of stressors and pain can magnify (and be magnified by) emotional distress and diminish quality of life (Nightingale et al. 2011). Psychological and socio-environmental factors also intensify pain, disability, and distress. (Marcus et al. 2000) Therefore, within the BPS framework, treatment consists of careful assessment to lay the groundwork for development of a treatment plan that combines behavioral therapy, substance abuse treatment, and pharmacologic agents.
The nature of chronic pain is long-term and patients will have to make long-term behavioral changes and carry out self-management activities to ensure adherence to ART and pain medications, as well as other medications (e.g. psychiatric medications) and treatments (e.g. psychotherapy) (Krein et al. 2007). Multiple psychosocial treatments exist to reduce pain and aberrant drug behavior, and improve daily functioning. However, these psychological interventions require cooperation, psychological insight, and intact cognitive functioning (Krashin et al. 2012). Challenges that pose barriers to optimal pain management among older PLWHA include: lack of transportation, unstable housing, low or fixed income, insurance and health care cost issues, psychiatric disorders, neurocognitive decline, poor treatment perceptions, inadequate social support, social isolation, complex medication regimens, poor knowledge of medication regimens, age related comorbidities, and substance misuse and abuse (Douaihy 2007a, b).
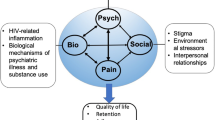
To date, only two studies have utilized a BPS framework for HIV pain management (Marcus et al. 2000; Merlin et al. 2014). However, neither addressed these issues within the context of aging. We selected an adapted version of the BPS framework as our source model by Merlin and colleagues (Merlin et al. 2014) published in Pain Practice. Merlin et al. (2014) addressed HIV related pain using the BPS framework. The framework proposed by Merlin included biological factors associated with HIV including the biological mechanisms of psychiatric illness, substance abuse, and pain. Merlin and colleagues (Merlin et al. 2014) point out the importance of understanding that HIV pain has varied etiologies including those related to HIV itself and those related to other disease processes. Psychiatric factors identified by Merlin & colleagues (Merlin et al. 2014) included distress, anger, fear, and traumatic life events with social factors including stigma, relationship factors, and environmental stressors.
The conceptual framework depicted in Fig. 1 builds upon the work of Merlin and colleagues (Merlin et al. 2014) by adapting their model to the aging HIV population. Our model views pain in older HIV positive adults as largely stemming from: pain related to HIV (HIV-SN), pain due to the natural process of aging with HIV, ongoing pain due to other health conditions/injuries, and side effects of ARTs and other medications. Our conceptual framework includes Merlin’s original biological factors, psychiatric factors, psychosocial factors, with the addition of medical/provider related factors and age-related factors that are likely to influence pain management in PLWHA.
We included Merlin’s original psychosocial factors with the addition of race, gender, socioeconomic status, cultural norms regarding pain, and vulnerability to abuse. Additions made to the psychiatric and substance abuse section included pain perception and cognitive abilities due to older persons being at higher risk for HAND.
We also added age related consideration to the model which included misconceptions which providers and others may have about older adults regarding substance abuse, cognitive functioning, community engagement, and social isolation. Social engagement verses social isolation was emphasized because the research reviewed suggested older adults are at higher risk for social isolation.
The addition of medical/provider related factors to the framework was included because the BPS model emphasizes the importance of understanding illness within a broader context. Thus in order to understand and treat the illness, the BPS model suggests that providers must understand the personal meaning of the illness to the patient (Mead and Bower 2000). However, the BPS perspective alone is not sufficient for fully understanding patients’ experience of illness because as developed, the original BPS model relied solely on the patient’s individual ‘biography’ (Mead and Bower 2000). The proposed model emphasizes a critical component of health care delivery: patient-centered care. Patient centered care emphasizes provider communication factors that promote: listening, respect, patient education, and communication (Nicolaidis 2011). This approach promotes a therapeutic alliance between the provider and patient through viewing illness within the BPS perspective and viewing the “patient-as-person” (Nicolaidis 2011). “Patient-as-person” refers to individual’s experience of illness, mutual participation in care, and responsibility is shared with the patient (Mead and Bower 2000; Nicolaidis 2011). Attention is given to the idea of the HCP as a person (attention to the influence of personal qualities of providers and how they impact treatment outcomes) (Nicolaidis 2011). An emphasis on patient-provider communication is emphasized within the BPS framework because communication has demonstrated to be a key factor related to social support and pain management outcomes (Hadjistavropoulos et al. 2011). Considerable evidence exists linking good provider-patient communication to positive health outcomes such as psychiatric well-being, symptom reduction, functional health, and pain management (Roter 2000). The BPS framework promotes interdisciplinary team management, which has been shown to be one of the most successful approaches to reducing symptoms and improving functioning (DeBar et al. 2012). Lastly, the findings in the review portion of this manuscript demonstrate that further research is needed examining the complex relationship between substance abuse, psychiatric illness, and adherence to cART. Regardless of pain, adherence to cART is critical to PLWHA. Suboptimal adherence to cART can lead to drug resistance, increased viral replication, viral mutations, increased likelihood of HIV transmission, and higher morbidity and mortality among PLWHA.
Treatment Implications
Clinical Assessment and Differential Diagnosis
Domains of pain assessment include: pain assessment, physical functioning, medication history, assessment of cognitive functioning, assessment of psychiatric functioning, and specialized assessment of pain to address the etiology (nociceptive versus neuropathic pain) (Hadjistavropoulos et al. 2007). Pain assessment should include: intensity, timing, location, quality, personal meaning of pain, aggravating factors, alleviating factors, and pain behaviors. Clinical assessment should also assess all aspects of patient demographics, medical and psychiatric history, family history, and HIV history. Information related to socioeconomic status and access to health care is essential to help HCPs understand the basic needs and systems of support available to their patients. One functional barrier to health adherence among older adults is cognitive impairment (Watkins and Treisman 2012). Older PLWHA are at higher risk for HIV associated neurocognitive disorders (HAND), and assessment for cognitive impairment should not be overlooked. The HIV Dementia Scale is recommended as an initial screen because it has been validated with older PLWHA and is quick and easy to administer (Bhavan et al. 2008). Differential diagnosis of pain is critical because HCPs are more likely to initiate aggressive treatment when the etiology of the pain is known. In order to diagnose, a comprehensive clinical assessment is necessary. One goal of clinical assessment is to identify the etiology of the disease or condition that is causing the pain.
Assessment of past medical history is essential to rule out underlying non-HIV related conditions. These include past and present medication regimens (ART and non-HIV related medication), past history of traumatic injury, surgery, brain injury, psychiatric history, nutrition, radiculopathy, polyneuropathy, postherpetic neuralgia, nerve trauma, entrapment neuropathy, trigeminal neuralgia, stroke, multiple sclerosis, spinal injuries, and substance use and abuse history (Haanpää et al. 2009). Substance and drug history should not only include assessment of illicit substances, but also neurotoxic antiretroviral medications, cytotoxic chemotherapy, isoniazid, and ‘megadoses’ of vitamins that may have neurotoxic effects such as pyridoxine (Phillips et al. 2010a, b).
Interdisciplinary team management approach and collaboration is needed to address and holistically manage the wide spectrum of elderly persons’ pain related health conditions. Interdisciplinary team management consisting of the following health disciplines may be consulted: nursing, pain medicine, psychiatry, family medicines, geriatrics, neurology, occupational therapy, physical therapy, pharmacy, and rheumatology (Hadjistavropoulos et al. 2007).
Multifactorial Treatment Plan
Pain in older PLWHA with co-morbid chronic pain and substance abuse is a challenging condition to accurately diagnose and treat. Pain requires comprehensive multifactorial treatment, including: primary medical care, nursing care, psychiatric care, and ongoing assessments in the domains of pain, substance abuse and misuse, and continued follow up. Older adults may be less likely to seek out treatment and adhere to treatment plans due to limited resources, social support, stigma related to having HIV, and mild to severe cognitive disabilities (Watkins and Treisman 2012). Barriers to treatment adherence among older adults include chronic or acute illness, mental illness, neurocognitive decline, substance abuse or dependence, disease-related knowledge, health literacy, adverse effects of polypharmacy, and patient provider relationship (Ettenhofer et al. 2009; Gellad et al. 2011). Older PLWHA with HAND or drug problems are at a heightened risk for poor adherence, which makes this population more vulnerable to neurocognitive decline and immunosuppression related morbidities (Ettenhofer et al. 2009).
Patient-provider engagement and education are essential for both providers and the patient in ensuring treatment adherence and positive health outcomes (Baron et al. 2010). Patient-provider engagement can be defined as the relationship between patient and provider that improves health promotion and utilization of health services characterized by active listening and supportive decision-making (Mitchell et al. 2017). A study by Mitchell and colleagues (Mitchell et al. 2017) examined the effects of chronic pain, depression and current substance use on provider engagement among a cohort of African American PLWHA. Provider engagement was measured using three questions: “My doctor listens to me,” “My doctor answers my questions,” and “My doctor involves me in decisions” rated using and ordinal scale from 0 = Never to 3 = Always. Self-reported audio computer-assisted self-interview (ACASI) was used to assess depression (Center for Epidemiologic Studies Depression Scale (CESD-20)), substance use (substances used in the last 6 months), pain (likert scale measures by the question, “How often have you been bothered by pain in the past six months?”), and adherence (percentage of pills missed in the past 7 days). Results demonstrated that chronic pain and depressive symptoms were both significantly associated with poorer engagement. Interestingly, substance use was associated with improved provider engagement. Patients with higher provider engagement had improved adherence suggesting chronic pain and poor provider engagement can have negative impacts on HIV health outcomes (Mitchell et al. 2017).
HCPs need to engage in discussions with patients about realistic treatment outcomes so feasible patient expectations can be established. It is important to note that setting arbitrary treatment relief targets such as 30% or 50% reduction in pain, although useful in clinical trials to establish efficacy, is not always essential for clinical practice (Varrassi et al. 2010). Treatment expectations will be variable and individualized by patient. Some patients may prefer to accept a higher level of pain in exchange for fewer side effects, while others may require higher analgesia relief. Identifying and meeting those outcomes is the principle for effective pain management (Varrassi et al. 2010).
Older adults are more likely to underreport pain due to misconceptions that pain is a part of normal ageing. Although pain is common in older adults, it is not a normal part of ageing and this misconception should be corrected to ensure accurate reporting of pain (Chai and Horton 2010). HCPs should take into account the possibility that older adults may have lived with the pain for an extended period of time and therefore may be less likely to report pain due to fear of being seen as weak or disabled (Bernhofer and Sorrell 2012). Older adults have a tendency to under-report pain and show increased stoicism in regard to reporting pain (Hadjistavropoulos et al. 2007). HCPs should recognize patients expressing attitudes such as “it is not good to complain” as a red-flag for potential pain under-reporting (Hadjistavropoulos et al. 2007).
Screening Tools
There is a growing field of research addressing relevant pain and substance abuse screening and assessment among older adults; however, to date there are no scales specifically validated to assess the multidimensional aspects of pain in older PLWHA. An overview of the available assessment scales, internal consistency, test retest reliability, and strengths and weaknesses for pain and substance abuse assessment is provided in Appendix Table 3. Pain assessment tools were selected if they have been used in HIV populations previously or in older adults.
Many health care agencies use the Faces Pain Scale (Stuppy 1998), Numerical Rating Scale (NRS) (Farrar et al. 2001), and Visual Analog Scale (VAS) (Wewers and Lowe 1990). These tools have good sensitivity, take limited time to administer, and translate cross-culturally. The FPS has shown to be validated in older adults with cognitive impairment and with patients from different racial and cultural backgrounds (Hadjistavropoulos et al. 2014). Although similar, the NRS and VDS are preferred to the NRS in older adults and in individuals with cognitive impairment due to higher error rates and patient preference (Hadjistavropoulos et al. 2014). For patients that cannot verbally communicate, the Checklist of Nonverbal Pain Indicators (CNPI) can be utilized (Feldt 2000).
Diagnostic tests to screen for sensory neuron function are recommended, although this form of intensive testing is often not feasible outside of specialty centers (Phillips et al. 2010a, b). Therefore, utilizing the Brief Peripheral Neuropathy Screening (BPSN), which has been tested to be effective in identifying HIV-SN is recommended as a first tool for pain assessment (Cherry et al. 2005). The BPSN is practical because it is easy to administer and does not require specialized equipment or diagnostic training. However, this tool has not yet been validated for use in older adults. The Leeds Assessment of Neuropathic Symptoms and Signs (S-LANNS) has been validated in patients with neuropathic pain and is sensitive to treatment effects and thus is useful for monitoring (Bennett et al. 2007). However, a portion of the S-LANNS requires clinical examination, and therefore may not be fit for some settings. Conversely, the painDETECT instrument does not require physical examination and has good utility in both HIV neuropathic pain and older adults (Cappelleri et al. 2015a). The ID-Pain Assessment and Neuropathic Pain Questionnaire (NPQ) are both short self-report questionnaires that do not require physical examination and are useful in quickly identifying the likely presence of a neuropathic pain component to a patient’s pain (Bennett et al. 2007; Krause and Backonja 2003).
The McGill Pain Questionnaire (MPQ) is a multidimensional pain scale composed of 78 pain descriptors that are categorized into 20 subclasses designed to evaluate the sensory, affective, and evaluative features of pain in addition to a 1-item pain intensity scale (Hawker et al. 2011). The MPQ has been validated in older adults and patients with chronic pain and uses pain descriptors to help delineate between neuropathic and non-neuropathic pain (Dworkin et al. 2009; Gauthier et al. 2014; Grafton et al. 2005). There is also a short-form version consisting of 15 words that make up two subscales assessing sensory related pain (11 items) and affective related pain (4 items) (Dworkin et al. 2009). However, the ability of the short form version to differentiate between neuropathic versus non-neuropathic pain has been disputed (Hadjistavropoulos et al. 2007). For purposes of reliability and consistency in monitoring, it is critical that the same scale be used consistently over the course of treatment.
Non-Pharmacologic Treatment
The existing research on non-pharmacologic treatment for older PLWHA suffering from chronic pain is relatively new and a growing field of research. Cognitive behavioral therapy (CBT) for chronic pain focuses on improving coping mechanisms, reducing maladaptive behaviors and thoughts, and improving self-efficacy (Ehde et al. 2014). Specific cognitive behavioral techniques shown to be effective in treating pain in older adults include relaxation techniques, activity-rest cycle, attention diversion techniques, cognitive restructuring, and meditation. CBT should be considered for older adults with intact cognitive function who have poor coping strategies and for individuals with an active psychosocial component to their chronic pain (Chai and Horton 2010).
A recent systematic review by Merlin and colleagues (Merlin et al. 2016) examined non-pharmacologic and pharmacologic interventions for the treatment of chronic pain among PLWHA. A total of four studies examined non-pharmacologic interventions with only one being a randomized clinical trial (RCT). The RCT examined smoked cannabis versus placebo cigarettes with the cannabinoids extracted three times daily for 5 days among PLWHA and neuropathic pain. This study found a reduction in pain measured on the VAS two-fold (34% vs. 17%) in the cannabis group compared to the placebo (Abrams et al. 2007; Merlin et al. 2016). The other non-pharmacologic studies were pre-post behavioral interventions, two were CBT interventions and one self-hypnosis intervention conducted on populations above the age of 50. The self-hypnosis study consisted of three self-hypnosis sessions and found only a small reduction in pain at 10 weeks and the CBT studies found small improvements in pain at 12 and 24 weeks but were limited due to adherence issues (Cucciare et al. 2009; Dorfman et al. 2013; Merlin et al. 2016; Trafton et al. 2012).
Another pilot study assessing the feasibility of a cognitive behavioral therapy intervention (HIV-PASS) for management of pain and depressive symptoms among PLWHA had promising results (Uebelacker et al. 2016). The behavioral intervention emphasized that pain is not harmful, avoidance is a natural pain response, and that patients will have to find balance between behaviors that will allow for achieving long term goals while minimizing short-term discomfort. The intervention was compared to an active health education condition. Although not significant, the effect size for change in average pain score favored the health education condition rather than HIV-PASS. Conversely, pain related interference with psychosocial and physical function was in the expected direction. The only statistically significant finding was participants in the CBT intervention showed decreased symptoms of depression which the authors found encouraging (Uebelacker et al. 2016). The authors also reported good attendance and qualitative data demonstrating that many participants understood and used skills taught during the intervention and improved communication with their PCP. The authors believe this study was limited due to the pilot study nature (HIV-PASS n = 11; Health Education Condition n = 12), but demonstrates evidence that merits a clinical trial with more stringent methods. In addition to CBT, biofeedback in combination with relaxation therapy has been shown to be effective in treatment of pain among older adults (Morone and Greco 2007).
Acupuncture for HIV-related pain has not yet been evaluated, but one systematic evaluating efficacy versus adverse effects had mixed results. The review did not evaluate HIV related pain and generated little convincing evidence for efficacy with the exception of neck pain. The authors reported numerous adverse effects with infection and pneumothorax being the most prominent (Ernst et al. 2011).
Mindfulness Based Stress Reduction (MBSR) is an 8-week course developed to reduce stress and symptoms including pain in patients with chronic disease. Studies on the general population have shown MBSR may be helpful in reducing symptoms of pain and improving quality of life (Cherkin et al. 2016; Gardner-Nix et al. 2008; Zeidan et al. 2016). Preliminary data demonstrated that it may be beneficial for PLWHA for immunologic function, physical symptoms, psychological symptoms, and medication adherence (Creswell et al. 2009; George et al. 2017). George et al. (2017) conducted a mixed methods feasibility study on 32 older PLWHA comparing MBSR to a health education attention control group. Outcome measures included Brief Pain Inventory, Perceived Stress Scale, HIV Symptoms Index, autonomic function testing, and focus groups. The MBSR intervention group reported subtle improvements on pain and stress but there was no significant group assignment effect. However, 79% of the MBSR group continued to practice and pain intensity was improved at 3-month follow-up, whereas the control groups’ pain had worsened. The authors concluded that the MBSR intervention was acceptable and feasible and may aid in reducing pain related to HIV, but larger RCT style studies are needed (George et al. 2017).
Limited research exists on non-pharmacologic interventions for HIV related pain, especially in older adults, yet non-pharmacologic interventions are amongst the most effective treatments for chronic pain among the general population (Merlin et al. 2016). One barrier to such treatments is lack of providers with knowledge of these therapies as well as lack of direct access to these services. Since most pain management begins in a primary care setting, HCPs are in an optimal position to discuss multimodal forms of treatment and provide appropriate referrals to psychosocial care.
Pharmacologic Management
To date, there has been no specific evidence based treatment for older PLWHA and pain. Rather pharmacologic treatment for cancer has been adapted based on guidelines developed by WHO in which a stepwise process starting with non-opioids before moving to opioids (see Fig. 2) (Basu et al. 2007). In accordance with the WHO step ladder, patients with mild pain should begin with a non-opioid such as acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs). The WHO ladder suggests that Opioids should only be used for patients with moderate to severe pain, after an initial attempt with non-opioids (NSAIDs and acetaminophen) (Basu et al. 2007). Acetaminophen is a primary choice for first-line therapy because it is relatively safe (Newshan and Staats 2013). In comparison to NSAIDs, acetaminophen is not associated with adverse renal effects, gastrointestinal bleeds, and cardiovascular toxicities (American Geriatrics Society 2009; Newshan and Staats 2013). However, The American Geriatric Society recommends reducing the dose of acetaminophen by 50–70% in patients with hepatic insufficiency or a history of alcohol abuse. NSAIDs are suggested to be more effective than acetaminophen for inflammatory pain, especially for short-term use (American Geriatrics Society 2009). Providers should take caution when using NSAIDs in patients that have low creatinine clearance, gastropathy, cardiovascular disease, and in patients suffering from heart failure (American Geriatrics Society 2009).
In severe chronic pain, step three advocates for long-acting opioids with or without adjunctive analgesics (Basu et al. 2007; O'Connor and Dworkin 2009). Providers should be cognizant of potential interactions between pain medications and ART. Table 2 summarizes pharmacologic recommendations for first line therapies and opioids (starting doses, titration, side effects, abuse potential) and drug interactions with ART (O'Connor and Dworkin 2009; University of Liverpool 2017). For further research addressing pharmacologic management see Basu et al. (2007); Chetty et al. (2012); Crana and Fudin (2013); and Newshan and Staats (2013).
One barrier to adequate analgesia is provider concerns about opioid abuse and dependence (Krashin et al. 2012). This can affect management of pain and patient compliance, and likely may be one of the key contributors to the undertreatment of pain in older PLWHA. HCPs should note that addiction and pain are not conceptualized as dichotomous, but rather on a continuum, and opioids used to treat chronic pain may be a problem, a solution, or an intersection of the two. Personal biases or discomfort with assessing substance use in older adults may make it difficult for HCPs to assess substance abuse, thus being mindful and sensitive is essential for providing optimal care (Gourlay and Heit 2006). Patients may also subscribe to these fears and may be reluctant to take analgesics for fear of addiction. Conversely Tsao et al. (2007) found that PLWHA with a history of substance abuse reported higher levels of pain and were more likely to engage in atypical use of prescription analgesics. In the context of ageing, Papaleontiou et al. (2010) conducted a meta-analysis that demonstrated overall current drug abuse and misuse was less prevalent among older adults.
Before implementing an opioid medication treatment, it is important that care providers establish boundaries and expectations for prescribing narcotic medications and have clear communication between all treatment team members (Krashin et al. 2012). Establishing a contingent intervention plan is important in case the patient is unable to adhere to treatment. HCPs and patients benefit from signing controlled substance patient and provider contracts for prescribing opioids regardless of whether the patient has a history of substance use (Basu et al. 2007), which gives the patient a sense of control. Urine toxicology analysis is also an effective way to monitor patient’s use of substances, however this may compromise patients’ trust in the HCP.
Management of Substance Use and Abuse
HCPs managing pain in PLWHA with histories of substance abuse, particularly abuse of opiates and/or prescription narcotic medications must carefully assess and monitor patients. It is critical to be mindful that management of pain in older PLWHA should be informed by prior drug use, but not defined by it. The strongest predictors of addiction and dependence are a personal history of alcohol and substance abuse, family history of drug abuse (Turk et al. 2008). Ives et al. (2006) also found patients with histories of legal problems such as driving under the influence (DUI) convictions, lost or stolen prescriptions offenses, and using non-medical means to was predictive of opioid abuse. Before initiating opioid therapy it is critical that the benefits to the patient will exceed its risk (Chou et al. 2009). Research hasn’t demonstrated concise ways to measure or qualify the benefits of opioid therapy (Chapman et al. 2010), however it is assumes the benefit to the patient is dependent in part on the extent to which the pain is reduced resulting in improved daily functioning and wellbeing. There is no gold standard on an exact protocol to measure these risks. This requires assessment via self-report, as well as reports from collateral observers including family members, residential care facility staff, and HCPs.
When it comes to opioid treatment and patients with a past history of substance dependence or abuse HCPs are faced with an even greater problem because the behaviors do not always resemble those similar to addiction to illicit substances. Explanations for lowered pain threshold and addictive behaviors may be due a myriad of factors including: 1) psychological or physical dependence, 2) result from a turbulent lifestyle, 3) inadequate treatment of pain, 4) signify a patients search for sympathy and understanding, 5) preoccupation with being unwell, 6) or may reflect a need for opioids to relieve an additional comorbid condition such as depression or anxiety (Ballantyne and LaForge 2007).
Clinical screening tools for identifying substance abuse risk can include urine toxicology, Current Opioid Misuse Measure (COMM), Screener and Opioid Assessment for Patients with Pain (SOAPP-R) (Butler et al. 2008, 2009, 2010). Both tools are helpful in identifying future and current opioid misuse and have been validated older adults (Butler et al. 2007a, 2010; Finkelman et al. 2017). The Current Opioid Misuse Measure (COMM) is a 17-item questionnaire useful for assessing opioid adherence, opioid abuse, and for documenting continued compliance with opioids (Butler et al. 2010). The COMM was developed specifically to track patient opioid compliance over time, so the items can be used repeatedly to track a patient’s “current” status (Butler et al. 2010). Similar to the COMM, the Opioid Assessment for Patients with Pain (SOAPP-R) and SOAPP-R-12 (short form version) are useful for identifying chronic pain patients at risk for misuse of opioid medications. The SOAPP-R was developed specifically for pain patients, is easy to administer, and helps identify patients who may be having difficulty adjusting medical use of opioids and need additional monitoring (Butler et al. 2008, 2009). The primary limitation to the self-reported screening tools is reactivity and social desirability bias. In addition, pain diaries are helpful in identifying and monitoring factors that increase, maintain, or decrease pain, such as incident evoked pains. Some limitations of pain diaries include recall bias, problems associated with retrospective reporting, and non-adherence (Hadjistavropoulos et al. 2007), and these issues may be exacerbated in older PLWHA for whom memory difficulties may be more pronounced resulting in poor retrospective recall.
Psychosocial Considerations
Sociocultural issues are important in the treatment of older PLWHA because the experience of pain is formulated by an interplay of social factors in addition to psychological and biological factors. Pain is not just a physiologic response to tissue damage but also is influenced by past emotional and behavioral experiences to pain such as the familial and cultural norms (Belfer 2013). Contextualizing pain, and viewing a patient holistically are critical safeguards against stereotyping and “one size fits all” approaches to pain management (Wilson-Stronks et al. 2008). Another factor to consider in treating older PLWHA is cognitive processes such as pain catastrophizing, negative social cognitions, and negative self-statements (Kamerman et al. 2012). Negative self-statements, self-blaming, and social cognitions may heighten pain perception among PLWHA (Belfer 2013).
Minority and socioeconomic factors influence both the subjective experience of pain and providers’ approach to treatment of pain. Providers, like their patients learn about pain as part of cultural socialization, thus, they have learned a so called “normal” or “right” and the “abnormal” or “wrong” response to pain (Narayan 2010). Providers also learn the “right” way to care for patients with pain through professional training that results in an unconscious idea of “good practice” (Narayan 2010). Meaning HCPs may unconsciously allow their own prejudices, biases, and sociocultural norms guide their practice (Narayan 2010). This is an example of “ethnocentrism”, the pattern to feel that a provider’s own cultural development and personal beliefs are correct (Narayan 2010). Providers need to be mindful of that a patient’s pain response is influenced by a variety of social, ethnic, and cultural factors that the provider may recognize as ‘wrong’ or not appropriate when they are in fact just different (Narayan 2010). For example, HCPs working in international settings should note that perception of pain is influenced by societal norms as well. Within various African societies, barriers such as HIV-stigma itself may prevent certain cultures from acknowledging HIV disease related pain (Alexander et al. 2015). For example, selected Nigerian subcultures believe that ‘non-expression’ demonstrates strength and individuals exhibiting pain externally may be regarded poorly (Alexander et al. 2015).
HCPs should be watchful for signs of elder abuse such as patients presenting with multiple unexplained or implausible injuries (Muehlbauer and Crane 2006). Elderly abuse is defined as: “infliction of injury, unreasonable confinement, intimidation, or punishment, with resulting physical harm, pain, or mental anguish” (Muehlbauer and Crane 2006). The American Psychological Association also considers abuse as: “willful deprivation by a caregiver of goods or services that are necessary to maintain physical or mental health” (Muehlbauer and Crane 2006). In 2010, a study in the US found that of 5777 older adults, 11.4% had experienced abuse within the last year (Acierno et al. 2010). Within the group that experienced abuse the types of abuse included: 5.2% financial abuse by a family member, 5.1% potential neglect (need for assistance that no one was actively addressing), 4.6% emotional abuse 1.6% physical abuse, and 0.6% sexual abuse (Acierno et al. 2010). The Hurt, Insult, Threaten, and Scream (HITS) is a short four item screening tool helpful in identifying domestic partner violence (Sherin et al. 1998). Additionally the Elderly Abuse Questionnaire is a fifteen-question screening scale helpful in identifying physical abuse, emotional abuse, neglect, and financial abuse (Carney et al. 2003).
Monitoring and Follow Up
Monitoring and follow up requires a team approach and should incorporate (1) ongoing pain assessment, (2) monitoring of daily living activities, (3) pain management team communication to ensure proper medication management, (4) monitoring of mental health and psychiatric care, and (5) assessment of psychosocial function, stress, and coping.Upon beginning treatment follow up should occur at least 1 month and 3 months after initiating a treatment plan (Nicholas et al. 2014). Frequency of monitoring will also vary on a case-by-case basis depending on other acute clinical issues.
Ongoing Pain Assessment
Upon follow up, consistent evaluation of pain and response to treatment is essential. It is essential that providers recognize pain screeners are not interchangeable, upon choosing a pain scale(s) it should be consistently used throughout the course of treatments in order to consistently monitor change over time. Consistent monitoring of pain diaries and communication with caregivers and family allow for optimal drug management. Consistent monitoring and follow up is essential for responsible care, and providers should differentiate between aberrant opioid dependence behavior and other aberrant behaviors (Hadjistavropoulos et al. 2007).
Monitoring of Daily Activities
Pain is considered significant when it impacts a patient’s ability to engage in functional activities of daily living and quality of life (Kaye et al. 2010). Pain can be manifested in multiple ways and therefore older PLWHA should be assessed on their ability to do ADLs (e.g., bathing, dressing, eating) and IADLs (housework, financial responsibilities, shopping, meal preparation) (Kaye et al. 2010). Assessment of psychosocial functioning (e.g., such as social engagement, mood, and beliefs about pain), and cognitive function are imperative (Hadjistavropoulos et al. 2007). Interventions can be implemented to assist with home care, adherence to ART, and ADLs such as occupational therapies or assistance from family members (Watkins and Treisman 2012).
Health Care Team Coordination
Team management and communication is essential. Primary care practitioners benefit from input from psychiatrists, psychologists, geriatricians, and other pain specialists to ensure adequate pain and medication management (Hadjistavropoulos et al. 2007). Concerns about aberrant drug behavior, drug abuse, and addiction warrant advice from a licensed psychiatrist, psychologist, or other mental health professionals (Krashin et al. 2012). When necessary, psychosocial support and structure can help prevent drug abuse and misuse, such as having a partner or caregiver assist in administering medications (Krashin et al. 2012). Having family members dispense medications weekly is a helpful way to monitor adherence and prevent drug misuse.
Assessment of Psychosocial Care
Continued behavioral therapy and psychosocial assessment to monitor psychosocial functioning, stress, and coping methods is necessary. Older adults with pain benefit from CBT strategies aimed at modifying thoughts and behaviors to increase their sense of control with the goal of improving the ability to cope with pain. The importance of psychosocial interventions for older PLWHA has received continued recognition (Brown and Vanable 2008). Accounting for HIV-specific psychosocial factors such as survivor guilt, loss of loved ones, depression, anxiety, minority status, gender, sexuality, life events, loneliness, coping skills, familial factors, and need for HIV specific social support (Chida and Vedhara 2009; Halkitis 2013; Halkitis et al. 2016) are important adjunctive elements of pain management in older adults living with HIV. For example, one study examining social support and ART adherence found that PLWHA who have higher self-perceived social support are more likely to adhere to ART and stay linked to care (Kelly et al. 2014). HCPs should encourage individuals to engage in group therapy, group intervention, group education, and involvement of spouse, family, friends, and community organizations.
Summary
Worldwide, approximately 3.6 (3.2–3.9) million PWLHA are above the age of 50 (UNAIDS 2013). In the United States, older PLWHA accounted for 17% of new diagnoses in 2014 and in 2013 42% of PLWHA were above the age of 50 (Centers for Disease Control and Prevention 2015). As the population of older PLWHA continues to grow, new challenges emerge, especially as they relate to the complex synergies of HIV, substance abuse, and chronic pain. Concurrent psychiatric illnesses, substance abuse, HIV, and psychosocial factors may magnify the pain experience. In addition to pain, older PLWHA experience complex social issues brought forth by ageing such as complex and greater care needs, fragile social networks, and variable stigmas due to age, HIV, race, socioeconomic status, sexual orientation, and survivor guilt. This research proposes an adapted BPS framework to meet the needs of the ageing population of PLWHA and pain. Research on improving management and treatment of pain among older PLWHA should be a priority with the intent of improving the lives of older PLWHA. Future research is needed using exclusively older cohorts as the needs of this population is unique.
References
Abrams, D. I., Jay, C. A., Shade, S. B., Vizoso, H., Reda, H., Press, S., Kelly, M. E., Rowbotham, M. C., & Petersen, K. L. (2007). Cannabis in painful HIV-associated sensory neuropathy A randomized placebo-controlled trial. Neurology, 68(7), 515–521.
Acierno, R., Hernandez, M. A., Amstadter, A. B., Resnick, H. S., Steve, K., Muzzy, W., & Kilpatrick, D. G. (2010). Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National Elder Mistreatment Study. American Journal of Public Health, 100, 292–297.
Alexander, C. S., Pappas, G., Henley, Y., Kangalawe, A. K., Oyebola, F. O., Obiefune, M., Nwene, E., Stanis-Ezeobi, W., Enejoh, V., & Nwizu, C. (2015). Pain management for persons living with HIV disease: Experience with interprofessional education in Nigeria. American Journal of Hospice & Palliative Medicine, 32, 555–562.
American Geriatrics Society. (2009). American Geriatrics Society panel on the pharmacological management of persistent pain in older persons. Pharmacological management of persistent pain in older person. Pain Medicine, 10, 1062–1083.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub.
Aziz-Donnelly, A., & Harrison, T. B. (2017). Update of HIV-associated sensory neuropathies. Current Treatment Options in Neurology, 19(10), 36.
Babor, T. F., Higgins-Biddle, J. C., Saunders, J. B., & Monteiro, M. G. (2001). The alcohol use disorders identification test. World Health Organization.
Ballantyne, J. C., & LaForge, K. S. (2007). Opioid dependence and addiction during opioid treatment of chronic pain. Pain, 129, 235–255 doi: S0304-3959(07)00161-3 [pii].
Baron, R., Binder, A., & Wasner, G. (2010). Neuropathic pain: diagnosis, pathophysiological mechanisms, and treatment. The Lancet Neurology, 9, 807–819.
Basu, S., Bruce, R. D., Barry, D. T., & Altice, F. L. (2007). Pharmacological pain control for human immunodeficiency virus–infected adults with a history of drug dependence. Journal of Substance Abuse Treatment, 32, 399–409.
Belfer, I. (2013). Nature and nurture of human pain. Scientifica (Cairo), 2013, 415279–415219. https://doi.org/10.1155/2013/415279.
Bennett, M. (2001). The LANSS pain scale: the Leeds assessment of neuropathic symptoms and signs. Pain, 92, 147–157.
Bennett, M. I., Smith, B. H., Torrance, N., & Potter, J. (2005). The S-LANSS score for identifying pain of predominantly neuropathic origin: validation for use in clinical and postal research. The Journal of Pain, 6, 149–158.
Bennett, M. I., Attal, N., Backonja, M. M., Baron, R., Bouhassira, D., Freynhagen, R., Scholz, J., Tolle, T. R., Wittchen, H. U., & Jensen, T. S. (2007). Using screening tools to identify neuropathic pain. Pain, 127, 199–203 doi: S0304-3959(06)00595-1 [pii].
Berg, K. M., Cooperman, N. A., Newville, H., & Arnsten, J. H. (2009). Self-efficacy and depression as mediators of the relationship between pain and antiretroviral adherence. AIDS Care, 21(2), 244–248.
Bernhofer, E. I., & Sorrell, J. M. (2012). Chronic pain in older adults. Journal of Psychosocial Nursing and Mental Health Services, 50, 19–23.
Bhavan, K. P., Kampalath, V. N., & Overton, E. T. (2008). The aging of the HIV epidemic. Current HIV/AIDS Reports, 5, 150–158.
Boonstra, A. M., Schiphorst Preuper, H. R., Reneman, M. F., Posthumus, J. B., & Stewart, R. E. (2008). Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. International Journal of Rehabilitation Research, 31, 165–169. https://doi.org/10.1097/MRR.0b013e3282fc0f93.
Bouhassira, D., Attal, N., Alchaar, H., Boureau, F., Brochet, B., Bruxelle, J., Cunin, G., Fermanian, J., Ginies, P., & Grun-Overdyking, A. (2005). Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain, 114, 29–36.
Bouhassira, D., Lantéri-Minet, M., Attal, N., Laurent, B., & Touboul, C. (2008). Prevalence of chronic pain with neuropathic characteristics in the general population. Pain, 136(3), 380–387.
Boyd, D., Butler, M., Carr, D., Cohen, M., Devor, M., Dworkin, R., Greenspan, J., Jensen, T., King, S., Koltzenburg, M. (2011) IASP Pain Terminology. An update on the IASP Taskforce on Taxonomy. Part III: Pain Terms, A Current List with Definitions and Notes on Usage. IASP Taxonomy 2011.
Brown, J. L., & Vanable, P. A. (2008). Cognitive–behavioral stress management interventions for persons living with HIV: a review and critique of the literature. Annals of Behavioral Medicine, 35, 26–40.
Butler, S. F., Budman, S. H., Fernandez, K., & Jamison, R. N. (2004). Validation of a screener and opioid assessment measure for patients with chronic pain. Pain, 112, 65–75.
Butler, S. F., Budman, S. H., Fernandez, K. C., Houle, B., Benoit, C., Katz, N., & Jamison, R. N. (2007a). Development and validation of the current opioid misuse measure. Pain, 130, 144–156.
Butler, S. F., Fernandez, K., Benoit, C., Budman, S. H., & Jamison, R. N. (2008). Validation of the revised screener and opioid assessment for patients with pain (SOAPP-R). The Journal of Pain, 9, 360–372.
Butler, S. F., Budman, S. H., Fernandez, K. C., Fanciullo, G. J., & Jamison, R. N. (2009). Cross-validation of a screener to predict opioid misuse in chronic pain patients (SOAPP-R). Journal of Addiction Medicine, 3, 66–73. https://doi.org/10.1097/ADM.0b013e31818e41da.
Butler, S. F., Budman, S. H., Fanciullo, G. J., & Jamison, R. N. (2010). Cross validation of the current opioid misuse measure to monitor chronic pain patients on opioid therapy. The Clinical Journal of Pain, 26, 770–776. https://doi.org/10.1097/AJP.0b013e3181f195ba.
Cappelleri, J. C., Koduru, V., Bienen, E. J., & Sadosky, A. (2015a). A cross-sectional study examining the psychometric properties of the painDETECT measure in neuropathic pain. Journal of Pain Research, 8, 159–167. https://doi.org/10.2147/JPR.S80046.
Carney, M. T., Kahan, F. S., & Paris, B. E. B. E. (2003). Elder abuse: is every bruise a sign of abuse? Mount Sinai Journal of Medicine, 70, 69–74.
Carr, D. (2005) Pain in HIV/AIDS a major global healthcare problem.
Centers for Disease Control and Prevention. (2015). Diagnoses of HIV infection in the United States and dependent areas, 2011. HIV Surveillance Report, 25, 1–25.
Cervia, L. D., McGowan, J. P., & Weseley, A. J. (2010). Clinical and demographic variables related to pain in HIV-infected individuals treated with effective, combination antiretroviral therapy (cART). Pain Medicine, 11(4), 498–503.
Chai, E., & Horton, J. R. (2010). Managing pain in the elderly population: pearls and pitfalls. Current Pain and Headache Reports, 14, 409–417.
Chang, V. T., Sorger, B., Rosenfeld, K. E., & Lorenz, K. A. (2007). Pain and palliative medicine. Journal of Rehabilitation Research and Development, 44, 279–294.
Chapman CR (2010) Painful multi-symptom disorders: a systems perspective. Kruger L, Light AR. Translational pain research: from mouse to man. Boca Raton, by Taylor and Francis Group, LLC.
Chapman, C. R., Lipschitz, D. L., Angst, M. S., Chou, R., Denisco, R. C., Donaldson, G. W., Fine, P. G., Foley, K. M., Gallagher, R. M., & Gilson, A. M. (2010). Opioid pharmacotherapy for chronic non-cancer pain in the United States: a research guideline for developing an evidence-base. The Journal of Pain, 11, 807–829.
Cherkin, D. C., Sherman, K. J., Balderson, B. H., Cook, A. J., Anderson, M. L., Hawkes, R. J., Hansen, K. E., & Turner, J. A. (2016). Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: a randomized clinical trial. Jama, 315(12), 1240–1249.
Cherry, C. L., Wesselingh, S. L., Lal, L., & McArthur, J. C. (2005). Evaluation of a clinical screening tool for HIV-associated sensory neuropathies. Neurology, 65, 1778–1781 doi: 65/11/1778 [pii].
Cherry, C. L., Wadley, A. L., & Kamerman, P. R. (2012). Painful HIV-associated sensory neuropathy. Pain, 2, 543–552.
Chetty, S., Baalbergen, E., Bhigjee, A., Kamerman, P., Ouma, J., Raath, R., Raff, M., & Salduker, S. (2012). Clinical practice guidelines for management of neuropathic pain: expert panel recommendations for South Africa. SAMJ: South African Medical Journal, 102, 312–325.
Chida, Y., & Vedhara, K. (2009). Adverse psychosocial factors predict poorer prognosis in HIV disease: a meta-analytic review of prospective investigations. Brain, Behavior, and Immunity, 23, 434–445.
Chou, R., Fanciullo, G. J., Fine, P. G., Adler, J. A., Ballantyne, J. C., Davies, P., Donovan, M. I., Fishbain, D. A., Foley, K. M., & Fudin, J. (2009). Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. The Journal of Pain 10, e22, 113–130.
Crana, S. E., & Fudin, J. (2013). Drug interactions among HIV patients receiving concurrent antiretroviral and pain. Practical Pain Management, 11, 105–124.
Creswell, J. D., Myers, H. F., Cole, S. W., & Irwin, M. R. (2009). Mindfulness meditation training effects on CD4+ T lymphocytes in HIV-1 infected adults: a small randomized controlled trial. Brain, Behavior, and Immunity, 23(2), 184–188.
Cucciare, M. A., Sorrell, J. T., & Trafton, J. A. (2009). Predicting response to cognitive-behavioral therapy in a sample of HIV-positive patients with chronic pain. Journal of Behavioral Medicine, 32(4), 340–348.
Cunningham, C. O. (2018). Opioids and HIV Infection: From Pain Management to Addiction Treatment. Topics in Antiviral Medicine, 25(4), 143.
Daeppen, J., Yersin, B., Landry, U., Pécoud, A., & Decrey, H. (2000). Reliability and validity of the alcohol use disorders identification test (AUDIT) imbedded within a general health risk screening questionnaire: Results of a survey in 332 primary care patients. Alcoholism: Clinical and Experimental Research, 24, 659–665.
Daly L, Bourke GJ (2008) Interpretation and uses of medical statistics. John Wiley & Sons.
Davis, M. P., & Srivastava, M. (2003). Demographics, assessment and management of pain in the elderly. Drugs & Aging, 20, 23–57.
DeBar, L. L., Kindler, L., Keefe, F. J., Green, C. A., Smith, D. H., Deyo, R. A., Ames, K., & Feldstein, A. (2012). A primary care-based interdisciplinary team approach to the treatment of chronic pain utilizing a pragmatic clinical trials framework. Translational behavioral medicine, 2, 523–530.
Dorfman, D., George, M. C., Schnur, J., Simpson, D. M., Davidson, G., & Montgomery, G. (2013). Hypnosis for treatment of HIV neuropathic pain: a preliminary report. Pain Medicine, 14(7), 1048–1056.
Douaihy, A. B. (2007a). Psychiatric aspects of comorbid HIV/AIDS and pain, part 1. The AIDS Reader, 17, 310–310.
Douaihy, A. B. (2007b). Psychiatric aspects of comorbid HIV/AIDS and pain, part 2. The AIDS Reader, 17, 350–350.
Durvasula, R., & Miller, T. R. (2014). Substance abuse treatment in persons with HIV/AIDS: challenges in managing triple diagnosis. Behavioral Medicine, 40, 43–52.
Dworkin, R. H., Turk, D. C., Revicki, D. A., Harding, G., Coyne, K. S., Peirce-Sandner, S., Bhagwat, D., Everton, D., Burke, L. B., & Cowan, P. (2009). Development and initial validation of an expanded and revised version of the short-form McGill pain questionnaire (SF-MPQ-2). PAIN®, 144, 35–42.
Earp, J. A., & Ennett, S. T. (1991). Conceptual models for health education research and practice. Health Education Research, 6(2), 163–171.
Edlund, M. J., Steffick, D., Hudson, T., Harris, K. M., & Sullivan, M. (2007). Risk factors for clinically recognized opioid abuse and dependence among veterans using opioids for chronic non-cancer pain. Pain, 129(3), 355–362.
Ehde, D. M., Dillworth, T. M., & Turner, J. A. (2014). Cognitive-behavioral therapy for individuals with chronic pain: Efficacy, innovations, and directions for research. The American Psychologist, 69, 153–166.
Ellis, R. J., Rosario, D., Clifford, D. B., McArthur, J. C., Simpson, D., Alexander, T., Gelman, B. B., Vaida, F., Collier, A., & Marra, C. M. (2010). Continued high prevalence and adverse clinical impact of human immunodeficiency virus–associated sensory neuropathy in the era of combination antiretroviral therapy: The CHARTER study. Archives of Neurology, 67, 552–558.
Engel, G. L. (1977). The need for a new medical model: a challenge for biomedicine. Science, 196, 129–196.
Ernst, E., Lee, M. S., & Choi, T. Y. (2011). Acupuncture: does it alleviate pain and are there serious risks? A review of reviews. PAIN®, 152(4), 755–764.
Ersek, M., Herr, K., Neradilek, M. B., Buck, H. G., & Black, B. (2010). Comparing the psychometric properties of the checklist of nonverbal pain behaviors (CNPI) and the pain assessment in advanced dementia (PAIN-AD) instruments. Pain Medicine, 11, 395–404.
Ettenhofer, M. L., Hinkin, C. H., Castellon, S. A., Durvasula, R., Ullman, J., Lam, M., Myers, H., Wright, M. J., & Foley, J. (2009). Aging, neurocognition, and medication adherence in HIV infection. The American Journal of Geriatric Psychiatry, 17, 281–290.
Farrar, J. T., Young, J. P., LaMoreaux, L., Werth, J. L., & Poole, R. M. (2001). Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain, 94, 149–158.
Fauconnier, A., Dallongeville, E., Huchon, C., Ville, Y., & Falissard, B. (2009). Measurement of acute pelvic pain intensity in gynecology: a comparison of five methods. Obstetrics and Gynaecology, 113, 260–269. https://doi.org/10.1097/AOG.0b013e318195bd6c.
Feldt, K. S. (2000). The checklist of nonverbal pain indicators (CNPI). Pain Management Nursing, 1, 13–21.
Finkelman, M. D., Jamison, R. N., Kulich, R. J., Butler, S. F., Jackson, W. C., Smits, N., & Weiner, S. G. (2017). Cross-validation of short forms of the Screener and Opioid Assessment for Patients with Pain-Revised (SOAPP-R). Drug and Alcohol Dependence, 178, 94–100.
Freynhagen, R., Baron, R., Gockel, U., & Tölle, T. R. (2006). Pain DETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Current Medical Research and Opinion, 22, 1911–1920.
Gardner-Nix, J., Backman, S., Barbati, J., & Grummitt, J. (2008). Evaluating distance education of a mindfulness-based meditation programme for chronic pain management. Journal of Telemedicine and Telecare, 14(2), 88–92.
Gatchel, R. J. (2001). A biopsychosocial overview of pretreatment screening of patients with pain. The Clinical Journal of Pain, 17, 192–199.
Gatchel, R. J. (2004). Comorbidity of chronic pain and mental health disorders: the biopsychosocial perspective. The American Psychologist, 59, 795–805.
Gatchel, R. J., Peng, Y. B., Peters, M. L., Fuchs, P. N., & Turk, D. C. (2007). The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychological Bulletin, 133, 581–624.
Gauthier, L. R., Young, A., Dworkin, R. H., Rodin, G., Zimmermann, C., Warr, D., Librach, S. L., Moore, M., Shepherd, F. A., & Riddell, R. P. (2014). Validation of the short-form McGill pain questionnaire-2 in younger and older people with cancer pain. The Journal of Pain, 15, 756–770.
Gellad, W. F., Grenard, J. L., & Marcum, Z. A. (2011). A systematic review of barriers to medication adherence in the elderly: looking beyond cost and regimen complexity. The American Journal of Geriatric Pharmacotherapy, 9, 11–23.
George, M. C., Wongmek, A., Kaku, M., Nmashie, A., & Robinson-Papp, J. (2017). A mixed-methods pilot study of mindfulness-based stress reduction for HIV-associated chronic pain. Behavioral Medicine, 43(2), 108–119.
Ghosh, S., Chandran, A., & Jansen, J. P. (2012). Epidemiology of HIV-related neuropathy: a systematic literature review. AIDS Research and Human Retroviruses, 28(1), 36–48.
Gliem, J. A., & Gliem, R. R. (2003). Calculating, interpreting, and reporting Cronbach’s alpha reliability coefficient for Likert-type scales. Midwest Research-to-Practice Conference in Adult, Continuing, and Community Education.
Goel, A., Koolwal, A., & Jain, N. (2018). Elder abuse in HIV-positive people. In Abuse and Neglect of the Elderly in India (pp. 189–199). Singapore: Springer.
Gormsen, L., Rosenberg, R., Bach, F. W., & Jensen, T. S. (2010). Depression, anxiety, health-related quality of life and pain in patients with chronic fibromyalgia and neuropathic pain. European Journal of Pain, 14, 127 e1–127. e8.
Gourlay, D., & Heit, H. (2006). Universal precautions: a matter of mutual trust and responsibility. Pain Medicine, 7, 210–211 author reply 212. doi: PME114 [pii].
Grafton, K. V., Foster, N. E., & Wright, C. C. (2005). Test-retest reliability of the short-form McGill pain questionnaire: Assessment of intraclass correlation coefficients and limits of agreement in patients with osteoarthritis. The Clinical Journal of Pain, 21, 73–82.
Gray, G., & Berger, P. (2007). Pain in women with HIV/AIDS. Pain, 132, S13–S21.
Green, L., & McGhie, J. (2011). Assessment of acute and chronic pain. Anaesthesia & Intensive Care Medicine, 12, 9–11.
Green, T. C., Kershaw, T., Lin, H., Heimer, R., Goulet, J. L., Kraemer, K. L., Gordon, A. J., Maisto, S. A., Day, N. L., & Bryant, K. (2010). Patterns of drug use and abuse among aging adults with and without HIV: A latent class analysis of a US veteran cohort. Drug and Alcohol Dependence, 110, 208–220.
Gudbergsen, H., Bartels, E. M., Krusager, P., Wæhrens, E. E., Christensen, R., Danneskiold-Samsøe, B., & Bliddal, H. (2011). Test-retest of computerized health status questionnaires frequently used in the monitoring of knee osteoarthritis: A randomized crossover trial. BMC Musculoskeletal Disorders, 12, 190.
Haanpää, M. L., Backonja, M., Bennett, M. I., Bouhassira, D., Cruccu, G., Hansson, P. T., Jensen, T. S., Kauppila, T., Rice, A. S., & Smith, B. H. (2009). Assessment of neuropathic pain in primary care. The American Journal of Medicine, 122, S13–S21.
Hadjistavropoulos, T., Herr, K., Turk, D. C., Fine, P. G., Dworkin, R. H., Helme, R., Jackson, K., Parmelee, P. A., Rudy, T. E., Lynn Beattie, B., Chibnall, J. T., Craig, K. D., Ferrell, B., Ferrell, B., Fillingim, R. B., Gagliese, L., Gallagher, R., Gibson, S. J., Harrison, E. L., Katz, B., Keefe, F. J., Lieber, S. J., Lussier, D., Schmader, K. E., Tait, R. C., Weiner, D. K., & Williams, J. (2007). An interdisciplinary expert consensus statement on assessment of pain in older persons. The Clinical Journal of Pain, 23, S1–S43. https://doi.org/10.1097/AJP.0b013e31802be869.
Hadjistavropoulos, T., Craig, K. D., Duck, S., Cano, A., Goubert, L., Jackson, P. L., Mogil, J. S., Rainville, P., Sullivan, M. J., Williams, d. C., & Amanda, C. (2011). A biopsychosocial formulation of pain communication. Psychological Bulletin, 137, 910–939.
Hadjistavropoulos, T., Herr, K., Prkachin, K. M., Craig, K. D., Gibson, S. J., Lukas, A., & Smith, J. H. (2014). Pain assessment in elderly adults with dementia. The Lancet Neurology, 13, 1216–1227.
Halkitis, P. N. (2013). The AIDS generation: Stories of survival and resilience. In Oxford University Press.
Halkitis, P. N., Krause, K. D., & Vieira, D. L. (2016). Mental health, psychosocial challenges and resilience in older adults living with HIV. Anonymous HIV and Aging., Karger Publishers, 187–203.
Hawker, G. A., Mian, S., Kendzerska, T., & French, M. (2011). Measures of adult pain: Visual analog scale for pain (vas pain), numeric rating scale for pain (nrs pain), mcgill pain questionnaire (mpq), short-form mcgill pain questionnaire (sf-mpq), chronic pain grade scale (cpgs), short form-36 bodily pain scale (sf-36 bps), and measure of intermittent and constant osteoarthritis pain (icoap). Arthritis Care & Research, 63(S11), S240–S252.
Herr, K. A., Spratt, K., Mobily, P. R., & Richardson, G. (2004). Pain intensity assessment in older adults: Use of experimental pain to compare psychometric properties and usability of selected pain scales with younger adults. The Clinical Journal of Pain, 20, 207–219.
Herr, K., Bjoro, K., & Decker, S. (2006a). Tools for assessment of pain in nonverbal older adults with dementia: A state-of-the-science review. Journal of Pain and Symptom Management, 31, 170–192.
Herr, K., Coyne, P. J., Key, T., Manworren, R., McCaffery, M., Merkel, S., Pelosi-Kelly, J., & Wild, L. (2006b). Pain assessment in the nonverbal patient: Position statement with clinical practice recommendations. Pain Management Nursing, 7, 44–52.
High, K. P., Brennan-Ing, M., Clifford, D. B., Cohen, M. H., Currier, J., Deeks, S. G., Deren, S., Effros, R. B., Gebo, K., Goronzy, J. J., Justice, A. C., Landay, A., Levin, J., Miotti, P. G., Munk, R. J., Nass, H., Rinaldo CR Jr, Shlipak, M. G., Tracy, R., Valcour, V., Vance, D. E., Walston, J. D., Volberding, P., & OAR Working Group on HIV and Aging. (2012). HIV and aging: State of knowledge and areas of critical need for research. A report to the NIH Office of AIDS Research by the HIV and aging working group. Journal of Acquired Immune Deficiency Syndromes, 60(Suppl 1), S1–S18. https://doi.org/10.1097/QAI.0b013e31825a3668.
Hjermstad, M. J., Fayers, P. M., Haugen, D. F., Caraceni, A., Hanks, G. W., Loge, J. H., Fainsinger, R., Aass, N., Kaasa, S., & European Palliative Care Research Collaborative (EPCRC). (2011). Studies comparing numerical rating scales, verbal rating scales, and visual analogue scales for assessment of pain intensity in adults: A systematic literature review. Journal of Pain and Symptom Management, 41, 1073–1093.
Inui, T. S. (2003). The need for an integrated biopsychosocial approach to research on successful aging. Annals of Internal Medicine, 139, 391–394.
Ives, T. J., Chelminski, P. R., Hammett-Stabler, C. A., Malone, R. M., Perhac, J. S., Potisek, N. M., Shilliday, B. B., DeWalt, D. A., & Pignone, M. P. (2006). Predictors of opioid misuse in patients with chronic pain: A prospective cohort study. BMC Health Services Research, 6, 46.
Jeevanjee, S., Penko, J., Guzman, D., Miaskowski, C., Bangsberg, D. R., & Kushel, M. B. (2014). Opioid analgesic misuse is associated with incomplete antiretroviral adherence in a cohort of HIV-infected indigent adults in San Francisco. AIDS and Behavior, 18(7), 1352–1358.
Jiao, J. M., So, E., Jebakumar, J., George, M. C., Simpson, D. M., & Robinson-Papp, J. (2016). Chronic pain disorders in HIV primary care: clinical characteristics and association with healthcare utilization. Pain, 157, 931–937. https://doi.org/10.1097/j.pain.0000000000000462.
Jun, L., Yi, F., & Jisheng, H. (2012). Linguistic adaptation, validation and comparison of 3 routinely used neuropathic pain questionnaires. Pain Physician, 15, 179–186.
Kaku, M., & Simpson, D. M. (2014). HIV neuropathy. Current Opinion in HIV and AIDS, 9(6), 521–526.
Kamerman, P. R., Wadley, A. L., & Cherry, C. L. (2012). HIV-associated sensory neuropathy: Risk factors and genetics. Current Pain and Headache Reports, 16, 226–236.
Kandiah, P. A., Atadzhanov, M., Kvalsund, M. P., & Birbeck, G. L. (2010). Evaluating the diagnostic capacity of a single-question neuropathy screen (SQNS) in HIV positive Zambian adults. Journal of Neurology, Neurosurgery, and Psychiatry, 81, 1380–1381. https://doi.org/10.1136/jnnp.2009.183210.
Kaye, A. D., Baluch, A., & Scott, J. T. (2010). Pain management in the elderly population: A review. The Ochsner Journal, 10(3), 179–187.
Kelly, J. D., Hartman, C., Graham, J., Kallen, M. A., & Giordano, T. P. (2014). Social support as a predictor of early diagnosis, linkage, retention, and adherence to HIV care: Results from the steps study. Journal of the Association of Nurses in AIDS Care, 25, 405–413.
Kim, E. J., & Buschmann, M. T. (2006). Reliability and validity of the faces pain scale with older adults. International Journal of Nursing Studies, 43, 447–456.
Knowlton, A. R., Nguyen, T. Q., Robinson, A. C., Harrell, P. T., & Mitchell, M. M. (2015). Pain symptoms associated with opioid use among vulnerable persons with HIV: An exploratory study with implications for palliative care and opioid abuse prevention. Journal of Palliative Care, 31, 228–233.
Koc, R., & Erdemoglu, A. K. (2010). Validity and reliability of the Turkish self-administered Leeds assessment of neuropathic symptoms and signs (S-LANSS) questionnaire. Pain Medicine, 11, 1107–1114.
Kohli, R., Klein, R. S., Schoenbaum, E. E., Anastos, K., Minkoff, H., & Sacks, H. S. (2006). Aging and HIV infection. Journal of Urban Health, 83, 31–42.
Korthuis, P. T., Zephyrin, L. C., Fleishman, J. A., Saha, S., Josephs, J. S., McGrath, M. M., et al. (2008). Health-related quality of life in HIV-infected patients: The role of substance use. AIDS Patient Care and STDs, 22(11), 859–867.
Krashin, D. L., Merrill, J. O., & Trescot, A. M. (2012). Opioids in the management of HIV-related pain. Pain Physician, 15, ES157–ES168.
Krause, S. J., & Backonja, M. (2003). Development of a neuropathic pain questionnaire. The Clinical Journal of Pain, 19, 306–314.
Krein, S. L., Heisler, M., Piette, J. D., Butchart, A., & Kerr, E. A. (2007). Overcoming the influence of chronic pain on older patients' difficulty with recommended self-management activities. Gerontologist, 47, 61–68 doi: 47/1/61 [pii].
Kupprat, S. A., Halkitis, P. N., Pérez-Figueroa, R., Solomon, T. M., Ashman, T., Kingdon, M. J., & Levy, M. D. (2015). Age-and education-matched comparison of aging HIV men who have sex with men to general population on common neuropsychological assessments. Journal of Health Psychology, 20, 1175–1185.
Lachs, M. S., & Pillemer, K. A. (2015). Elder abuse. New England Journal of Medicine, 373(20), 1947–1956.
Lawson, E., Sabin, C., Perry, N., Richardson, D., Gilleece, Y., Churchill, D., Dean, G., Williams, D., Fisher, M., & Walker-Bone, K. (2014). Is HIV painful? An epidemiologic study of the prevalence and risk factors for pain in HIV-infected patients. The Clinical Journal of Pain, 1. https://doi.org/10.1097/AJP.0000000000000162.
Lee, K. A., Gay, C., Portillo, C. J., Coggins, T., Davis, H., Pullinger, C. R., & Aouizerat, B. E. (2009). Symptom experience in HIV-infected adults: A function of demographic and clinical characteristics. Journal of Pain and Symptom Management, 38(6), 882–893.
Lucey, B. P., Clifford, D. B., Creighton, J., Edwards, R. R., McArthur, J. C., & Haythornthwaite, J. (2011). Relationship of depression and catastrophizing to pain, disability, and medication adherence in patients with HIV-associated sensory neuropathy. AIDS Care, 23(8), 921–928.
Maisto, S. A., Conigliaro, J., McNeil, M., Kraemer, K., & Kelley, M. E. (2000). An empirical investigation of the factor structure of the AUDIT. Psychological Assessment, 12, 346–353.
Malvar, J., Vaida, F., Sanders, C. F., Atkinson, J. H., Bohannon, W., Keltner, J., et al. (2015). Predictors of new onset distal neuropathic pain in HIV-infected individuals in the era of combination antiretroviral therapy. Pain, 156(4), 731–739.
Manchikanti, L., Singh, V., Caraway, D. L., & Benyamin, R. M. (2011). Breakthrough pain in chronic non-cancer pain: Fact, fiction, or abuse. Pain Physician, 14, E103–E117.
Marcus, K. S., Kerns, R. D., Rosenfeld, B., & Breitbart, W. (2000). HIV/AIDS-related pain as a chronic pain condition: Implications of a biopsychosocial model for comprehensive assessment and effective management. Pain Medicine, 1, 260–273.
McArthur, J. H. (1998). The reliability and validity of the subjective peripheral neuropathy screen. Journal of the Association of Nurses in AIDS Care, 9, 84–94.
McCaffery M (1968) Nursing practice theories related to cognition, bodily pain, and man-environment interactions. University of California Print. Office.
McGowan, J., Sherr, L., Rodger, A., Fisher, M., Miners, A., Anderson, J., Johnson, M., Elford, J., Collins, S., & Hart, G. (2017). Age, time living with diagnosed HIV infection, and self-rated health. HIV Medicine, 18, 89–103.
Mead, N., & Bower, P. (2000). Patient-centredness: A conceptual framework and review of the empirical literature. Social Science & Medicine, 51, 1087–1110.
Merlin, J. S., Cen, L., Praestgaard, A., Turner, M., Obando, A., Alpert, C., Woolston, S., Casarett, D., Kostman, J., & Gross, R. (2012a). Pain and physical and psychological symptoms in ambulatory HIV patients in the current treatment era. Journal of Pain and Symptom Management, 43, 638–645.
Merlin, J. S., Westfall, A. O., Raper, J. L., Zinski, A., Norton, W. E., Willig, J. H., et al. (2012b). Pain, mood, and substance abuse in HIV: Implications for clinic visit utilization, ART adherence, and virologic failure. Journal of Acquired Immune Deficiency Syndromes, 61(2), 164.
Merlin, J. S., Zinski, A., Norton, W. E., Ritchie, C. S., Saag, M. S., Mugavero, M. J., Treisman, G., & Hooten, W. M. (2014). A conceptual framework for understanding chronic pain in patients with HIV. Pain Practice, 14, 207–216.
Merlin, J. S., Bulls, H. W., Vucovich, L. A., Edelman, E. J., & Starrels, J. L. (2016). Pharmacologic and non-pharmacologic treatments for chronic pain in individuals with HIV: A systematic review. AIDS Care, 28(12), 1506–1515.
Miaskowski, C., Penko, J. M., Guzman, D., Mattson, J. E., Bangsberg, D. R., & Kushel, M. B. (2011). Occurrence and characteristics of chronic pain in a community-based cohort of indigent adults living with HIV infection. The Journal of Pain, 12, 1004–1016.
Milanini, B., Catella, S., Perkovich, B., Esmaeili-Firidouni, P., Wendelken, L., Paul, R., Greene, M., Ketelle, R., & Valcour, V. (2017). Psychiatric symptom burden in older people living with HIV with and without cognitive impairment: The UCSF HIV over 60 cohort study. AIDS Care, 29(9), 1178–1185.
Mitchell, M. M., Nguyen, T. Q., Maragh-Bass, A. C., Isenberg, S. R., Beach, M. C., & Knowlton, A. R. (2017). Patient-provider engagement and chronic pain in drug-using, primarily African American persons living with HIV/AIDS. AIDS and Behavior, 21(6), 1768–1774.
Morone, N. E., & Greco, C. M. (2007). Mind–body interventions for chronic pain in older adults: A structured review. Pain Medicine, 8(4), 359–375.
Muehlbauer, M., & Crane. (2006). Elder abuse and neglect. Journal of Psychosocial Nursing and Mental Health Services, 44, 43.
Mukaka, M. (2012). A guide to appropriate use of correlation coefficient in medical research. Malawi Medical Journal, 24, 69–71.
Narayan MC (2010) Culture's effects on pain assessment and management. The American Journal of Nursing 110:38–47; quiz 48-9. https://doi.org/10.1097/01.NAJ.0000370157.33223.6d
Navis, A., Jiao, J., George, M. C., Simpson, D., & Robinson-Papp, J. (2018). Comorbid Pain Syndromes in HIV-Associated Peripheral Neuropathy. Pain Medicine, 19(7), 1445–1450. https://doi.org/10.1093/pm/pnx129.
Newshan, G., & Staats, J. A. (2013). Evidence-based pain guidelines in HIV care. Journal of the Association of Nurses in AIDS Care, 24, S112–S126.
Nicholas, P. K., Corless, I. B., & Evans, L. A. (2014). Peripheral neuropathy in HIV: An analysis of evidence-based approaches. Journal of the Association of Nurses in AIDS Care, 25, 318–329.
Nicolaidis, C. (2011). Police officer, deal-maker, or health care provider? Moving to a patient-centered framework for chronic opioid management. Pain Medicine, 12, 890–897.
Nightingale, V. R., Sher, T. G., Mattson, M., Thilges, S., & Hansen, N. B. (2011). The effects of traumatic stressors and HIV-related trauma symptoms on health and health related quality of life. AIDS and Behavior, 15, 1870–1878.
Nygaard, H. A., & Jarland, M. (2006). The checklist of nonverbal pain indicators (CNPI): Testing of reliability and validity in Norwegian nursing homes. Age and Ageing, 35, 79–81 doi: 35/1/79 [pii].
O'Connor, A. B., & Dworkin, R. H. (2009). Treatment of neuropathic pain: An overview of recent guidelines. The American Journal of Medicine, 122, S22–S32.
Ohnhaus, E. E., & Adler, R. (1975). Methodological problems in the measurement of pain: A comparison between the verbal rating scale and the visual analogue scale. Pain, 1, 379–384.
Papaleontiou, M., Henderson Jr., C. R., Turner, B. J., Moore, A. A., Olkhovskaya, Y., Amanfo, L., & Reid, M. C. (2010). Outcomes associated with opioid use in the treatment of chronic noncancer pain in older adults: A systematic review and meta-analysis. Journal of the American Geriatrics Society, 58, 1353–1369.
Phillips, T. J., Cherry, C. L., Cox, S., Marshall, S. J., & Rice, A. S. (2010a). Pharmacological treatment of painful HIV-associated sensory neuropathy: A systematic review and meta-analysis of randomised controlled trials. PLoS One, 5, e14433.
Phillips, T., Cherry, C., Moss, P., & Rice, A. (2010b). Painful HIV-associated sensory neuropathy. IASP-Pain: Clinical Updates, 18(13), 1–8.
Portenoy, R. (2006). Development and testing of a neuropathic pain screening questionnaire: ID pain. Current Medical Research and Opinion, 22, 1555–1565.
Reinert, D. F., & Allen, J. P. (2007). The alcohol use disorders identification test: An update of research findings. Alcoholism: Clinical and Experimental Research, 31, 185–199.
Robinson-Papp, J., Morgello, S., Vaida, F., Fitzsimons, C., Simpson, D., Elliott, K., Al-Lozi, M., Gelman, B., Clifford, D., & Marra, C. M. (2010). Association of self-reported painful symptoms with clinical and neurophysiologic signs in HIV-associated sensory neuropathy. PAIN®, 151, 732–736.
Roter, D. (2000). The enduring and evolving nature of the patient–physician relationship. Patient Education and Counseling, 39, 5–15.
Sakai, Y., Ito, K., Hida, T., Ito, S., & Harada, A. (2015). Neuropathic pain in elderly patients with chronic low back painand effects of pregabalin: A preliminary study. Asian spine journal, 9, 254–262.
Schifano, F. (2014). Misuse and abuse of pregabalin and gabapentin: Cause for concern? CNS Drugs, 28, 491–496.
Selin, K. H. (2003). Test-retest reliability of the alcohol use disorder identification test in a general population sample. Alcoholism: Clinical and Experimental Research, 27, 1428–1435.
Sherin, K. M., Sinacore, J. M., Li, X., Zitter, R. E., & Shakil, A. (1998). HITS: A short domestic violence screening tool for use in a family practice setting. Family Medicine-Kansas City, 30, 508–512.
Simbayi, L. C., Kalichman, S. C., Jooste, S., Mathiti, V., Cain, D., & Cherry, C. (2004). Alcohol use and sexual risks for HIV infection among men and women receiving sexually transmitted infection clinic services in Cape Town, South Africa. Journal of Studies on Alcohol, 65, 434–442.
Skinner, H. A. (1982). The drug abuse screening test. Addictive Behaviors, 7, 363–371.
Smith, R. D., Delpech, V. C., Brown, A. E., & Rice, B. D. (2010). HIV transmission and high rates of late diagnoses among adults aged 50 years and over. AIDS, 24, 2109–2115. https://doi.org/10.1097/QAD.0b013e32833c7b9c.
Stuppy, D. J. (1998). The faces pain scale: Reliability and validity with mature adults. Applied Nursing Research, 11, 84–89.
Surratt, H. L., Kurtz, S. P., Levi-Minzi, M. A., Cicero, T. J., Tsuyuki, K., & O'grady, C. L. (2015). Pain treatment and antiretroviral medication adherence among vulnerable HIV-positive patients. AIDS Patient Care and STDs, 29, 186–192.
Taylor, L. J., & Herr, K. (2003). Pain intensity assessment: A comparison of selected pain intensity scales for use in cognitively intact and cognitively impaired African American older adults. Pain Management Nursing, 4, 87–95.
Thomson Micromedex®. (1974-2017). Micromedex. Ann Arbor: Truven Health Analytics, Inc.
Trafton, J. A., Sorrell, J. T., Holodniy, M., Pierson, H., Link, P., Combs, A., & Israelski, D. (2012). Outcomes associated with a cognitive-behavioral chronic pain management program implemented in three public HIV primary care clinics. The Journal of Behavioral Health Services & Research, 39(2), 158–173.
Treede, R. D., Jensen, T. S., Campbell, J. N., Cruccu, G., Dostrovsky, J. O., Griffin, J. W., Hansson, P., Hughes, R., Nurmikko, T., & Serra, J. (2008). Neuropathic pain: Redefinition and a grading system for clinical and research purposes. Neurology, 70, 1630–1635 doi: 01.wnl.0000282763.29778.59 [pii].
Tsao, J. C., & Soto, T. (2009). Pain in persons living with HIV and comorbid psychologic and substance use disorders. The Clinical Journal of Pain, 25, 307–312. https://doi.org/10.1097/AJP.0b013e31819294b7.
Tsao, J. C., Stein, J. A., & Dobalian, A. (2007). Pain, problem drug use history, and aberrant analgesic use behaviors in persons living with HIV. PAIN®, 133, 128–137.
Tsao, J. C., Plankey, M. W., & Young, M. A. (2012). Pain, psychological symptoms and prescription drug misuse in HIV: A literature review. J Pain Manag, 5, 111–118.
Turk, D., Swanson, K., & Gatchel, R. (2008). Predicting opioid misuse by chronic pain patients: A systematic review and literature synthesis. The Clinical Journal of Pain, 24(6), 497–508. https://doi.org/10.1097/AJP.0b013e31816b1070.
Uebelacker, L., Weisberg, R., Herman, D., Bailey, G., Pinkston-Camp, M., Garnaat, S., & Stein, M. (2016). Pilot randomized trial of collaborative behavioral treatment for chronic pain and depression in persons living with HIV/AIDS. AIDS and Behavior, 20(8), 1675–1681. https://doi.org/10.1007/s10461-016-1397-7.
UNAIDS, H. (2013). Aging. Genève: A special supplement to the UNAIDS report on the global AIDS epidemic.
University of Liverpool (2017) HIV-Druginteractions.org. http://www.hiv-druginteractions.org/. Accessed July 122017.
Vance, D. E., & Robinson, F. P. (2004). Reconciling successful aging with HIV: A biopsychosocial overview. Journal of HIV/AIDS & Social Services, 3(1), 59–78.
Varrassi, G., Müller-Schwefe, G., Pergolizzi, J., Oronska, A., Morlion, B., Mavrocordatos, P., Margarit, C., Mangas, C., Jaksch, W., & Huygen, F. (2010). Pharmacological treatment of chronic pain–the need for CHANGE. Current Medical Research and Opinion, 26, 1231–1245.
Volkow, N. D., Koob, G. F., & McLellan, A. T. (2016). Neurobiologic advances from the brain disease model of addiction. The New England Journal of Medicine, 374(4), 363–371. https://doi.org/10.1056/NEJMra1511480.
Ware, L. J., Epps, C. D., Herr, K., & Packard, A. (2006). Evaluation of the revised faces pain scale, verbal descriptor scale, numeric rating scale, and Iowa pain thermometer in older minority adults. Pain Management Nursing, 7, 117–125.
Watkins, C. C., & Treisman, G. J. (2012). Neuropsychiatric complications of aging with HIV. Journal of Neurovirology, 18, 277–290.
Weisberg, J. N. (2000). Personality and personality disorders in chronic pain. Current Review of Pain, 4, 60–70.
Wewers, M. E., & Lowe, N. K. (1990). A critical review of visual analogue scales in the measurement of clinical phenomena. Research in Nursing & Health, 13, 227–236.
Wiebe, L. A., Phillips, T. J., Li, J., Allen, J. A., & Shetty, K. (2011). Pain in HIV: An evolving epidemic. The Journal of Pain, 12, 619–624.
Williamson, A., & Hoggart, B. (2005). Pain: A review of three commonly used pain rating scales. Journal of Clinical Nursing, 14, 798–804.
Wilson-Stronks, A., Lee, K. K., Cordero, C. L., Kopp, A., & Galvez, E. (2008). One size does not fit all: Meeting the health care needs of diverse populations. Oakbrook Terrace: The Joint Commission.
World Health Organization (WHO). (2009). WHO’s Pain Relief Ladder. www.who.int/cancer/palliative/painladder/en/ Accessed July 16, 2017.
World Health Organization (WHO). (2018). Lexicon of alcohol and drug terms published by the World Health Organization.
Yudko, E., Lozhkina, O., & Fouts, A. (2007). A comprehensive review of the psychometric properties of the drug abuse screening test. Journal of Substance Abuse Treatment, 32, 189–198.
Zanjani, F., Saboe, K., & Oslin, D. (2007). Age difference in rates of mental health/substance abuse and behavioral care in HIV-positive adults. AIDS Patient Care and STDs, 21(5), 347–355.
Zeidan, F., Adler-Neal, A. L., Wells, R. E., Stagnaro, E., May, L. M., Eisenach, J. C., McHaffie, J. G., & Coghill, R. C. (2016). Mindfulness-meditation-based pain relief is not mediated by endogenous opioids. Journal of Neuroscience, 36(11), 3391–3397.
Acknowledgments
The authors gratefully acknowledge the contributions of Dr. Linda Honan, Professor of Nursing, Yale University, for her expert guidance and review of the final stages of this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest.
Informed Consent
Obtained from all individual participants of studies included for this research. For this type of study formal consent is not required.
Ethical Treatment of Experimental Subjects (Animal and Human)
This article does not contain any studies with human participants or animals performed by any of the authors.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Miller, T.R., Halkitis, P.N. & Durvasula, R. A Biopsychosocial Approach to Managing HIV-Related Pain and Associated Substance Abuse in Older Adults: a Review. Ageing Int 44, 74–116 (2019). https://doi.org/10.1007/s12126-018-9333-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12126-018-9333-y