Abstract
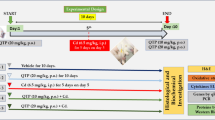
Cerebral ischemia is characterized by several pathological reaction evolving over time. Hyperactivation of glutamatergic neurons is the main factor leading to excitotoxicity which potentiates oxidative stress and triggers the mechanisms of neural apoptosis after cerebral ischemia. However, it is unclear whether glutamate in the ventral hippocampal Cornus Ammonis 1 (vCA1) acts a part in neurological deficits, pain perception, anxiety, and depression induced by ischemic stroke. We investigated the effects of chemogenetic inhibition or activation of vCA1 pyramidal neurons which are mainly glutamatergic neurons on sequelae induced by cerebral ischemia. Our results revealed that inhibition of vCA1 pyramidal neurons by chemogenetics alleviated neurological deficits, pain perception, anxiety, and depression caused by cerebral ischemia in mice, but activation of vCA1 pyramidal neurons had limited effects. Moreover, we found that stroke was accompanied by decreased levels of cAMP-response element-binding protein (CREB) and brain-derived neurotrophic factor (BDNF) in vCA1, which are modulated by glutamate. In this study, overexpression of CREB protein in pyramidal neurons in vCA1 by AAV virus significantly upregulated the content of BDNF and ameliorated the dysfunction induced by ischemic stroke. Our results demonstrated activation of the CREB-BDNF pathway in vCA1 pyramidal neurons significantly improved neurological deficits, pain perception, anxiety, and depression induced by ischemic stroke.








Similar content being viewed by others
Data Availability
The datasets generated and/or analyzed during the current study are available upon reasonable request.
References
Song M, Zhou Y, Fan X (2022) Mitochondrial quality and quantity control: mitophagy is a potential therapeutic target for ischemic stroke. Mol Neurobiol 59(5):3110–3123. https://doi.org/10.1007/s12035-022-02795-6
Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP et al (2020) Heart disease and stroke statistics-2020 update: a report from the American heart association. Circulation 141(9):e139–e596. https://doi.org/10.1161/CIR.0000000000000757
Chamorro A, Dirnagl U, Urra X, Planas AM (2016) Neuroprotection in acute stroke: targeting excitotoxicity, oxidative and nitrosative stress, and inflammation. Lancet Neurol 15(8):869–881. https://doi.org/10.1016/S1474-4422(16)00114-9
Manochkumar J, Doss C, El-Seedi HR, Efferth T, Ramamoorthy S (2021) The neuroprotective potential of carotenoids in vitro and in vivo. Phytomed 91:153676. https://doi.org/10.1016/j.phymed.2021.153676
Campbell B, Khatri P (2020) Stroke. Lancet 396(10244):129–142. https://doi.org/10.1016/S0140-6736(20)31179-X
Gorelick PB (2019) The global burden of stroke: persistent and disabling. Lancet Neurol 18(5):417–418. https://doi.org/10.1016/S1474-4422(19)30030-4
Grigoras IF, Stagg CJ (2021) Recent advances in the role of excitation-inhibition balance in motor recovery post-stroke. Fac Rev 10:58. https://doi.org/10.12703/r/10-58
Rodriguez-Chavez V, Moran J, Molina-Salinas G, Zepeda RW, Rodriguez MC, Picazo O et al (2021) Participation of glutamatergic ionotropic receptors in excitotoxicity: the neuroprotective role of prolactin. Neurosci 461:180–193. https://doi.org/10.1016/j.neuroscience.2021.02.027
Mira RG, Cerpa W (2021) Building a bridge between NMDAR-mediated excitotoxicity and mitochondrial dysfunction in chronic and acute diseases. Cell Mol Neurobiol 41(7):1413–1430. https://doi.org/10.1007/s10571-020-00924-0
Chen QY, Li XH, Zhuo M (2021) NMDA receptors and synaptic plasticity in the anterior cingulate cortex. Neuropharmacol 197:108749. https://doi.org/10.1016/j.neuropharm.2021.108749
de Sousa RT, Loch AA, Carvalho AF, Brunoni AR, Haddad MR, Henter ID et al (2017) Genetic studies on the tripartite glutamate synapse in the pathophysiology and therapeutics of mood disorders. Neuropsychopharmacol 42(4):787–800. https://doi.org/10.1038/npp.2016.149
Lyu Z, Guo Y, Gong Y, Fan W, Dou B, Li N et al (2021) The role of neuroglial crosstalk and synaptic plasticity-mediated central sensitization in acupuncture analgesia. Neural Plast 2021:8881557. https://doi.org/10.1155/2021/8881557
Cifuentes F, Morales MA (2021) Functional implications of neurotransmitter segregation. Front Neural Circuits 15:738516. https://doi.org/10.3389/fncir.2021.738516
Saura CA, Cardinaux JR (2017) Emerging roles of CREB-regulated transcription coactivators in brain physiology and pathology. Trends Neurosci 40(12):720–733. https://doi.org/10.1016/j.tins.2017.10.002
Kuo CY, Lin CH, Lane HY (2021) Molecular basis of late-life depression. Int J Mol Sci 22(14):7421. https://doi.org/10.3390/ijms22147421
Zheng J, Jiang YY, Xu LC, Ma LY, Liu FY, Cui S, at al, (2017) Adult hippocampal neurogenesis along the dorsoventral axis contributes differentially to environmental enrichment combined with voluntary exercise in alleviating chronic inflammatory pain in mice. J Neurosci 37(15):4145–4157. https://doi.org/10.1523/JNEUROSCI.3333-16.2017
Lai TW, Zhang S, Wang YT (2014) Excitotoxicity and stroke: identifying novel targets for neuroprotection. Prog Neurobiol 115:157–188. https://doi.org/10.1016/j.pneurobio.2013.11.006
Caracciolo L, Marosi M, Mazzitelli J, Latifi S, Sano Y, Galvan L et al (2018) CREB controls cortical circuit plasticity and functional recovery after stroke. Nat Commun 9(1):2250. https://doi.org/10.1038/s41467-018-04445-9
Bannerman DM, Sprengel R, Sanderson DJ, McHugh SB, Rawlins JN, Monyer H et al (2014) Hippocampal synaptic plasticity, spatial memory and anxiety. Nat Rev Neurosci 15(3):181–192. https://doi.org/10.1038/nrn3677
Ma L, Yue L, Zhang Y, Wang Y, Han B, Cui S et al (2019) Spontaneous pain disrupts ventral hippocampal CA1-infralimbic cortex connectivity and modulates pain progression in rats with peripheral inflammation. Cell Rep 29(6):1579–1593. https://doi.org/10.1016/j.celrep.2019.10.002
Jiang YY, Shao S, Zhang Y, Zheng J, Chen X, Cui S et al (2018) Neural pathways in medial septal cholinergic modulation of chronic pain: distinct contribution of the anterior cingulate cortex and ventral hippocampus. Pain 159(8):1550–1561. https://doi.org/10.1097/j.pain.0000000000001240
Jimenez JC, Su K, Goldberg AR, Luna VM, Biane JS, Ordek G et al (2018) Anxiety cells in a hippocampal-hypothalamic circuit. Neuron 97(3):670–683. https://doi.org/10.1016/j.neuron.2018.01.016
Ma H, Li C, Wang J, Zhang X, Li M, Zhang R et al (2021) Amygdala-hippocampal innervation modulates stress-induced depressive-like behaviors through AMPA receptors. Proc Natl Acad Sci U S A 118(6):e2019409118. https://doi.org/10.1073/pnas.2019409118
Woods D, Jiang Q, Chu XP (2020) Monoclonal antibody as an emerging therapy for acute ischemic stroke. Int J Physiol Pathophysiol Pharmacol 12(4):95–106
Sternson SM, Roth BL (2014) Chemogenetic tools to interrogate brain functions. Annu Rev of Neurosci 37:387–407. https://doi.org/10.1146/annurev-neuro-071013-014048
Guettier JM, Gautam D, Scarselli M, Ruiz DAI, Li JH, Rosemond E et al (2009) A chemical-genetic approach to study G protein regulation of beta cell function in vivo. Proc Natl Acad Sci U S A 106(45):19197–19202. https://doi.org/10.1073/pnas.0906593106
Percie DSN, Hurst V, Ahluwalia A, Alam S, Avey MT, Baker M et al (2020) The ARRIVE guidelines 2.0: updated guidelines for reporting animal research. J Cereb Blood Flow Metab 40(9):1769–1777. https://doi.org/10.1177/0271678X20943823
Morris GP, Wright AL, Tan RP, Gladbach A, Ittner LM, Vissel B (2016) A comparative study of variables influencing ischemic injury in the Longa and Koizumi methods of intraluminal filament middle cerebral artery occlusion in mice. PLoS One 11(2):e148503. https://doi.org/10.1371/journal.pone.0148503
Rousselet E, Kriz J, Seidah NG (2012) Mouse model of intraluminal MCAO: cerebral infarct evaluation by cresyl violet staining. J Vis Exp https://doi.org/10.3791/4038
Nouraee C, Fisher M, Di Napoli M, Salazar P, Farr TD, Jafarli A et al (2019) A brief review of edema-adjusted infarct volume measurement techniques for rodent focal cerebral ischemia models with practical recommendations. J Vasc Interv Neurol 10(3):38–45
Mosienko V, Bert B, Beis D, Matthes S, Fink H, Bader M et al (2012) Exaggerated aggression and decreased anxiety in mice deficient in brain serotonin. Transl Psychiatry 2:e122. https://doi.org/10.1038/tp.2012.44
Yankelevitch-Yahav R, Franko M, Huly A, Doron R (2015) The forced swim test as a model of depressive-like behavior. J Vis Exp https://doi.org/10.3791/52587
Mahler SV, Vazey EM, Beckley JT, Keistler CR, McGlinchey EM, Kaufling J et al (2014) Designer receptors show role for ventral pallidum input to ventral tegmental area in cocaine seeking. Nat Neurosci 17(4):577–585. https://doi.org/10.1038/nn.3664
Zheng J, Li HL, Tian N, Liu F, Wang L, Yin Y et al (2020) Interneuron accumulation of phosphorylated tau impairs adult hippocampal neurogenesis by suppressing GABAergic transmission. Cell Stem Cell 26(3):331–345. https://doi.org/10.1016/j.stem.2019.12.015
Sun H, Fu S, Cui S, Yin X, Sun X, Qi X et al (2020) Development of a CRISPR-SaCas9 system for projection- and function-specific gene editing in the rat brain. Sci Adv 6(12):y6687. https://doi.org/10.1126/sciadv.aay6687
Harciarek M, Mankowska A (2021) Hemispheric stroke: Mood disorders. Handb Clin Neurol 183:155–167. https://doi.org/10.1016/B978-0-12-822290-4.00007-4
Murphy TH, Corbett D (2009) Plasticity during stroke recovery: from synapse to behaviour. Nat Rev Neurosci 10(12):861–872. https://doi.org/10.1038/nrn2735
Zhang J, Song S, Zhao Y, Ma G, Jin Y, Zheng ZJ (2021) Economic burden of comorbid chronic conditions among survivors of stroke in China: 10-year longitudinal study. BMC Health Serv Res 21(1):978. https://doi.org/10.1186/s12913-021-07010-1
Boot E, Ekker MS, Putaala J, Kittner S, De Leeuw FE, Tuladhar AM (2020) Ischaemic stroke in young adults: a global perspective. J Neurol Neurosurg Psychiatry 91(4):411–417. https://doi.org/10.1136/jnnp-2019-322424
Ayerbe L, Ayis S, Wolfe CD, Rudd AG (2013) Natural history, predictors and outcomes of depression after stroke: systematic review and meta-analysis. Br J Psychiatry 202(1):14–21. https://doi.org/10.1192/bjp.bp.111.107664
Knapp P, Dunn-Roberts A, Sahib N, Cook L, Astin F, Kontou E et al (2020) Frequency of anxiety after stroke: an updated systematic review and meta-analysis of observational studies. Int J Stroke 15(3):244–255. https://doi.org/10.1177/1747493019896958
Zhang SJ, Steijaert MN, Lau D, Schutz G, Delucinge-Vivier C, Descombes P et al (2007) Decoding NMDA receptor signaling: identification of genomic programs specifying neuronal survival and death. Neuron 53(4):549–562. https://doi.org/10.1016/j.neuron.2007.01.025
Hardingham GE, Arnold FJ, Bading H (2001) Nuclear calcium signaling controls CREB-mediated gene expression triggered by synaptic activity. Nat Neurosci 4(3):261–267. https://doi.org/10.1038/85109
Lonze BE, Riccio A, Cohen S, Ginty DD (2002) Apoptosis, axonal growth defects, and degeneration of peripheral neurons in mice lacking CREB. Neuron 34(3):371–385. https://doi.org/10.1016/s0896-6273(02)00686-4
Simpkins AN, Tahsili-Fahadan P, Buchwald N, De Prey J, Farooqui A, Mugge LA et al (2021) Adapting clinical practice of thrombolysis for acute ischemic stroke beyond 4.5 hours: a review of the literature. J Stroke Cerebrovasc Dis 30(11):106059. https://doi.org/10.1016/j.jstrokecerebrovasdis.2021.106059
Navis A, Garcia-Santibanez R, Skliut M (2019) Epidemiology and outcomes of ischemic stroke and transient ischemic attack in the adult and geriatric population. J Stroke Cerebrovasc Dis 28(1):84–89. https://doi.org/10.1016/j.jstrokecerebrovasdis.2018.09.013
Funding
This work is supported by the National Natural Science Foundation of China (No. 81901196 and No. 82001182).
Author information
Authors and Affiliations
Contributions
YJ, QL, and MS developed the study concept and experimental design. YJ and YZ were involved in conducting the experiment and data collection. YJ, CW, and MS analyzed the data. YJ wrote the paper, and MS edited the paper. All coauthors have approved the paper submitted for publication.
Corresponding author
Ethics declarations
Ethics Approval
The animal study was reviewed and approved by the Institutional Animal Care and Use Committee of Beijing Neurosurgical Institute (Permit Number: 201904004).
Consent to Participate
This is not applicable.
Consent for Publication
All authors have read and approved the submission of the manuscript.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jiang, Y., Liu, Q., Zhao, Y. et al. Activation of CREB-BDNF Pathway in Pyramidal Neurons in the Hippocampus Improves the Neurological Outcome of Mice with Ischemic Stroke. Mol Neurobiol 60, 1766–1781 (2023). https://doi.org/10.1007/s12035-022-03174-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-022-03174-x