Abstract
Background
Patients who have undergone intracranial neurosurgical procedures have traditionally been admitted to an intensive care unit (ICU) for close postoperative neurological observation. The purpose of this study was to systematically review the evidence for routine ICU admission in patients undergoing intracranial neurosurgical procedures and to evaluate the safety of alternative postoperative pathways.
Methods
We were interested in identifying studies that examined selected patients who presented for elective, non-emergent intracranial surgery whose postoperative outcomes were compared as a function of ICU versus non-ICU admission. A systematic review was performed in July 2016 using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist of the Medline database. The search strategy was created based on the following key words: “craniotomy,” “neurosurgical procedure,” and “intensive care unit.”
Results
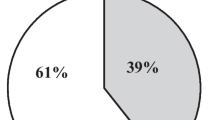
The nine articles that satisfied the inclusion criteria yielded a total of 2227 patients. Of these patients, 879 were observed in a non-ICU setting. The most frequent diagnoses were supratentorial brain tumors, followed by patients with cerebrovascular diseases and infratentorial brain tumors. Three percent (30/879) of the patients originally assigned to floor or intermediate care status were transferred to the ICU. The most frequently observed neurological complications leading to ICU transfer were delayed postoperative neurological recovery, seizures, worsening of neurological deficits, hemiparesis, and cranial nerves deficits.
Conclusion
Our systematic review demonstrates that routine postoperative ICU admission may not benefit carefully selected patients who have undergone elective intracranial neurosurgical procedures. In addition, limiting routine ICU admission may result in significant cost savings.

From [41]
Similar content being viewed by others
References
Kelly DF. Neurosurgical postoperative care. Neurosurg Clin N Am. 1994;5:789–810.
Bruder NJ. Awakening management after neurosurgery for intracranial tumours. Curr Opin Anaesthesiol. 2002;15:477–82.
Weissman C, Klein N. Who receives postoperative intensive and intermediate care? J Clin Anesth. 2008;20:263–70.
Hanak BW, Walcott BP, Nahed BV, Muzikansky A, Mian MK, Kimberly WT, et al. Postoperative intensive care unit requirements after elective craniotomy. World Neurosurg. 2014;81:165–72.
Beauregard CL, Friedman WA. Routine use of postoperative ICU care for elective craniotomy: a cost-benefit analysis. Surg Neurol. 2003;60:483–9.
Zimmerman JE, Junker CD, Becker RB, Draper EA, Wagner DP, Knaus WA. Neurological intensive care admissions: identifying candidates for intermediate care and the services they receive. Neurosurgery. 1998;42:91–102.
Knaus WA, Draper E, Lawrence DE, Wagner DP, Zimmerman JE. Neurosurgical admissions to the intensive care unit: intensive monitoring versus intensive therapy. Neurosurgery. 1981;8:438–42.
McLaughlin N, Buxey F, Chaw K, Martin NA. Value-based neurosurgery: the example of microvascular decompression surgery. J Neurosurg. 2014;120:462–72.
Schneider MA, Pomidor MA. The value of a progressive care environment for neurosurgical patients. J Neurosci Nurs. 2014;46(306–311):6p.
Ziser A, Alkobi M, Markovits R, Rozenberg B. The postanaesthesia care unit as a temporary admission location due to intensive care and ward overflow. Br J Anaesth. 2002;88:577–9.
Lindsay M. Is the postanesthesia care unit becoming an intensive care unit? J PeriAnesthesia Nurs. 1999;14:73–7.
Boulton M, Bernstein M. Outpatient brain tumor surgery: innovation in surgical neurooncology. J Neurosurg. 2008;108:649–54.
Grundy PL, Weidmann C, Bernstein M. Day-case neurosurgery for brain tumours: the early United Kingdom experience. Br J Neurosurg. 2008;22:360–7.
Rhondali O, Genty C, Halle C, Gardellin M, Ollinet C, Oddoux M, et al. Do patients still require admission to an intensive care unit after elective craniotomy for brain surgery? J Neurosurg Anesthesiol. 2011;23:118–23.
Bui JQH, Mendis RL, van Gelder JM, Sheridan MMP, Wright KM, Jaeger M. Is postoperative intensive care unit admission a prerequisite for elective craniotomy? J Neurosurg. 2011;115:1236–41.
Terada Y, Inoue S, Tanaka Y, Kawaguchi M, Hirai K, Furuya H. The impact of postoperative intensive care on outcomes in elective neurosurgical patients in good physical condition: a single centre propensity case-matched study. Can J Anesth. 2010;57:1089–94.
Ziai WC, Varelas PN, Zeger SL, Mirski MA, Ulatowski JA. Neurologic intensive care resource use after brain tumor surgery: an analysis of indications and alternative strategies. Crit Care Med. 2003;31:2782–7.
Nitahara JA, Valencia M, Bronstein MA. Medical case management after laminectomy or craniotomy: Do all patients benefit from admission to the intensive care unit? Neurosurg Focus. 1998;5:e4.
Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100:1619–36.
Teplick R, Caldera DL, Gilbert JP, Cullen DJ. Benefit of elective intensive care admission after certain operations. Anesth Analg. 1983;62:572–7.
Reponen E, Tuominen H, Korja M. Evidence for the use of preoperative risk assessment scores in elective cranial neurosurgery: a systematic review of the literature. Anesth Analg. 2014;119:420–32.
Reponen E, Korja M, Niemi T, Silvasti-Lundell M, Hernesniemi J, Tuominen H. Preoperative identification of neurosurgery patients with a high risk of in-hospital complications: a prospective cohort of 418 consecutive elective craniotomy patients. J Neurosurg. 2015;123:1–11.
Anthofer J, Wester M, Zeman F, Brawanski A, Schebesch K-M. Case-control study of patients at risk of medical complications after elective craniotomy. World Neurosurg. 2016;91:58–65.
Cai Y-H, Wang H-T, Zhou J-X. Perioperative predictors of extubation failure and the effect on clinical outcome after infratentorial craniotomy. Med Sci Monit. 2016;22:2431–8.
Taylor WA, Thomas NW, Wellings JA, Bell BA. Timing of postoperative intracranial hematoma development and implications for the best use of neurosurgical intensive care. J Neurosurg. 1995;82:48–50.
Fontes RBV, Smith AP, Muñoz LF, Byrne RW, Traynelis VC. Relevance of early head CT scans following neurosurgical procedures: an analysis of 892 intracranial procedures at Rush University Medical Center. J Neurosurg. 2014;121:307–12.
Dube SK, Rath GP, Bharti SJ, Bindra A, Vanamoorthy P, Gupta N, et al. Causes of tracheal re-intubation after craniotomy: a prospective study. Saudi J Anaesth. 2013;7:410–4.
Dasta JF, McLaughlin TP, Mody SH, Tak Piech C. Daily cost of an intensive care unit day: the contribution of mechanical ventilation*. Crit Care Med. 2005;33:1266–71.
Milbrandt EB, Kersten A, Rahim MT, Dremsizov TT, Clermont G, Cooper LM, et al. Growth of intensive care unit resource use and its estimated cost in medicare. Crit Care Med. 2008;36:2504–10.
Moerer O, Plock E, Mgbor U, Schmid A, Schneider H, Wischnewsky MB, et al. A German national prevalence study on the cost of intensive care: an evaluation from 51 intensive care units. Crit Care. 2007;11:R69.
Shorr AF. An update on cost-effectiveness analysis in critical care. Curr Opin Crit Care. 2002;8:337–43.
Lefrant J-Y, Garrigues B, Pribil C, Bardoulat I, Courtial F, Maurel F, et al. The daily cost of ICU patients: a micro-costing study in 23 French Intensive care units. Anaesth Crit Care Pain Med. 2015;34:151–7.
Lang JM, Meixensberger J, Unterberg AW, Tecklenburg A, Krauss JK. Neurosurgical intensive care unit-essential for good outcomes in neurosurgery? Langenbeck’s Arch Surg. 2011;396:447–51.
Martin DK, Singer PA, Bernstein M. Access to intensive care unit beds for neurosurgery patients: a qualitative case study. J Neurol Neurosurg Psychiatry. 2003;74:1299–303.
Diringer MN, Edwards DF. Admission to a neurologic/neurosurgical intensive care unit is associated with reduced mortality rate after intracerebral hemorrhage. Crit Care Med. 2001;29:635–40.
Dyson EW, Kolias AG, Burnstein RM, Hutchinson PJA, Garnett MR, Menon DK, et al. Neuro-critical care: a valuable placement during foundation and early neurosurgical training. Br J Neurosurg. 2014;28:675–9.
Price JA, Rizk NW. Who goes to the ICU postoperatively? chest. Am Coll Chest Phys. 1999;115:125S–9S.
Ward NS, Teno JM, Curtis JR, Rubenfeld GD, Levy MM. Perceptions of cost constraints, resource limitations, and rationing in United States intensive care units: results of a national survey. Crit Care Med. 2008;36:471–6.
Edbrooke DL, Minelli C, Mills GH, Iapichino G, Pezzi A, Corbella D, et al. Implications of ICU triage decisions on patient mortality: a cost-effectiveness analysis. Crit Care. 2011;15:R56.
Porter ME. What is value in health care? N Engl J Med. 2010;363:2477–81.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi:10.1371/journal.pmed1000097
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Almeida, C.C., Boone, M.D., Laviv, Y. et al. The Utility of Routine Intensive Care Admission for Patients Undergoing Intracranial Neurosurgical Procedures: A Systematic Review. Neurocrit Care 28, 35–42 (2018). https://doi.org/10.1007/s12028-017-0433-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-017-0433-4